Abstract
This pilot study tested the feasibility of Family-Based Hip-Hop to Health, a school-based obesity prevention intervention for 3–5 year old Latino children and their parents, and estimated its effectiveness in producing smaller average changes in body mass index at one year follow-up.
Four Head Start preschools administered through the Chicago Public Schools were randomly assigned to receive a Family-Based Intervention (FBI) or a General Health intervention (GHI). Parents signed consent forms for 147 of the 157 children enrolled.
Both the school-based and family-based components of the intervention were feasible, but attendance for the parent intervention sessions was low. Contrary to expectations, a downtrend in BMI Z score was observed in both the intervention and control groups.
While the data reflect a downward trend in obesity among these young Hispanic children, obesity rates remained higher at one-year follow-up (15%) than those reported by the National Health and Nutrition Examination Survey (2009–2010) for 2–5 year old children (12.1%). Developing evidence-based strategies for obesity prevention among Hispanic families remains a challenge.
Keywords: childhood obesity, minorities, parents, diet, physical activity
INTRODUCTION
Obesity, which is epidemic in the US, is associated with increased risk for numerous medical problems. (1) Many obesity-related risk factors and diseases are strikingly common in minority populations. (2–5) Prevalence of overweight is particularly high among Hispanic preschool children. (6) Specifically, among children two to five years of age, 23.8% of non-Hispanic whites, 28.9% of non-Hispanic Blacks, and 33.1% of Hispanic children are overweight. (7) The projected growth of the Hispanic population (expected to comprise 30% of the US population by 2050), (8) coupled with the high prevalence of obesity necessitate the development of early interventions to alter excessive weight gain trajectory among Hispanic children.
This article reports the results of a pilot study of an obesity prevention intervention for Hispanic preschool children that built upon the findings of “Hip-Hop to Health Jr.” a successful preschool- based intervention. (6) The primary aim of Hip-Hop to Health Jr. was to compare changes in body mass index (BMI, kg/m2) in two groups of three to five year old low-income minority children randomized to a Weight Control Intervention (WCI) or a General Health Intervention (GHI). At 12- and 24-month follow-up, children from predominantly black preschools who participated in the WCI had significantly smaller relative changes in BMI compared to children in the GHI control group. (6) However, children attending predominantly Latino preschools did not derive similar benefit from the WCI. (9) Like many other school-based childhood obesity prevention interventions, our original Hip-Hop to Health intervention did not include or evaluate a well-defined parental component. (6) Since it is well documented that the family environment is crucial for shaping children’s eating and physical activity patterns (10) and that parental involvement in weight loss treatment has proven effective, (11) we sought to add a family-targeted component to the preschool-based Hip-Hop to Health intervention.
METHODS AND PROCEDURES
Design and Setting
The Family-Based Hip-Hop to Health study compared a Family-Based Intervention (FBI) (i.e., Hip-Hop to Health plus a targeted family component) with a General Health Intervention (GHI). Four early childhood education programs affiliated with the Chicago Public Schools (CPS) were randomly assigned to one of two conditions: 1) The FBI, which targeted reductions in dietary fat and television viewing, as well as increases in fruits, vegetables, and physical activity and which placed emphasis on the family environment and parenting skills; or 2) The GHI control intervention, which addressed health and safety topics not covered in the FBI (e.g., 911 training, immunization, dental health, and seat belt safety.)
The primary aim of Family-Based Hip-Hop to Health was to test the feasibility of a 14-week intervention designed for three to five year old Hispanic children and their parents. The secondary aims were: 1. to estimate the effectiveness of the FBI in producing smaller average changes in body mass index (BMI) appropriate for growth in these children at one year follow-up; and 2. to estimate the effectiveness of the FBI in producing changes in physical activity, screen time, fat intake, fiber intake, and fruit and vegetable intake in the children and their parents at post-intervention and Year 1 follow-up.
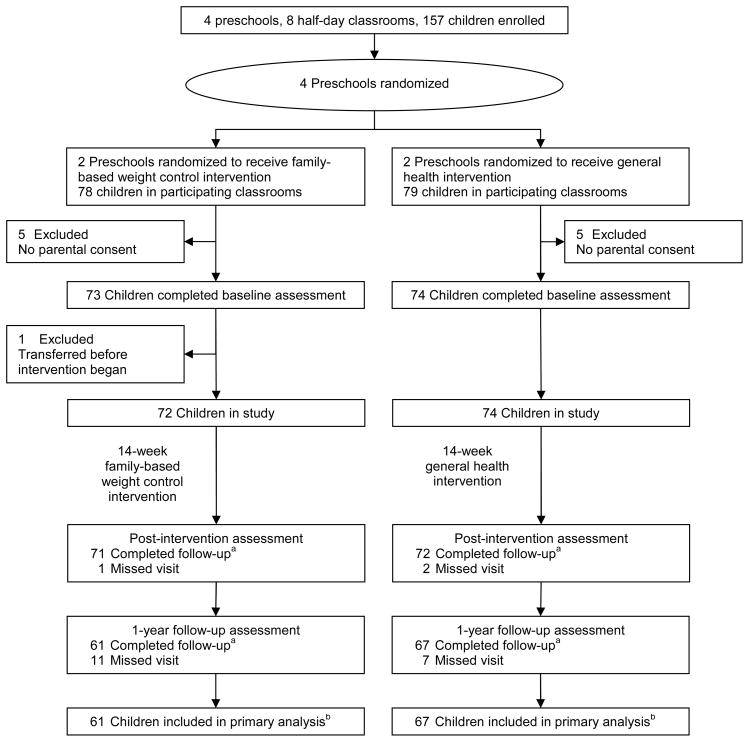
The Institutional Review Boards at the University of Illinois at Chicago and the Chicago Public Schools approved this study. The study design and participant flow are shown in Figure 1.
Figure 1.
Recruitment, enrollment, and retention, Family-Based Hip-Hop to Health
a Follow-up was considered complete if the child’s height and weight were measured.
b Only children with follow-up data were included in the primary analysis.
Eligibility
A parent-child dyad was eligible if the parent gave informed consent for herself and the child, the child’s height and weight were measured at baseline, and the child was still enrolled in a participating classroom when the intervention began. Since interventions were conducted during regular class time, all children in the participating classrooms received one of the interventions, but data were collected only from those with informed consent. Up to two children per family were eligible to participate.
Theoretical Framework
We developed Hip-Hop to Health and the parental component of the FBI in accordance with Social Cognitive Theory (SCT). (12) However, in recognition of the value of multiple theoretical approaches to intervention development, (13) we also incorporated relevant components of the Health Belief Model (HBM) (14) and self-determination theory, (15) though these were not formally tested in the study.
Interventions
Child Intervention
The curriculum developed for the children was conceptually similar to the original “Hip-Hop to Health” curriculum. However, after meeting with parents and other stakeholders, we felt that the continuity of delivery could be further strengthened. Therefore, we decided to develop a Spanish language CD to supplement the curriculum. The CD was used in each session to structure both the nutrition instruction and the physical activity session. The CD was also used in the parent sessions, and each family received a copy in order to reinforce the classroom material at home. The overall intervention was tailored to the cultural and developmental needs of the target population. The child component of the FBI included a 14-week (3 times weekly) intervention led by a bilingual/bicultural educator. Each session included 20 minutes of nutrition instruction and 20 minutes of aerobic activity. The nutrition instruction included activities led by puppets representing food groups. The nutrition and physical activity components were designed to target specific child behaviors to increase consumption of fruits, vegetables, and fiber; decrease fat intake; reduce television viewing; and increase the duration and level of daily physical activity. Children in the GHI control schools received a once weekly intervention for 14 weeks (20 minutes each week) that taught general health concepts such as dental health, seat belt safety, and calling 911.
Parent Intervention
The parent curriculum was developed following discussions with a variety of stakeholders and feedback groups with parents. We addressed their perceptions about the role of diet and exercise in weight management as well as their definition of a healthy weight for themselves and their child. Parents also participated in a 30 minute exercise session so we could understand their preferences regarding activity options. The parent component included classes and newsletters adapted for a lower-income, Hispanic population. Parents of children receiving the FBI were encouraged to attend six weekly 90-minute classes that included 60 minutes of interactive instruction on healthful eating and family exercise plus 30 minutes of moderate physical activity (e.g., salsa aerobics, walking group). Topics were based on input from Hispanic parents of similar acculturation and socioeconomic level as well as current research related to predictors of overweight in Hispanic children, (16) parent practices related to child overweight in Hispanic children, (16–17) and predictors of physical activity in Hispanic preschoolers. (18) The parent intervention also incorporated concepts related to the HBM and SCT, including instruction on risks associated with childhood obesity, health concerns associated with childhood obesity, the importance of modeling and reinforcing healthy eating and exercise patterns, and creating a home environment to facilitate healthy choices. Parents also received weekly newsletters containing culturally adapted information that paralleled the 14-week school-based component. Parents of children receiving the GHI received weekly newsletters that paralleled the 14-week GHI curriculum.
Measures
Trained bilingual, bicultural interviewers administered all questionnaires. Because of the study design, both parents and interviewers were aware of group assignments.
Sociodemographic Variables
Parents completed a sociodemographic questionnaire at baseline.
Acculturation
At baseline, parents who identified themselves as Hispanic/Latino completed a 4-item acculturation questionnaire. (19) The acculturation score was the mean of the 4 responses, ranging from 1 (least acculturated) to 5 (most acculturated). Parents also reported where they were born and how many years they had lived in the United States.
Anthropometric Variables
Children’s height and weight were measured at baseline, post-intervention, and 1-year follow-up. Parents’ height was measured at baseline, and weight was measured at baseline, post-intervention, and 1-year follow-up. Height was measured using a Seca 214 portable stadiometer (Seca, Hanover, MD). Weight was measured using a Tanita BWB-800 digital scale (Tanita Corporation of America, Inc., Arlington Heights, IL). Participants removed their shoes and any heavy outer clothing for the anthropometric measurements. BMI was computed from height and weight for children and parents, and BMI Z scores and BMI percentiles for age and sex were calculated for children using a SAS program developed by the CDC. [http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. Accessed 2/13/2012.]
Perception of Overweight
At all visits, parents were asked to classify their child’s weight as very underweight, underweight, average, overweight, or very overweight.
Physical Activity
Child and parent physical activity was measured at baseline and post-intervention using an ActiGraph GT1M activity monitor (ActiGraph, Pensacola, FL). Accelerometer data were not collected at 1-year follow-up due to resource limitations. The ActiGraph is a small, lightweight uniaxial accelerometer designed to detect normal body motion and filter out motion from other sources. The acceleration signal is sampled 30 times per second, and signals are summed at the end of a specified period (15 seconds for children, 1 minute for parents) and stored in non-volatile flash memory. Parents and children were asked to wear the ActiGraph on a belt around the waist during waking hours for seven days. Study staff called the parents each morning during the 7-day period to remind them about the accelerometers and to answer any questions or concerns.
Activity counts were downloaded from the accelerometers using ActiLife GT1M software (ActiGraph, Pensacola, FL), and the resulting text files were read and analyzed using SAS for Windows v 9.2 (SAS Institute Inc., Cary, NC). For each day in the record, the amount of time the accelerometer was actually worn was estimated. Time not worn was defined as at least 60 minutes with 0 activity counts, allowing for interruptions of up to 2 consecutive minutes with counts ≤ 100. (20) Only days with at least 8 hours of wear were included in the main analyses, and participants with fewer than 4 valid days were excluded.
To convert accelerometer counts into estimated activity levels for the children’s records, we used count thresholds from a calibration study conducted with preschool children: <38 counts/15 sec for sedentary behavior, 38–419 counts/15 sec for light activity, 420–841 counts/15 sec for moderate activity, and ≥ 842 counts/15 sec for vigorous activity. (21) For the parents’ records, we used the count thresholds from the 2003–2004 National Health and Nutritional Examination Survey (NHANES) analyses, which were derived from several calibration studies: <100 counts/min for sedentary, 100–2019 counts/min for light, 2020–5998 counts/min for moderate, and ≥5999 counts/min for vigorous activity. (22) Based on accelerometer data, we estimated the percentage of parents and children meeting national guidelines for physical activity at baseline and post-intervention. For children, the guidelines recommend 60 minutes per day of moderate to vigorous physical activity. (23) Since preschool children often engage in brief episodes of activity rather than sustained bouts, all time spent in MVPA was included in calculations. For adults, the guidelines recommend 150 minutes/week of moderate activity, 75 minutes/week of vigorous activity, or a combination of the two resulting from bouts of at least 10 minutes. A parent was considered to have met the recommendations if she engaged in 150 min/wk of MVPA in bouts at least 10 minutes long.
Television Viewing and Screen Time
At all visits, parents were asked to report the amount of time their child spent watching television (broadcast, cable, or satellite), watching DVDs or videotapes, playing video games, or using a computer on an average school day and on an average weekend day. (24) Parents were also asked how much time they spent in each of these activities on an average weekday and an average weekend day. Time spent watching television and total screen time in minutes/day were calculated using a weighted average of time spent on weekdays and weekend days. We also calculated the percentage of children meeting the American Academy of Pediatrics guidelines of ≤2 hr/day of total screen time. (25)
Dietary Intake
At each visit, parents completed a 24-hour dietary recall for the child and for their own consumption. Dietary intake for children was estimated from the dietary recall in combination with in-school observations.
Meal Observation at Preschool
Breakfast and lunch were served family-style in the preschool classrooms each day, and the children served themselves. Research staff unobtrusively documented the amount of food served to and consumed by 3–5 children/classroom each day over a 3–5 day period at each school. All leftover food remaining on the trays was labeled and measured with utensils and a digital ounce/gram scale that was calibrated daily. The amount of food/beverages eaten by each child was determined by calculating the difference between the amount of food served and the amount discarded.
Foods Consumed Outside of Preschool
The day before a child was to be observed, the child’s parent/guardian was given a packet containing a food record form for recording meals and snacks consumed outside of school, a food portion visual guide to assist in estimating the amount of food eaten, and a product identification notebook. The parent was asked to record all food and drinks consumed by the child outside of school that afternoon/evening and the following morning prior to school. The parent was also asked to record her own intake for the full 24-hour period. On the morning that the child was observed, these records were collected and reviewed by the research staff for completeness. A single day’s classroom observation plus the parent’s record or recall represented 24 hours of nutrient intake. The dietary intake data were processed using the Nutrition Data System for Research, Version 2007 (NDS-R, Nutrition Coordinating Center, University of Minnesota). The food group variables created by NDS-R were used to calculate consumption of fruit, 100% fruit juice, and vegetables. The fruit variable includes citrus and non-citrus fruits and excludes juices, avocado, fried fruits, and fruit-based savory snacks. The vegetable variable includes all vegetable food group variables, plus avocado: dark green and deep yellow vegetables, tomatoes, white potatoes and other starchy vegetables, legumes, fried potatoes, other fried vegetables, vegetable juice, and other vegetables. We also conducted a secondary analysis excluding fried potatoes, other fried vegetables, and vegetable juice.
The percentage of children and parents meeting national guidelines for several nutrients and food groups was also estimated. (26) Since guidelines differ for children ages 3 and under and there were not enough 3-year-olds to analyze separately, only children ≥4 years were included in the dietary guideline analysis. Similarly, since most parents were women aged 19–50 years, all women under 19 or over 50 and all men of any age were excluded from the dietary guideline analysis.
Statistical Analyses
Differences in baseline characteristics between the intervention and control groups were tested for significance using the Wilcoxon rank sum test for income, t-tests for all other continuous variables, and chi-square tests for categorical variables. T-tests were used to test for gender differences in physical activity, screen time, and diet at baseline. To test for differences between groups in BMI and BMI Z score change at post-intervention and 1-year follow-up, we used a mixed model analysis of variance, controlling for school and classroom nested within school, as well as a mixed model analysis of covariance, controlling for school, classroom nested within school, the BMI percentile at baseline (<85th or ≥ 85th), baseline age, and time between visits. Change from baseline was the dependent variable. We used a mixed model analysis of covariance to test for differences between groups in physical activity at post-intervention and in screen time and diet at post-intervention and 1-year follow-up, controlling for school, classroom nested within school, and the baseline value. The value at post-intervention or 1-year follow-up was the dependent variable. Test statistics had 2 degrees of freedom. (27) Only participants with height and weight measurements, valid accelerometer records, complete screen time data, or valid diet data at baseline and follow-up were included in the relevant follow-up analyses. Parent diet records with total energy < 500 kcal/day or > 5000 kcal/day were excluded from analyses of dietary intake. (28) All analyses were conducted using SAS version 9.2 (SAS Institute Inc., Cary, NC).
RESULTS
Feasibility
Recruitment and retention
Principals and preschool teachers from four CPS schools agreed to allow children in their preschool classrooms to participate in the study (see Figure 1). Two half-day classrooms from each school participated. Parents signed consent forms for 147 of the 157 children enrolled in the participating classrooms (94%). One child left the school before the intervention began, so 146 children from 142 families participated in the study. Four parents had two children participating. Of the 142 parents who signed consent forms, 123 completed an interview at baseline (61 intervention, 62 control.) Almost all of the children completed the post-intervention visit (98%), and 88% had height and weight measured at 1-year follow-up.
Parent attendance
Of the 61 intervention group parents who completed the baseline interview, 23 (38%) attended at least one of the six classes offered.
Baseline data
Characteristics of parents and children at baseline are shown in Table 1. In general, Hispanic parents’ acculturation level was quite low: mean (SD) 1.8 (1.0) on a 1–5 scale. Most (86%) of the Hispanic parents were born in Mexico. Most (78%) of the Hispanic parents chose to complete the interview in Spanish.
Table 1.
Characteristics of participating children and parents at baseline, Family-Based Hip-Hop to Health
| INTERVENTION | CONTROL | ALL | ||||
|---|---|---|---|---|---|---|
| N | Mean (SD) | N | Mean (SD) | N | Mean (SD) | |
| CHILDREN | ||||||
| Female, n (%) | 72 | 38 (53%) | 74 | 35 (47%) | 146 | 73 (50%) |
| Race, n (%) | 72 | 74 | 146 | |||
| Latino | 69 (96%) | 68 (92%) | 137 (94%) | |||
| Black | 0 (0%) | 3 (4%) | 3 (2%) | |||
| Multiracial/other | 3 (4%) | 3 (4%) | 6 (4%) | |||
| Age, months | 72 | 53.7 (4.9) | 74 | 54.7 (5.1) | 146 | 54.2 (5.0) |
| BMI, kg/m2 | 72 | 17.0 (1.9) | 74 | 16.9 (2.0) | 146 | 17.0 (2.0) |
| BMI Z score for age and sex | 72 | 0.96 (1.07) | 74 | 0.83 (0.97) | 146 | 0.90 (1.02) |
| BMI percentile for age and sex, n (%) | 72 | 74 | 146 | |||
| < 5th | 2 (3%) | 1 (1%) | 3 (2%) | |||
| 5th – < 85th | 37 (51%) | 39 (53%) | 76 (52%) | |||
| 85th – < 95th | 13 (18%) | 23 (31%) | 36 (25%) | |||
| ≥ 95th | 20 (28%) | 11 (15%) | 31 (21%) | |||
| Weight, kg | 72 | 19.2 (3.3) | 74 | 19.1 (3.4) | 146 | 19.1 (3.4) |
| Height, cm | 72 | 105.8 (5.3) | 74 | 106.0 (4.9) | 146 | 105.9 (5.1) |
| MVPA, min/day | 42 | 90.6 (24.9) | 28 | 98.8 (38.7) | 70 | 93.9 (31.2) |
| Percentage of time in sedentary behavior | 42 | 53.7 (6.0) | 28 | 53.4 (7.7) | 70 | 53.6 (6.7) |
| Counts/min | 42 | 610 (130) | 28 | 638 (177) | 70 | 621 (150) |
| TV viewing, hr/day | 60 | 2.0 (1.3) | 64 | 1.8 (1.4) | 124 | 1.9 (1.4) |
| Screen timea, hr/day | 60 | 3.2 (1.7) | 64 | 3.0 (1.6) | 124 | 3.1 (1.7) |
| Energy, kcal | 55 | 1340 (481) | 58 | 1366 (481) | 113 | 1353 (479) |
| Total fat, % kcal | 55 | 29.0 (8.2) | 58 | 33.4 (9.0) | 113 | 31.3 (8.9) |
| Fiber, g/1000 kcal | 55 | 9.0 (3.7) | 58 | 8.2 (3.8) | 113 | 8.6 (3.8) |
| Fruitb, servings/day | 55 | 0.7 (0.9) | 58 | 1.1 (1.2) | 113 | 0.9 (1.1) |
| 100% fruit juice, servings/day | 55 | 0.9 (1.2) | 58 | 1.2 (1.4) | 113 | 1.0 (1.3) |
| Vegetablesc, servings/day | 55 | 1.4 (1.5) | 58 | 1.1 (0.9) | 113 | 1.2 (1.2) |
| PARENTS | ||||||
| Relationship to childd, n (%) | 61 | 62 | 123 | |||
| Mother | 54 (89%) | 59 (95%) | 113 (92%) | |||
| Father | 5 (8%) | 3 (5%) | 8 (7%) | |||
| Grandparent/other | 2 (3%) | 0 (0%) | 2 (2%) | |||
| Female, n (%) | 72 | 63 (88%) | 70 | 64 (91%) | 142 | 127 (89%) |
| Age, years | 61 | 32.0 (6.2) | 62 | 33.6 (5.8) | 123 | 32.8 (6.0) |
| Education, years | 61 | 11.2 (2.3) | 62 | 11.3 (2.2) | 123 | 11.2 (2.2) |
| Income, $, median | 58 | 15,000 | 59 | 15,000 | 117 | 15,000 |
| Married or living with a partner, n (%) | 61 | 48 (79%) | 62 | 54 (87%) | 123 | 102 (83%) |
| Employed full-time, n (%) | 61 | 16 (26%) | 62 | 13 (21%) | 123 | 29 (24%) |
| Children < 18 in household | 61 | 2.6 (1.1) | 62 | 2.8 (1.1) | 123 | 2.7 (1.1) |
| Other adults in household | 61 | 1.5 (1.0) | 62 | 1.3 (0.9) | 123 | 1.4 (1.0) |
| BMI, kg/m2 | 50 | 30.1 (5.8) | 47 | 30.5 (5.8) | 97 | 30.3 (5.7) |
| Weight, kg | 50 | 73.7 (17.2) | 47 | 74.0 (15.2) | 97 | 73.9 (16.2) |
| Height, cm | 50 | 156.1 (8.0) | 47 | 155.7 (5.4) | 97 | 155.9 (6.9) |
| BMI categoriese, n (%) | 50 | 47 | 97 | |||
| Underweight | 0 (0%) | 0 (0%) | 0 (0%) | |||
| Normal weight | 12 (24%) | 9 (19%) | 21 (22%) | |||
| Overweight | 14 (28%) | 17 (36%) | 31 (32%) | |||
| Obese | 24 (48%) | 21 (45%) | 45 (46%) | |||
| MVPA, min/day | 30 | 33.0 (17.9) | 13 | 21.4 (12.7) | 43 | 29.5 (17.2) |
| MVPA in bouts ≥ 10 min, min/wk | 30 | 30.5 (43.3) | 13 | 13.4 (22.6) | 43 | 25.4 (38.8) |
| Percentage of time in sedentary behavior | 30 | 50.0 (7.8) | 13 | 54.2 (6.5) | 43 | 51.3 (7.6) |
| Counts/min | 30 | 406 (104) | 13 | 344 (86) | 43 | 387 (102) |
| TV viewing, hr/day | 60 | 1.9 (1.2) | 61 | 1.7 (1.1) | 121 | 1.8 (1.1) |
| Screen timea, hr/day | 60 | 3.4 (2.4) | 61 | 2.8 (1.6) | 121 | 3.1 (2.0) |
| Energy, kcal | 54 | 1809 (640) | 52 | 1446 (624) | 106 | 1631 (655) |
| Total fat, % kcal | 54 | 31.1 (8.1) | 52 | 33.7 (10.2) | 106 | 32.4 (9.2) |
| Fiber, g/1000 kcal | 54 | 11.1 (5.2) | 52 | 10.6 (4.8) | 106 | 10.8 (5.0) |
| Fruitb, servings/day | 54 | 1.0 (1.5) | 52 | 0.8 (1.1) | 106 | 0.9 (1.3) |
| 100% fruit juice, servings/day | 54 | 0.6 (1.4) | 52 | 0.4 (0.9) | 106 | 0.5 (1.2) |
| Vegetablesc, servings/day | 54 | 3.2 (2.7) | 52 | 2.2 (1.7) | 106 | 2.7 (2.3) |
| Latino parents only | ||||||
| Acculturationf | 61 | 2.0 (0.9) | 60 | 1.7 (1.1) | 121 | 1.8 (1.0) |
| Born in Mexico, no. (%) | 61 | 55 (90%) | 60 | 49 (82%) | 121 | 104 (86%) |
MVPA, moderate-to-vigorous physical activity.
Time spent watching television, DVDs or videos, playing video games, or using a computer.
Excludes juices, avocado, fried fruits, and fruit-based savory snacks.
Includes all NDS vegetable food groups and avocado.
Only one child per family is included.
Underweight: < 18.5 kg/m2, normal weight: 18.5-<25 kg/m2, overweight: 25-<30 kg/m2, obese: ≥30 kg/m2.
From 4-item Marin scale; scores can range from 1 (least acculturated) to 5 (most acculturated).
At baseline, 70 children and 43 parents had valid accelerometer records. Mean (SD) time worn was 12.3 (1.7) hr/day for the children with valid records and 12.7 (1.7) hr/day for the parents. Of the 76 children without accelerometer records, 54 did not wear the accelerometer (usually because the parent could not be reached on the night before the accelerometers were distributed), and 22 wore the accelerometer but did not wear it for at least 8 hours on at least 4 days. Similarly, 94 parents did not wear an accelerometer, and 5 wore one but did not have a valid record. Screen time data were missing if the parent did not complete the baseline interview or they did not respond to all items on the questionnaire; 124 children and 121 parents had screen time data. At baseline, 24-hour diet recalls were collected for 115 children and 108 parents. Two child records and 2 parent records were excluded because information about one or more meals was missing from the record; 113 children and 106 parents had valid records. Energy was between 500 and 5000 kcal for all parent records at baseline.
Perception of overweight
At baseline, very few mothers of overweight or obese children perceived their child as overweight, and none perceived their child as very overweight. Only 1 of 27 children with BMI between the 85th and 95th percentile (4%) and 2 of 15 children with BMI between the 95th and 99th percentile (13%) were perceived as overweight by their mothers. However, among children whose BMI was ≥ 99th percentile, 67% of mothers (8 of 12) said that their child was overweight.
Gender differences
At baseline, no significant gender differences were observed in BMI (17.0 (1.6) kg/m2 for boys and 16.9 (2.2) kg/m2 for girls, p=.83) or BMI Z score (0.97 (1.03) for boys and 0.83 (1.01) for girls, p=.42). On average, boys were more active than girls, spending 107.7 (29.4) vs 78.4 (25.7) min/day in MVPA, p<.001. Boys were significantly more likely than girls to achieve the level of activity recommended for preschool children (i.e., at least 60 minutes of MVPA/day): 97% vs 76%, p=.01. Accelerometer counts/min were also significantly different: 677 (136) vs 558 (140) counts per min, p<.001. Boys spent about 52% of the time in sedentary behavior, and girls spent about 56% (p=.02). Although boys were more active than girls, their average screen time was also higher: 3.5 (1.8) vs 2.7 (1.5) hr/day, p=.007. There were no significant gender differences in diet (energy, fat, fiber, fruits, or vegetables).
Estimated effectiveness
BMI and Z score change
Changes in child BMI, BMI Z score, weight, and height at post-intervention and 1-year follow-up are shown in Table 2. As expected, no significant differences were observed between groups at the post-intervention visit. BMI and BMI Z score were lower at 1-year follow-up in both groups, and the estimated decline was somewhat greater in the control group than in the intervention group. The difference between groups was statistically significant for BMI change adjusted for BMI percentile at baseline (<85th or ≥ 85th), baseline age (years), months from baseline, preschool, and classroom, but not for BMI change adjusted for school and classroom only or for BMI Z score change.
Table 2.
Adjusted change in children’s BMI, BMI Z score, weight, and height at post-intervention and 1-year follow-up, Family-Based Hip-Hop to Health
| INTERVENTION | CONTROL | DIFFERENCE | |
|---|---|---|---|
| Mean | Mean | (FBI-GHI) | |
| change (SE) | change (SE) | (95% CI) | |
| POST-INTERVENTION | N=71 | N=72 | |
| BMI (kg/m2)a,b | 0.16 (0.05) | 0.09 (0.05) | 0.07 (−0.23 to 0.38) |
| Adjusted BMI (kg/m2)c | 0.11 (0.01) | 0.15 (0.01) | −0.04 (−0.13 to 0.05) |
| BMI Z scorea | 0.00 (0.01) | 0.03 (0.01) | −0.02 (−0.08 to 0.03) |
| Adjusted BMI Z scorec | 0.00 (0.02) | 0.03 (0.01) | −0.03 (−0.13 to 0.06) |
| Weight (kg)a | 1.66 (0.22) | 1.13 (0.22) | 0.53 (−0.83 to 1.89) |
| Height (cm)a | 3.93 (0.40) | 2.80 (0.40) | 1.13 (−1.33 to 3.60) |
| YEAR 1 | N=61 | N=67 | |
| BMI (kg/m2)a,d | −0.51 (0.11) | −0.68 (0.10) | 0.17 (−0.45 to 0.80) |
| Adjusted BMI (kg/m2)c | −0.43 (0.03) | −0.65 (0.03) | 0.22 (0.02 to 0.41)* |
| BMI Z scorea | −0.51 (0.05) | −0.54 (0.05) | 0.03 (−0.28 to 0.34) |
| Adjusted BMI Z scorec | −0.48 (0.02) | −0.55 (0.01) | 0.07 (−0.03 to 0.17) |
| Weight (kg)a | 3.61 (0.19) | 3.04 (0.18) | 0.57 (−0.55 to 1.68) |
| Height (cm)a | 11.31 (0.17) | 10.42 (0.17) | 0.89 (−0.14 to 1.92) |
p < .05.
Adjusted for preschool and classroom using SAS Proc Mixed.
For children with post-intervention anthropometric data, the unadjusted mean (SD) BMI at baseline was 17.1 (1.9) kg/m2 in the intervention group and 16.9 (2.0) kg/m2 in the control group. At post-intervention, the unadjusted mean (SD) was 17.2 (2.3) kg/m2 in the intervention group and 16.9 (2.2) kg/m2 in the control group.
Adjusted for BMI percentile at baseline (<85th or ≥ 85th), baseline age (years), months from baseline, preschool and classroom using SAS Proc Mixed.
For children with Year 1 anthropometric data, the unadjusted mean (SD) BMI at baseline was 17.0 (1.9) kg/m2 in the intervention group and 16.9 (2.1) kg/m2 in the control group. At Year 1, the unadjusted mean (SD) was 16.4 (2.5) kg/m2 in the intervention group and 16.2 (2.3) kg/m2 in the control group.
The parent intervention was not designed to be a weight loss program. As expected, there was not a significant difference between groups in parent weight or BMI change at post-intervention or 1-year follow-up.
Physical activity
Children’s post-intervention physical activity, adjusted for baseline activity, preschool, and classroom, is shown in Table 3. Estimates of MVPA and accelerometer counts/min were higher in the intervention group than in the control group, though these differences were not statistically significant. Among the 27 parents with valid accelerometer records at baseline and post-intervention, unadjusted MVPA in ≥ 10-minute bouts was similar in both groups at post-intervention: mean (SD) = 55.2 (60.7) min/wk in the intervention group and 51.4 (71.8) min/wk in the control group.
Table 3.
Adjusteda physical activity, screen time, and diet at post-intervention, Family-Based Hip-Hop to Health
| DIFFERENCE | |||
|---|---|---|---|
| INTERVENTION | CONTROL | (FBI-GHI) | |
| Mean (SE) | Mean (SE) | (95% CI) | |
| CHILDREN | |||
| Physical activity | N=23 | N=23 | |
| MVPA, min/day | 109.9 (7.5) | 100.9 (7.0) | 9.02 (−35.1 to 53.2) |
| MVPA, min/hour worn | 7.9 (0.2) | 7.8 (0.2) | 0.07 (−1.31 to 1.46) |
| Moderate activity, min/day | 77.9 (5.7) | 75.1 (5.0) | 2.78 (−30.0 to 35.6) |
| Vigorous activity, min/day | 25.9 (2.2) | 24.1 (2.1) | 1.81 (−11.5 to 15.1) |
| % time sedentary | 53.7 (1.0) | 53.9 (1.0) | −0.27 (−6.59 to 6.05) |
| Counts/min worn | 643 (24) | 631 (23) | 11.6 (−130.0 to 153.3) |
| Screen time | N=55 | N=61 | |
| Television, hr/day | 2.1 (0.1) | 2.0 (0.1) | 0.07 (−0.41 to 0.56) |
| Screen timeb, hr/day | 3.5 (0.1) | 3.2 (0.1) | 0.26 (−0.58 to 1.10) |
| Diet | N=50 | N=56 | |
| Energy, kcal | 1313 (12) | 1339 (12) | −26.3 (−96.0 to 43.5) |
| Fat, % kcal | 28.1 (0.8) | 30.2 (0.7) | −2.06 (−6.92 to 2.79) |
| Fiber, g/1000 kcal | 9.5 (0.3) | 8.9 (0.2) | 0.63 (−0.77 to 2.03) |
| Fruitc, servings/day | 1.3 (0.1) | 1.1 (0.1) | 0.28 (−0.36 to 0.92) |
| 100% fruit juice, servings/day | 1.0 (0.3) | 1.8 (0.3) | −0.83 (−2.84 to 1.18) |
| Vegetablesd, servings/day | 1.1 (0.2) | 1.3 (0.2) | −0.18 (−1.35 to 0.99) |
| PARENTS | |||
| Screen time | N=54 | N=58 | |
| Television, hr/day | 1.8 (0.1) | 1.9 (0.1) | −0.11 (−0.85 to 0.64) |
| Screen timeb, hr/day | 3.1 (0.04) | 2.9 (0.05) | 0.25 (−0.01 to 0.51) |
| Diet | N=45 | N=48 | |
| Energy, kcal | 1643 (71) | 1582 (67) | 61.5 (−368.5 to 491.5) |
| Fat, % kcal | 28.9 (2.4) | 28.9 (2.4) | −0.05 (−14.7 to 14.5) |
| Fiber, g/1000 kcal | 13.0 (0.4) | 12.9 (0.4) | 0.11 (−2.31 to 2.54) |
| Fruitc, servings/day | 1.3 (0.2) | 1.2 (0.2) | 0.03 (−1.46 to 1.52) |
| 100% fruit juice, servings/day | 0.7 (0.4) | 0.9 (0.4) | −0.26 (−2.52 to 2.01) |
| Vegetablesd, servings/day | 2.4 (0.5) | 2.9 (0.5) | −0.48 (−3.62 to 2.66) |
MVPA, moderate-to-vigorous physical activity.
p < .05.
Adjusted for the baseline value, preschool and classroom using SAS Proc Mixed.
Time spent watching television, DVDs or videos, playing video games, or using a computer.
Excludes juices, avocado, fried fruits, and fruit-based savory snacks.
Includes all NDS vegetable food groups and avocado.
Screen time
Table 3 shows television viewing and total screen time at post-intervention, adjusted for the baseline value, preschool, and classroom. Estimated screen time was similar in the two groups at post-intervention and 1-year follow-up for children and parents. At 1-year follow-up, adjusted mean (SE) screen time for children was 3.3 (0.5) hr/day in the intervention group and 3.4 (0.5) hr/day in the control group.
Diet
Post-intervention dietary intake, adjusted for baseline intake, preschool, and classroom is shown in Table 3. At post-intervention, no statistically significant differences were observed between groups in children’s or parents’ dietary intake. Excluding fried vegetables, juices, and avocado did not substantially alter the vegetable intake results; for children, the estimated difference between groups (95% CI) at post-intervention was −0.16 (−1.15 to 0.83) servings/day. A total of 68 children and 75 parents had valid diet records at both baseline and one-year follow-up. There were no statistically significant differences between groups in children’s or parents’ dietary intake at one-year follow-up.
Physical Activity/Dietary Guidelines
Most of the 46 children with valid accelerometer data at baseline and post-intervention met national guidelines by engaging in at least 60 minutes of MVPA/day: 91% at baseline, 93% at post-intervention. However, very few parents engaged in ≥ 150 min/wk of MVPA at either visit: 1 parent at baseline, 3 at post-intervention, N=27. Relatively few children had ≤2 hours of screen time/day at any visit. At post-intervention, 26% of children had ≤2 hours of screen time/day, (N=116). Recommended fat consumption for children aged 4–8 years is 25–35% kcal; 40% were in that range at baseline and 53% at post-intervention, (N=93). Fiber intake was <25 g/day for almost all of the children at baseline and post-intervention; 1 child consumed the recommended amount at baseline and 3 at post-intervention. Most children (80%) met the recommendations for fruit intake (≥1 serving/day) at post-intervention, but fruit juices made up a substantial fraction of fruit consumption. When juices were excluded, only 48% of children ate at least 1 serving/day of fruit. Similarly, only 30% of children consumed the recommended ≥1.5 servings/day of vegetables.
DISCUSSION
The purpose of this study was to assess the feasibility of a family-based obesity prevention intervention (FBI) for 3–5 year old Hispanic children and to estimate its effectiveness in producing smaller average changes in BMI appropriate for growth at one year follow-up. We also sought to estimate the effectiveness of the FBI in producing changes in physical activity, television viewing, fat intake, fiber intake, and fruit and vegetable intake in three to five year old Hispanic children and their parents at post-intervention and Year 1 follow-up.
Our results reflect the feasibility of the school-based and family-based component, but adherence to the parent intervention sessions was limited. To date, only a few weight-related interventions have focused specifically on Hispanic populations. (9, 29) A recent article by Ramirez and colleagues (30) highlighted the scarcity of data available on Latinos related to prevention childhood obesity. A systematic analysis of childhood obesity prevention and treatment interventions designed specifically for Hispanic children (29) found more treatment programs than prevention programs; the interventions included varying levels of parental involvement. (31) The most promising results were shown by weight loss interventions targeting already overweight or obese older children and adolescents, rather than by obesity prevention interventions. (31) These results suggest that obesity prevention efforts may not be especially compelling for Hispanic families, and interest in altering behaviors associated with excessive weight gain may not be a strong priority until a child is becomes overweight or obese.
Although the family unit is seen as one of the major influences on a child’s developing weight status, (32) evidence-based strategies for engaging parents in obesity prevention efforts are lacking. Like another multi-site randomized trial targeting obesity prevention with minority families, (33) we conducted extensive formative work in an effort to develop an intervention that aligned with the articulated needs of our target population and incorporated a theoretically sound framework. Data suggest that individuals are more apt to engage in interventions that are reflective of their cultural characteristics. (34) Parents indicated that creating a healthy home environment was a high priority. Nonetheless, our intervention may not have sufficiently acknowledged and countered the perception among Hispanic parents that larger body sizes for young children reflect a healthier child. (35) Some data also suggest that among low-income mothers, there is a belief that weight is determined more by genetics than by diet and activity patterns. (35) Therefore, although we developed the FBI to be culturally sound, we may not have addressed some key beliefs or perceptions specific to this population that influence receptivity to obesity prevention strategies. A home-based intervention, utilizing promatoras, might have improved acceptability of the intervention. The majority of the parents did not perceive their overweight or obese children as overweight, so they may have been less concerned, which translated into lower attendance levels. This is similar to other studies, (36–38) but does present a challenge for obesity prevention efforts.
The decrease in BMI Z score in both the intervention and control groups was unexpected. However, our findings are similar to other recent findings among low-income minority children, reflecting a possible decreasing trend in obesity prevalence. (39) National Health and Nutrition Examination Survey (NHANES) estimates of prevalence of high BMI for age from 1999–2010 also suggest that obesity may have peaked among 2–5 year old children. (40)
The downward trend in BMI Z score in this population may also be due, in part, to the increased recognition of obesity as a growing public health problem, both at national and local levels. For example, the first lady, Michelle Obama, has made healthy eating and activity part of the national agenda, by creating “Let’s MOVE” [http://www.letsmove.gov/. Accessed 2/13/2012.] Local efforts, including the Consortium to Lower Obesity in Chicago Children (CLOCC) have been developed to support systemic changes supporting healthy lifestyles across a large metropolitan area [http://www.clocc.net/. Accessed 2/13/2012.] School-based data indicate falling rates of obesity in young children in the Chicago area [http://www.clocc.net/coc/prevalence.html. Accessed 2/13/2012.] While declining rates represent positive news, the prevalence of obesity among children in our pilot at one-year follow-up (15%) was still somewhat higher than the prevalence in a nationally representative sample of 2–5 year old children (12.1%). (7)
There were no differences between groups in activity, diet, or TV/screen time in children. Likewise, no differences in these variables were observed for parents. When comparing our results with national recommendations for diet, (26) physical activity, (23) and TV/screen time (25) for adults and children, the children in our sample were generally meeting recommendations for MVPA of at least 60 minute per day at both baseline and post-intervention. On average, parents engaged in 29.5 (17.2) min/day of MVPA at baseline. However, most of that MVPA occurred in short bursts rather than in the recommended bouts of 10 minutes or more. When only 10-minute bouts were considered, parents had an average of 25.4 (38.8) min/week of MVPA, far short of the recommended 150 min/week. For many parents and children, the reported dietary intake did not conform to recommended standards. This was particularly noteworthy for fiber intake, where only 1% of the children met intake recommendations at baseline and 3% at post-intervention. Parents were somewhat more likely to meet intake recommendations for fiber: 25% at post-intervention. TV/screen time was also high for both parents and children, and there were no group differences as a function of the intervention. Only 26% of the children met the recommendation of ≤2 hours of TV/screen time per day at post-intervention.
Limitations of the study include a relatively homogenous sample of low-acculturated and low-income Hispanic families, thereby limiting generalizability. Additional limitations were the use of a single 24-hour diet recall rather than multiple recalls, and incomplete data from the dietary recall and activity (acceleromtery) records for some participants.
Published studies demonstrate that intensive weight loss interventions can be successful in reducing weight among overweight and obese Hispanic children. (31) However, even these successful weight loss treatment studies do not provide insight into how to best engage parents in obesity prevention. The lack of evidence-based approaches to involving parents in obesity prevention for Hispanic children suggests that continued research is essential.
Acknowledgments
This study was funded, in part, by the National Cancer Institute (CA121423), R25CA057699, and the Consortium to Lower Obesity in Chicago Children (CLOCC). We would also like to thank the Chicago Public Schools Early Childhood Education Program, the families and teachers who participated in the project, and the principals who supported the project. We would like to thank Ms. Guadalupe Compean for her technical assistance.
Footnotes
No financial disclosure information.
Disclosure
The authors have no conflicts of interest to disclose.
Cited Literature
- 1.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012 doi: 10.1001/jama.2012.39. Published online January 17, 2012. [DOI] [PubMed] [Google Scholar]
- 2.Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282(16):1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 3.National Institutes of Health / National Heart, Lung and Blood Institute. [Last accessed on February 13, 2012];Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. 1998 Available from: http://www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.pdf.
- 4.Winkleby MA, Kraemer HC, Ahn DK, Varady AN. Ethnic and socioeconomic differences in cardiovascular disease risk factors: findings for women from the Third National Health and Nutrition Examination Survey, 1988–1994. JAMA. 1998;280(4):356–362. doi: 10.1001/jama.280.4.356. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 6.Fitzgibbon ML, Stolley MR, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Two year follow-up results for Hip-Hop to Health Jr.: a randomized controlled trial for overweight prevention in preschool minority children. J Pediatr. 2005;146(5):618–625. doi: 10.1016/j.jpeds.2004.12.019. [DOI] [PubMed] [Google Scholar]
- 7.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ortman JM, Guarneri CE. [Last accessed on February 13, 2012];United States Population Projections: 2000 to 2050 United States Census Bureau. 2009 Available from: http://www.census.gov/population/www/projections/analytical-document09.pdf.
- 9.Fitzgibbon ML, Stolley MR, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Hip-Hop to Health Jr. for Latino preschool children. Obesity. 2006;14(9):1616–1625. doi: 10.1038/oby.2006.186. [DOI] [PubMed] [Google Scholar]
- 10.Golan M. Parents as agents of change in childhood obesity--from research to practice. Int J Pediatr Obes. 2006;1(2):66–76. doi: 10.1080/17477160600644272. [DOI] [PubMed] [Google Scholar]
- 11.Epstein LH. Family-based behavioural intervention for obese children. Int J Obes Relat Metab Disord. 1996;20 (Suppl 1):S14–21. [PubMed] [Google Scholar]
- 12.Bandura A. Self-efficacy: the exercise of control. W.H. Freeman and Company; New York, NY, USA: 1997. [Google Scholar]
- 13.Clark NM, Valerio MA. The role of behavioural theories in educational interventions for paediatric asthma. Paediatric Respir Rev. 2003;4:325–333. [PubMed] [Google Scholar]
- 14.Rosenstock IM. The health belief model and preventive health behavior. Health Education Monograph. 1974;2:354–386. [Google Scholar]
- 15.Deci EL. The relation of interest to the motivation of behavior: a self-determination theory perspective. In: Renninger KA, Hidi S, Krapp A, editors. The Role of Interest in Learning and Development. Lawrence Erlbaum Associates; Hillsdale, NJ, USA: 1992. pp. 43–70. [Google Scholar]
- 16.Ariza AJ, Chen EH, Binns HJ, KauferChristoffel K. Risk factors for overweight in five- to six-year-old Hispanic-American children: A pilot study. J Urban Health. 2004;81(1):150–161. doi: 10.1093/jurban/jth091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sherry B, McDivitt J, Birch LL, et al. Attitudes, practices, and concerns about child feeding and child weight status among socioeconomically diverse White, Hispanic, and African-American mothers. J Am Diet Assoc. 2004;104:215–221. doi: 10.1016/j.jada.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 18.Sallis JF, Nader PR, Broyles SL, et al. Correlates of physical activity at home in Mexican-American and Anglo-American preschool children. Health Psychol. 1993;12(5):390–398. doi: 10.1037//0278-6133.12.5.390. [DOI] [PubMed] [Google Scholar]
- 19.Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable E. Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Sciences. 1987;9(2):183–205. [Google Scholar]
- 20.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 21.Pfeiffer KA, Dowda M, McIver KL, Pate RR. Factors related to objectively measured physical activity in preschool children. Pediatric Exerc Sci. 2009;21(2):196–208. doi: 10.1123/pes.21.2.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167(7):875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.U.S. Department of Health and Human Services (USDHHS) Physical Activity Guidelines for Americans. [Last accessed on February 13, 2012];Be Active, Healthy, and Happy! 2008 Available from: http://www.health.gov/paguidelines/pdf/paguide.pdf.
- 24.Borzekowski DL, Robinson TN. The remote, the mouse, and the no. 2 pencil: the household media environment and academic achievement among third grade students. Arch Pediatr Adolesc Med. 2005;159(7):607–613. doi: 10.1001/archpedi.159.7.607. [DOI] [PubMed] [Google Scholar]
- 25.Committee on Public Education. American Academy of Pediatrics: Children, Adolescents, and Television. Pediatrics. 2001;107(2):423–426. doi: 10.1542/peds.107.2.423. [DOI] [PubMed] [Google Scholar]
- 26.U.S. Department of Agriculture and U.S. Department of Health and Human Services. [Last accessed on February 13, 2012];Dietary Guidelines for Americans. 2010 Available from: http://health.gov/dietaryguidelines/dga2010/dietaryguidelines2010.pdf.
- 27.Murray DM. Design and Analysis of Group-Randomized Trials. Oxford University Press; New York, New York, USA: 1998. [Google Scholar]
- 28.Stamler J, Elliott P, Dennis B, et al. INTERMAP: background, aims, design, methods, and descriptive statistics (nondietary) J Hum Hypertens. 2003;17(9):591–608. doi: 10.1038/sj.jhh.1001603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Branscum P, Sharma M. A systematic analysis of childhood obesity prevention interventions targeting Hispanic children: lessons learned from the previous decade. Obesity Revs. 2011;12(5):e151–e158. doi: 10.1111/j.1467-789X.2010.00809.x. [DOI] [PubMed] [Google Scholar]
- 30.Ramirez AG, Chalela P, Gallion KJ, Green LW, Ottoson J. Salud America! Developing a national Latino childhood obesity research agenda. Health Educ Behav. 2011;38(3):251–260. doi: 10.1177/1090198110372333. [DOI] [PubMed] [Google Scholar]
- 31.Olvera N, Power TG. Brief report: parenting styles and obesity in Mexican American children: a longitudinal study. J Pediatr Psychol. 2010;35(3):243–249. doi: 10.1093/jpepsy/jsp071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McGarvey E, Keller A, Forrester M, Williams E, Seward D, Suttle DE. Feasibility and benefits of a parent-focused preschool child obesity intervention. Am J Public Health. 2004;94(9):1490–1495. doi: 10.2105/ajph.94.9.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Klesges RC, Obarzanek E, Kumanyika S, et al. The Memphis Girls’ Health Enrichment Multi-site Studies (GEMS): an evaluation of the efficacy of a 2-year obesity prevention program in African American girls. Arch Pediatr Adolesc Med. 2010;164(11):1007–1014. doi: 10.1001/archpediatrics.2010.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kumpfer KL, Alvarado R, Smith P, Bellamy N. Cultural sensitivity and adaptation in family-based prevention interventions. Prev Sci. 2002;3(3):241–246. doi: 10.1023/a:1019902902119. [DOI] [PubMed] [Google Scholar]
- 35.Crawford PB, Gosliner W, Anderson C, et al. Counseling Latina mothers of preschool children about weight issues: suggestions for a new framework. J Am Diet Assoc. 2004;104(3):387–394. doi: 10.1016/j.jada.2003.12.018. [DOI] [PubMed] [Google Scholar]
- 36.Baughcum AE, Chamberlin LA, Deeks CM, Powers SW, Whitaker RC. Maternal perceptions of overweight preschool children. Pediatrics. 2000;106(6):1380–1386. doi: 10.1542/peds.106.6.1380. [DOI] [PubMed] [Google Scholar]
- 37.Chaparro MP, Langellier BA, Kim LP, Whaley SE. Predictors of accurate maternal perception of their preschool child’s weight status among Hispanic WIC participants. Obesity. 2011;19(10):2026–2030. doi: 10.1038/oby.2011.105. [DOI] [PubMed] [Google Scholar]
- 38.Hackie M, Bowles CL. Maternal perception of their overweight children. Public Health Nurs. 2007;24(6):538–546. doi: 10.1111/j.1525-1446.2007.00666.x. [DOI] [PubMed] [Google Scholar]
- 39.Sekhobo JP, Edmunds LS, Reynolds DK, Dalenius K, Sharma A. Trends in prevalence of obesity and overweight among children enrolled in the New York State WIC program, 2002–2007. Public Health Rep. 2010;125(2):218–224. doi: 10.1177/003335491012500210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]