Abstract
Background
South Africa’s Western Cape has experienced a dramatic increase in methamphetamine (“meth”) use over the past decade. There is concern that meth may further fuel the HIV epidemic in this country because of its association with risky sexual behaviors. This study describes the prevalence of meth use and its relation to HIV sexual risk behaviors among patrons of alcohol-serving venues.
Methods
Participants (N=3,328) were surveyed in 12 venues in a mixed race township. Logistic regression models were used to examine the relations between meth use and sexual risk behaviors, and structural equation models were used to test whether meth use mediates the relationship between childhood sexual abuse and current sexual risk.
Results
Meth use in the past 4 months was more common among Coloured than Black persons (10.5% vs. 3.5%). Meth users were more likely than non users to use marijuana, inhalants, and injection drugs, have a history of childhood sexual and/or physical abuse, and experience and/or perpetrate intimate partner violence. Among both men and women, meth use was associated with greater odds of engaging in sexual risk behaviors, and meth use partially mediated the relationships between childhood sexual abuse and all sexual risk behaviors.
Conclusions
Meth users in this setting are at increased risk for HIV due to their greater likelihood of engaging in sexual risk behaviors and being in violent relationships. There is an urgent need to provide targeted HIV prevention and substance abuse treatment to meth users living in townships in Cape Town.
Keywords: methamphetamine, sexual risk behavior, interpersonal violence, HIV/AIDS, South Africa
1. INTRODUCTION
The Western Cape of South Africa has experienced a dramatic increase in methamphetamine (“meth”) use over the past decade. With 5.3 million adults living with HIV/AIDS (the most of any country; SSA, 2010; UNAIDS, 2008), there is concern that meth use may further fuel the HIV epidemic due to its association with sexual risk behaviors (SRBs; Morris and Parry, 2006; Pluddemann et al., 2008a; Simbayi et al., 2006; Wechsberg et al., 2008). However, little data is available on the relation between meth use and HIV sexual risk in South Africa.
Meth, the second most widely abused drug worldwide (UNODC, 2009), has only recently become prevalent in South Africa (Parry et al., 2008). Here meth is typically smoked and is known as “tik” because of the sound it makes when heated and inhaled. Data from treatment facilities in the Western Cape indicate that the proportion of patients with meth as their primary substance of abuse increased from <1% in 2000 to 34% in 2010 (Pluddemann et al., 2010b). Community-based studies provide further evidence of a growing meth epidemic (Simbayi et al., 2006; Wechsberg et al., 2010). Meth use is most common among young adults, males, and ‘Coloured’ persons (an ethnic group of historically mixed race people; Pluddemann et al., 2010b; Simbayi et al., 2006; Wechsberg et al., 2010). Since meth users are more likely than non users to report concurrent or hazardous alcohol use (Simbayi et al., 2006; Wechsberg et al., 2010), alcohol-serving venues may be one place in which to reach meth users.
Meth is a stimulant that increases sexual desire, energy, and feelings of euphoria, among other physiological effects (Volkow et al., 2007). Research from around the world has documented that meth use is associated with increased rates of SRBs and HIV infection (Corsi and Booth, 2008; Degenhardt et al., 2010), and is most prevalent among men who have sex with men (MSM; Colfax et al., 2004; Shoptaw and Reback, 2007; Woody et al., 2001). Emerging data indicates that meth users in Cape Town may also engage in SRBs, including multiple partners, unprotected intercourse, and sex for drugs/money (Pluddemann et al., 2008a; Simbayi et al., 2006; Wechsberg et al., 2010). Qualitative research has found that meth is often used to augment sexual experiences (Parry et al., 2008; Sawyer-Kurian et al., 2009). Since many drug users have multiple sex partners, they may be a high-risk population that may promote the wider spread of HIV (Parry et al., 2008).
South Africa’s recent history of political violence and gross inequalities has contributed to a society in which interpersonal violence, including childhood sexual abuse (CSA) and intimate partner violence, is common (Jewkes and Abrahams, 2002; Kaminer et al., 2008; Williams et al., 2007). These experiences may make individuals vulnerable to initiating meth use as a way to manage symptoms of traumatic stress (Cohen et al., 2003; Dube et al., 2003). Meth users are more likely to experience and perpetrate intimate partner violence as adults (Cohen et al., 2003; Sommers et al., 2006). The heightened risk of interpersonal violence among meth users is concerning because of its association with SRBs in South Africa and elsewhere (Dunkle et al., 2006; Jewkes, 2010; Lenderking et al., 1997; Mimiaga et al., 2009; Mosack et al., 2010; Schraufnagel et al., 2010; Senn et al., 2006).
Despite widespread concern about meth, there has been limited empirical research on the intersection of meth use, interpersonal violence, and HIV sexual risk in South Africa. This study describes the prevalence of meth use and its association with SRBs in patrons of alcohol-serving venues. Specifically, we: (1) report the prevalence of meth use by gender and race/ethnicity; (2) compare meth users and non users on demographic characteristics, substance use, and interpersonal violence; (3) examine the association between meth use and SRBs; and (4) test whether meth use mediates the relationships between CSA and SRBs.
2. METHODS
2.1 Procedures
Data were collected as part of a mixed-methods study conducted in alcohol-serving venues in a peri-urban township 15 miles outside of Cape Town’s city center. This township, established in the early 1990s, has a fairly equal number of Xhosa-speaking Black African and Afrikaans-speaking Coloured residents. These terms originate from the Apartheid era, when all individuals had a race classification that determined political and social privileges. Although Coloured people had more privileges than Black people under the Apartheid government, both were subjected to forced relocation and restrictions on employment and mobility. In present day South Africa, individuals continue to self-identify as Black or Coloured, and there is consensus that these are culturally distinct groups in terms of shared language and customs.
Street intercept surveys identified 124 local drinking establishments. Of these, 38 met the initial eligibility criteria of >50 unique sit-down patrons per week and >10% female patrons. Several additional venues were excluded because they were located in areas with violent crime, were not operational on weekdays and/or throughout the year, or refused participation. Of the remaining venues, 12 were selected for diversity in size, location, and race/ethnicity of patrons.
Trained fieldworkers, matched by race/ethnicity, visited the venues for four 1-week periods over 1 year. After building rapport, they approached patrons entering the venue, unless visibly intoxicated, and asked them to complete an anonymous survey (92.5% accepted). After providing oral consent, participants completed a 96-item paper-pencil survey in their preferred language (Xhosa, Afrikaans, or English). A small minority (4.7%) chose to have the survey read by a fieldworker. Fieldworkers protected participants’ privacy by finding less crowed spaces in the venues and ensuring that other patrons kept their distance while the survey was completed. The survey took 10–15 minutes, and participants received a small gift (e.g., key ring). The study was approved by ethics committee in the United States and South Africa.
2.2 Measures
Substance use
Participants reported how often they had used each of the following drugs in the past 4 months: meth (“tik”), marijuana (“dagga”), inhalants (“sniffers”), and injection drugs. Response options were never, a few times, weekly, and daily. Given the highly skewed distribution, we created dichotomous variables indicating any use (yes/no) for each drug. Using the WHO Alcohol Use Disorders Identification Test (AUDIT), three items assessed frequency of drinking, number of drinks on typical drinking days, and frequency of ≥6 drinks on one occasion(Babor et al., 2001). Using the AUDIT scoring guidelines, hazardous drinking was defined as ≥3–4 drinks on a typical drinking day and/or ≥6 drinks on one occasion (Babor et al., 2001).
Childhood abuse
CSA was assessed using one item adapted from the Traumatic Events Questionnaire (TEQ; Kaplan et al., 1995). Specifically, participants were asked, “As a child, were you ever sexually abused (that is, forced to have some kind of sexual contact, like touching, oral sex, or intercourse).” An additional item assessed childhood physical abuse.
Intimate partner violence
For the past 4 months only, participants indicated whether or not they had been hit by a sex partner or forced to have sex when they did not want to (2 items) and/or perpetrated either of these behaviors (2 items). These items were adapted from the Conflict Tactics Scale (CTQ; Straus et al., 1996).
Sexual risk
Participants reported how many women and men they had sex with in the past 4 months and the number of times they had vaginal or anal intercourse with and without a condom. The following dichotomous (yes/no) variables were created: sexual activity, multiple (≥2) sex partners, and unprotected sex. They also reported, for the past 4 months, whether or not they had “sold” or “bought” sex for money, alcohol/drugs, or a place to stay (2 items) or been diagnosed with a sexually transmitted infection (e.g., syphilis, gonorrhea). Finally, participants reported whether they had ever been tested for HIV and the result of their most recent test.
Demographics
A single item assessed race/ethnicity: “What best describes you?” Response options were Black, White, Indian, Coloured, and other; participants were encouraged to select just one. They also reported gender, age, marital status, employment, and education. Men who had male sex partners in the past 4 months were categorized as “MSM” (86% of these men also had sex with women); all others were categorized as “no MSM.”
2.3 Data analysis
Surveys were scanned into a database using Remark Office OMR 6.0, and manual checks identified errors. On the survey, participants were asked if, when, and where they had “completed a survey like this before.” Approximately one fifth indicated that they had previously completed the survey and were eliminated from this analysis. Since the vast majority of participants (98.8%) identified as either Coloured or Black, we excluded individuals of other race/ethnicities. Furthermore, since meth use is most common among young adults, we restricted the sample to the 3,415 participants who were 18–50 years old (only one meth user was >50). Five participants did not report gender and 82 did not answer the question about meth use, leaving a final sample of 3,328.
Analyses were conducted in SPSS 19.0 and MPlus 6.1. First, prevalence of meth use by gender (women, MSM, and other men) and race/ethnicity (Coloured and Black) was examined using χ2-tests. Second, meth users and non users were compared on demographics, substance use, and interpersonal violence using t-tests for continuous variables and χ2-tests for categorical variables. Third, a series of logistic regression models tested the relations between meth use and sexual risk variables: multiple partners, unprotected sex, selling sex, buying sex, sexually transmitted infection, HIV-positive status, and MSM for men. All models were run separately for men and women and controlled for age, race/ethnicity, and education (which differed between meth users and non users). Fourth, the hypothesized mediated pathways from CSA to SRBs through meth use were tested by first estimating the overall relations between CSA and each SRB and, if significant, testing whether meth use significantly mediated these relations. A structural equation model depicting all mediation hypotheses of interest provides estimates of the paths from CSA to meth use and from meth use to each SRB.
3. RESULTS
Participants were 18–50 years old (M=29.9, SD=5.6), with similar proportions across gender (56.3% male, 43.7% female) and race/ethnicity (59.1% Black, 40.9% Coloured). About half did not finish secondary school (52.6%) and were unemployed (53.6%). The majority were single (77.5%) and lived within walking distance of the venue (88.1%). Most reported hazardous drinking (90.4%), but current drug use was uncommon (17.3% marijuana, 6.4% meth, 3.6% inhalants, 2.5% injection drugs).
3.1 Prevalence of recent meth use
In the full sample, 6.4% of participants reported using meth in the past 4 months (Table 1). Meth use was more common among Coloured than Black participants (10.5% vs. 3.5%; χ2(1)=66.23, p<.001). Among Black participants only, meth use was more common among MSM than among women and non-MSM males. Among meth users, 63.7% used it occasionally, 20.3% weekly, and 16.0% daily. Black participants were more likely to have used meth at least weekly (46.8% vs. 24.4%; χ2(1)=11.12, p=.001) and to have used inhalants (63.2% vs. 18.6%; χ2(1)=41.19, p<.001) and injection drugs (54.4% vs. 14.1%; χ2(1)=37.81, p<.001). These race/ethnicity differences persisted when analyses were stratified by gender.
Table 1.
Prevalence of meth use by race/ethnicity and gender/MSM in the full sample (n= 3,328)
| Total | Women | Men | |||
|---|---|---|---|---|---|
| No MSM | MSM1 | χ2 value | |||
| Coloured | 10.5% (143/1,360) | 10.4% (81/780) | 10.6% (55/519) | 11.5% (7/61) | 0.08 |
| Black | 3.5% (69/1,968) | 2.1% (14/675) | 3.6% (41/1,136) | 8.9% (14/157) | 17.72*** |
p < .001
MSM: men who had sex with men, including men who had sex with men and women.
3.2 Comparison of meth users and non users
As shown in Table 2, meth users were younger than non users, more likely to be Coloured, and less likely to have finished secondary school. There was no difference between meth users and non users on hazardous drinking, but meth users were more likely to report use of marijuana, inhalants, and injection drugs. The relationship between meth and injection drug use was particularly strong among Black participants, with 54.4% of Black meth users reporting recent injection drug use, compared to just 0.7% of Black non users (χ2(1)=764.2, p<.001). Among men and women, meth users were more likely than non users to experience all six types of interpersonal violence. Considering meth users only, those who also used other drugs were more likely than those who did not to have experienced childhood physical abuse (39.0% vs. 14.8%; χ2(1)=8.04, p=.005), but there was no difference between the groups on other types of interpersonal violence (all p>.05). Among meth users currently involved in violent intimate partnerships, there was large overlap between experiencing and perpetrating violence, with 39.5% of women and 25.0% of men reporting both behaviors. MSM were generally more likely than other men to report CSA (20.4% vs. 7.6%) and recently experience (22.7% vs. 11.1%) and perpetrate (16.3% vs. 10.0%) intimate partner violence (all p<.01). After excluding MSM from the analysis, meth use remained strongly associated with each of these variables (all p<.01).
Table 2.
Comparison of meth users and non meth users (n=3,328)
| WOMEN | MEN | |||||||
|---|---|---|---|---|---|---|---|---|
| Total n=1,455 | Meth n=95 | No meth n=1,360 | Test of differences | Total n=1,873 | Meth n=117 | No meth n=1,756 | Test of differences | |
| Demographics | ||||||||
| Age, M (SD) | 30.1 (9.2) | 26.4 (7.5) | 30.3 (9.3) | 4.04*** | 29.7 (8.1) | 27.1 (7.0) | 30.0 (8.1) | 3.75*** |
| Black (vs. Coloured) | 46.4% | 14.7% | 48.6% | 40.95*** | 69.0% | 47.0% | 70.5% | 28.32*** |
| Finished secondary school | 33.8% | 24.2% | 34.5% | 4.21* | 57.9% | 33.3% | 59.5% | 30.05*** |
| Currently employed | 72.8% | 77.9% | 72.5% | 1.32 | 38.7% | 43.6% | 38.3% | 1.27 |
| Married | 23.4% | 21.1% | 23.6% | 0.31 | 21.4% | 14.9% | 21.9% | 3.07 |
| Current substance abuse | ||||||||
| Hazardous drinking | 86.7% | 89.5% | 86.5% | 0.66 | 93.4% | 95.7% | 93.2% | 1.09 |
| Marijuana | 11.6% | 53.7% | 8.7% | 170.33*** | 21.7% | 70.5% | 18.5% | 174.54*** |
| Inhalants | 2.0% | 20.2% | 0.7% | 170.64*** | 4.9% | 43.9% | 2.3% | 397.51*** |
| Injection drugs | 1.6% | 15.8% | 0.6% | 131.89*** | 3.2% | 36.5% | 1.0% | 446.22*** |
| Interpersonal violence | ||||||||
| Childhood physical abuse | 19.2% | 30.9% | 18.4% | 8.86** | 21.9% | 34.5% | 21.0% | 11.53** |
| Childhood sexual abuse | 9.4% | 23.3% | 8.5% | 22.40*** | 9.2% | 22.6% | 8.4% | 26.08*** |
| Experienced physical assault | 18.7% | 34.7% | 17.6% | 17.21*** | 12.0% | 29.1% | 10.9% | 34.20*** |
| Experienced forced sex | 11.2% | 19.1% | 10.6% | 6.46* | 12.5% | 28.9% | 11.4% | 30.16*** |
| Perpetrated physical assault | 11.5% | 21.1% | 10.8% | 9.17** | 13.3% | 22.4% | 12.6% | 9.03** |
| Perpetrated forced sex | 5.7% | 15.8% | 5.0% | 19.30*** | 10.7% | 21.4% | 10.0% | 14.69*** |
p<.05,
p<.01,
p<.001
3.3 Associations between meth use and sexual risk
Most participants (83.7%) were sexually active in the past 4 months, with no difference between meth users and non users (85.7% vs. 83.6%, respectively; χ2(1)=0.67, p=.41). Table 3 describes the prevalence of SRBs. Among women and men, meth users were more likely than non users to report multiple partners, sex trade (both selling and buying), and sexually transmitted infection. Among women, meth users were also more likely to report unprotected sex. The prevalence of sex trading was strikingly high among meth users (54.6% for men, 45.4% for women). MSM were more likely than other men to have sold (20.0% vs. 7.3%) and bought (15.1% vs. 8.8%) sex (both p<.01). When excluding MSM, meth use remained strongly associated with both behaviors (both p<.01). Women were more likely than men to have been tested for HIV (77.7% vs. 62.9%; χ2(1)=83.90, p<.001), but there were no differences by race/ethnicity or meth use. Among men who had been tested, meth users were more likely than non users to report HIV-positive status. Among women, meth use was unrelated to HIV-positive status. Considering meth users only, there were no differences between those who also used other drugs and those who did not on any SRBs (all p>.05).
Table 3.
Associations between meth use and HIV sexual risk in the past 4 months (n=3,328)
| WOMEN | MEN | |||||||
|---|---|---|---|---|---|---|---|---|
| Total n=1,455 | Meth n=95 | No meth n=1,360 | AOR (95% CI)1 | Total n=1,873 | Meth n=117 | No meth n=1,756 | AOR (95% CI)1 | |
| MSM behavior | -- | -- | -- | 11.8% | 18.3% | 11.4% | 1.65 (0.99 – 2.75) | |
| Multiple partners | 19.5% | 28.4% | 18.9% | 2.42** (1.46 – 4.01) | 44.6% | 56.4% | 44.2% | 1.79** (1.18 – 2.71) |
| Unprotected sex | 44.2% | 66.3% | 42.6% | 2.45** (1.56 – 3.84) | 48.8% | 60.0% | 48.0% | 1.45 (0.98 – 2.17) |
| “Sold” sex | 5.1% | 16.8% | 4.2% | 6.34** (3.26 – 12.35) | 9.5% | 31.6% | 8.1% | 4.64*** (2.96 – 7.27) |
| “Bought” sex | 2.6% | 6.3% | 2.4% | 3.45** (1.31 – 9.06) | 10.0% | 28.2% | 8.7% | 4.80*** (3.03 – 7.61) |
| Sexually transmitted infection | 4.8% | 11.6% | 4.4% | 3.84*** (1.84 – 8.02) | 6.7% | 15.55% | 5.9% | 2.95*** (1.66 – 5.26) |
| HIV-positive | 8.3% | 8.6% | 8.2% | 1.46 (0.59 – 3.59) | 6.6% | 15.2% | 6.1% | 3.93 (1.83 – 8.45)*** |
Bivariate logistic regression models controlling for age, race/ethnicity, and education.
p<.05,
p<.01,
p<.001
3.4 Meth use as a mediator of the relationship between CSA and SRBs
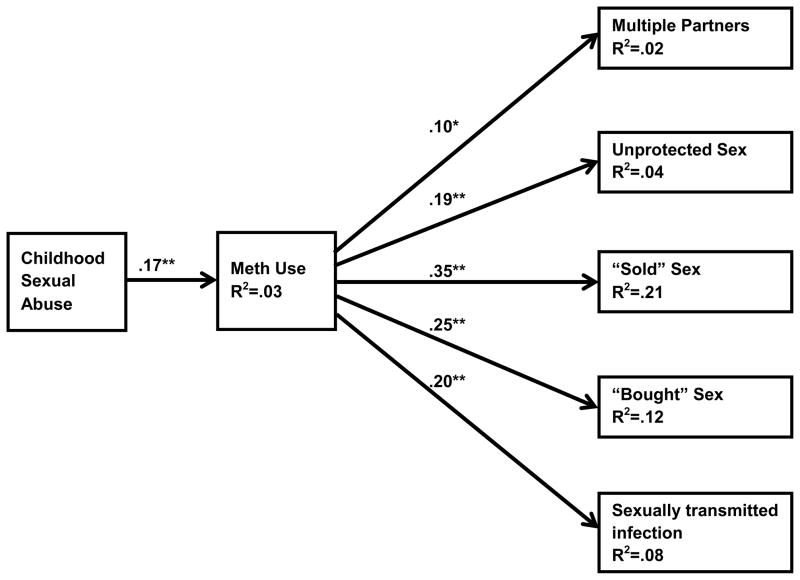
Participants who experienced CSA were more likely than those who had not to report multiple partners (45.6% vs. 32.3%; χ2(1)=21.34), unprotected sex (58.5% vs. 45.6%; χ2(1)=18.23), selling sex (29.9% vs. 5.3%; χ2(1)=239.95), buying sex (21.9% vs. 5.2%; χ2(1)=124.04), and sexually transmitted infection (χ2(1)=17.2% vs. 4.6%; χ2(1)=79.16) (all p<.001). Figure 1 depicts our mediation model. CSA was significantly related to meth use and meth use was significantly related to each SRB, supporting our mediation hypotheses. Direct paths from CSA to each SRB were allowed and remained significant, but were attenuated when meth was included as a mediator. This suggests that meth use partially mediated the effects of CSA on SRBs. Because we allowed all direct and indirect paths from CSA to SRBs, and correlations among SRBs, the model was exactly identified; hence, no fit statistics are provided. This model explained a significant proportion of variability in all outcomes: multiple partners (R2=.02), unprotected sex (R2=.04), buying sex (R2=.21), selling sex (R2=.12), and sexually transmitted infection (R2=.08). Multiple group analyses showed no significant differences between men and women on any of the five mediated paths. Finally, we ran a model in which race/ethnicity, age, and education were added as predictors of meth use and all SRBs. When controlling for these covariates, mediated relations between CSA and SRBs remained significant.
Figure 1.
Structural equation model depicting mediated effects of childhood sexual abuse on current sexual risk through meth use
Note. Exactly identified model; no fit statistics provided. Standardized path estimates shown. ** p<.001, * p<.05.
4. DISCUSSION
This study examined the relationship between meth use and SRBs among >3,000 patrons of alcohol-serving venues in a racially diverse township in the Western Cape. Within this sample of heavy alcohol drinkers (>90% screened positive for hazardous drinking), 6.4% reported current meth use. Meth users were more likely than non users to experience interpersonal violence, including history of CSA and current intimate partner violence, and to engage in SRBs. Our model provides evidence that meth use is a significant partial mediator of the relation between CSA and SRB, though it does not completely explain it. Meth users and non users were equally likely to report hazardous drinking, suggesting that meth use poses an additional HIV risk above and beyond the effects of alcohol abuse. However, meth users were much more likely to use other drugs, including injection drugs, which may contribute to HIV risk. Our results point to the urgent need for targeted HIV prevention services for meth users in this community, and the potential to reach meth users in alcohol-serving venues.
Meth use was more common among Coloured than Black participants, with >10% of Coloured men and women reporting meth use in the past 4 months. This is consistent with reports from other communities (Pluddemann et al., 2008a; Simbayi et al., 2006; Wechsberg et al., 2010; Wechsberg et al., 2008) and treatment centers (Pluddemann et al., 2008b) in the Western Cape. In Cape Town, meth was initially used by gangs in the Coloured communities, though it is spreading to the wider community (Kapp, 2008; Wechsberg et al., 2010). While the HIV prevalence is lower among Coloured than Black persons (Shisana et al., 2005), the higher prevalence of meth use among Coloured persons could fuel the spread of HIV.
While meth use was less common among Black participants, Black meth users tended to use it more frequently and in combination with other drugs, suggesting that they may represent a high-risk sub-group. Of particular concern, over half of Black meth users had injected drugs in the past 4 months. Unfortunately, we did not assess the types of drugs injected, injection risk practices, or availability of sterile syringes. Ethnographic research suggests that heroin is the most commonly injected drug in South Africa (Parry et al., 2008), but it is possible that our participants were injecting meth, either independently or in combination with other drugs. In other settings, the switch from smoking to injecting meth has been precipitated by the development of dependence (Chamla et al., 2006; Darke et al., 1994; Neaigus et al., 2001). Many injection drug users in this region engage in risky injecting practices, including sharing and re-using needles, thus introducing further HIV risk (Parry et al., 2008).
In the United States and other regions, meth use is particularly common among MSM (CDC, 2007; Couture et al., 2011; Liao et al., 2011; Melbye et al., 2002; Shoptaw and Reback, 2007; Stall et al., 2001) and is associated with SRBs among MSM (Bolding et al., 2006; Koblin et al., 2006; Shoptaw and Reback, 2007). We found a similar pattern in our sample, with MSM reporting the highest prevalence of meth use. There is some evidence from South Africa to suggest that drug use during sex is common among MSM (Parry et al., 2008), but additional research is needed to better understand the relation between meth and SRB among MSM.
The Western Cape has opened several facilities that specialize in the treatment of amphetamine-related disorders (Bateman, 2006). Nevertheless, many meth users do not seek treatment, largely due to inequitable access, competing financial pressures, and lack of awareness of available resources (Myers et al., 2010). Meth carries a high risk for dependence (Darke et al., 2008), and data from South African townships suggest that meth is a serious problem, contributing to school dropout, crime, and violence (Kapp, 2008; Pluddemann et al., 2010a; Simbayi et al., 2006). Improved access to substance abuse treatment, an important component of HIV prevention (Metzger et al., 2010), is sorely needed in this setting.
Consistent with research from other regions, meth users in our sample were more likely than non users to engage in SRBs, including multiple partners, unprotected sex, and sex trade. Meth has direct effects on sexual desire that may contribute to increased risk taking (Volkow et al., 2007). While intoxicated, judgment is impaired, and individuals are more likely to have unprotected sex with risky partners (Purdie et al., 2011; Schacht et al., 2010; Stoner et al., 2008). The high prevalence of sex trade among meth users is of particular concern – 55% of men and 45% of women reported either buying or selling sex in exchange for money, alcohol/drugs, or a place to stay in the past 4 months. In the context of poverty and high unemployment, sex trade may be a means of acquiring meth (Floyd et al., 2010; Semple et al., 2010; Shannon et al., 2008). Given the higher prevalence of SRBs among meth users, it is not surprising that meth users were more likely than non users to have a recent sexually transmitted infection. Among men, meth use was also associated with HIV-positive status. As our study was limited by self-report, future research would benefit from biological testing of HIV and other sexually transmitted infections among meth users in this setting.
Our data suggests that, among both men and women, meth users are more likely to experience interpersonal violence. In this sample, nearly one quarter of meth users had a history of CSA, and nearly half were currently involved in intimate partner violence. Childhood abuse, and CSA in particular, is predictive of adult substance abuse (Arreola et al., 2008; MacMillan et al., 2001; Simpson and Miller, 2002; Wilsnack et al., 1997), often serving as a maladaptive coping strategy for emotional distress and relationship problems (Edwards et al., 2003; Molnar et al., 2001). Survivors of childhood abuse are at increased risk for being revictimized later in life (Arriola et al., 2005; Classen et al., 2005; Coid et al., 2001), and substance abuse may make individuals more vulnerable to both experiencing and perpetrating intimate partner violence due to its intoxicating effects and the high-risk settings in which it often occurs (Chermack et al., 2010; Chuang et al., 2007; Kaysen et al., 2010; McCauley et al., 2010; Parrott et al., 2003; Taft et al., 2010). Interpersonal violence has implications for HIV risk, as individuals with CSA are more likely to engage in SRBs and have sexually transmitted infections (Lenderking et al., 1997; Mimiaga et al., 2009; Mosack et al., 2010; Schraufnagel et al., 2010; Senn et al., 2006). Our results suggest that meth use may partially mediate the relation between CSA and HIV sexual risk. This finding is consistent with previous research (Brennan et al., 2007; Greenberg, 2001; Mimiaga et al., 2009; Senn et al., 2008), but our study is the first to examine this relationship in a community-based sample in South Africa. Qualitative and prospective studies are needed to clarify the relation between meth use and interpersonal violence and to explore its interactive effect on HIV risk. While CSA may put individuals at increased risk for meth use later in life, substance abuse and interpersonal violence likely have bidirectional and cyclical effects on each other (e.g., sex trading could lead to meth use and sexual assault) (Boles and Miotto, 2003; Kilpatrick et al., 1997; Swartout and White, 2010). However, the cross-sectional design of our study precludes any inferences regarding causality.
Our study has several noteworthy strengths, including a large, racially diverse sample of men and women recruited from 12 alcohol-serving venues over 1 year, and the inclusion of a high-risk comparison group of non meth users. However, results must be interpreted in light of the following limitations. First, the study was conducted in alcohol-serving venues. Previous research suggests that meth users are more likely to drink alcohol, but our sample may nevertheless represent a higher functioning and less addicted sub-set. Our qualitative work suggests that meth use is highly stigmatized, and that venue owners attempt to keep meth users out of their establishments. Second, our study relied on self-report. Despite our efforts to maintain privacy, the surveys were completed in a public place, which may have resulted in under-reporting of sensitive and stigmatized experiences, including meth use, interpersonal violence, and SRBs. In addition, a small minority completed the survey via interview, further increasing the possibility of under-reporting. However, we do not expect that response bias would undermine the strength of our findings. Third, the AUDIT does not provide gender-specific guidelines for defining hazardous drinking. As expected, given that our sample was recruited from alcohol-serving venues, nearly all met criteria for hazardous drinking using this highly sensitive screener. Finally, due to the cross-sectional design and setting in which it was conducted, our measures were necessarily brief.
In conclusion, there is an urgent need to provide targeted HIV prevention and substance abuse treatment to meth users living in townships in the Western Cape of South Africa. Our results suggest that meth use occurs in the context of violent relationships and contributes to SRBs that are associated with HIV infection and transmission. Integrated intervention strategies that aim to reduce both substance use and SRBs, while addressing the interpersonal context in which these behaviors occur, offer promise (Wechsberg et al, 2008; 2010). Our study has shown that alcohol-serving venues may be one setting in which to reach meth users for HIV prevention intervention. Given the rapid increase in meth use in South Africa over the past decade, providing access to effective substance abuse treatment and risk reduction intervention is critical to curbing the further spread of HIV in these communities.
Acknowledgments
Role of Funding Source
This project was supported by grants from the National Institute of Alcohol Abuse and Alcoholism (R01 AA018074) and the National Institute on Drug Abuse (K23 DA028660). The NIH had no further role in study design, data collection, analysis and interpretation of data, writing the report, or in the decision to submit the paper for publication.
We are grateful to all the men and women who participated in this study. We would like to acknowledge the South African research team that collected the data, specifically Simphiwe Dekeda, Albert Africa, Judia Adams, Bulelwa Nyamza and Jabulile Mantantana. We appreciate the support of Annemie Stewart and Lisa Eaton in management of the data.
Footnotes
Conflict of Interest
All authors declare that they have no conflicts of interest
Contributors
Kalichman, Sikkema, and Skinner designed the original project and secured grant funding; Meade and Watt conceptualized the current study and conducted most of the analyses; Ranby conducted additional analyses; Meade wrote the first draft of the manuscript; Deng conducted relevant literature searches; Pieterse provided oversight and conducted data collection; and all authors contributed to and have approved the final manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Arreola S, Neilands T, Pollack L, Paul J, Catania J. Childhood sexual experiences and adult health sequelae among gay and bisexual men: defining childhood sexual abuse. J Sex Res. 2008;45:246–252. doi: 10.1080/00224490802204431. [DOI] [PubMed] [Google Scholar]
- Arriola KRJ, Louden T, Doldren MA, Fortenberry RM. A meta-analysis of the relationship of child sexual abuse to HIV risk behavior among women. Child Abuse Negl. 2005;29:725–746. doi: 10.1016/j.chiabu.2004.10.014. [DOI] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. WHO Department of Mental Health and Substance Dependence; Geneva: 2001. [Google Scholar]
- Bateman C. ‘Tik’ causing a health crisis. S Afr Med J. 2006;96:672–674. [PubMed] [Google Scholar]
- Bolding G, Hart G, Sherr L, Elford J. Use of crystal methamphetamine among gay men in London. Addiction. 2006;101:1622–1630. doi: 10.1111/j.1360-0443.2006.01571.x. [DOI] [PubMed] [Google Scholar]
- Boles SM, Miotto K. Substance abuse and violence: a review of the literature. Aggression Violent Behav. 2003;8:155–174. [Google Scholar]
- Brennan DJ, Hellerstedt WL, Ross MW, Welles SL. History of childhood sexual abuse and HIV risk behaviors in homosexual and bisexual men. Am J Public Health. 2007;97:1107–1112. doi: 10.2105/AJPH.2005.071423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. Methamphetamine Use and Risk for HIV/AIDS. US Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta: 2007. [Google Scholar]
- Chamla D, Chamla JH, Dabin W, Delin H, Rennes N. Transition to injection and sharing of needles/syringes: potential for HIV transmission among heroin users in Chengdu, China. Addict Behav. 2006;31:697–701. doi: 10.1016/j.addbeh.2005.05.048. [DOI] [PubMed] [Google Scholar]
- Chermack ST, Grogan-Kaylor A, Perron BE, Murray RL, De Chavez P, Walton MA. Violence among men and women in substance use disorder treatment: a multi-level event-based analysis. Drug Alcohol Depend. 2010;112:194–200. doi: 10.1016/j.drugalcdep.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang CH, Liebschutz JM, Cheng DM, Raj A, Samet JH. Substance use during sexual and physical assault in HIV-infected persons. Violence Vict. 2007;22:216–225. doi: 10.1891/088667007780477311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Classen CC, Palesh OG, Aggarwal R. Sexual revictimization: a review of the empirical literature. Trauma Violence Abuse. 2005;6:103–129. doi: 10.1177/1524838005275087. [DOI] [PubMed] [Google Scholar]
- Cohen JB, Dickow A, Horner K, Zweben JE, Balabis J, Vandersloot D, Reiber C. Abuse and violence history of men and women in treatment for methamphetamine dependence. Am J Addict. 2003;12:377–385. [PubMed] [Google Scholar]
- Coid J, Petruckevitch A, Feder G, Chung WS, Richardson J, Moorey S. Relation between childhood sexual and physical abuse and risk of revictimisation in women: a cross-sectional survey. Lancet. 2001;358:450–454. doi: 10.1016/s0140-6736(01)05622-7. [DOI] [PubMed] [Google Scholar]
- Colfax G, Vittinghoff E, Husnik MJ, McKirnan D, Buchbinder S, Koblin B, Celum C, Chesney M, Huang Y, Mayer K, Bozeman S, Judson FN, Bryant KJ, Coates TJ. Substance use and sexual risk: a participant- and episode-level analysis among a cohort of men who have sex with men. Am J Epidemiol. 2004;159:1002–1012. doi: 10.1093/aje/kwh135. [DOI] [PubMed] [Google Scholar]
- Corsi KF, Booth RE. HIV sex risk behaviors among heterosexual methamphetamine users: literature review from 2000 to present. Curr Drug Abuse Rev. 2008;1:292–296. doi: 10.2174/1874473710801030292. [DOI] [PubMed] [Google Scholar]
- Couture MC, Sansothy N, Sapphon V, Phal S, Sichan K, Stein E, Evans J, Maher L, Kaldor J, Vun MC, Page K. Young women engaged in sex work in Phnom Penh, Cambodia, have high incidence of HIV and sexually transmitted infections, and amphetamine-type stimulant use: new challenges to HIV prevention and risk. Sex Transm Dis. 2011;38:33–39. doi: 10.1097/OLQ.0b013e3182000e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darke S, Kaye S, McKetin R, Duflou J. Major physical and psychological harms of methamphetamine use. Drug Alcohol Rev. 2008;27:253–262. doi: 10.1080/09595230801923702. [DOI] [PubMed] [Google Scholar]
- Darke S, Ross J, Cohen J. The use of benzodiazepines among regular amphetamine users. Addiction. 1994;89:1683–1690. doi: 10.1111/j.1360-0443.1994.tb03769.x. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Bradley M, Mauro G, Samiran P, Benjamin P, Steffanie AS, Mark T, Lucas W, Alex W, John H. Meth/amphetamine use and associated HIV: implications for global policy and public health. Int J Drug Policy. 2010;21:347–358. doi: 10.1016/j.drugpo.2009.11.007. [DOI] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics. 2003;111:564–572. doi: 10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- Dunkle KL, Jewkes RK, Nduna M, Levin J, Jama N, Khuzwayo N, Koss MP, Duvvury N. Perpetration of partner violence and HIV risk behaviour among young men in the rural Eastern Cape, South Africa. AIDS. 2006;20:2107–2114. doi: 10.1097/01.aids.0000247582.00826.52. [DOI] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: results from the adverse childhood experiences study. Am J Psychiatry. 2003;160:1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- Floyd LJ, Hedden S, Lawson A, Salama C, Moleko AG, Latimer W. The association between poly-substance use, coping, and sex trade among black South African substance users. Subst Use Misuse. 2010;45:1971–1987. doi: 10.3109/10826081003767635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg J. Childhood sexual abuse and sexually transmitted diseases in adults: a review of and implications for STD/HIV programmes. Int J STD AIDS. 2001;12:777–783. doi: 10.1258/0956462011924380. [DOI] [PubMed] [Google Scholar]
- Jewkes R. Associations between childhood adversity and depression, substance abuse and HIV and HSV2 incident infections in rural South African youth. Child Abuse Negl. 2010;34:833–841. doi: 10.1016/j.chiabu.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes R, Abrahams N. The epidemiology of rape and sexual coercion in South Africa: an overview. Soc Sci Med. 2002;55:1231–1244. doi: 10.1016/s0277-9536(01)00242-8. [DOI] [PubMed] [Google Scholar]
- Kaminer D, Grimsrud A, Myer L, Stein DJ, Williams DR. Risk for post-traumatic stress disorder associated with different forms of interpersonal violence in South Africa. Soc Sci Med. 2008;67:1589–1595. doi: 10.1016/j.socscimed.2008.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan ML, Asnis GM, Lipschitz DS, Chorney P. Suicidal behavior and abuse in psychiatric outpatients. Compr Psychiat. 1995;36:229–235. doi: 10.1016/0010-440x(95)90087-c. [DOI] [PubMed] [Google Scholar]
- Kapp C. Crystal meth boom adds to South Africa’s health challenges. Lancet. 2008;37:193–194. doi: 10.1016/s0140-6736(08)60120-8. [DOI] [PubMed] [Google Scholar]
- Kaysen DL, Lindgren KP, Lee CM, Lewis MA, Fossos N, Atkins DC. Alcohol-involved assault and the course of PTSD in female crime victims. J Trauma Stress. 2010;23:523–527. doi: 10.1002/jts.20542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Resnick HS, Saunders BE, Best CL. A 2-year longitudinal analysis of the relationships between violent assault and substance use in women. J Consult Clin Psychol. 1997;65:834–847. doi: 10.1037//0022-006x.65.5.834. [DOI] [PubMed] [Google Scholar]
- Koblin BA, Husnik MJ, Colfax G, Huang Y, Madison M, Mayer K, Barresi PJ, Coates TJ, Chesney MA, Buchbinder S. Risk factors for HIV infection among men who have sex with men. AIDS. 2006;20:731–739. doi: 10.1097/01.aids.0000216374.61442.55. [DOI] [PubMed] [Google Scholar]
- Lenderking WR, Wold C, Mayer KH, Goldstein R, Losina E, Seage GR. Childhood sexual abuse among homosexual men: prevalence and association with unsafe sex. J Gen Intern Med. 1997;12:250–253. doi: 10.1046/j.1525-1497.1997.012004250.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao M, Jiang Z, Zhang X, Kang D, Bi Z, Liu X, Fu J, Zhang N, Mao W, Jiang B, Jia Y. Syphilis and methamphetamine use among female sex workers in Shandong Province, China. Sex Transm Dis. 2011;38:57–62. doi: 10.1097/OLQ.0b013e3181ebb475. [DOI] [PubMed] [Google Scholar]
- MacMillan HL, Fleming JE, Streiner DL, Lin E, Boyle MH, Jamieson E, Duku EK, Walsh CA, Wong MY, Beardslee WR. Childhood abuse and lifetime psychopathology in a community sample. Am J Psychiatry. 2001;158:1878–1883. doi: 10.1176/appi.ajp.158.11.1878. [DOI] [PubMed] [Google Scholar]
- McCauley JL, Calhoun KS, Gidycz CA. Binge drinking and rape: a prospective examination of college women with a history of previous sexual victimization. J Interpers Violence. 2010;25:1655–1668. doi: 10.1177/0886260509354580. [DOI] [PubMed] [Google Scholar]
- Melbye K, Khamboonruang C, Kunawararak P, Celentano DD, Prapamontol T, Nelson KE, Natpratan C, Beyrer C. Lifetime correlates associated with amphetamine use among northern Thai men attending STD and HIV anonymous test sites. Drug Alcohol Depend. 2002;68:245–253. doi: 10.1016/s0376-8716(02)00218-1. [DOI] [PubMed] [Google Scholar]
- Metzger DS, Woody GE, O’Brien CP. Drug treatment as HIV prevention: a research update. J Acquir Immune Defic Syndr. 2010;55:S32–S36. doi: 10.1097/QAI.0b013e3181f9c10b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mimiaga MJ, Noonan E, Donnell D, Safren SA, Koenen KC, Gortmaker S, O’Cleirigh C, Chesney MA, Coates TJ, Koblin BA, Mayer KH. Childhood sexual abuse is highly associated with HIV risk-taking behavior and infection among MSM in the EXPLORE Study. J Acquir Immune Defic Syndr. 2009;51:340–348. doi: 10.1097/QAI.0b013e3181a24b38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molnar BE, Buka SL, Kessler RC. Child sexual abuse and subsequent psychopathology: results from the National Comorbidity Survey. Am J Public Health. 2001;91:753–760. doi: 10.2105/ajph.91.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris K, Parry C. South African methamphetamine boom could fuel further HIV. Lancet Infect Dis. 2006;6:471. doi: 10.1016/s1473-3099(06)70539-4. [DOI] [PubMed] [Google Scholar]
- Mosack KE, Randolph ME, Dickson-Gomez J, Abbott M, Smith E, Weeks MR. Sexual risk-taking among high-risk urban women with and without histories of childhood sexual abuse: mediating effects of contextual factors. J Child Sex Abuse. 2010;19:43–61. doi: 10.1080/10538710903485591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers BJ, Louw J, Pasche SC. Inequitable access to substance abuse treatment services in Cape Town, South Africa. Subst Abuse Treat Prev Policy. 2010;5:28–39. doi: 10.1186/1747-597X-5-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neaigus A, Miller M, Friedman SR, Des Jarlais DC. Sexual transmission risk among noninjecting heroin users infected with human immunodeficiency virus or hepatitis C virus. J Infect Dis. 2001;184:359–363. doi: 10.1086/322020. [DOI] [PubMed] [Google Scholar]
- Parrott DJ, Drobes DJ, Saladin ME, Coffey SF, Dansky BS. Perpetration of partner violence: effects of cocaine and alcohol dependence and posttraumatic stress disorder. Addict Behav. 2003;28:1587–1602. doi: 10.1016/j.addbeh.2003.08.036. [DOI] [PubMed] [Google Scholar]
- Parry CD, Petersen P, Carney T, Dewing S, Needle R. Rapid assessment of drug use and sexual HIV risk patterns among vulnerable drug using populations in Cape Town, Durban, and Pretoria, South Africa. Sahara J. 2008;5:113–119. doi: 10.1080/17290376.2008.9724909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pluddemann A, Flisher AJ, Mathews C, Carney T, Lombard C. Adolescent methamphetamine use and sexual risk behaviour in secondary school students in Cape Town, South Africa. Drug Alcohol Rev. 2008a;27:687–692. doi: 10.1080/09595230802245253. [DOI] [PubMed] [Google Scholar]
- Pluddemann A, Flisher AJ, McKetin R, Parry CD, Lombard CJ. A prospective study of methamphetamine use as a predictor of high school non-attendance in Cape Town, South Africa. Subst Abuse Treat Prev Policy. 2010a;5:25. doi: 10.1186/1747-597X-5-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pluddemann A, Myers BJ, Parry CD. Surge in treatment admissions related to methamphetamine use in Cape Town, South Africa: implications for public health. Drug Alcohol Rev. 2008b;27:185–189. doi: 10.1080/09595230701829363. [DOI] [PubMed] [Google Scholar]
- Pluddemann A, Parry CD, Bhana A, Harker N, Potgieter H, Gerber W. Monitoring alcohol and drug abuse trends in South Africa (Phase 27) SACENDU Res Brief. 2010b;9:291–300. [Google Scholar]
- Purdie MP, Norris J, Davis KC, Zawacki T, Morrison DM, George WH, Kiekel PA. The effects of acute alcohol intoxication, partner risk level, and general intention to have unprotected sex on women’s sexual decision making with a new partner. Exp Clin Psychopharmacol. 2011;19:378–388. doi: 10.1037/a0024792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawyer-Kurian KM, Wechsberg W, Luseno W. Exploring the differences and similarities between Black/African and Coloured men regarding violence against women, substance abuse, and HIV risks in Cape Town, South Africa. Psychol Men Masculinity. 2009;10:13–29. [Google Scholar]
- Schacht R, George W, Davis K, Heiman J, Norris J, Stoner S, Kajumulo K. Sexual abuse history, alcohol intoxication, and women’s sexual risk behavior. Arch Sex Behav. 2010;39:898–906. doi: 10.1007/s10508-009-9544-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schraufnagel TJ, Davis KC, George WH, Norris J. Childhood sexual abuse in males and subsequent risky sexual behavior: a potential alcohol-use pathway. Child Abuse Negl. 2010;34:369–378. doi: 10.1016/j.chiabu.2009.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semple SJ, Strathdee SA, Zians J, Patterson TL. Social and behavioral characteristics of HIV-positive MSM who trade sex for methamphetamine. Am J Drug Alcohol Abuse. 2010;36:325–331. doi: 10.3109/00952990.2010.505273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senn TE, Carey MP, Vanable PA. Childhood and adolescent sexual abuse and subsequent sexual risk behavior: evidence from controlled studies, methodological critique, and suggestions for research. Clin Psychol Rev. 2008;28:711–735. doi: 10.1016/j.cpr.2007.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senn TE, Carey MP, Vanable PA, Coury-Doniger P, Urban MA. Childhood sexual abuse and sexual risk behavior among men and women attending sexually transmitted disease clinic. J Consult Clin Psychol. 2006;74:720–731. doi: 10.1037/0022-006X.74.4.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shannon K, Kerr T, Bright V, Gibson K, Tyndall MW. Drug sharing with clients as a risk marker for increased violence and sexual and drug-related harms among survival sex workers. AIDS Care. 2008;20:228–234. doi: 10.1080/09540120701561270. [DOI] [PubMed] [Google Scholar]
- Shisana O, Rehle T, Simbayi L, Parker W, Zuma K, Bhana A, Connolly C, Jooste S, Pillay V. South African National HIV Prevalence, HIV Incidence, Behaviour and Communication Survey, 2005. HSRC Press; Cape Town: 2005. [Google Scholar]
- Shoptaw S, Reback CJ. Methamphetamine use and infectious disease-related behaviors in men who have sex with men: implications for interventions. Addiction. 2007;102:130–135. doi: 10.1111/j.1360-0443.2006.01775.x. [DOI] [PubMed] [Google Scholar]
- Simbayi L, Kalichman S, Cain D, Cherry C, Henda N, Cloete A. Methamphetamine use and sexual risks for HIV infection in Cape Town, South Africa. J Subst Use. 2006;11:291–300. [Google Scholar]
- Simpson TL, Miller WR. Concomitance between childhood sexual and physical abuse and substance use problems: a review. Clin Psychol Rev. 2002;22:27–77. doi: 10.1016/s0272-7358(00)00088-x. [DOI] [PubMed] [Google Scholar]
- Sommers I, Baskin D, Baskin-Sommers A. Methamphetamine use among young adults: health and social consequences. Addict Behav. 2006;31:1469–1476. doi: 10.1016/j.addbeh.2005.10.004. [DOI] [PubMed] [Google Scholar]
- SSA. Mid-year Population Estimates. Statistics South Africa; Pretoria: 2010. [Google Scholar]
- Stall R, Paul JP, Greenwood G, Pollack LM, Bein E, Crosby GM, Mills TC, Binson D, Coates TJ, Catania JA. Alcohol use, drug use and alcohol-related problems among men who have sex with men: the Urban Men’s Health Study. Addiction. 2001;96:1589–1601. doi: 10.1046/j.1360-0443.2001.961115896.x. [DOI] [PubMed] [Google Scholar]
- Stoner SA, Norris J, George WH, Morrison DM, Zawacki T, Davis KC, Hessler DM. Women’s condom use assertiveness and sexual risk-taking: effects of alcohol intoxication and adult victimization. Addict Behav. 2008;33:1167–1176. doi: 10.1016/j.addbeh.2008.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised Conflict Tactics Scales (CTS2) - development and preliminary psychometric data. J Family Issues. 1996;17:283–316. [Google Scholar]
- Swartout KM, White JW. The relationship between drug use and sexual aggression in men across time. J Interpers Violence. 2010;25:1716–1735. doi: 10.1177/0886260509354586. [DOI] [PubMed] [Google Scholar]
- Taft CT, O’Farrell TJ, Doron-LaMarca S, Panuzio J, Suvak MK, Gagnon DR, Murphy CM. Longitudinal risk factors for intimate partner violence among men in treatment for alcohol use disorders. J Consult Clin Psychol. 2010;78:924–935. doi: 10.1037/a0021093. [DOI] [PubMed] [Google Scholar]
- UNAIDS. Report on the Global HIV/AIDS Epidemic. World Health Organization; Geneva: 2008. [Google Scholar]
- UNODC. World Drug Report 2009. United Nations; Vienna: 2009. [Google Scholar]
- Volkow ND, Wang GJ, Fowler JS, Telang F, Jayne M, Wong C. Stimulant-induced enhanced sexual desire as a potential contributing factor in HIV transmission. Am J Psychiatry. 2007;164:157–160. doi: 10.1176/ajp.2007.164.1.157. [DOI] [PubMed] [Google Scholar]
- Wechsberg WM, Jones HE, Zule WA, Myers BJ, Browne FA, Kaufman MR, Luseno W, Flisher AJ, Parry CDH. Methamphetamine (tik) use and its association with condom use among out-of-school females in Cape Town, South Africa. Am J Drug Alcohol Abuse. 2010;36:208–213. doi: 10.3109/00952990.2010.493592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM, Luseno WK, Karg RS, Young S, Rodman N, Myers B, Parry CD. Alcohol, cannabis, and methamphetamine use and other risk behaviours among Black and Coloured South African women: a small randomized trial in the Western Cape. Int J Drug Policy. 2008;19:130–139. doi: 10.1016/j.drugpo.2007.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams SL, Williams DR, Stein DJ, Seedat S, Jackson PB, Moomal H. Multiple traumatic events and psychological distress: the South Africa stress and health study. J Trauma Stress. 2007;20:845–855. doi: 10.1002/jts.20252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilsnack SC, Vogeltanz ND, Klassen AD, Harris TR. Childhood sexual abuse and women’s substance abuse: national survey findings. J Stud Alcohol. 1997;58:264–271. doi: 10.15288/jsa.1997.58.264. [DOI] [PubMed] [Google Scholar]
- Woody GE, VanEtten-Lee ML, McKirnan D, Donnell D, Metzger D, Seage G, 3rd, Gross M. Substance use among men who have sex with men: comparison with a national household survey. JAIDS. 2001;27:86–90. doi: 10.1097/00126334-200105010-00015. [DOI] [PubMed] [Google Scholar]