Abstract
Objective
To examine the structure of illicit opioid abuse and dependence within an opioid dependent sample, and its relationship to other clinical variables.
Method
1511 opioid dependent participants underwent an interview covering substance use and dependence, psychiatric history, child maltreatment, family background, adult violence and criminal history. Dimensional, latent class and factor mixture models were fit to the abuse and dependence data. Classes were then compared on a range of demographic and clinical covariates.
Results
A two class, one factor model provided the best fit of all the models tested. The two classes differed with respect to endorsement probabilities on a range of abuse and dependence criteria, and also with respect to the odds of other drug dependence diagnoses, antisocial personality disorder, and non-fatal opioid overdose. Within class severity was associated with similar variables: other drug dependence, borderline personality disorder, and opioid overdose.
Conclusion
In an in-treatment, opioid dependent sample, there appears to be two classes of individuals exhibiting distinct patterns of abuse and dependence criteria endorsement and to differ on externalizing but not internalizing disorders. This study provides preliminary evidence that the proposed DSM-V opioid use disorder distinction between moderate and severely dependent persons is valid. Class one participants were not only more severely dependent, but had greater odds for opioid overdoses, other drug dependence, and ASPD.
1. Introduction
Opioid dependence is frequently associated with polydrug use, mental health disorders, suicidality, overdose, criminal justice system involvement and early onset of substance use and other externalizing behaviors [1-4]. The Diagnostic and Statistical Manual of Mental Disorders (4th edition, DSM-IV) assumes two hierarchically organized categories of opioid use disorder: heroin abuse or heroin dependence [5]. To be diagnosed with opioid dependence, three of seven dependence criteria must be met [5]. Thus, two people with entirely different dependence symptoms may be given the same diagnosis [6]. An important empirical and clinical question is whether or not these differences actually matter. Evidence from the alcohol dependence diagnosis suggests that they do: different patterns of symptoms and levels of severity are likely to be associated with different demographic and clinical characteristics [7-9]. Thus, the current categorical approach to the diagnosis may not reflect what could be a potentially variable expression of the disorder: many disorders, including opioid dependence, may be heterogeneous in both nosologically and clinically meaningful ways. These differences may be important in understanding the course of the disorder and treatment response. Moreover, there is increasing evidence that there is a dimensional aspect associated with many mental disorders [10-13].
This raises a further empirical question of the most appropriate way to represent differences within the opioid dependence diagnosis. One possibility is that the diagnosis is continuous or dimensional and that the severity of opioid dependence is graded. For substance abuse and dependence, most factor analysis studies have found that the criteria form a single dimension [14-23].
A group of heterogeneous individuals may also be grouped into more homogenous classes by applying latent class models. Latent class analysis is a categorical approach which classifies individuals into more homogenous subgroups [24]. It has been used to examine patterns of dependence symptom endorsement and other variables for cannabis, alcohol and opioid analgesics [7, 9, 25, 26]. For both opioid analgesic dependence and cannabis use disorder, the latent class models were suggestive of a severity spectrum [9, 26].
A third possibility is that there are discrete classes of individuals and that within each class there is a dimensional trait that allows for within-class degrees of severity. This combination of classes and dimensions has only recently been examined through factor mixture models (otherwise known as hybrid models). The fit of these models can be compared with the fit of dimensional and latent class models using fit indices such as likelihood-based tests or information criteria [27, 28]. Such an approach has been used with alcohol, tobacco, and performance and image enhancing drugs (PIEDs). These studies have found that the factor mixture models provided the best fit when compared to dimensional and categorical models [29-32].
These different conceptualizations of substance use disorders have implications for research and clinical practice. Where a dimensional model provides a better fit than a categorical model, it can provide richer information [33]. Within a unidimensional structure it is possible to apply item response theory analysis to distinguish which criteria perform best in terms of discriminating those who have the disorder versus those who don't, and whether the criteria represent all levels of the severity spectrum. Such analysis has yielded useful information about the performance of substance abuse and dependence criteria in the lead up to DSM-V, [17-21, 34, 35] leading to the likely exclusion of the legal criterion from substance use disorders in DSM-V. However the application of a dimensional model to the diagnosis will not provide valid information if it is not in fact a dimensional construct.
Earlier research has not directly compared dimensional, categorical and hybrid models of opioid abuse and dependence criteria. If opioid abuse and dependence is best represented as a single latent severity trait, then increasing severity may be associated with other clinical outcomes. Alternatively, if a categorical model provides the best representation of the diagnosis and thus identifies more homogenous groups of individuals within the diagnosis, those groups will have more similar opioid dependence symptoms but also potentially different physical and mental health profiles [7, 25, 36]. Both models would provide important clinical information and phenotypes for research that are not available under the current diagnostic system. Therefore the aims of this paper are to:
Examine the structure of opioid abuse and dependence criteria within an opioid dependent treatment sample using latent class analysis, factor analysis and factor mixture modeling.
Examine the relationship between severity or sub-types of opioid dependence and other clinically relevant variables: other substance dependence diagnoses, mental health, suicide attempts, opioid overdose, and demographic characteristics. Examining the clinical covariates of opioid dependence is one way of externally validating the structure identified in the first part of the analysis (comparing categorical, dimensional and mixture models).
2. Method
2.1. Procedure
This study used data from the Comorbidity and Trauma Study, a retrospective case-control study examining genetic and environmental factors contributing to opioid dependence severity. The study was funded by the National Institute of Drug Abuse, and was run in collaboration with Washington University, the Queensland Institute of Medical Research, and the National Drug and Alcohol Research Centre (NDARC), University of New South Wales. Participants were recruited from opioid pharmacotherapy clinics in the greater Sydney area. Written informed consent was obtained from all participants. Ethics approval was obtained from the ethics committees of the University of New South Wales, Washington University, the Queensland Institute of Medical Research, and the area health service ethics committees governing the participating clinics. Participants were reimbursed AU$50.00 for out-of-pocket expenses.
2.2. Participants
Participants were recruited from 34 out of 35 available public and private opioid pharmacotherapy clinics in the greater Sydney region, New South Wales (NSW), between November 2005 and March 2008. Participating clinics were located in urban, suburban, regional and rural centres. An estimated 50% of opioid dependent persons in New South Wales are in opioid replacement therapy (ORT) at any one time [37]. Participants in ORT in New South Wales typically cycle in and out of treatment and many have tried several treatment modalities, including drug-free residential rehabilitation, and detoxification [38]. Before being accepted for ORT in NSW, individuals are assessed for opioid dependence. Respondents were eligible if they were aged 18 years or over; had an adequate understanding of English (in order to provide informed consent and participate in a long interview); and had participated in pharmacotherapy maintenance treatment for opioid dependence. Participants reporting recent suicidal intent or who were found to be psychotic were excluded from the study. A total of 1511 opioid dependent participants were interviewed. An estimated 5900 patients were dosing at the 35 ORT clinics in the greater Sydney area during the recruitment phase. Thus, the sample represents more than 25% of the available clinical population.
Most participants (86.1 per cent) were in treatment at the time of interview. The median age of initiation to heroin use was 18 years and the median age for first seeking treatment for opioid dependence was 24 years. The median duration of opioid dependence was 8 years. Males constituted 60.3 per cent of the sample (Table 1).
Table 1. Sample characteristics (socio-demographic, heroin use, substance dependence and mental health).
| Characteristics | Total (n=1511) |
|---|---|
| Mean age in years (SD) | 36.5 (8.5) |
| Sex (male %) | 60.3 |
| Unemployment % | 82.6 |
| Married/defacto % | 65.2 |
| 10 yrs education or less % | 70.6 |
| Mean age of first heroin use in years (SD) | 19.5 (5.6) |
| Mean days per month heroin use (SD) | 29.2 (3.3) |
| Lifetime opioid overdose % | 46.5 |
| Sedative dependence % | 36.3 |
| Stimulant dependence % | 49.8 |
| Cannabis dependence % | 55.5 |
| Cocaine dependence % | 31.9 |
| Alcohol dependence % | 39.8 |
| Nicotine dependence % | 64.3 |
| Depression % | 60.7 |
| PTSD# % | 37.9 |
| Panic disorder % | 25.8 |
| ASPD# % | 45.9 |
| BPD# % | 58.4 |
| Lifetime suicide attempt % | 31.9 |
PTSD = posttraumatic stress disorder; ASPD = antisocial personality disorder; BPD = borderline personality disorder
2.3. Structured interview
Each participant completed a 1.5 to 2.5 hour face-to-face structured interview. The diagnostic sections of the interview were based on the Semi-Structured Assessment of the Genetics of Alcoholism - Australia (SSAGA-OZ) and allow for lifetime DSM-IV and/or DSM-III-R diagnoses to be made for opioid abuse and dependence, alcohol, cannabis, sedative, stimulants, and cocaine abuse and dependence, nicotine dependence, post-traumatic stress disorder (PTSD), major depressive episode, panic disorder and antisocial personality disorder (ASPD) [39, 40]. A screener for borderline personality disorder (BPD) was adapted from the International Personality Disorder Examination (IPDE) [41]. Sections of the Christchurch Health and Development Study interview were modified to assess for childhood trauma and adult victimization history [42]. Childhood trauma items assessed sexual abuse and physical abuse and conflict between parents. Family history information was collected using the Family History Assessment Module (FHAM) and the Family History Screen (FHS) [43]. There was also an additional section on heroin use adapted from the SSAGA-OZ [39, 40]. Information was also collected on suicidality, heroin overdose, and heroin treatment history.
2.4. Statistical analysis
Confirmatory factor analysis (CFA), latent class analysis (LCA), and factor mixture models (FMM) were applied to the 11 DSM-IV opioid abuse and dependence criteria (Table 3). The models were also run without the legal criterion, since it is likely to be excluded from substance use disorders in DSM-V, in order to determine if this would make a difference to the latent structure of the diagnosis. Although the DSM-IV separates abuse from dependence, abuse and dependence criteria were included because many studies have found that in general population and other samples, substance abuse and dependence criteria form a unidimensional structure [15-17, 19, 21]. The abuse criteria were also included to provide more information and an improved ability to grade people on a continuum of severity. In the early stages of model development, exploratory factor analysis (EFA) is typically used instead of CFA to determine the number of factors that best fit the data. However, many studies over the past 20 years have confirmed that the substance abuse and dependence criteria form either one or two factors [14-23]. In the current analysis, one and two factor models were tested.
Table 3. factor loadings for 2 class 1 factor model, without covariates (n=1511).
| Criteria | Factor loading | Standard errors | p-value |
|---|---|---|---|
| Continue: Continued substance use despite having persistent or recurrent social or interpersonal problems caused/exacerbated by the effects of the substance | 0.95 | 0.002 | 0.03 |
| Role: Recurrent substance use resulting in a failure to fulfil major role obligations at work, school, or home | 0.51 | 0.22 | 0.01 |
| Legal: Recurrent substance-related legal problems | 0.81 | 0.13 | 0.00 |
| Hazard: Recurrent substance use in situations in which it is physically hazardous | 0.42 | 0.16 | 0.00 |
| Withdrawal: The characteristic withdrawal syndrome for the substance, or the same (or a closely related) substance is taken to relieve or avoid withdrawal symptoms | 0.43 | 0.17 | 0.00 |
| Tolerance: A need for markedly increased amounts of the substance to achieve intoxication or desired effect, or a markedly diminished effect with continued use of the same amount of the substance | 0.50 | 0.22 | 0.01 |
| Longer: The substance is often taken in larger amounts or over a longer period than was intended | 0.41 | 0.18 | 0.00 |
| Give up: Important social, occupational, or recreational activities are given up or reduced because of substance use | 0.63 | 0.24 | 0.02 |
| Time spent: A great deal of time is spent in activities necessary to obtain the substance, use the substance, or recover from its effects | 0.50 | 0.19 | 0.00 |
| Cut down: There is a persistent desire or unsuccessful efforts to cut down or control substance use | 0.48 | 0.17 | 0.00 |
| Harmful: The substance use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance | 0.38 | 0.15 | 0.00 |
Latent class analysis is a person centred approach which is aimed at categorizing individuals into groups where individuals are similar to one and another, and dissimilar across groups [24]. Individuals are classified on the basis of a number of observed variables: in this instance, their endorsement of opioid abuse and dependence criteria. Within each class, conditional item probabilities provide information on the probability of an individual in that class endorsing each item or criterion [28]. The current study tested latent class models with two to five classes.
Factor mixture models combine a categorical representation of the data with dimensional variation within each class [44]. The categorical latent variable identifies distinct groups in the population, and the dimensional latent variable (or the factor) is used to describe a continuum that exists within each class, for example, a severity continuum [28]. Models can have different numbers of classes and factors. In this analysis, factor mixture models with one to three classes were run. Conceptually, the 1 factor model can also be thought of as a 1 class, 1 factor model. To avoid confusion, the model will be referred to herein as a 1 class, 1 factor model. Models with one to three classes and one factor were tested: no further classes were added as the 3 class, 1 factor model was an inferior fit compared to the models with fewer classes.
A maximum likelihood estimator was used for all models. The Akaike Information Criterion (AIC), the Bayesian Information Criterion (BIC), the sample size-adjusted Bayesian Information Criterion (ABIC), and likelihood ratio tests (LRT) were used to choose the best model. AIC, BIC and ABIC are global fit indices which combine goodness of fit (log-likelihood value) and parsimony. A smaller value indicates better model fit. The bootstrap likelihood ratio test (BLRT) and the Lo Mendell Rubin likelihood ratio test (LMR-LRT) provide a p value which indicates whether the k-1 class model is rejected in favour of the k model [28]. Greater importance was given to the BIC and BLRT because they are typically more reliable than the AIC, and to a lesser extent, the ABIC and the Lo Mendell Rubin likelihood ratio test (LMR-LRT) [28]. Although classification quality is not a useful means of identifying the best fitting model, classification quality for the LCA and FMM was evaluated using entropy. Entropy is a summary indicator of classification quality and ranges from 0 to 1, with figures closer to 1 indicating higher classification quality [45].
FMM can be specified with class specific or class invariant parameters, such as factor loadings, means, variances, and item thresholds. Different levels of measurement invariance were tested for the 2 class, 1 factor model, including class specific thresholds, variances, means and loadings, and various combinations of these (for instance, class specific thresholds and loadings). In order to ensure that the model did not converge on local maxima, all 2 class, 1 factor models were run with 200 initial stage random sets of starting values, and 20 final stage optimizations. The best fitting FMM was subsequently run with 1000 initial stage random sets of starting values, 60 final stage optimizations and 60 initial stage iterations. The final stage solutions all had the same loglikelihood value, suggesting that the global maximum had been identified [45]. The model estimation terminated normally.
Subsequently, the 2 class, 1 factor mixture model was run with covariates, with class membership and the factor regressed on all covariates simultaneously. In Mplus, factor mixture modelling with covariates takes into account the uncertainty of group membership by using posterior class membership probabilities instead of taking class membership to be certain. A more conservative alpha level of p<0.01 was used to correct for testing multiple effects. The covariates were selected because the research literature indicates that they are associated with long-term opioid dependence: age, male sex, a measure of opioid use (times per day during heaviest period of use); suicide attempts; other substance dependence diagnoses; and mental health variables (depression, PTSD, ASPD and BPD) [1, 46-48]. Some variables (alcohol, nicotine and stimulant dependence, employment status, and panic disorder) were removed from the final model because they had not been significant in earlier models. All analyses were conducted in Mplus version 5.0 [49].
3. Results
3.1. Mental disorders and substance use characteristics
The average number of lifetime substance dependence diagnoses excluding opioids was two (SD 1.3). Lifetime prevalence ranged from 31.9% for cocaine dependence to 55.5% for cannabis dependence. Depression was the highest lifetime prevalence mental disorder at 60.7% (Table 1). The opioid abuse and dependence criteria were highly endorsed, with the lowest endorsement being 73% for legal problems, and the highest 97% for withdrawal.
3.2. Confirmatory factor, latent class and factor mixture model analysis
Latent class models were tested first. Of these, the best fitting were the 3 or 4 class models: the BIC indicated the 3 class model; the ABIC and LMR-LRT indicated the 4 class model (Table 2). However even the worst fitting factor mixture models were superior to the latent class models.
Table 2. Summary of results for latent class analysis and mixture model analysis (n = 1511).
| No of classes/ dimensions | 2 classes | 3 classes | 4 classes | 5 classes | 1 class 1 factor | 2 class 1 factor | 3 class 1 factor | 2 factor |
|---|---|---|---|---|---|---|---|---|
| AIC# | 10151 | 10073 | 10021 | 10007 | 10059 | 9996 | 9970 | 10054 |
| BIC# | 10273 | 10259 | 10291 | 10321 | 10176 | 10177 | 10215 | 10176 |
| ABIC# | 10200 | 10148 | 10122 | 10134 | 10106 | 10069 | 10069 | 10103 |
| Entropy | 0.78 | 0.80 | 0.75 | 0.79 | - | 0.51 | 0.38 | - |
| LMR-LRT# | 989*** | 101*** | 75** | 37 | - | 86** | 49 | - |
| BLRT# | 897*** | 102*** | 76*** | 38*** | - | 86*** | 50 | - |
| Free parameters | 23 | 35 | 47 | 59 | 22 | 34 | 46 | 23 |
AIC= Akaike information criterion; BIC= Bayesian information criterion; ABIC = sample size adjusted Bayesian information criterion; LMR-LRT= Lo- Mendell-Rubin likelihood ratio test, BLRT = Bootstrap likelihood ratio test.
p<0.01
p<0.001
A 2 factor model with abuse criteria loading onto one factor and dependence criteria loading onto a second factor was rejected because the goodness of fit criteria (AIC, BIC and ABIC) were almost identical to the 1 class, 1 factor model, and the correlation between the two factors was high (0.91), suggesting that a 1 class, 1 factor model was a more parsimonious solution. Having ruled out the 2 factor model, likelihood ratio tests confirmed that the 2 class, 1 factor model was marginally superior to the other factor mixture models and to the latent class models. Overall, the 2 class, 1 factor model appeared to provide the best fit. Although the BIC for the 1 class, 1 factor model and the 2 class, 1 factor model was very similar, the bootstrap and LMR likelihood ratio tests indicated that the 2 class, 1 factor model was a superior fit to the 1 class, 1 factor model, but that adding a third class did not improve model fit (Table 2). When the legal criterion was excluded from the analysis, the 2 class, 1 factor model remained the best fitting model. The results shown in Table 2 pertain to the models that included all 11 abuse and dependence criteria.
The 2 class, 1 factor model with class specific item thresholds and class invariant factor loadings, means and variances proved the best fit when comparing levels of measurement invariance. The 2 class, 1 factor model was either not identified or did not converge when thresholds and factor means were class specific or when variances and thresholds were class specific. All other models converged, albeit with an increased number of random starts and final stage optimizations.
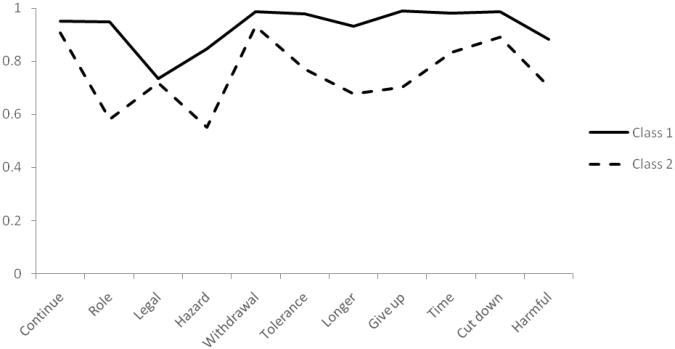
Class 1 (74% of the sample) had higher endorsement probabilities on most criteria than class 2 (26% of the sample) (Figure 1). The two classes differed on role, hazard, tolerance, longer, give up, time, cut down, and harmful. The differences in endorsement probabilities were reflected in the item thresholds which were different across classes, with class 1 having lower thresholds than class 2 on all criteria except continue and legal. Factor loadings on most criteria were moderate to high (Table 3), with continue having the highest loading, and harmful the lowest.
Figure 1. Criteria endorsement probabilities for class 1 (74%) and class 2 (26%), n=1511.
3.3. The relationship between opioid abuse and dependence and other clinical variables
Significant covariates of class membership were ASPD, cocaine dependence, sedative dependence, and non-fatal opioid overdose (Table 4). Significant covariates of the factor were BPD, cannabis dependence, cocaine dependence, and non-fatal opioid overdose. Including covariates in the 2 class, 1 factor model improved entropy to 0.79 (from 0.51), indicating that participants were more precisely classified once the covariates were taken into consideration. The proportion of participants in each class changed very slightly once the covariates were included: class one was 72%, and class two was 28% of the sample.
Table 4. Relationship between selected covariates and best fitting mixture model (2 class, 1 factor) (n=1511).
| Covariate | Class 1 (n=1120) | Class 2 (n=390) | Class regressed onto covariates: OR (95% CI)1. | Factor regressed onto covariates: β (SE)2. |
|---|---|---|---|---|
| Sex (male) % | 67 | 45 | 0.98 (0.95-1.01) | -0.02 (0.11) |
| Depression % | 62 | 56 | 0.72 (0.41-1.24) | 0.25 (0.15) |
| BPD % | 65 | 41 | 0.97 (0.51-1.88) | 0.47 (0.18)** |
| ASPD % | 54 | 25 | 2.05 (1.22-3.45) *** | 0.06 (0.10) |
| Cannabis dependence % | 61 | 41 | 1.08 (0.59-1.98) | 0.62 (0.10)*** |
| Sedative dependence % | 45 | 14 | 1.99 (1.12-3.53) ** | 0.21 (0.12) |
| Cocaine dependence % | 41 | 10 | 2.47 (1.22-5.02) *** | 0.39 (0.14)** |
| Non-fatal opioid overdose % | 28 | 12 | 3.53 (1.38-9.04) *** | 0.40 (0.12)** |
| Suicide attempts % | 22 | 16 | 0.69 (0.32-1.50) | 0.09 (0.07) |
| Times per day opioid use | 2.9 | 2.2 | 1.55 (0.96-2.49) | 0.01 (0.01) |
p<0.01
p<0.001
OR = odds ratio, CI = confidence interval, SE = standard error
Odds ratios represent the odds of covariate in class 2 compared to class 1.
Beta coefficients represent the mean change (increase or decrease) in the severity dimension in standard deviation units associated with the covariate.
4. Discussion
This is the first study to compare categorical, continuous and mixed models of opioid abuse and dependence in a large opioid dependent sample. Findings suggest that individuals with opioid abuse and dependence are best represented as two separate classes with within-class variation of severity.
This study provides preliminary evidence that the proposed DSM-V opioid use disorder distinction between moderate and severe dependence is valid. Further, the classes are clearly distinguished from each other by other externalizing disorders and multiple opioid overdoses. The association between opioid dependence and other externalizing disorders is consistent with the occurrence of a range of externalizing problems along a continuum [10, 11, 50-52]. As such, increasing severity of one externalizing disorder increases the chances of having other externalizing disorders [11]. The more severe class 1 had an increased risk of meeting criteria for sedative and cocaine dependence, and antisocial personality disorder, as well as experiencing multiple non-fatal opioid overdoses. Removing cocaine and sedative dependence from the model did result in cannabis dependence but not alcohol, nicotine or stimulant dependence, becoming significantly associated with class membership. However, in the final model cannabis dependence did not differ with respect to class membership, perhaps suggesting that cocaine and sedative dependence are better indicators of more severe polydrug dependence. The inclusion of the covariates demonstrates the usefulness of factor mixture modeling, as several covariates were also associated with within-class severity. Interestingly, although BPD and cannabis dependence were not significantly associated with class membership, they did vary within class according to severity.
Given the high levels of criteria endorsement, long-term opioid dependence and other substance dependence observed in this sample it is likely that these participants represent the most severe end of the spectrum. As such, it is not surprising to find such high levels of co-occurring substance dependence and ASPD. Nevertheless, the prevalence of internalizing disorders in the current study was also high and these disorders were not associated with membership of the more severely dependent group; nor did they vary within class as severity increased. Given this, one might speculate that there are different determinants of internalizing and externalizing problems in this population. Nonetheless Krueger and others have found that there is considerable correlation between the externalizing and internalizing dimensions [10, 11, 50].
4.1 Implications
The variations in severity noted within this treatment sample and the problems associated with increasing severity of opioid dependence highlight the importance of distinguishing between more and less severely dependent individuals in a clinical setting. There are scales available to assess severity of opiate and other dependence (for instance, the Severity of Dependence Scale) [53]. The proposed substance use disorders category in DSM-V uses a symptom count to specify severity, and recent evidence suggests that although not all criteria are equal in terms of their capacity to measure severity, criteria counts are a reasonable proxy for severity [54]. Whichever approach is used, a broader conceptualization of opioid dependence which recognizes the increasing risk of other externalizing disorders as severity of opioid dependence increases makes sense from both a clinical and research perspective. In addition to a greater number of substance dependence diagnoses and personality disorders, increasing severity both across and within classes greatly increased the risk of opioid overdose, most likely due to greater opioid and other drug use [55]. Overdose is an independent risk factor for cognitive impairment which in turn has implications for problem solving, behavioral disinhibition, capacity to comply with treatment, and poorer functioning across several other domains [56].
4.2 Limitations
It is worth noting several limitations to the current study. The use of a treatment sample means firstly that the results may not be generalizable to those opioid users who have never been in treatment. All the same, there is evidence that most opioid dependent individuals in Australia have been in treatment at some point [1, 37]. Secondly, using a dependent sample means that the abuse and dependence data is restricted in range, which may be biased towards lesser order factor solutions [57]. The same analysis on a general population sample may yield different models. However because of the low population prevalence of opioid dependence, applying this analysis to a general population sample would require a larger sample size than is currently available. A further limitation is that the participants were predominantly heroin dependent, not opioid analgesic dependent. Differences between these two groups may mean that different subtypes and associations exist amongst opioid analgesic users [58]. Nevertheless, there may be significant overlap between the two groups, with almost half of IDU in one survey having injected morphine [59].
4.3 Conclusions
This study provides preliminary evidence that the proposed DSM-V opioid use disorder distinction between moderate and severe dependence is valid. Further, the distinction has clear implications for other clinical problems, particularly externalizing disorders and opioid overdose. However, it is important to acknowledge that although class 2 had a lower prevalence of externalizing disorders, both classes exhibited high levels of Axis I and Axis II disorders, suicidality and non-fatal overdose. Finally, given the co-occurrence of opioid dependence with other externalizing disorders, research and treatment should be framed within an externalizing spectrum.
Acknowledgments
This study was funded by NIDA (Grant No. 5 R01 DA017305-02). The authors thank the treatment agencies and the research participants for their support of this study. We also thank Elizabeth Conroy, Elizabeth Maloney, Michelle Torok, Caitlin McCue and Cherie Kam for assistance with data collection. Finally, thank you to Richard Mattick of NDARC and to the collaborating research centres.
Footnotes
Conflict of interest declaration: Louisa Degenhardt received an untied educational grant from Reckitt Benckiser to examine the extent of misuse, diversion and injection of buprenorphine-naloxone in Australia, 2006-2008. The design, conduct, interpretation and reporting of the post-marketing surveillance studies' findings were determined by the study investigators; the funder had no role in these. The funder also had no role in or knowledge of the conception and writing of this particular manuscript. We declare that we have no conflict of interest.
References
- 1.Ross J, et al. The characteristics of heroin users entering treatment: findings from the Australian Treatment Outcome Study (ATOS) Drug and Alcohol Review. 2005;24:411–418. doi: 10.1080/09595230500286039. [DOI] [PubMed] [Google Scholar]
- 2.Craddock SG, Rounds-Bryant JL, Flynn PM, Hubbard RL. Characteristics and pretreatment behaviors of clients entering drug abuse treatment: 1969 to 1993. American Journal of Drug and Alcohol Abuse. 1997;23(1):43–60. doi: 10.3109/00952999709001686. [DOI] [PubMed] [Google Scholar]
- 3.Fischer B, Firestone Cruz M, Rehm J. Illicit opioid use and its key characteristics: a select overview and evidence from a Canadian multisite cohort of illicit opioid users (OPICAN) Canadian Journal of Psychiatry - Revue Canadienne de Psychiatrie. 2006;51(10):624–634. doi: 10.1177/070674370605101002. [DOI] [PubMed] [Google Scholar]
- 4.Fergusson DM, Boden JM, Horwood LJ. The developmental antecedents of illicit drug use: Evidence from a 25-year longitudinal study. Drug and Alcohol Dependence. 2008;96:165–177. doi: 10.1016/j.drugalcdep.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 5.American Psychological Association. Diagnostic and Statistical Manual of Mental Disorders. 4th. Washington, DC: American Psychiatric Press; 1994. [Google Scholar]
- 6.Krueger RF, Watson D, Barlow DH. Introduction to the special section: toward a dimensionally based taxonomy of psychopathology. Journal of Abnormal Psychology. 2005;114(4):491–3. doi: 10.1037/0021-843X.114.4.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moss HB, Chen CM, Yi H. Empirical subtyping of alcohol dependence in a nationally representative sample: A latent class analysis. Alcoholism: Clinical and Experimental Research. 2006;30(6):166A–166A. [Google Scholar]
- 8.McCutcheon VV, et al. Alcohol criteria endorsement and psychiatric and drug use disorders among DUI offenders: Greater severity among women and multiple offenders. Addictive Behaviors. 2009;34:432–439. doi: 10.1016/j.addbeh.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ghandour LA, Martins HD, Chilcoat HD. Understanding the patterns and distribution of opioid analgesic dependence symptoms using a latent empirical approach. Journal of Methods in Psychiatric Research. 2008;17(2):89–103. doi: 10.1002/mpr.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vollebergh WA, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders: the NEMESIS study. Archives of General Psychiatry. 2001;58(6):597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- 11.Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56(10):921–6. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- 12.Krueger RF, Markon KE, Patrick CJ, Iacono WG. Externalizing psychopathology in adulthood: a dimensional-spectrum conceptualization and its implications for DSM-V. Journal of Abnormal Psychology. 2005;114(4):537–50. doi: 10.1037/0021-843X.114.4.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hasin DS, Liu X, Alderson D, Grant BF. DSM-IV alcohol dependence: a categorical or dimensional phenotype? Psychological Medicine. 2006;36(12):1695–705. doi: 10.1017/S0033291706009068. [DOI] [PubMed] [Google Scholar]
- 14.Kirisci L, Tarter RE, Vanyukov M, Martin C, Mezzich A, Brown S. Application of item response theory to quantify substance use disorder severity. Addictive Behaviors. 2006;31(6):1035–1049. doi: 10.1016/j.addbeh.2006.03.033. [DOI] [PubMed] [Google Scholar]
- 15.Proudfoot H, Baillie AJ, Teesson M. The structure of alcohol dependence in the community. Drug and Alcohol Dependence. 2006;81(1):21–26. doi: 10.1016/j.drugalcdep.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 16.Teesson M, Lynskey M, Manor B, Baillie A. The structure of cannabis dependence in the community. Drug and Alcohol Dependence. 2002;68(3):255–262. doi: 10.1016/s0376-8716(02)00223-5. [DOI] [PubMed] [Google Scholar]
- 17.Gillespie NA, Neale MC, Prescott CA, Aggen SH, Kendler KS. Factor and item-response analysis DSM-IV criteria for abuse of and dependence on cannabis, cocaine, hallucinogens, sedatives, stimulants and opioids. Addiction. 2007;102(6):920–930. doi: 10.1111/j.1360-0443.2007.01804.x. [DOI] [PubMed] [Google Scholar]
- 18.Hartman CA, et al. Item response theory analysis of DSM-IV cannabis abuse and dependence criteria in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47(2):165–173. doi: 10.1097/chi.0b013e31815cd9f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Langenbucher JW, et al. An application of Item Response Theory analysis to alcohol, cannabis and cocaine criteria in DSM-IV. Journal of Abnormal Psychology. 2004;113(1):72–80. doi: 10.1037/0021-843X.113.1.72. [DOI] [PubMed] [Google Scholar]
- 20.Martin CS, Chung T, Kirisci L, Langenbucher JW. Item response theory analysis of diagnostic criteria for alcohol and cannabis use disorders in adolescents: Implications for DSM-V. Journal of Abnormal Psychology. 2006;115(4):807–814. doi: 10.1037/0021-843X.115.4.807. [DOI] [PubMed] [Google Scholar]
- 21.Lynskey MT, Agrawal A. Psychometric properties of DSM assessments of illicit drug abuse and dependence: results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Psychological Medicine. 2007;37(9):1345–55. doi: 10.1017/S0033291707000396. [DOI] [PubMed] [Google Scholar]
- 22.Blanco C, Harford TC, Nunes E, Grant B, Hasin D. The latent structure of marijuana and cocaine use disorders: Results from the National Longitudinal Alcohol Epidemiologic Survey (NLAES) Drug & Alcohol Dependence. 2007;91:91–96. doi: 10.1016/j.drugalcdep.2007.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nelson CB, Rehm J, Bedirhan U, Grant B, Chatterji S. Factor structures for DSM-IV substance disorder criteria endorsed by alcohol, cannabis, cocaine and opiate users: results from the WHO validity and reliability study. Addiction. 1999;94(843-855) doi: 10.1046/j.1360-0443.1999.9468438.x. [DOI] [PubMed] [Google Scholar]
- 24.Lazarsfeld P, Henry N. Latent structure analysis. New York: Houghton-Mifflin; 1968. [Google Scholar]
- 25.Banta-Green CJ, Merrill JO, Doyle SR, Boudreau DM, Calsyn DA. Opioid use behaviors, mental health and pain - Development of a typology of chronic pain patients. Drug and Alcohol Dependence. 2009;104:34–42. doi: 10.1016/j.drugalcdep.2009.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grant JD, Scherrer JF, Neuman RJ, Todorov AA, Price RK, Bucholz KK. A comparison of the latent class structure of cannabis problems among adult men and women who have used cannabis repeatedly. Addiction. 2006;101(8):1133–1142. doi: 10.1111/j.1360-0443.2006.01463.x. [DOI] [PubMed] [Google Scholar]
- 27.Muthen B. Should substance use disorders be considered as categorical or dimensional? Addiction. 2006;101(1):6–16. doi: 10.1111/j.1360-0443.2006.01583.x. [DOI] [PubMed] [Google Scholar]
- 28.Nylund KJ, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Structural Equation Modeling. 2007;14:535–569. [Google Scholar]
- 29.Kuo PH, Aggen SH, Prescott CA, Kendler KS, Neale MC. Using a factor mixture modeling approach in alcohol dependence in a general population sample. Drug and Alcohol Dependence. 2008;98:105–114. doi: 10.1016/j.drugalcdep.2008.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Muthén B, Asparouhov T. Item response mixture modeling: Application to tobacco dependence criteria. Addictive Behaviors. 2006;31(6):1050–1066. doi: 10.1016/j.addbeh.2006.03.026. [DOI] [PubMed] [Google Scholar]
- 31.Muthén BO. Should substance use disorders be considered as categorical or dimensional? Addiction. 2006;101(s1):6–16. doi: 10.1111/j.1360-0443.2006.01583.x. [DOI] [PubMed] [Google Scholar]
- 32.Hildebrandt T, Langenbucher JW, Carr SJ, Sanjuan P. Modeling population heterogeneity in appearance-and performance-enhancing drug (APED) use: Applications of mixture modeling in 400 regular APED users. Journal of Abnormal Psychology. 2007;116(4):717–733. doi: 10.1037/0021-843X.116.4.717. [DOI] [PubMed] [Google Scholar]
- 33.Krueger RF, et al. Using latent trait modeling to conceptualize an alcohol problems continuum. Psychological Assessment. 2004;16(2):107–19. doi: 10.1037/1040-3590.16.2.107. [DOI] [PubMed] [Google Scholar]
- 34.Saha TD, Chou SP, Grant BF. Toward an alcohol use disorder continuum using item response theory: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine. 2006;36(7):931–941. doi: 10.1017/S003329170600746X. [DOI] [PubMed] [Google Scholar]
- 35.Gilder DA, Lau P, Ehlers CL, Gilder DA, Lau P, Ehlers CL. Item response theory analysis of lifetime cannabis-use disorder symptom severity in an American Indian community sample. Journal of Studies on Alcohol & Drugs. 2009;70(6):839–49. doi: 10.15288/jsad.2009.70.839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Moss HB, Chen CM, Yi HY. Subtypes of alcohol dependence in a nationally representative sample. Drug & Alcohol Dependence. 2007;91(2-3):149–58. doi: 10.1016/j.drugalcdep.2007.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ritter A, Chalmers J. Polygon: The many sides to the Australian opioid pharmacotherapy maintenance system; ANCD Research Paper #18; 2009; Canberra. Sydney: Australian National Council on Drugs; [Google Scholar]
- 38.Ross J, et al. The characteristics of heroin users entering treatment: findings from the Australian treatment outcome study (ATOS) Drug & Alcohol Review. 2005;24(5):411–8. doi: 10.1080/09595230500286039. [DOI] [PubMed] [Google Scholar]
- 39.Bucholz KK, Cadoret R, Cloninger RC, Dinwiddie SH, Hesselbrock VM, Nurnberger JI. A new, semi-structured psychiatric interview for use in genetic linkage studies: A report on the reliability of SSAGA. Journal of Studies on Alcohol. 1994;55:149–158. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- 40.Hesselbrock M, Easton C, Bucholz KK, Schuckit M, Hesselbrock V. A validity study of the SSAGA - a comparison with the SCAN. Addiction. 1999;94(9):1361–1370. doi: 10.1046/j.1360-0443.1999.94913618.x. [DOI] [PubMed] [Google Scholar]
- 41.Loranger AW, Sartorius N, Andreoli A, Berger P, Buchheim P, Channabasavanna SM, et al. The International Personality Disorder Examination: The World Health Organization/Alcohol, Drug Abuse, and Mental Health Administration International Pilot Study of Personality Disorders. Archives of General Psychiatry. 1994;51(3):215–224. doi: 10.1001/archpsyc.1994.03950030051005. [DOI] [PubMed] [Google Scholar]
- 42.Fergusson D, Horwood L, Shannon F, Lawton J. The Christchurch Child Development Study: A review of epidemiological findings. Paedatric and Perinatal Epidemiology. 1989;3:302–325. doi: 10.1111/j.1365-3016.1989.tb00382.x. [DOI] [PubMed] [Google Scholar]
- 43.Weissman MM, Wickramaratne P, Adams P, Wolk S, Verdeli H, Olfson M. Brief screening for family psychiatric history: the family history screen. Archives of General Psychiatry. 2000;57(7):675–82. doi: 10.1001/archpsyc.57.7.675. [DOI] [PubMed] [Google Scholar]
- 44.Lubke GH, Muthen B. Investigating population heterogeneity with factor mixture models. Psychological Methods. 2005;10(1):21–39. doi: 10.1037/1082-989X.10.1.21. [DOI] [PubMed] [Google Scholar]
- 45.Muthen B. Mplus Technical Appendices. Muthen & Muthen; Los Angeles, CA: 1998-2004. [Google Scholar]
- 46.Hser YI, Huang B, Chou CP, anglin MD. Trajectories of heroin addiction: Growth Mixture Modeling results based on a 33-year follow-up study. Evaluation Review. 2007;31:548–563. doi: 10.1177/0193841X07307315. [DOI] [PubMed] [Google Scholar]
- 47.Fischer B, et al. Illicit opioid use in Canada: comparing social, health, and drug use characteristics of untreated users in five cities (OPICAN study) Journal of Urban Health. 2005;82(2):250–66. doi: 10.1093/jurban/jti049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bargarli AM, et al. VedeTTE, a longitudinal study on effectiveness of treatments for heroin addiction in Italy: Study protocol and characteristics of study population. Substance Use & Misuse. 2006;41(14):1861–1879. doi: 10.1080/10826080601025482. [DOI] [PubMed] [Google Scholar]
- 49.Muthén LK, Muthén BO. Mplus User's Guide. Fifth. Los Angeles, CA: Muthén & Muthén; 1998-2007. [Google Scholar]
- 50.Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): a longitudinal-epidemiological study. Journal of Abnormal Psychology. 1998;107(2):216–27. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- 51.Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, and personality: an integrative quantitative model of the adult externalizing spectrum. Journal of Abnormal Psychology. 2007;116(4):645–66. doi: 10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Markon KE, Krueger RF. Categorical and continuous models of liability to externalizing disorders: a direct comparison in NESARC. Archives of General Psychiatry. 2005;62(12):1352–9. doi: 10.1001/archpsyc.62.12.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gossop M, et al. The Severity of Dependence Scale (SDS): psychometric properties of the SDS in English and Australian samples of heroin, cocaine and amphetamine users. Addiction. 1995;90(5):607–14. doi: 10.1046/j.1360-0443.1995.9056072.x. [DOI] [PubMed] [Google Scholar]
- 54.Hasin DS, Beseler CL. Dimensionality of lifetime alcohol abuse, dependence and binge drinking. Drug & Alcohol Dependence. 2009;101(1-2):53–61. doi: 10.1016/j.drugalcdep.2008.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Darke S, Ross J, Hall W. Overdose among heroin users in Sydney, Australia: prevalence and correlates of non-fatal overdose. Addiction. 1996;91:405–411. [PubMed] [Google Scholar]
- 56.Darke S, Sims J, McDonald S, Wickes W. Cognitive impairment among methadone maintenance patients. Addiction. 2000;95(5):687–95. doi: 10.1046/j.1360-0443.2000.9556874.x. [DOI] [PubMed] [Google Scholar]
- 57.Nelson CB, Rehm J, Üstün TB, Grant B, Chatterji S. Factor structures for DSM-IV substance disorder criteria endorsed by alcohol, cannabis, cocaine and opiate users: Results from the WHO reliability and validity study. Addiction. 1999;94(6):843–855. doi: 10.1046/j.1360-0443.1999.9468438.x. [DOI] [PubMed] [Google Scholar]
- 58.Subramaniam GA, Stitzer M. Clinical characteristics of treatment-seeking prescription opioid vs. heroin-using adolescents with opioid use disorder. Drug & Alcohol Dependence. 2009;101:13–19. doi: 10.1016/j.drugalcdep.2008.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Degenhardt L, et al. Trends in morphine prescriptions, illicit morphine use and associated harms among regular injecting drug users in Australia. Drug and Alcohol Review. 2006;25(5):403–12. doi: 10.1080/09595230600868504. [DOI] [PubMed] [Google Scholar]