Abstract
Objectives
The Coronary Heart Disease (CHD) Policy Model-China, a national scale cardiovascular disease computer simulation model, was used to project future impact of urbanization.
Methods
Populations and cardiovascular disease incidence rates were stratified into four submodels: North-Urban, South-Urban, North-Rural, and South-Rural. 2010 was the base year, and high and low urbanization rate scenarios were used to project 2030 populations.
Results
Rural-to-urban migration, population growth, and aging were projected to more than double cardiovascular disease events in urban areas and increase by 27.0–45.6% in rural areas. Urbanization is estimated to raise age-standardized coronary heart disease incidence by 73–81 per 100,000 and stroke incidence only slightly.
Conclusions
Rural-to-urban migration will likely be a major demographic driver of the cardiovascular disease epidemic in China.
Keywords: urbanization, migration, cardiovascular disease, China
INTRODUCTION
China’s urban population growth is driven mostly by internal migration, and the urban-rural migration following economic reforms in the 1980’s may represent the largest in history. The proportion of Chinese living in cities increased from 26% to 45% from 1990–2010, and will reach close to 60% by 2030 (Figure). (United Nations Population Division 2009)
Figure. Past and projected evolution of total, urban and rural populations, China, 1950–2005 assumed for the analysis.
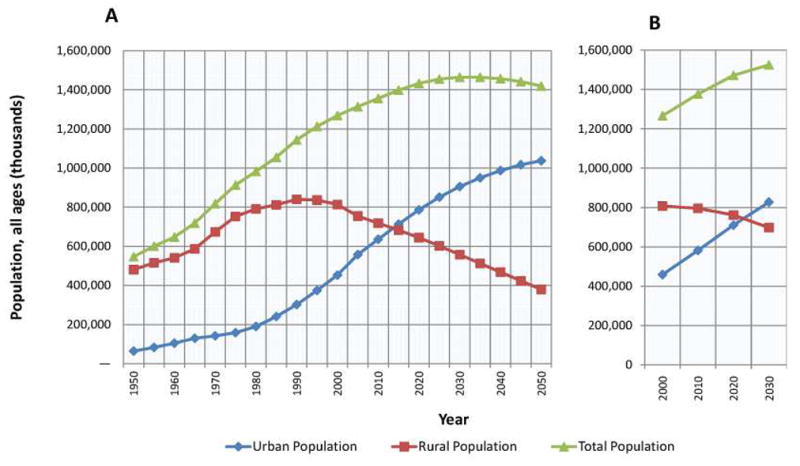
Panel A shows United Nations urbanization forecast [logistic regression trend; (Source: 2009 Urbanization Prospects, 2009 revision, United Nations)]. Panel B shows linear trend forecast (Liu 2003).
Prevalence of high cholesterol and diabetes and mortality from coronary heart disease (CHD) are higher in urban compared with rural China.(Gu et al. 2005; He et al. 2005) Stroke mortality is higher in rural areas. Forecasting future cardiovascular disease burden in China’s urban and rural areas may guide allocation of treatment and preventive services. We used a simulation model to project the potential impact of urbanization on the number of cardiovascular disease events and incidence rates in China in 2010 and 2030. The objective of the analysis was to project the potential impact of urbanization, assuming that rural migrants to urban areas eventually assume the same risk as urban residents. It was assumed that the change in risk with increasing urbanization was mediated by lifestyle, followed by risk factor changes. We therefore did not simulate urbanization and risk factor changes additively.
METHODS
The CHD Policy Model-China is a computer simulation model of cardiovascular disease, defined as CHD and total (ischemic and hemorrhagic) stroke, in Chinese adults ages 35–85 years (Appendix).(Moran et al. 2010; Moran et al. 2008) The national model started with CHD and stroke incidence from the China Hypertension Epidemiology Survey Follow-up Study (CHEFS, a prospective cohort study of 158,666 adults from 17 diverse provinces followed from 1991–2000; details in the Appendix) using a multi-stage process of case identification, verification, and adjudication. Cases were classified according to the International Classification of Diseases, Ninth Revision (ICD-9). For this analysis, strokes were defined by ICD-9 codes 430–438. Coronary Heart Disease events were defined as myocardial infarction (ICD-9 410, 412 or ICD-10 I21, I22), angina and other CHD (ICD-9 411, 413 and 414, or IC-10 I20, I23–I25), and a recommended fixed proportion of “ill-defined” cardiovascular disease coded events and deaths (ICD-9 codes 427.1, 427.4, 427.5, 428, 429.0, 429.1, 429.2, 429.9, 440.9 or ICD-10 I47.2, I49.0, I46, I50, I51.4, I51.5, I51.9, and I70.9).(Lozano 2001; Moran et al. 2010; Moran et al. 2008)
National stroke and IHD incidence rates were calibrated to fit age-specific mortality rates in 2002 and with national cause-specific mortality estimates over the years 2000–2010 (Appendix).(Moran et al. 2010; Moran et al. 2008) CHEFS sampled urban and rural sites in North and South China (above and below the Yangtze River). Urban areas were defined as equally or more populated than their local county’s capital, and rural areas as areas less populated than the capital.
For this analysis, CHD Policy Model-China was stratified into four demographic submodels: North/urban, North/rural, South/urban, and South/rural. Submodels were assigned relative rates of CHD and stroke among the same strata in CHEFS, then calibrated to match national incidence and mortality rates in 2010. Submodel age- and sex- specific cardiovascular disease rates were held constant for the 2030 projection, and it was assumed that implicit in urban cardiovascular disease rates was exposure to urban risk factor levels (examples, Appendix Table 1). Submodel populations for 2010 were obtained from the United Nations (U.N.) Population Division. (United Nations Population Division 2009) Two 2030 population scenarios were simulated: 1) a low urbanization rate projection from the linear regression analysis of Liu et al.,(Figure, panel B)(Liu 2003) and 2) a high urbanization rate projection using logistic regression from the U.N.(Figure, panel A). (United Nations Population Division 2009) Both projection methods used Chinese Census definitions of urban and rural. U.N. 2005 urban and rural age structures were applied to the urban and rural projections, respectively; these age structures corresponded well with 2030 urban and rural estimates for China by Cao et al.(Cao 2012)
Projected populations were entered into demographic submodels, and incident CHD and stroke events simulated. Projected populations and incident cardiovascular disease events are reported for 2010 and 2030. Incidence rates were directly age-standardized to the U.N. 2010 Chinese population using 10-year age categories.
Projected incident stroke and CHD events in Chinese adults from the urbanization scenarios were compared with two other scenarios: one assuming only demographic changes (aging and population growth alone; no urbanization effects), and a second assuming the projection of recent cardiovascular disease risk factor trends up to 2030 from a past analysis (Appendix Table 2).(Moran et al. 2010)
RESULTS
In 2010, China was still predominantly rural (44.9% urban, Table 1, Figure). Except for stroke in rural Northern China, cardiovascular disease rates were generally higher in urban areas. By 2030, the absolute size of China’s urban population will increase by a half or more and comprise 54.3–60.4% of the population. While overall adult rural populations will decline or increase only slightly, the younger adult rural population will decrease by 18–30% (Table 1, Figure). At the same time, the urban population aged 55–84 years will more than double by 2030 (increase by 120–146%) and the rural population the same age will increase by only 32–51%.
Table 1.
Projected populations and coronary heart disease (CHD) and stroke events by demographic category, total population and age-stratified, Chinese adults aged 35–84 years in 2010 and 2030.
| Urban
|
Rural
|
All of China
|
|||
|---|---|---|---|---|---|
| North | South | North | South | Totals | |
| 2010 | |||||
| Population | |||||
| Ages 35–84 years | 123,857,642 | 169,366,434 | 150,281,873 | 209,114,947 | 652,620,896 |
| Ages 35–54 years | 81,548,794 | 111,512,122 | 91,945,410 | 127,940,644 | 412,946,971 |
| Ages 55–84 years | 42,308,847 | 57,854,312 | 58,336,463 | 81,174,303 | 239,673,925 |
| CHD | |||||
| Total | |||||
| Incident events | 358,000 | 235,000 | 339,000 | 142,000 | 1,384,000 |
| Crude rate (per 100,000) | 286 | 137 | 223 | 67 | 164 |
| Age 35–54 | |||||
| Incident events | 61,000 | 37,000 | 72,000 | 15,000 | 185,000 |
| Crude rate (per 100,000) | 75 | 33 | 79 | 12 | 45 |
| Age 55–84 | |||||
| Incident events | 297,000 | 198,000 | 266,000 | 127,000 | 888,000 |
| Crude rate (per 100,000) | 702 | 342 | 456 | 156 | 370 |
| Stroke | |||||
| Total | |||||
| Incident events | 1,196,000 | 1,080,000 | 1,646,000 | 1,235,000 | 5,120,000 |
| Crude rate (per 100,000) | 966 | 637 | 1,095 | 591 | 790 |
| Age 35–54 | |||||
| Incident events | 302,000 | 184,000 | 392,000 | 166,000 | 559,000 |
| Crude rate (per 100,000) | 370 | 164 | 427 | 130 | 253 |
| Age 55–84 | |||||
| Incident events | 894,000 | 896,000 | 1,254,000 | 1,068,000 | 2,322,000 |
| Crude rate (per 100,000) | 2,113 | 1,550 | 2,149 | 1,316 | 1,716 |
| 2030 | |||||
| Population | |||||
| Ages 35–84 years | |||||
| High urbanization projection | 215,030,000 | 294,039,000 | 144,499,000 | 201,067,000 | 854,636,000 |
| Low urbanization projection | 192,102,000 | 262,685,000 | 167,197,000 | 232,652,000 | 854,636,000 |
| % Change (range) | (53.2–71.5) | (53.2–71.5) | (−4.9–10.0) | (−4.9–10.0) | |
| Ages 35–54 years | |||||
| High urbanization projection | 106,211,000 | 145,236,000 | 64,634,000 | 89,938,000 | 406,019,000 |
| Low urbanization projection | 94,885,000 | 129,749,000 | 75,732,223 | 105,380,000 | 405,746,546 |
| % Change (range) | (16.4–30.2) | (16.4–30.2) | (−29.7– −17.6) | (−29.7– −17.6) | |
| Ages 55–84 years | |||||
| High urbanization projection | 104,184,000 | 142,465,000 | 77047000 | 107,210,000 | 430,906,000 |
| Low urbanization projection | 93,075,000 | 127,273,000 | 88238711 | 122,783,000 | 431,370,000 |
| % Change (range) | (120.0–146.3 | (120.0–146.3) | (32.1–51.3) | (32.1–51.3) | |
| Incident CHD | |||||
| Ages 35–84 years | |||||
| High urbanization projection | 840,000 | 554,000 | 416,000 | 187,000 | 1,998,000 |
| Low urbanization projection | 751,000 | 495,000 | 477,000 | 215,000 | 1,938,000 |
| % Change (range) | (109.6–134.7) | (111.0–136.2) | (23.5–41.7) | (32.2–51.5) | (80.6–86.2) |
| Ages 35–54 years | |||||
| High urbanization projection | 81,000 | 50,000 | 51,000 | 11,000 | 193,000 |
| Low urbanization projection | 73,000 | 45,000 | 59,000 | 13,000 | 189,000 |
| % Change (range) | (19.2–33.4) | (20.4–34.8) | (−28.8– −17.7) | (−27.8– −16.35) | (2.2–4.4) |
| Ages 55–84 years | |||||
| High urbanization projection | 759,000 | 505,000 | 364,000 | 176,000 | 1,805,000 |
| Low urbanization projection | 678,000 | 451,000 | 417,000 | 202,000 | 1,748,000 |
| % Change (range) | (128.2–155.4) | (128.0–155.2) | (36.9–59.6) | (39.3–59.5) | (103.3–96.6) |
| Incident stroke | |||||
| Ages 35–84 years | |||||
| High urbanization projection | 2,699,000 | 2,599,000 | 2,032,000 | 1,634,000 | 8,963,000 |
| Low urbanization projection | 2,411,000 | 2,321,000 | 2,332,000 | 1,872,000 | 8,936,000 |
| % Change (range) | (101.6–125.6) | (115.0–140.7) | (23.5–41.7) | (32.3–51.6) | (73.3–73.8) |
| Ages 35–54 years | |||||
| High urbanization projection | 409,000 | 251,000 | 285,000 | 122,000 | 1,067,000 |
| Low urbanization projection | 366,000 | 225,000 | 330,000 | 140,000 | 1,061,000 |
| % Change (range) | (21.1–35.5) | (22.7–37.3) | (−27.5– −15.8) | (−27.0–15.8) | (1.6–2.2) |
| Ages 55–84 years | |||||
| High urbanization projection | 2,289,000 | 2,347,000 | 1,747,000 | 1,512,000 | 7,896,000 |
| Low urbanization projection | 2,045,000 | 2,097,000 | 2,001,000 | 1,732,000 | 7,875,000 |
| % Change (range) | (128.8–156.1) | (161.8–133.9) | (39.4–59.6) | (41.5–62.1) | (91.5–92.0) |
Because the entire population will grow and age, cardiovascular disease events were projected to increase in all demographic strata between 2010 and 2030 except for adults aged 35–54 years (Table 1). Cardiovascular disease events were projected to increase overall by 27.0–45.6% in rural areas and to more than double in number in urban areas. It was notable that in the age 35–54 age group, the number of rural CHD and stroke events decreased between 2010–2030, while urban events increased. Urbanization was projected to increase national age-standardized CHD incidence from 164.4 to 237.0–244.9 per 100,000. Age-standardized stroke rates were projected to increase only slightly (ranging in the two urbanization scenarios from 790.1 to 801.1–830.9 per 100,000).
Compared with the base case scenario assuming no urbanization effects, urbanization scenarios resulted in 13–16% more incident CHD events and 17% more stroke events (Table 2). Urbanization projection results were the similar to slightly less than prior national risk factor trend scenario projections.
Table 2.
Comparison of projected coronary heart disease (CHD) and stroke events in China, 2030 from three scenarios: demographic changes without change in % urban, demographic changes plus urbanization scenarios projected in the analysis, and demographic changes plus risk factor trends (Moran et al. 2010).
| Demographic and/or risk factor scenario | Projections for 2030 [number of events (% higher than 2030 estimate assuming demographic changes only)] | |
|---|---|---|
| CHD events | Stroke events | |
| Demographic changes only (aging and population growth) | 1,718,000 | 7,656,000 |
|
| ||
| Demographic changes plus urbanization trend | ||
| High urbanization projection | 1,998,000 (16.3) | 8,963,000 (16.7) |
| Low urbanization projection | 1,938,000 (12.8) | 8,936,000 (17.1) |
|
| ||
| Demographic changes plus risk factor trends | ||
| Projected trends in blood pressure, total cholesterol, diabetes; smoking decline | 1,958,952 (14.0) | 8,989,000 (17.4) |
| Projected trends in blood pressure, total cholesterol, diabetes; no smoking decline | 2,077,000 (20.9) | 9,034,000 (18.0) |
DISCUSSION
Assuming rural-to-urban population shifts, population growth, aging, and constant cardiovascular disease risk factors and rates within demographic strata, we projected that incident cardiovascular disease event numbers will more than double in China’s cities between 2010 and 2030. Urbanization was projected to increase age-standardized national CHD rates more markedly than stroke rates.
In a prior analysis, we projected that annual cardiovascular disease events will increase by >50% between 2010 and 2030 due to population growth and aging alone, and that continued adverse national trends in risk factors along with a steady decline in active smoking would add at least an additional 20% increase.(Moran et al. 2010) Blood pressure, body mass index, and cholesterol have been shown to increase in migrants from rural to urban China.(He et al. 1991; He et al. 1996; Stamler 1991) Comparing numbers of incident events projected for 2030, national CHD increases projected incremental to aging effects in urbanization scenarios (13–16% additional incident events) were close to main but less than pessimistic national risk factor trend forecasts (range 14–21%), while stroke increases predicted in urbanization scenarios explained close to the 17–18% stroke event numbers increase predicted by main risk factor trend forecasts. Our simulations may have overestimated future CHD and stroke events in China due to failure to account for lag time between migration (which can lead to relatively rapid changes in risk factor exposures) and real increase in CHD risk. We also did not account for the possibilities that continued economic development may reduce cardiovascular disease or that increased mobility and rural development might lead to the adaptation of “urban” lifestyles and risks in rural areas.
An implicit assumption of this analysis is that risk factors and consequently cardiovascular risk changes quickly in rural-to-urban migrants. One example of relatively rapid change in a risk factor is blood pressure change with migration. Urban migrants in China were found to have 6.0 to 7.0 mm Hg higher systolic blood pressure compared with their rural counterparts.(He et al. 1991) The Kenya Luo study found that substantial blood pressure changes (and corresponding increases in urinary sodium excretion) were found one year after rural-to-urban migration.(Poulter et al. 1984; Poulter et al. 1990) Changes in cholesterol numbers are presumed to occur just as rapidly. Change in body mass index appears to occur more gradually. Migration studies consistently show a relative increase of 1.0 to 1.7 kg/m2 body mass index by 15 years after migration.(Goel et al. 2004; Sanchez-Vaznaugh et al. 2008) Urban Yi urban migrants in China had 0.6 kg/m2 higher body mass index compared with Yi farmers, similar to other urban/rural comparison studies.(He et al. 1994) This difference is supported in comparing mean body mass index between urban and rural China in a national survey.(Gu et al. 2005).
Active smoking prevalence remains >50% in urban and rural adult Chinese men. (World Health Organization Global Adult Tobacco Survey (GATS) 2010) Our risk factor-based projections for 2030 suggest that smoking trends are as important as urbanization in determining future cardiovascular disease in China. Whjle national surveys demonstrated a decline in active smoking prevalence between 1996 and 2010,(GATS 2010; Gu et al. 2004) a continued decline is not guaranteed, and the specter of increased female smoking prevalence remains a possibility.
China faces a cardiovascular disease epidemic driven mainly by population aging and growth, but potentially augmented by rural-to-urban migration and urbanization. Urbanization scenarios simulated in our analysis suggest that in future decades population and cardiovascular disease events will concentrate in cities. For CHD in particular, it may make sense to focus prevention efforts on urban populations. Projecting disease burden in urban and rural areas of China may guide resource allocation and target prevention efforts.
Supplementary Material
Acknowledgments
Grants and financial support: This study was supported by a Columbia University Earth Institute Cross-Cutting Initiative grant to Drs. Adamo and Moran and Mentored Career Development Award number K08HL089675 from the United States National Heart, Lung, and Blood Institute of the NIH to Dr. Moran.
Footnotes
Ethics Compliance
The authors have no conflicts of interest to report.
References
- Source: United Nations, Department of Economic and Social Affairs, Population Division. World Urbanization Prospects: The 2009 Revision. 2010. [Google Scholar]
- Cao GY, Chen G, Pang LH, Zheng XY, Nilsson S. Urban growth in China: past, prospect, and its impacts. Popul Environ. 2012;33:137–160. [Google Scholar]
- World Health Organization. Global Adult Tobacco Survey (GATS) 2010. [Google Scholar]
- Goel MS, McCarthy EP, Phillips RS, Wee CC. Obesity among US immigrant subgroups by duration of residence. JAMA. 2004;292(23):2860–2867. doi: 10.1001/jama.292.23.2860. [DOI] [PubMed] [Google Scholar]
- Gu D, Gupta A, Muntner P, Hu S, Duan X, Chen J, Reynolds RF, Whelton PK, He J. Prevalence of cardiovascular disease risk factor clustering among the adult population of China: results from the International Collaborative Study of Cardiovascular Disease in Asia (InterAsia) Circulation. 2005;112(5):658–665. doi: 10.1161/CIRCULATIONAHA.104.515072. [DOI] [PubMed] [Google Scholar]
- Gu D, Wu X, Reynolds K, Duan X, Xin X, Reynolds RF, Whelton PK, He J. Cigarette smoking and exposure to environmental tobacco smoke in China: the international collaborative study of cardiovascular disease in Asia. Am J Public Health. 2004;94(11):1972–1976. doi: 10.2105/ajph.94.11.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He J, Gu D, Wu X, Reynolds K, Duan X, Yao C, Wang J, Chen CS, Chen J, Wildman RP, et al. Major causes of death among men and women in China. The New England journal of medicine. 2005;353(11):1124–1134. doi: 10.1056/NEJMsa050467. [DOI] [PubMed] [Google Scholar]
- He J, Klag MJ, Whelton PK, Chen JY, Mo JP, Qian MC, Mo PS, He GQ. Migration, blood pressure pattern, and hypertension: the Yi Migrant Study. Am J Epidemiol. 1991;134(10):1085–1101. doi: 10.1093/oxfordjournals.aje.a116012. [DOI] [PubMed] [Google Scholar]
- He J, Klag MJ, Whelton PK, Chen JY, Qian MC, He GQ. Body mass and blood pressure in a lean population in southwestern China. Am J Epidemiol. 1994;139(4):380–389. doi: 10.1093/oxfordjournals.aje.a117010. [DOI] [PubMed] [Google Scholar]
- He J, Klag MJ, Wu Z, Qian MC, Chen JY, Mo PS, He QO, Whelton PK. Effect of migration and related environmental changes on serum lipid levels in southwestern Chinese men. Am J Epidemiol. 1996;144(9):839–848. doi: 10.1093/oxfordjournals.aje.a009018. [DOI] [PubMed] [Google Scholar]
- Liu S, Li X, Zhang M. Scenario Analysis on Urbanization and Rural-Urban Migration in China, International Institute for Applied Systems Analysis, Interim Report IR-03–036. Interim Report IR-03–036 2003 [Google Scholar]
- Lozano R, Murray CJL, Lopez AD, Satoh T. Global Programme on Evidence for Health Policy Working Paper No 12. Geneva: World Health Organization; 2001. Miscoding and misclassification of ischaemic heart disease mortality. [Google Scholar]
- Moran A, Gu D, Zhao D, Coxson P, Wang YC, Chen CS, Liu J, Cheng J, Bibbins-Domingo K, Shen YM, et al. Future cardiovascular disease in china: markov model and risk factor scenario projections from the coronary heart disease policy model-china. Circ Cardiovasc Qual Outcomes. 2010;3(3):243–252. doi: 10.1161/CIRCOUTCOMES.109.910711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran A, Zhao D, Gu D, Coxson P, Chen CS, Cheng J, Liu J, He J, Goldman L. The future impact of population growth and aging on coronary heart disease in China: projections from the Coronary Heart Disease Policy Model-China. BMC public health. 2008;8:394. doi: 10.1186/1471-2458-8-394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulter N, Khaw KT, Hopwood BE, Mugambi M, Peart WS, Rose G, Sever PS. Blood pressure and its correlates in an African tribe in urban and rural environments. J Epidemiol Community Health. 1984;38(3):181–185. doi: 10.1136/jech.38.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulter NR, Khaw KT, Hopwood BEC, Mugambi M, Peart WS, Rose G, Sever PS. THE KENYAN LUO MIGRATION STUDY - OBSERVATIONS ON THE INITIATION OF A RISE IN BLOOD-PRESSURE. British Medical Journal. 1990;300(6730):967–972. doi: 10.1136/bmj.300.6730.967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez-Vaznaugh EV, Kawachi I, Subramanian SV, Sanchez BN, Acevedo-Garcia D. Differential effect of birthplace and length of residence on body mass index (BMI) by education, gender and race/ethnicity. Soc Sci Med. 2008;67(8):1300–1310. doi: 10.1016/j.socscimed.2008.06.015. [DOI] [PubMed] [Google Scholar]
- Stamler J. The Yi Migrant Study: population exposures influencing blood pressure patterns. Epidemiology. 1991;2(2):83–87. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


