Abstract
Purpose
To investigate the prevalence of osteoarthritic changes and condylar positioning of the temporomandibular joint (TMJ) in Korean children and adolescents with or without temporomandibular disorders (TMDs).
Materials and Methods
A total of 101 asymptomatic and 181 symptomatic children and adolescents aged 10 to 18 years old were included in the study. Osteoarthritic changes such as flattening, sclerosis, osteophytes, or erosion, and the parasagittal positioning of the condyle were assessed using cone-beam computed tomography (CBCT) images.
Results
The overall prevalence of osteoarthritic changes was higher in symptomatic (26.8%) than in asymptomatic adolescents (9.9%) (p<0.05). In the symptomatic group, the frequency was higher in males (33.3%) than in females (23.0%) (p<0.05). Erosion was the most common change for the symptomatic group (15.6%), whereas sclerosis was the most common change for the asymptomatic group (5.4%). Posterior condylar position was more frequently observed in the symptomatic group (p<0.05). Erosion was more common in the samples with TMJ pain or mouth opening limitations as compared to those without them (p<0.05).
Conclusion
This study showed that osteoarthritic changes in TMJ were common in children and adolescents, with a much higher prevalence in symptomatic patients.
Keywords: Adolescent, Temporomandibular Joint, Cone-Beam Computed Tomography
Introduction
Temporomandibular joint (TMJ) disorders are common problems among children and adolescents. Their incidence has been reported as being between 6% and 68% in previous studies.1-5 Radiographic examination may serve to provide additional information along with clinical findings. Despite the high incidence of TMJ dysfunction in children and adolescents, radiographic studies have rarely been carried out. It has been reported that osteoarthritis of the TMJ is an age-related change and is more frequent in older persons than in younger persons.6,7 However, a study reported that the pediatric age group with TMJ pain and dysfunction showed evidence of degenerative arthritis in 37% of cases.8 Osteoarthritis (OA) of the TMJ in children might potentially have an effect on mandibular growth and lead to an altered skeletal structure.9 Therefore, attention should be paid to any osteoarthritic changes in the TMJ in children.
The clinical significance of condylar positioning in the glenoid fossa is controversial. It seems that TMJ disorder (TMD) patients are more likely to have posterior condylar positioning.10-13 However, some investigators have suggested no significant association between condylar positioning and clinical or radiographic findings.14-18
This study was performed to assess the prevalence of osteoarthritic changes and the parasagittal condylar positioning of TMJ in children and adolescents with or without TMJ symptoms.
Materials and Methods
Subjects
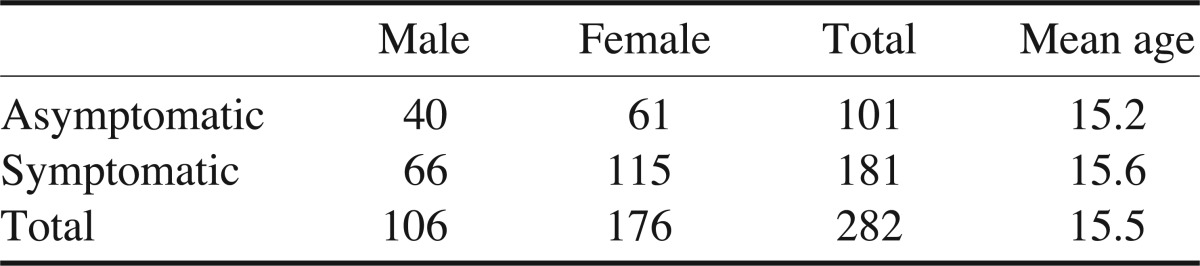
We retrospectively reviewed the data of 10- to 18-year-old patients who underwent cone beam computed tomography (CBCT) images in our hospital between October 2009 and March 2011, and collected 181 symptomatic and 101 asymptomatic patients (Table 1). The symptomatic group consisted of 66 males and 115 females who presented for the treatment of TMDs. A clinical examination was performed to assess the presence of mouth opening limitation, pain, and TMJ noise in each patient. A maximum opening under 40 mm was considered to be limited mouth opening. TMJ pain was assessed by asking the patient if he or she felt joint or muscle pain during mandibular function. TMJ noise was based on either crepitation or a clicking sound.
Table 1.
Gender and age distribution of patients included in the study
The asymptomatic group was composed of 40 males and 61 females who had no TMJ signs or symptoms. All of them had undergone CBCT scans for the thorough examination of tooth impaction or an orthodontic evaluation.
In both groups, the patients who had any conditions that could affect TMJ components such as skeletal abnormalities, TMJ tumors, or other infectious disease were excluded.
Methods
CBCT scans were obtained with PaX-Zenith3D (Vatech, Kihung, Korea) in the maximal intercuspal position, with a rotation of 360 degrees for data acquisition. The exposure factors were a 24×19 cm field of view, 120 kVp, 5-6 mA, and a 24 seconds exposure time. Images were reconstructed using a high spatial frequency reconstruction algorithm immediately after acquisition, and the acquired image data consisted of a 14-bit scale with a 0.3mm3 voxel size. For interpretation, real-time reconstruction was performed using an Ez3D 2009 3D image viewer (Vatech, Kihung, Korea), and the axial, coronal, and sagittal two-dimensional (2D) multi-planar reformatted slices were provided.
Two experienced oral and maxillofacial radiologists independently assessed the images on Coronis 5MP monitors (Barco, Brussels, Belgium 2,048×2,560 image matrices, 10-bit viewable gray scale, and 145.9-ft-lambert luminescence). Interpretation was made using a combination of all three plane images via an interactive multi-planar display. They were allowed to adjust the window width, window level, and magnification. No demographic data or clinical features were available to them.
Radiographic osteoarthritic changes of flattening, sclerosis, osteophytes, and erosion for both the temporal part and condyle of the TMJ were evaluated.
The criteria were as follows: flattening-a loss of the round contour of the condyle at the load bearing area, sclerosis-an increased density of the cortical lining or the subchondral bone, osteophyte-a marginal bone outgrowth, and erosion-an interruption or absence of the cortical lining.
Parasagittal condylar positioning was assessed in accordance with the method of Pullinger and Hollender,19 suggesting linear measurement of the subjective closest anterior and posterior interarticular space (Fig. 1). Parasagittal plane perpendicular to the long axis of the condyle on axial plane was created and the image passing through the center was used to evaluate condylar positioning. The values of the narrowest anterior (A) and posterior (P) interarticular space were transferred to the following formula from Pullinger et al.10
Fig. 1.
Linear measurement of anterior (A) and posterior (P) subjective closest joint spaces.
(P-A) / (P+A)×100
The position was expressed as a percentage of the anterior or posterior displacement from absolute concentricity (zero). The range of ±12% was considered to be concentric. Values smaller than -12 indicated that the condyle was in a posterior position, and values greater than +12 indicated that the condyle was in an anterior position.
Statistical analysis
First, we calculated the interobserver agreement by using Cohen's kappa coefficient,20 which showed substantial agreement (k=0.67). Then, the two observers discussed the disagreed-upon cases together and reached an agreement. We used these results for further statistical analysis.
A comparison was carried out to evaluate differences between the asymptomatic and the symptomatic groups. Additionally, gender and age differences were analyzed within each group. For the symptomatic group, differences in the clinical variables of mouth opening limitation, TMJ pain, and noise were assessed. The statistical analysis was performed using χ2 test and the Fisher exact test. The level of statistical significance was set at .05. The calculations were performed with PASW Statistics 18 (SPSS Inc., Chicago, IL, USA).
Results
The occurrence of osteoarthritic change was much higher in the symptomatic group (26.8%) than in the asymptomatic group (9.9%), showing a significantly higher prevalence of sclerosis, osteophytes, and erosion in the symptomatic group (p<0.05) (Fig. 2). The concentric condylar position was most common in the asymptomatic group (72.3%), while posterior positioning of the condyle was dominant in the symptomatic group (52.8%) (p<0.05) (Fig. 2).
Fig. 2.
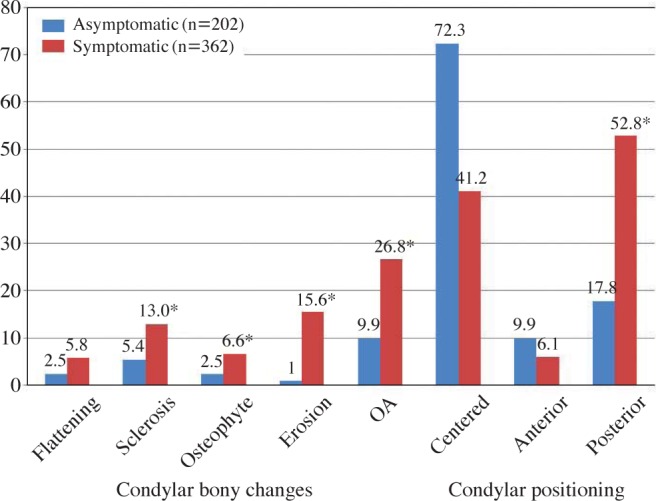
Comparison of osteoarthritic changes of TMJs and parasagittal positioning of the condyles between the asymptomatic and the symptomatic groups.
*statistically significant difference between asymptomatic and symptomatic groups (p<0.05)
OA: one or more osteoarthritic changes of flattening, sclerosis, osteophyte, or erosion
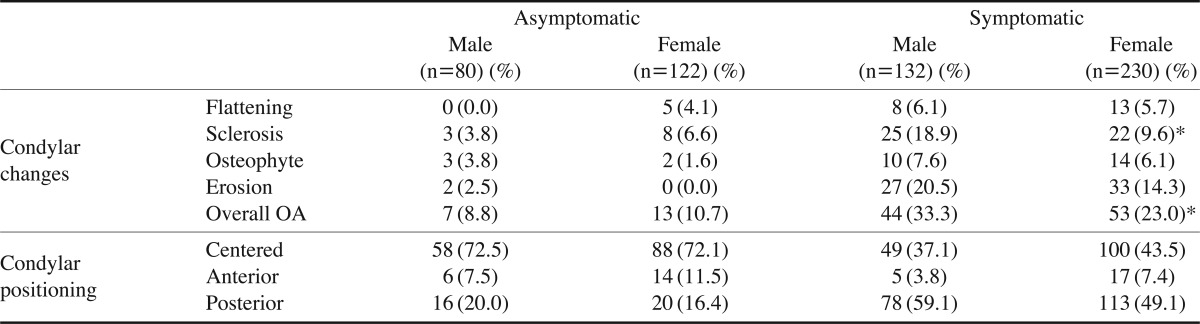
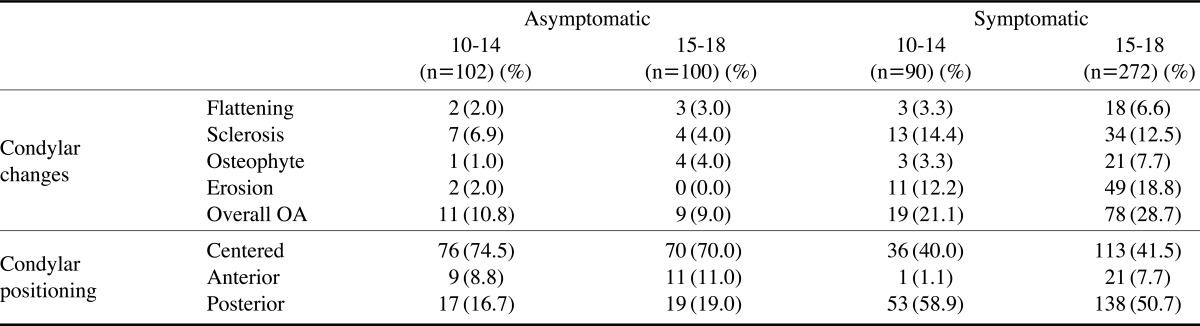
Gender differences were found in the symptomatic group; sclerosis and overall osteoarthritic changes were more frequently observed in males than in females (p<0.05) (Table 2). In both the asymptomatic and symptomatic groups, there were no significant differences between the two age groups of 10 to 14 and 15 to 18 (Table 3).
Table 2.
Prevalence of osteoarthritic changes of TMJs and parasagittal positioning of the condyles by gender
*statistically significant difference between two gender groups (p<0.05)
Overall OA: one or more osteoarthritic changes of flattening, sclerosis, osteophyte, or erosion
Table 3.
Prevalence of osteoarthritic changes of TMJs and parasagittal positioning of the condyles by age group
Overall OA: one or more osteoarthritic changes of flattening, sclerosis, osteophyte, or erosion
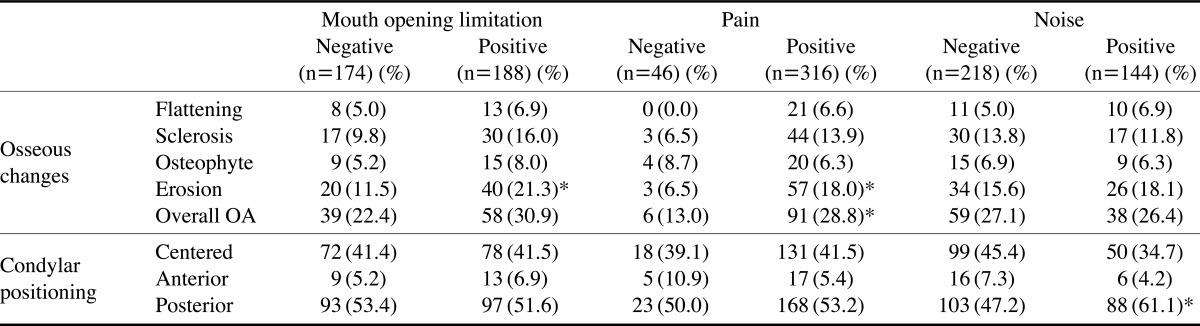
In relation to the clinical findings, the patients with mouth opening limitation or TMJ pain showed more erosion than those without them (p<0.05). TMJ noise showed a statistically significant difference in terms of condylar positioning; posterior positioning of the condyle was observed more often in cases of TMJ noise (p<0.05) (Table 4).
Table 4.
Prevalence of osteoarthritic changes of TMJs and parasagittal positioning of the condyles according to clinical features
*statistically significant difference between negative and positive groups (p<0.05)
Overall OA: one or more osteoarthritic changes of flattening, sclerosis, osteophyte, or erosion
Discussion
CBCT is an excellent imaging modality for the assessment of bony TMJ components.21,22 It provides 2D multi-planar reformatted images with submillimeter spatial resolution and allows the observer to customize the slices interactively by using a volumetric data set. Honey et al23 reported that CBCT images gave superior reliability and great accuracy in evaluating the TMJ, and when the observers interpreted the images through an interactive display, the diagnostic accuracy was much higher than that achieved through static captured images. In this study, the observers were allowed to access the volumetric data and evaluate osteoarthritic changes by scrolling the multi-planar images interactively.
TMJ osteoarthritis is very common in adults. The radiographic changes corresponding to osteoarthritis can be observed in 12-44% of the general adult population.1,24 However, aging is not the crucial factor in the pathogenesis of osteoarthritis.25 Our results show that TMJ osteoarthritis is also common among children and adolescents. In the asymptomatic group, the prevalence was 9.9%, comparable to that of Petrikowski and Grace's study.26 They reported that the overall occurrence of TMJ radiographic abnormalities in preorthodontic patients was 6.9% in the 9 to 11 age group and 7.5% in the 12 to 15 age group.
In the symptomatic group, the prevalence of TMJ osteoarthritis was 26.8%, being significantly higher than that of the asymptomatic group. Sanchez-Woodworth et al8 studied pediatric patients (7 to 16 years) with TMJ pain and dysfunction and indicated that 37% of the patients showed evidence of degenerative arthritis on one or both sides. Zhao et al25 reported a lower prevalence of TMJ osteoarthritis. In their study using conventional radiography, the frequency was 13.3% in girls and 8.0% in boys over the range of 11 to 14 years, and it was 17.5% in girls and 10.7% in boys over the range of 15 to 19 years. We attributed the variation in prevalence mainly to the difference in diagnostic criteria, population sampling, and radiographic examination method used. However, all those studies showed that TMJ osteoarthritis was a common finding in children as well.
A number of studies1,7,14,21 have found that degenerative arthritis of TMJ increased with age. However, that would not always be the case for young people. In this study, there was no significant difference between the two age groups (11-14 and 15-18), although there was a tendency toward a higher prevalence of osteoarthritic changes in the older age group. This finding was in agreement with previous studies that sampled similar age groups.25,26
It is widely accepted that TMD is more common in females. Many studies also claimed that the frequency of osteoarthritic changes was higher in females.14,25,26 Some investigators, however, found no gender differences.7 In our study, the asymptomatic group showed no significant gender differences, however in the symptomatic group, the prevalence of osteoarthritic changes was higher in males than in females. We speculated that the results arose from gender differences in the willingness to seek help. Boys might be less likely to seek treatment than girls and only visit a hospital in a more advanced stage of the disease.
There has been controversy regarding whether clinical signs and symptoms have effects on radiographic findings. There were several previous studies7,27-29 that indicated a poor correlation between TMJ osteoarthritis and the signs and symptoms of TMD. Wiese et al14 reported that pain was not associated with the increased risk of degenerative findings in TMJ tomograms. On the other hand, Kurita et al30 reported a significant relationship between the presence of TMJ pain upon mandibular function and osteoarthritic changes at the articular surface. Among other degenerative findings, erosion seems to be associated with subjective symptoms. In this study, erosion was the most common finding in the symptomatic cases, which was consistent with a previous study.31 Zhao et al25 suggested that the presence of TMJ pain was associated with erosive changes, and Yamada et al9 found that erosive bone change was usually accompanied by pain and difficulty in mouth opening. In accordance with these studies, our study demonstrated that erosion was more frequently observed in the subjects with pain or limited mouth opening. Another controversy existed over the clinical significance of condylar positioning in the glenoid fossa. There have been many studies showing no significant association between condylar positioning and clinical and radiographic manifestations.14-18 On the other hand, several studies found that TMD patients appeared to have posterior condyle positioning.10-13 For the asymptomatic patients, there have been also conflicting reports concerning condylar positioning. One study indicated that asymptomatic volunteers showed almost randomly distributed condylar positions in the glenoid fossa,32 while another claimed that the majority of joints had condyles centered in the glenoid fossa. Our study showed a significantly different distribution between the asymptomatic and the symptomatic groups; a concentric position was more common in the asymptomatic group, and a retruded position was more common in the symptomatic group. It is usually accepted that a retruded condyle is not always associated with TMD. Nonetheless, the posterior positioning of the condyle is commonly observed in TMD patients.
In conclusion, our retrospective study demonstrated that TMJ osteoarthritis was not unusual in children and adolescents, whether they were complaining of TMD symptoms or not, and considering their age, dentists should pay more attention to monitoring the progression of degenerative changes of TMJ until the stability of mandibular growth would be established.
Footnotes
This study was supported by a grant of Pusan National University Hospital.
References
- 1.Poveda Roda R, Bagan JV, Díaz Fernández JM, Hernández Bazán S, Jiménez Soriano Y. Review of temporomandibular joint pathology. Part I: classification, epidemiology and risk factors. Med Oral Patol Oral Cir Bucal. 2007;12:E292–E298. [PubMed] [Google Scholar]
- 2.Dibbets JM, van der Weele LT. Prevalence of structural bony change in the mandibular condyle. J Craniomandib Disord. 1992;6:254–259. [PubMed] [Google Scholar]
- 3.Vanderas AP. Prevalence of craniomandibular dysfunction in children and adolescents: a review. Pediatr Dent. 1987;9:312–316. [PubMed] [Google Scholar]
- 4.Magnusson T, Egermark-Eriksson I, Carlsson GE. Four-year longitudinal study of mandibular dysfunction in children. Community Dent Oral Epidemiol. 1985;13:117–120. doi: 10.1111/j.1600-0528.1985.tb01690.x. [DOI] [PubMed] [Google Scholar]
- 5.Gazit E, Lieberman M, Eini R, Hirsch N, Serfaty V, Fuchs C, et al. Prevalence of mandibular dysfunction in 10-18 year old Israeli schoolchildren. J Oral Rehabil. 1984;11:307–317. doi: 10.1111/j.1365-2842.1984.tb00581.x. [DOI] [PubMed] [Google Scholar]
- 6.Ishibashi H, Takenoshita Y, Ishibashi K, Oka M. Age-related changes in the human mandibular condyle: a morphologic, radiologic, and histologic study. J Oral Maxillofac Surg. 1995;53:1016–1024. doi: 10.1016/0278-2391(95)90117-5. [DOI] [PubMed] [Google Scholar]
- 7.Widmalm SE, Westesson PL, Kim IK, Pereira FJ, Jr, Lundh H, Tasaki MM. Temporomandibular joint pathosis related to sex, age, and dentition in autopsy material. Oral Surg Oral Med Oral Pathol. 1994;78:416–425. doi: 10.1016/0030-4220(94)90031-0. [DOI] [PubMed] [Google Scholar]
- 8.Sanchez-Woodworth RE, Katzberg RW, Tallents RH, Guay JA. Radiographic assessment of temporomandibular joint pain and dysfunction in the pediatric age-group. ASDC J Dent Child. 1988;55:278–281. [PubMed] [Google Scholar]
- 9.Yamada K, Saito I, Hanada K, Hayashi T. Observation of three cases of temporomandibular joint osteoarthritis and mandibular morphology during adolescence using helical CT. J Oral Rehabil. 2004;31:298–305. doi: 10.1046/j.1365-2842.2003.01246.x. [DOI] [PubMed] [Google Scholar]
- 10.Pullinger AG, Solberg WK, Hollender L, Guichet D. Tomographic analysis of mandibular condyle position in diagnostic subgroups of temporomandibular disorders. J Prosthet Dent. 1986;55:723–729. doi: 10.1016/0022-3913(86)90450-6. [DOI] [PubMed] [Google Scholar]
- 11.Pereira LJ, Gavião MB, Bonjardim LR, Castelo PM. Ultrasound and tomographic evaluation of temporomandibular joints in adolescents with and without signs and symptoms of temporomandibular disorders: a pilot study. Dentomaxillofac Radiol. 2007;36:402–408. doi: 10.1259/dmfr/16641858. [DOI] [PubMed] [Google Scholar]
- 12.Gateno J, Anderson PB, Xia JJ, Horng JC, Teichgraeber JF, Liebschner MA. A comparative assessment of mandibular condylar position in patients with anterior disc displacement of the temporomandibular joint. J Oral Maxillofac Surg. 2004;62:39–43. doi: 10.1016/j.joms.2003.05.006. [DOI] [PubMed] [Google Scholar]
- 13.Bonilla-Aragon H, Tallents RH, Katzberg RW, Kyrkanides S, Moss ME. Condyle position as a predictor of temporomandibular joint internal derangement. J Prosthet Dent. 1999;82:205–208. doi: 10.1016/s0022-3913(99)70157-5. [DOI] [PubMed] [Google Scholar]
- 14.Wiese M, Svensson P, Bakke M, List T, Hintze H, Petersson A, et al. Association between temporomandibular joint symptoms, signs, and clinical diagnosis using the RDC/TMD and radiographic findings in temporomandibular joint tomograms. J Orofac Pain. 2008;22:239–251. [PubMed] [Google Scholar]
- 15.Abdel-Fattah RA. Optimum temporomandibular joint (TMJ) condylar position. Todays FDA. 1989;1:1C–3C. [PubMed] [Google Scholar]
- 16.Robinson de Senna B, Marques LS, França JP, Ramos-Jorge ML, Pereira LJ. Condyle-disk-fossa position and relationship to clinical signs and symptoms of temporomandibular disorders in women. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:e117–e124. doi: 10.1016/j.tripleo.2009.04.034. [DOI] [PubMed] [Google Scholar]
- 17.Vasconcelos Filho JO, Menezes AV, Freitas DQ, Manzi FR, Bóscolo FN, de Almeida SM. Condylar and disk position and signs and symptoms of temporomandibular disorders in stress-free subjects. J Am Dent Assoc. 2007;138:1251–1255. doi: 10.14219/jada.archive.2007.0351. [DOI] [PubMed] [Google Scholar]
- 18.Katzberg RW, Keith DA, Ten Eick WR, Guralnick WC. Internal derangements of the temporomandibular joint: an assessment of condylar position in centric occlusion. J Prosthet Dent. 1983;49:250–254. doi: 10.1016/0022-3913(83)90511-5. [DOI] [PubMed] [Google Scholar]
- 19.Pullinger A, Hollender L. Variation in condyle-fossa relationships according to different methods of evaluation in tomograms. Oral Surg Oral Med Oral Pathol. 1986;62:719–727. doi: 10.1016/0030-4220(86)90270-7. [DOI] [PubMed] [Google Scholar]
- 20.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46. [Google Scholar]
- 21.Alexiou K, Stamatakis H, Tsiklakis K. Evaluation of the severity of temporomandibular joint osteoarthritic changes related to age using cone beam computed tomography. Dentomaxillofac Radiol. 2009;38:141–147. doi: 10.1259/dmfr/59263880. [DOI] [PubMed] [Google Scholar]
- 22.Tsiklakis K, Syriopoulos K, Stamatakis HC. Radiographic examination of the temporomandibular joint using cone beam computed tomography. Dentomaxillofac Radiol. 2004;33:196–201. doi: 10.1259/dmfr/27403192. [DOI] [PubMed] [Google Scholar]
- 23.Honey OB, Scarfe WC, Hilgers MJ, Klueber K, Silveira AM, Haskell BS, et al. Accuracy of cone-beam computed tomography imaging of the temporomandibular joint: comparisons with panoramic radiology and linear tomography. Am J Orthod Dentofacial Orthop. 2007;132:429–438. doi: 10.1016/j.ajodo.2005.10.032. [DOI] [PubMed] [Google Scholar]
- 24.Takayama Y, Miura E, Yuasa M, Kobayashi K, Hosoi T. Comparison of occlusal condition and prevalence of bone change in the condyle of patients with and without temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:104–112. doi: 10.1016/j.tripleo.2006.12.033. [DOI] [PubMed] [Google Scholar]
- 25.Zhao YP, Zhang ZY, Wu YT, Zhang WL, Ma XC. Investigation of the clinical and radiographic features of osteoarthrosis of the temporomandibular joints in adolescents and young adults. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:e27–e34. doi: 10.1016/j.tripleo.2010.09.076. [DOI] [PubMed] [Google Scholar]
- 26.Petrikowski CG, Grace MG. Age and gender differences in temporomandibular joint radiographic findings before orthodontic treatment in adolescents. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:380–385. doi: 10.1016/s1079-2104(99)70228-3. [DOI] [PubMed] [Google Scholar]
- 27.Wiese M, Wenzel A, Hintze H, Petersson A, Knutsson K, Bakke M, et al. Osseous changes and condyle position in TMJ tomograms: impact of RDC/TMD clinical diagnoses on agreement between expected and actual findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:e52–e63. doi: 10.1016/j.tripleo.2008.03.021. [DOI] [PubMed] [Google Scholar]
- 28.Wiberg B, Wänman A. Signs of osteoarthrosis of the temporomandibular joints in young patients: a clinical and radiographic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:158–164. doi: 10.1016/s1079-2104(98)90118-4. [DOI] [PubMed] [Google Scholar]
- 29.Hiltunen K, Peltola JS, Vehkalahti MM, Närhi T, Ainamo A. A 5-year follow-up of signs and symptoms of TMD and radiographic findings in the elderly. Int J Prosthodont. 2003;16:631–634. [PubMed] [Google Scholar]
- 30.Kurita H, Kojima Y, Nakatsuka A, Koike T, Kobayashi H, Kurashina K. Relationship between temporomandibular joint (TMJ)-related pain and morphological changes of the TMJ condyle in patients with temporomandibular disorders. Dentomaxillofac Radiol. 2004;33:329–333. doi: 10.1259/dmfr/13269559. [DOI] [PubMed] [Google Scholar]
- 31.Lee JU, Kim HS, Song JS, Kim KA, Koh KJ. Bone change of mandibular condyle using cone beam computed tomography. Korean J Oral Maxillofac Radiol. 2007;37:139–147. [Google Scholar]
- 32.Ren YF, Isberg A, Westesson PL. Condyle position in the temporomandibular joint. Comparison between asymptomatic volunteers with normal disk position and patients with disk displacement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:101–107. doi: 10.1016/s1079-2104(95)80025-5. [DOI] [PubMed] [Google Scholar]