Abstract
Objective
To evaluate the effectiveness of a worksite vitality intervention on vigorous physical activity (VPA), fruit intake, aerobic capacity, mental health and need for recovery after work among older hospital workers (ie, 45 years and older).
Methods
The 6-month intervention was evaluated using a randomised controlled trial design. Workers who were randomised to the intervention group (n=367; control: n=363) received the Vital@Work intervention containing (1) a Vitality Exercise Program (VEP) combined with (2) three visits to Personal Vitality Coach. The VEP consisted of a weekly yoga session, a weekly workout session and weekly unsupervised aerobic exercising. Free fruit was provided at the VEP. Data on the outcome measures were collected (ie, year 2009–2010) at baseline (n=730) and 6 months of follow-up after baseline (n=575) using questionnaires, accelerometers and 2 km walk tests. Effects were analysed according to the intention-to-treat principle with complete cases (n=575) and imputed data (n=730) using linear regression analyses. Additional analyses were performed for high yoga and workout compliance (ie, >mean number of sessions).
Results
Effects were found for sports activities (β=40.4 min/week, 95% CI 13.0 to 67.7) and fruit intake (β=2.7 pieces/week, 95% CI 0.07 to 4.7) and were stronger for workers with high compliance to yoga (sport: β=49.6 min/week, 95% CI 13.9 to 85.2; fruit: β=3.8 pieces/week, 95% CI 1.1 to 6.4) and workout sessions (sport: β=72.9 min/week, 95% CI 36.1 to 109.8; fruit: β=4.0 pieces/week, 95% CI 1.1 to 6.4). The intervention group lowered their need for recovery, when compared to controls (β=−3.5, 95% CI −6.4 to −0.54), with stronger effects for high workout compliance (β=−5.3, 95% CI −9.3 to −1.3). No effects were found on VPA, aerobic capacity or mental health.
Conclusions
Implementation of worksite yoga and workout facilities and minimal fruit interventions should be considered by employers to promote transitions into healthier lifestyles and thereby health.
Keywords: Lifestyle, older workers, randomised controlled trial, workplace yoga, workplace aerobic exercising, ageing, workplace, health promotion, randomised trials
Introduction
The baby boom after the Second World War, longer life expectancies and lower birth rates are leading to an ageing society and subsequently a shrinkage of the workforce. Hence, ageing workers are required in the near future. To do so, most Western countries, at which the official retirement age is around the age of 65 years,1 2 are considering to raise or have already raised the official retirement age. For instance, in the Netherlands, the government recently decided to raise the retirement age from 65 to 67 years in the upcoming decades.3 But also other solutions are needed to maintain ageing workers, who are defined as workers aged 45 years and older.4 This definition is based on the period at which major changes occur in functional capacities (eg, decline in aerobic capacity, higher prevalence of chronic diseases)5–7 and relevant work-related outcomes (eg, higher need for recovery (NFR) from work, lower work ability and more sick leave).8 9 Also, previous studies have shown that an age-related decline in health is a major contributor to early exit from work. Thus, in order to prolong the working life of older workers and increase their employability, it is important to promote and maintain good health.
A concept assumed to be closely related to and therefore may influence health is vitality. Vitality is related to both mental and physical factors of health.10–15 Regarding the mental factors, vitality reflects well-being, lower levels of fatigue, higher levels of emotional energy, mental resilience and perseverance.10–14 With respect to the physical factors, vitality is characterised by high energy levels and feeling ‘strong and fit’.14 In the field of occupational health, vitality has been described as one of the three dimensions of work engagement and is characterised by ‘feeling full of energy, strong and fit and being able to keep on working indefatigable’.14 15 In the Vital@Work study, a worksite lifestyle intervention was developed aiming at improving both mental (ie, by yoga sessions) and physical (ie, by aerobic exercising) factors of vitality.16
Healthy lifestyle choices, such as sufficient physical activity (PA) and healthy dietary habits (eg, sufficient fruit intake), contribute to better health outcomes, for example, mental health and lower risk for chronic diseases (ie, cardiovascular diseases, diabetes, cancer).17–21 Although the beneficial effects of yoga are not widely reported yet, studies among patient populations showed favourable effects on mental health and well-being.22–25 Therefore, a worksite health promotion (WHP) programme containing physical exercising (ie, aimed at improving aerobic capacity) and yoga is considered a potentially effective tool to keep older workers vital, promote their health and thereby prolong their labour participation. The beneficial effects of WHP programmes on work-related outcomes, such as sick leave and productivity, have indeed been reported.26–28 Also, positive effects of WHP programmes on health29 and aforementioned lifestyle behaviours have been reported.30 31
The objective of the present study was to evaluate the effectiveness of the Vital@Work intervention on (1) lifestyle behaviours, that is, sports, vigorous physical activities (VPA), fruit intake and (2) vitality-related outcomes, that is, aerobic capacity, mental health and the NFR after a day of work.
Methods
Study population and design
All workers aged 45 years and older from two academic hospitals in the Netherlands were invited to participate between April and October 2009. A worker was considered eligible when working at least 16 h a week, giving written informed consent and having no risk for developing adverse health effects when becoming physically active as assessed using the Physical Activity Readiness Questionnaire.32 The Medical Ethics Committee of VU University Medical Center approved the study protocol. Details on the randomised controlled trial design have been described extensively elsewhere.16
The workers who consented to participate were, after baseline measurements, individually randomised to the intervention or control group using Random Allocation Software (V.1.0, May 2004; Isfahan University of Medical Sciences, Isfahan, Iran). The research assistant notified each worker to which group he or she had been allocated and did not reveal the group allocation to the investigator responsible for data analyses. Blinding of participants or intervention providers was impossible. The sample size calculation is described extensively elsewhere16 but showed that 189 participants per group were needed at follow-up.
After randomisation, workers of both the intervention and control group received written information about a healthy lifestyle in general (ie, diet, PA and relaxation). Additionally, the intervention group received a 6-month lasting intervention consisting of (1) a Vitality Exercise Program (VEP) with (2) provision of free fruit and combined with (3) three visits to a Personal Vitality Coach (PVC). The VEP consisted of a weekly 45 min: (1) yoga session, (2) workout session and (3) unsupervised aerobic exercise session. Yoga was guided by a qualified yoga instructor and included relaxation and preparation postures for the joints, series of standing and forward bending postures and twists, light back bending postures and total relaxation and meditation. Workout sessions were guided by certified fitness instructors and consisted of a warming-up followed by aerobic exercises, resistance training and cooling-down. The intensity of the workout had to be 65%–90% of the age-predicted maximum heart rate (HRmax).33 34 The resistance training was progressive in nature and provided stimulus to all major muscle groups. Besides the yoga and workout sessions, workers were prescribed to perform weekly 45 min unsupervised vigorous PA (eg, fitness, running, spinning) with a similar intensity as the guided workout sessions. At the VEP group sessions, there was free provision of fruit. As to the PVC visits, the first PVC visit was scheduled at the start of the intervention and was followed by two consecutive visits at 4–6 weeks and 10–12 weeks after the first visit. During the 30-min PVC visits, five items were discussed, namely goal setting, confidence in achieving formulated goals, feedback on formulated goals, discussing barriers for formulated goals and problem solving. At the first visit, the items goal setting and confidence in achieving formulated goals were discussed. At the second and third visit, the following items were discussed, namely feedback on formulated goals, discussing barriers for formulated goals and problem solving.
Outcome measures
Data on outcome measures were collected (ie, year 2009–2010) at baseline (n=730) and 6 months of follow-up after baseline (n=575) using questionnaires, accelerometers and 2 km walk tests.
Lifestyle behaviours
The level of PA was measured both subjectively, using the Short QUestionnaire to ASses Health-enhancing physical activity (SQUASH),35 and objectively among a random subsample of 196 workers using Computer Science Application (CSA) accelerometers (Type GTM1 and ActiTrainer; ActiGraph, Pensacola, Florida, USA).
The SQUASH questionnaire35 measures habitual PA levels referring the past week of four PA domains, that is, commuting, occupational, household and leisure time. For each domain, workers were asked to indicate the frequency (times per week), self-reported intensity (light, moderate or vigorous) and average duration of the activity per day.35 As part of leisure time PA, workers could report up to four sports, with accompanying frequency, intensity and duration. For each domain, activities were subdivided into three age-dependent intensity categories (ie, light/moderate/vigorous), corresponding to the metabolic equivalents (METs) derived from Ainsworth's compendium of PAs.36 37 Since the Vital@Work intervention was aimed at improving sports and vigorous physical activities (VPA), the outcome measures used for this study were total minutes per week of: (1) sports activities, (2) VPA (aged<55 years: ≥6.5 METs; aged ≥55 years: ≥5.0 METs) and (3) total moderate-to-vigorous physical activities (MVPA). Total minutes per week of VPA and MVPA (aged <55 years: ≥4.0 METs; aged ≥55 years: ≥3.0 METs) were calculated by summing the time spent on at least moderate intensity activities across all domains.38
Among 214 older workers (nintervention=102; ncontrol=112), that is, a random sample out of the 730 workers included at baseline, PA was measured using accelerometers, which registered actual PA by detecting the magnitude of vertical accelerations and decelerations.39 Workers were asked to wear the accelerometers on the right hip during waking hours for 7 days. Activity counts were measured over a time interval of 60 s (epoch). Data were cleaned and scored using Meterplus40 according to the following criteria: (1) a wearing period of three or more valid days, (2) the minimal wearing time for a valid day was 10 h and (3) Freedson's cut-off points41 were used to quantify PA intensities. Since the wearing period varied between workers (range 3–7 days, the total minutes per intensity category were divided by the valid wearing days (resulting in minutes per day) multiplied by 7 (in minutes per week). The outcome measures obtained from the accelerometers were the total minutes per week of VPA: ≥5725 counts/min and MVPA: ≥1953 counts/min.
Weekly fruit intake was assessed using the validated Short Fruit and Vegetable Questionnaire,42 of which only the questions about fruit consumption were included, by verifying how many days per week they usually eat fruit and the number of pieces of fruit per day.
Vitality-related outcomes
Aerobic capacity (VO2max) was estimated using the UKK 2 km walk test. This test has shown to be a feasible and accurate method for predicting VO2max among healthy populations43 44 and was performed in a public park near the workplace. Workers were asked to fill out a form with their name, age and body height and weight and put on a heart rate monitor (type S610I; Polar Electro, Lake Success, New York, USA). Workers had to walk 2 km individually at a pace as brisk as possible, but without running. At the finish, the research assistant noted heart rate and performance time. VO2max was estimated using gender-specific equations including age, body mass index, performance time (in minutes) and heart rate at finish (HR).45
Mental health was measured using the mental health scale of the RAND-36 general health questionnaire,46 which consists of five questions that refer to the past 4 weeks: “Did you feel …?” (1) nervous, (2) down in dumps, (3) peaceful, (4) sad and (5) happy. The RAND-36 mental health scale, which has shown to be sufficiently reliable, ranges from 0 to 100 points (higher scores indicating better subjective mental health), with a score of >76.8 considered as good.46
NFR from work was assessed with a scale from the Dutch Questionnaire on the Experience and Evaluation of Work (VBBA)47 consisting of 11 statements (yes/no) concerning the recovery period after a day work. Examples of negative statements are: “My job causes me to feel rather exhausted at the end of a working day” and “I find it hard to relax at the end of a working day”. An illustration of a positive statement is: “After the evening meal, I generally feel good in shape”. The NFR scale ranges from 0 to 100 (higher scores being more unfavourable), with a score ≤54 being indicated as a sufficient NFR.47
Potential confounders and effect modifiers
At baseline, data on potential confounders and effect modifiers were assessed by questionnaire including age, gender (male/female), education (low=elementary school or less, medium=secondary education and high=college/university), chronic disease status (yes/no), smoking (yes/no), intervention location (Amsterdam/Leiden), type of work (blue/white collar) and marital status (married/cohabitating/single/divorced/widowed).
Statistical analysis
Differences in baseline characteristics (presented in table 1) between the intervention and control group and differences in outcome measures between completers and non-completers were tested using independent t test for continuous variables (eg, age, working hours per week) and Pearson's χ2 tests for categorical (ie, education) and dichotomous variables (eg, chronic diseases, smoking). To analyse the intervention effects (table 2), the differences in change over time between the intervention and control group (ie, β=the regression coefficient) were analysed using linear regression analyses.48 In this analyses, the outcome measures over 6-month follow-up (ie, PA, fruit intake, aerobic capacity, mental health and NFR) were regressed onto the baseline values of these outcomes. All analyses were performed according to the intention-to-treat principle. As adding potential confounders to crude models did not change intervention effects, >10% and no effect modifiers were found; only crude effect estimates are presented in this paper.
Table 1.
Mean and SD for continuous measures and numbers and percentages (%) for dichotomous and categorical measures for the intervention (n=367) versus control group (n=363) and for completers (n=575) versus non-completers (n=155)
| Study characteristics | Total study population (n=730) | |||
| Intervention group (n=367) | Control group (n=363) | Completers (n=575) | Non-completers (n=155) | |
| Female, n (%) | 274 (74.7) | 277 (76.3) | 429 (74.6) | 122 (78.7) |
| Age (years), mean (SD) | 52.5 (4.8) | 52.3 (4.9) | 52.5 (4.9) | 52.0 (4.7) |
| Partner (yes), n (%) | 268 (73.0) | 281 (77.4) | 436 (75.8) | 113 (72.9) |
| Chronic diseases (yes), n (%) | 207 (59.1) | 217 (57.0) | 326 (56.7) | 98 (63.2) |
| Smoking (yes), n (%) | 38 (10.4) | 40 (11.0) | 55 (9.6) | 23 (14.8) |
| Education level, n (%) | ||||
| Low | 42 (11.4) | 32 (8.8) | 55 (9.6) | 19 (12.3) |
| Intermediate | 100 (27.3) | 110 (30.3) | 162 (28.2) | 48 (31.0) |
| High | 225 (61.3) | 221 (60.9) | 358 (62.3) | 88 (56.8) |
| Working hours per week, mean (SD) | 30.4 (7.3) | 29.8 (7.0) | 30.2 (6.6) | 30.0 (7.9) |
| Irregular working hours, n (%) | ||||
| Yes | 44 (12.0) | 52 (14.3) | 69 (12.0) | 28 (18.1)* |
| No | 323 (88.0) | 311 (85.7) | 506 (88.0) | 127 (81.9) |
Significant difference (p=0.042) between completers and non-completers.
Differences between intervention and control group and between completers and non-completers were tested using independent t tests for continuous measures and Pearson's χ2 tests for dichotomous and categorical measures.
%, proportion of total group.
Table 2.
Mean and SD for complete cases and imputed data for missing values on PA (ie, sport, VPA and MVPA), fruit intake, aerobic capacity (estimated VO2max), mental health and need for recovery for the intervention and control group at baseline and after 6 months of follow-up after baseline
| Group | Complete cases analyses | Imputed data for missing values analyses | |||||||||
| n | T0m, mean (SD) | T6m, mean (SD) | ∆ (T0−T6m) | β (95% CI) | n | T0m, mean (SD) | T6m, mean (SD) | ∆ (T0−T6m) | β (95% CI) | ||
| PA—by the SQUASH | |||||||||||
| Sports (min/week) | I | 283 | 134.6 (139.2) | 209.9 (192.1) | 75.3 | 40.4 (13.0 to 67.7) * | 367 | 130.7 (136.7) | 205.6 (189.7) | 74.9 | 33.2 (29.5 to 36.9) * |
| C | 269 | 133.9 (139.8) | 169.0 (177.5) | 35.1 | 363 | 123.3 (135.0) | 167.9 (175.7) | 44.6 | |||
| VPA (min/week) | I | 286 | 356.9 (300.8) | 516.4 (655.0) | 159.5 | 48.5 (−81.0 to 178.1) | 367 | 178.8 (262.6) | 299.2 (523.6) | 120.4 | 24.9 (37.0 to 86.9) |
| C | 271 | 362.9 (292.7) | 473.2 (579.7) | 110.3 | 363 | 182.3 (270.3) | 277.0 (438.3) | 94.7 | |||
| MVPA (min/week) | I | 286 | 830.4 (611.6) | 1091.3 (832.4) | 260.9 | −1.4 (−126.0 to 123.2) | 367 | 803.7 (605.9) | 1093.4 (797.0) | 289.3 | −7.7 (−108.0 to 92.5) |
| C | 271 | 827.4 (620.9) | 1092.0 (264.6) | 264.6 | 363 | 825.2 (607.4) | 1113.5 (750.7) | 288.3 | |||
| PA—by CSA | |||||||||||
| VPA (min/week) (min/week) | I | 61 | 12.7 (33.6) | 20.3 (34.4) | 7.6 | 8.5 (−0.34 to 17.3) | 95 | 14.1 (32.1) | 18.7 (26.9) | 4.6 | 4.3 (−1.7 to 10.2) |
| C | 73 | 13.9 (35.3) | 12.4 (28.3) | −1.5 | 101 | 12.4 (30.4) | 13.7 (23.1) | 1.3 | |||
| MVPA (min/week) | I | 61 | 224.3 (173.8) | 244.6 (141.2) | 20.3 | 13.8 (−25.9 to 53.5) | 95 | 233.4 (157.0) | 241.6 (109.2) | 8.2 | 7.0 (−18.0 to 32.1) |
| C | 73 | 220.2 (156.4) | 229.8 (103.6) | 9.6 | 101 | 220.0 (158.0) | 232.2 (83.7) | 12.2 | |||
| Fruit intake | |||||||||||
| Pieces/week | I | 293 | 25.3 (14.6) | 31.0 (14.7) | 5.7 | 2.7 (0.63 to 4.7) * | 367 | 24.8 (14.9) | 30.5 (14.7) | 5.7 | 2.0 (0.13 to 3.9) * |
| C | 282 | 26.0 (13.2) | 28.7 (14.8) | 2.7 | 363 | 25.4 (13.4) | 28.8 (14.7) | 3.4 | |||
| Vitality-related outcomes | |||||||||||
| VO2max | I | 138 | 30.7 (6.7) | 31.7 (8.3) | 1.0 | 0.231 (0.82 to 1.03) | 209 | 30.1 (7.0) | 31.2 (8.1) | 1.1 | 0.06 (−1.2 to 1.3) |
| C | 122 | 31.7 (6.2) | 32.4 (8.3) | 0.7 | 218 | 31.8 (8.2) | 31.8 (8.2) | 1.0 | |||
| Mental health | I | 293 | 76.0 (14.2) | 76.9 (13.8) | 0.9 | 1.04 (−0.70 to 2.78) | 367 | 75.2 (14.8) | 76.2 (14.1) | 1.0 | 0.87 (−0.79 to 2.5) |
| C | 282 | 77.9 (13.3) | 77.0 (13.4) | −0.9 | 363 | 77.6 (13.4) | 76.9 (13.4) | −0.7 | |||
| Need for recovery | I | 293 | 28.5 (27.2) | 25.3 (26.7) | −3.2 | −3.5 (−6.4 to −0.54) * | 367 | 29.6 (27.7) | 26.4 (27.3) | −3.2 | −2.8 (−3.2 to −2.4) * |
| C | 282 | 26.9 (27.4) | 27.5 (28.0) | 0.6 | 363 | 27.8 (28.1) | 27.9 (28.2) | 0.1 | |||
p<0.05.
The intervention effects are also presented.
∆, mean difference between baseline and follow-up measure directly after the intervention ended (ie, 6 months); β, estimated intervention effect from linear regression analysis adjusted for baseline differences on the outcome measure; C, control group; I, intervention group; MVPA, moderate-to-vigorous physical activities; PA, physical activity; SQUASH, Short QUestionnaire to ASses Health-enhancing physical activity.
As not all the individuals included in the intervention group had participated in yoga sessions and workout sessions in the same way,49 additional analyses were performed taking this into account. Additionally, data analyses were performed to determine significant relationships between the compliance of workers to the guided yoga and workout group sessions and the study outcomes (table 3). The compliance to the guided group sessions was defined based on the mean number of followed yoga and workout group sessions, which were distinguished from the process evaluation of the Vital@Work intervention and were 10.4 and 11.1 sessions per 24 weeks, respectively.49 Compliance categories defined were (1) control group workers (ie, reference), (2) intervention group workers, who did not follow a guided session, (2) low compliance: ≤mean number of sessions and (3) high compliance: >mean number of sessions. To test differences between these compliance groups, linear regression analyses were used with dummy variables for each compliance category with the control group as reference category.
Table 3.
Dose–response relation for sports, fruit intake and need for recovery among yoga and workout subgroups for both complete cases and imputed data for missing values analyses
| Group | Complete cases analyses | Imputed data for missing values analyses | ||||
| No group sessions (nyoga=63; nworkout=79) | Low compliance (nyoga=110; nworkout=108) | High compliance (nyoga=120; nworkout=106) | No group sessions (nyoga=108; nworkout=133) | Low compliance (nyoga=135; nworkout=126) | High compliance (nyoga=124; nworkout=108) | |
| β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | |
| Sport (min/week) | ||||||
| Yoga | 36.7 (−8.7 to 82.0) | 32.2 (−5.0 to 69.4) | 49.6 (13.9 to 85.2) * | 25.9 (−14.2 to 66.0) | 30.5 (−5.8 to 66.8) | 42.3 (7.6 to 76.9) * |
| Workout | 16.2 (−25.1 to 57.4) | 25.0 (−12.6 to 62.6) | 72.9 (36.1 to 109.8) * | 16.0 (−22.3 to 54.4) | 21.8 (−14.3 to 57.8) | 67.4 (31.6 to 103.3) * |
| Fruit intake (piece/week) | ||||||
| Yoga | 1.2 (−2.2 to 4.5) | 2.3 (−0.5 to 5.0) | 3.8 (1.1 to 6.4) * | 0.98 (−2.0 to 4.0) | 1.7 (−0.87 to 4.3) | 3.3 (0.68 to 5.9) * |
| Workout | 0.96 (−2.1 to 4.0) | 2.6 (−0.14 to 5.4) | 4.2 (1.5 to 7.0) * | 0.67 (−2.1 to 3.4) | 2.0 (−0.67 to 4.6) | 3.8 (1.1 to 6.5) * |
| Need for recovery | ||||||
| Yoga | −3.3 (−8.2 to 1.6) | −3.3 (−7.2 to 0.7) | −3.8 (−7.6 to 0.05) | −2.4 (−6.9 to 2.0) | −2.6 (−6.6 to 1.4) | −3.4 (−7.3 to 0.41) |
| Workout | −4.2 (−8.6 to 0.28) | −1.2 (−5.1 to 2.8) | −5.3 (−9.3 to −1.3) * | −3.0 (−7.2 to 1.2) | −0.81 (−4.9 to 3.2) | −4.9 (−8.9 to −1.0) * |
p<0.05.
β, estimated intervention effect from linear regression analysis adjusted for baseline differences on the outcome measure; piece/week, pieces of fruits per week.
As the possible effects of the missing participants should be considered,50 51 it is recommended to perform, in addition to complete case analyses, sensitivity analyses with imputed data.52 For the sensitivity analyses (tables 2 and 3), missing data were imputed using multiple imputations based on Multivariate Imputation by Chained Equations.53 54 The multiple imputations procedure was performed in PASW (V.18.0) by generating 40 different data sets. By using Rubin's rules, PASW enabled to pool effects from these 40 data sets.55 All statistical analyses were performed using PASW.
Results
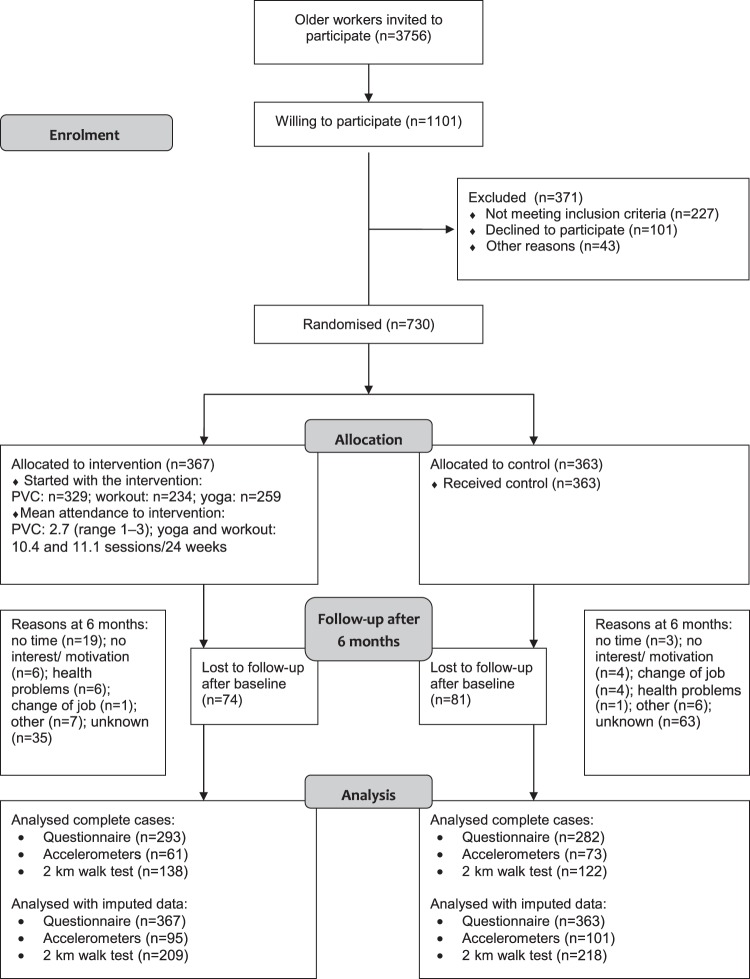
In figure 1, a flow diagram of the study population is presented. Enrolment of the study population took place between April and September 2009. In total, 730 older workers were included as they completed the baseline questionnaire and were subsequently randomised to the intervention (n=367) or control group (n=363). Of those workers randomised to the intervention group, 329 (89.6%) followed PVC visits, 259 (70.6%) and 234 (63.8%) guided yoga and workout sessions, respectively. After 6 months of follow-up, 575 workers (intervention n=293, control n=282) completed the questionnaire 6 months after baseline and were therefore used for complete cases analyses. Also, sensitivity analyses with imputed data among the total population (n=730) were performed. No adverse events of the intervention were reported. In table 1, baseline characteristics of the study population are presented with no significant differences between the groups in any of these variables. Employees with regular working hours (n=96) were more likely to complete participation (p=0.042) when compared to workers with irregular working hours (n=634).
Figure 1.
Flow diagram Vital@Work study. PVC, Personal Vitality Coach.
Effectiveness on lifestyle and vitality-related outcomes
Complete cases analyses, as shown in table 2, revealed effectiveness on sports activities (β: 40.4 min/week, 95% CI 13.0 to 67.7). The control group workers increased their sports activities with 35.1 min/week, but when compared to the intervention group, this increase was statistically higher (75.3 min/week). As for the subjectively measured VPA, in total 134 workers (intervention n=63, control n=73) completed these measures. It appeared that both the intervention and control group increased their VPA from baseline to 6 months later (+159.5 vs +110.3 min/week, respectively), with no significant differences between groups (β=48.5 min/week, 95% CI −81.0 to 178.1) (table 2). Also based on the accelerometer data, there were no significant differences between groups (β=8.5 min/week, 95% CI −0.34 to 17.3). No effects were found on total weekly MVPA (SQUASH: β=−1.4 min/week, 95% CI −126.0 to 123.2; CSA: β=13.8 min/week, 95% CI −25.9 to 53.5). Regarding fruit intake, the intervention group workers improved their fruit intake significantly more when compared to the control group (+5.7 vs +2.7 pieces/week), resulting in an intervention effect on increasing fruit intake (β=2.7 pieces/week, 95% CI 0.63 to 4.7) (table 2). As for the vitality-related outcomes, no significant effects were found on aerobic capacity or mental health (table 2). As for NFR, the intervention group significantly decreased their NFR more when compared to the control group (−3.2 vs 0.6 points). Hence, the intervention was effective in decreasing workers' NFR (β=−3.5 points, 95% CI −6.4 to −0.54) (table 2).
Additional analyses
In table 3, only the relationships between the outcomes measures and guided group compliance that appeared to be significant are presented. A significant relationship was found between sports and high compliance to the guided yoga (β=49.6 min, 95% CI 13.9 to 85.2) and workout sessions (β=72.9 min/week, 95% CI 36.1 to 109.8) when compared to the control group (table 3). Also for fruit intake, effects were stronger in the high compliance group of both the yoga (β=3.8 pieces, 95% CI 1.1 to 6.4) and the workout sessions (β=4.0 pieces/week, 95% CI 1.1 to 6.4).
Sensitivity analyses
Sensitivity analyses with imputed data for missing values showed similar findings when compared to the complete cases analyses (tables 2 and 3). However, the effect sizes, derived from the analyses with imputed data, were consistently smaller when compared to the complete cases.
Discussion
This study showed that intervention group workers significantly increased their weekly sports activities and fruit intake when compared to control group workers. Also, the intervention favourably affected the NFR after a day of work. No effects were observed for VPA, aerobic capacity and mental health.
Limitations and strengths
Some limitations of this study can be indicated. First, we studied a relatively healthy older workers population, mainly consisting of female workers, making it more difficult to generalise the study results. Another limitation is that we failed to ensure vigorous intensity physical activity compliance during the guided workout session, which was required to improve aerobic capacity. Also, sensitivity analyses showed similar but smaller estimates of effects, when compared to the complete cases analyses, indicating that the risk of bias is minimal. This is a commonly seen consequent of imputation52 but could indicate a potentially biased estimation obtained from complete cases. Nevertheless, both complete cases and imputed data analyses showed comparable intervention effects (table 2). Presenting sensitivity analyses with imputed data, as done in our study, can also be indicated as strength, as complete cases analyses are mostly used in trials.52 Another strength was that the intervention was specifically tailored to the needs of this specific group of older workers.16 Furthermore, to our knowledge, this study is the first one investigating a worksite intervention consisting of both yoga and aerobic exercising aiming to promote the mental and physical components of health. Another strength was that, both subjective (ie, questionnaires) and objective measurements (ie, accelerometers and 2 km walk tests for measuring of PA and aerobic capacity, respectively) were used to obtain data, although the latter due to practical reasons only among a random subsample. As structural labour shortages are expected in the near future,2 it is essential to extend the labour participation of older workers. The results of this study are therefore innovative and provided valuable information.
Comparison with other studies
Reviews have shown that workplace PA interventions have positive effects on PA behaviour,29 56 57 but effects on VPA are less clear. Our VPA findings were supported by a previous study evaluating a workplace PA intervention consisting of resistance training and physical exercise, which reported no differences on VPA.58 Interestingly, our study showed a positive effect on weekly sports activities but not on VPA. A likely explanation for this could be that the SQUASH is not able to detect small changes over time (ie, poor responsiveness) regarding PA intensities59 but is more useful for detecting changes in clearly defined activities (ie, sports). As the responsiveness of the SQUASH has not been evaluated before, it is recommended to do so. Furthermore, objectively measured could be indicated as more suitable to study changes in PA over time, sample sizes in the present study were too small for detecting significant differences between the intervention and control group. To illustrate, a sample size calculation based on data from our study (α=0.05; power=0.90; two-sided testing, mean baseline VPA: 13.3±34.5 min/week, loss to follow-up of 25%) showed that 199 older workers per group, and 498 in total, were needed. In contrast, our study managed to collect data regarding VPA among 134 workers. To detect changes over time and consequently effectiveness in future studies using accelerometers, it is therefore advised to use sample size calculations based on the specific PA outcome measure, for instance VPA.
The positive finding regarding fruit intake were supported by two other studies.60 61 Both offered free fruit at the workplace aimed to promote fruit intake by increasing availability and accessibility. In most Europe countries, daily fruit recommendations are not met by the majority of the adult population,62 and a worldwide trend for decreased fruit consumption has been seen.63 Thus, to promote population-wide fruit intake, effective strategies are needed. As the majority of the adults spend most their time at work and the positive effects shown in this study, we recommend implementation of minimal worksite fruit interventions.
The lack of impact on aerobic fitness and mental health may be caused by the relatively healthy, fit and physically active group of highly educated middle-aged workers we studied. This could indicate a healthy worker effect.64 65 Healthier workers are more likely to stay in the workforce than those who are sick or physically unfit. This may be especially true for older hospital workers, a population that has to deal with higher physical workloads than an average Dutch worker. Specific for aerobic fitness, a review of Proper et al (2003)56 showed inconclusive evidence for worksite PA programmes on aerobic capacity. This is probably due to the fact that quite intensive PA, required for enhancement of aerobic capacity, are often not reached.56 As the mean number of attended workout sessions was 11.1 (SD=7.2) during a 24-week intervention period,49 this could indeed be the case in our study. To ensure exercising with certain intensity in future research, it is recommended to objectively monitor exercise intensity compliance using heart rate monitors or accelerometers.
Effects of PA or yoga programmes on NFR have not been investigated before. The improvement found in NFR can be indicated as a relevant effect. It is known that the NFR worsens during ageing, and this seems to be especially true for highly educated women, who are largely represented in our study.66 Besides, high NFR predicts sickness absence duration,67 which is an important predictor for early retirement.68 69
Conclusion and implications
The Vital@Work intervention was successful in increasing sports participation and fruit intake, and positively affected NFR after a day work, but was not effective in improving VPA, aerobic capacity or mental health. To increase involvement in sports among older workers, implementation of worksite yoga and workout facilities might be considered by employers. Moreover, minimal worksite fruit interventions are recommended to promote transitions into better lifestyles and, on the long run, health.
What is already known on this subject.
A structural labour shortage is expected in the near future, making it important to extend the labour participation of older workers. By doing so, it is essential to promote and maintain their good health.
Previous research has shown that worksite physical activity programmes has positive effects on health- and work-related outcomes.
What this study adds.
This study is the first one investigating a worksite intervention containing both yoga and aerobic exercising aiming to promote both the mental and the physical components of health.
As the labour participation of specifically older workers need to be extended, the results of this study are innovative and provide valuable information for both (occupational) health epidemiology and employers.
Implementation of worksite yoga and workout facilities might be considered by employers.
Minimal worksite fruit interventions are recommended to promote healthier transitions into better lifestyles and, on the long run, health.
Footnotes
Funding: The Vital@Work study is financially supported by the ‘Foundation Institute GAK’. The trial is registered at the Dutch Trial Register (NTR) under trial registration number: NTR1240 (http://www.trialregister.nl/trialreg/admin/rctview.asp?TC=1240).
Competing interests: None.
Patient consent: Obtained.
Ethics approval: The study was approved by Medical Ethics Committee of VU University Medical Center.
Contributors: JES, KIP, AJvdB and WvM provided support in the design of the Vital@Work study. KIP wrote the initial research project proposal. JES coordinated the data collection, performed data analysis and drafted the manuscript. KIP, AJvdB and WvM contributed intellectual input and provided support for this study. All authors contributed to the further writing of the manuscript. All authors have read and corrected draft versions of the manuscript and approved the final manuscript.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Organisation for Economic Co-operation and Development (OECD) Live Longer, Work Longer: a Synthesis Report. Paris: OECD Publications, 2006 [Google Scholar]
- 2. Organisation for Economic Co-operation and Development (OECD) OECD Annual Report 2007. Paris: OECD Publications, 2007 [Google Scholar]
- 3. van Dalen HP, Henkens K, Henderikse W, et al. Do European employers support later retirement? Int J Manpower 2010;31:360–73 [Google Scholar]
- 4. Ilmarinen JE. Aging workers. Occup Environ Med 2001;58:546–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ilmarinen JE, Tuomi K, Klockars M. Changes in the work ability of active employees over an 11-year period. Scand J Work Environ Health 1997;23(Suppl 1):49–57 [PubMed] [Google Scholar]
- 6. Ilmarinen JE, Tuomi K. Work ability of aging workers. Scand J Work Environ Health 1992;18(Suppl 2):8–10 [PubMed] [Google Scholar]
- 7. Kessler RC, Greenberg PE, Mickelson KD, et al. The effects of chronic medical conditions on work loss and work cutback. J Occup Environ Med 2001;43:218–25 [DOI] [PubMed] [Google Scholar]
- 8. von Bonsdorff ME, Huuhtanen P, Tuomi K, et al. Predictors of employees' early retirement intentions: an 11-year longitudinal study. Occup Med (Lond) 2010;60:94–100 [DOI] [PubMed] [Google Scholar]
- 9. Rice NE, Lang IA, Henley W, et al. Common health predictors of early retirement: findings from the english longitudinal study of ageing. Age Ageing 2011;40:54–61 [DOI] [PubMed] [Google Scholar]
- 10. Shirom A. Feeling energetic at work: on vigor's antevendents. In: Bakker A, Leiter M, eds. Work Engagement: Recent Developments In Theory And Research. New York, NYC: Psychology Press, 2010 [Google Scholar]
- 11. Ryan RM, Frederick C. On energy, personality, and health: subjective vitality as a dynamic reflection of well-being. J Pers 1997;65:529–65 [DOI] [PubMed] [Google Scholar]
- 12. McNair DM, Lorr M, Droppleman LF. Manual for the Profile of Mood States. San Diego: Educational and Industrial Testing Service, 1971 [Google Scholar]
- 13. McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-Item short-form health Survey (SF-36): II. psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 1993;31:247–63 [DOI] [PubMed] [Google Scholar]
- 14. Schaufeli WB, Bakker AB. Utrecht Work Engagement Scale. Occupational Health Psychology Unit Utrecht University. Utrecht, the Netherlands: Occupational health psychology unit Utrecht university, 2003 [Google Scholar]
- 15. Schaufeli WB, Bakker AB. Bevlogenheid: een begrip gemeten. Gedrag en Organisatie 2004;17:90–112 [Google Scholar]
- 16. Strijk JE, Proper KI, van der Beek AJ, et al. The Vital@Work Study. The systematic development of a lifestyle intervention to improve older workers' vitality and the design of a randomised controlled trial evaluating this intervention. BMC Public Health 2009;9:408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bouchard C, Shephard RJ. Physical activity, fitness, and health: the model and key concepts. In: Bouchard C, Shephard RJ, Stepehns T, eds. Physical Activity, Fitness and Health. International Proceedings and Consensus Statement. Champaign: Human Kinetics Books, 1994 [Google Scholar]
- 18. Penedo FJ, Dahn JR. Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Curr Opin Psychiatry 2005;18:189–93 [DOI] [PubMed] [Google Scholar]
- 19. Van Duyn MA, Pivonka E. Overview of the health benefits of fruit and vegetable consumption for the dietetics professional: selected literature. J Am Diet Assoc 2000;100:1511–21 [DOI] [PubMed] [Google Scholar]
- 20. Shephard RJ. Exercise and relaxation in health promotion. Sports Med 1997;23:211–17 [DOI] [PubMed] [Google Scholar]
- 21. Rehm J, Room R, Graham K, et al. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction 2003;98:1209–28 [DOI] [PubMed] [Google Scholar]
- 22. Smith C, Hancock H, Blake-Mortimer J, et al. A randomised comparative trial of yoga and relaxation to reduce stress and anxiety. Complement Ther Med 2007;15:77–83 [DOI] [PubMed] [Google Scholar]
- 23. Sharma R, Gupta N, Bijlani RL. Effect of yoga based lifestyle intervention on subjective well-being. Indian J Physiol Pharmacol 2008;52:123–31 [PubMed] [Google Scholar]
- 24. Chen KM, Chen MH, Chao HC, et al. Sleep quality, depression state, and health status of older adults after silver yoga exercises: cluster randomized trial. Int J Nurs Stud 2009;46:154–63 [DOI] [PubMed] [Google Scholar]
- 25. Ross A, Thomas S. The health benefits of yoga and exercise: a review of comparison studies. J Altern Complement Med 2010;16:3–12 [DOI] [PubMed] [Google Scholar]
- 26. Cancelliere C, Cassidy JD, Ammendolia C, et al. Are workplace health promotion programs effective at improving presenteeism in workers? A systematic review and best evidence synthesis of the literature. BMC Public Health 2011;11:395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kuoppala J, Lamminpaa A, Husman P. Work health promotion, job well-being, and sickness absences–a systematic review and meta-analysis. J Occup Environ Med 2008;50:1216–27 [DOI] [PubMed] [Google Scholar]
- 28. Proper KI, Staal BJ, Hildebrandt VH, et al. Effectiveness of physical activity programs at worksites with respect to work-related outcomes. Scand J Work Environ Health 2002;28:75–84 [DOI] [PubMed] [Google Scholar]
- 29. Conn VS, Hafdahl AR, Cooper PS, et al. Meta-analysis of workplace physical activity interventions. Am J Prev Med 2009;37:330–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pronk NP, Boyle RB, O'Connor PJ. The association between physical fitness and diagnosed chronic disease in health maintenance organization members. Am J Health Promot 1998;12:300–6 [DOI] [PubMed] [Google Scholar]
- 31. Ni Mhurchu C, Aston LM, Jebb SA. Effects of worksite health promotion interventions on employee diets: a systematic review. BMC Public Health 2010;10:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Shephard RJ. PAR-Q, Canadian Home fitness test and exercise screening alternatives. Sports Med 1988;5:185–95 [DOI] [PubMed] [Google Scholar]
- 33. American College of Sports Medicine Position Stand The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc 1998;30:975–91 [DOI] [PubMed] [Google Scholar]
- 34. Pollock ML, Gaesser GA, Butcher JD, et al. ACSM position stand: the recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Indianapolis, IL: American Collega of Sport Medicine (ACSM), 1998:975–91 Report No.: 30(6). [DOI] [PubMed] [Google Scholar]
- 35. Wendel-Vos GC, Schuit AJ, Saris WH, et al. Reproducibility and relative validity of the short questionnaire to assess health-enhancing physical activity. J Clin Epidemiol 2003;56:1163–9 [DOI] [PubMed] [Google Scholar]
- 36. Ainsworth BE, Haskell WL, Leon AS, et al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc 1993;25:71–80 [DOI] [PubMed] [Google Scholar]
- 37. Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 2000;32(9 Suppl):S498–504 [DOI] [PubMed] [Google Scholar]
- 38. Hildebrandt VH, Ooijendijk WTM, Hopman-Rock M. Trendreport Physical Activity and Health (In Dutch). Leiden, The Netherlands: TNO Quality of Life, 2007 [Google Scholar]
- 39. Parker SJ, Strath SJ, Swartz AM. Physical activity measurement in older adults: relationships with mental health. J Aging Phys Act 2008;16:369–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Anonymous. MeterPlus Software [Computer Programme]. Version 4.2. La Jolla, CA, U.S.A: Santech, Inc, 2010 [Google Scholar]
- 41. Freedson PS, Melanson E, Sirard J. Calibration of the computer science and applications, inc. accelerometer. Med Sci Sports Exerc 1998;30:777–81 [DOI] [PubMed] [Google Scholar]
- 42. van Assema P, Brug J, Ronda G, et al. A short Dutch questionnaire to measure fruit and vegetable intake: relative validity among adults and adolescents. Nutr Health 2002;16:85–106 [DOI] [PubMed] [Google Scholar]
- 43. Laukkanen RMT, Oja P, Ojala KH, et al. Feasibility of a 2-km walking test for fitnes assessment in a population study. Scand J Soc Med 1992;20:119–25 [DOI] [PubMed] [Google Scholar]
- 44. Oja P, Laukkanen R, Pasanen M, et al. A 2-km walking test for assessing the cardiorespiratory fitness of healthy adults. Int J Sports Med 1991;12:356–62 [DOI] [PubMed] [Google Scholar]
- 45. Oja P, Mänttäri A, Pokki T, et al. UKK Walk Test—Tester's guide. Tampere, Finland: UKK Institute, 2001 [Google Scholar]
- 46. van der Zee KI, Sanderman R. Het Meten van Gezondheidstoestand Met De RAND-36: Een Handleiding. Groningen: Noordelijk Centrum voor Gezondheidsvraagstukken, 1993 [Google Scholar]
- 47. van Veldhoven MJ, Broersen S. Measurement quality and validity of the “need for recovery scale”. Occup Environ Med 2003;60(Suppl 1):i3–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Field A. Discovering statistics using SPSS. 3rd edn London: Sage Publications, 2009 [Google Scholar]
- 49. Strijk JE, Proper KI, van der Beek AJ, et al. A process evaluation of a worksite vitality intervention among ageing hospital workers. Int J Behav Nutr Phys Act 2011;8:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol 2010;63:e1–37 [DOI] [PubMed] [Google Scholar]
- 51. The Consolidated Standards of Reporting Trials (CONSORT) group The CONSORT Statement For Reporting of a Randomized Controlled Trial (RCT). Box 6-Intention-to-Treat Analysis. 2011. Ref Type: Internet Communication. (http://www.consort-statement.org/consort-statement/further-explanations/box6_intention-to-treat-analysis/) [Google Scholar]
- 52. Hollis S, Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ 1999;319:670–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Azur MJ, Stuart EA, Frangakis C, et al. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res 2011;20:40–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. van Buuren S. Multiple imputation of discrete and continuous data by fully conditional specification. Stat Methods Med Res 2007;16:219–42 [DOI] [PubMed] [Google Scholar]
- 55. Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley & Sons, 1987 [Google Scholar]
- 56. Proper KI, Koning M, van der Beek AJ, et al. The effectiveness of worksite physical activity programs on physical activity, physical fitness, and health. Clin J Sport Med 2003;13:106–17 [DOI] [PubMed] [Google Scholar]
- 57. Dugdill L, Brettle A, Hulme C, et al. Workplace physical activity interventions: a Sytematic review. IJWHM 2008;1:20–40 [Google Scholar]
- 58. Pedersen MT, Blangsted AK, Andersen LL, et al. The effect of worksite physical activity intervention on physical capacity, health, and productivity: a 1-year randomized controlled trial. J Occup Environ Med 2009;51:759–70 [DOI] [PubMed] [Google Scholar]
- 59. van Poppel MN, Chinapaw MJ, Mokkink LB, et al. Physical activity questionnaires for adults: a systematic review of measurement properties. Sports Med 2010;40:565–600 [DOI] [PubMed] [Google Scholar]
- 60. Alinia S, Lassen AD, Krogholm KS, et al. A workplace feasibility study of the effect of a minimal fruit intervention on fruit intake. Public Health Nutr 2010:1–6 [DOI] [PubMed] [Google Scholar]
- 61. Krogholm KS, Bredsdorff L, Alinia S, et al. Free fruit at workplace intervention increases total fruit intake: a validation study using 24 h dietary recall and urinary flavonoid excretion. Eur J Clin Nutr 2010;64:1222–8 [DOI] [PubMed] [Google Scholar]
- 62. Agudo A, Slimani N, Ocke MC, et al. Vegetable and fruit consumption in the EPIC cohorts from 10 European countries. IARC Sci Publ 2002;156:99–103 [PubMed] [Google Scholar]
- 63. World Health Organisation (WHO) Diet, Nutrition and the Prevention of Chronic Diseases: report of a joint WHO/FAO expert consultation. Geneva, World Health Organisation (WHO), 2003 [Google Scholar]
- 64. Heederik D. Micro-epidemiology of the healthy worker effect? Occup Environ Med 2006;63:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Li CY, Sung FC. A review of the healthy worker effect in occupational epidemiology. Occup Med (Lond) 1999;49:225–9 [DOI] [PubMed] [Google Scholar]
- 66. Verdonk P, Hooftman WE, van Veldhoven MJ, et al. Work-related fatigue: the specific case of highly educated women in the Netherlands. Int Arch Occup Environ Health 2010;83:309–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. de Croon EM, Sluiter JK, Frings-Dresen MH. Need for recovery after work predicts sickness absence: a 2-year prospective cohort study in truck drivers. J Psychosom Res 2003;55:331–9 [DOI] [PubMed] [Google Scholar]
- 68. Salonen P, Arola H, Nygard CH, et al. Factors associated with premature departure from working life among ageing food industry employees. Occup Med (Lond) 2003;53:65–8 [DOI] [PubMed] [Google Scholar]
- 69. Brenner H, Ahern W. Sickness absence and early retirement on health grounds in the construction industry in Ireland. Occup Environ Med 2000;57:615–20 [DOI] [PMC free article] [PubMed] [Google Scholar]