Abstract
Basophils are of interest in immunology due to their ability to produce a Th2-signature cytokine, IL-4, following activation. New understanding of the role of basophils in immunity shows novel functions at a cellular level through which basophils influence adaptive immunity. This review summarizes new advances in basophil biology and discusses new roles for basophils in human disease, especially in the mediation of the pathogenesis of lupus nephritis. Recently, basophils have been shown to contribute to self-reactive antibody production in systemic lupus erythematosus and may enhance pre-existing loss of B cell tolerance, suggesting that basophils, IL-4 and IgE mediate the pathogenesis of lupus nephritis by promoting the Th2 environment and activating autoreactive B cells. In addition to envisaging exciting therapeutic prospects, these novel findings open the way for the study of basophils in other autoimmune and renal diseases.
INTRODUCTION
Basophils are bone marrow-derived basophilic granulocytes that contain large cytoplasmic granules and 2–3 lobed nuclei. They constitute less than 0.3% of the total nucleated cells in the bone marrow and are the least-abundant granulocytes found in the circulation (1). Since the discovery of basophils more than 130 years ago, they have been implicated in many types of allergic inflammatory responses. Earlier studies using a guinea-pig model of cutaneous hypersensitivity found that basophils reach tissue sites where they are triggered by antigens to release mediators (2). Basophils have also been shown to confer resistance against ectoparasite infections (3). During Amblyomma americanum tick infection in calves, significant decreases in feeding are associated with cutaneous basophil infiltration and blood basophilia (4). Transfer of anti-basophil serum abolishes resistance to tick infection in guinea pigs (5). Nevertheless, a tool to identify or selectively purify basophils has not been available until recently. Studies in the last 7 years have made significant progress in identifying the biologic functions of basophils, a list which continues to grow (see below for details). Surface phenotypes to analyze and purify basophils have been extensively characterized: FcεRI+ CD49b+ CD203c+ Thy1+ ckit- FcγR+ CD45intermediate (6). Animal models to study basophil functions in vivo have been developed. Most importantly, genetically-engineered basophil-deficient animals have recently been generated (7, 8). We are now beginning to understand novel functions of basophils at the cellular level, through which they influence adaptive immunity. This review summarizes new advances in basophil biology and novel roles for basophils in human disease, particularly their mediation in the pathogenesis of lupus nephritis.
IL-3 IS A KEY FACTOR FOR BASOPHIL DEVELOPMENT
Interleukin (IL)-3 is involved in the differentiation of early precursors into fully mature basophils in the bone marrow and spleen (9, 10). Because basophil differentiation is controlled at a transcriptional level by differential expression of two key transcription factors, C/EBPα and GATA2 (11), IL-3 may regulate expression of these factors, influencing fate-decision during early development. IL-3-deficiency results in significant defects in the generation of basophils in the course of Th2 immunity (12, 13). Nonetheless, the basal production of basophils in naïve IL-3-deficient mice is similar to that in wild-type mice (12). Therefore, the role of IL-3 in basophil development during steady-state conditions and immune responses is likely to differ. Basophil differentiation in steady-state conditions could be IL-3-independent; however, IL-3 becomes the major factor enhancing basophil generation in the bone marrow under Th2 associated inflammatory conditions (13).
FACTORS INVOLVED IN BASOPHIL ACTIVATION
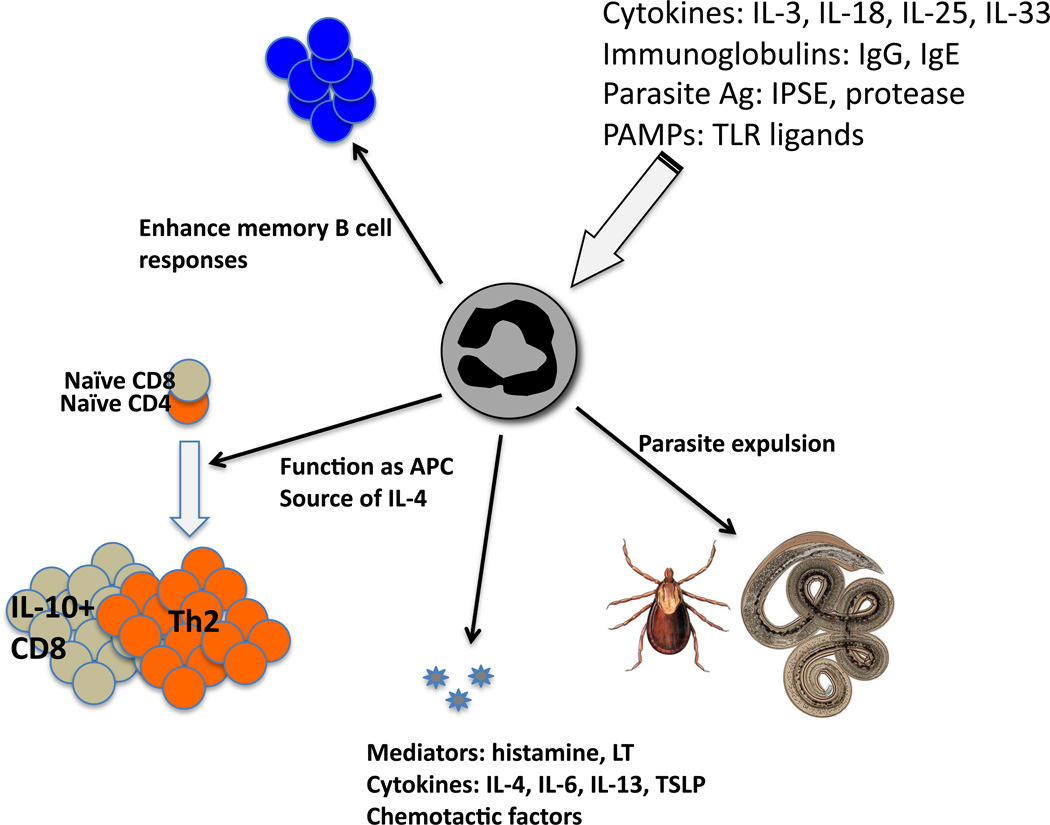
The list of factors that positively and negatively regulate basophil activation continues to grow (Figure 1). The primary action of IL-3 on mature basophils is to enhance IL-4 production (14–16). IL-3 also primes basophils to augment IL-4 production in response to other stimuli (15). Ig receptor (FcR) cross-linking induces both IL-4 and IL-13 production and histamine release in basophils (17); preincubation of basophils with IL-3 or the addition of IL-3 during stimulation significantly enhances cytokine production (15, 18). Both IL-18 and IL-33, members of the IL-1 family of cytokines, stimulate IL-4 and IL-13 production independently of FcR cross-linking (18–20). Notably, basophil survival significantly increases when stimulated with IL-18 or IL-33 by a PI3K/Akt-dependent pathway (21). IL-3 enhances basophil survival in vitro, although no in vivo effect on survival was observed (13). IL-25, a member of the IL-17 family of cytokines, plays a crucial role in developing Th2 immune responses (22). Basophils from patients with seasonal allergic rhinitis express high levels of IL-17RB, a receptor for IL-25 (23). In fact, IL-25 stimulation inhibits basophil apoptosis and enhances IgE-mediated degranulation, indicating the possible involvement of IL-25 in basophil activation and Th2 immunity (23).
Figure 1.
Potential functions of basophils stimulated via multiple pathways are illustrated. LT, leukotriene; TSLP, thymic stromal lymphopoietin; IPSE, PAMP, pathogen associated molecular pattern; TLR, Toll like receptor.
Basophils express receptors involved in innate immunity, including TLR2 and TLR4 (24–26). Stimulation of basophils with LPS increases cytokine production through FcR-dependent or independent pathways (26). Antigens associated with parasites are known to have basophil activating properties. IPSE/alpha-1, a glycoprotein from Schistosoma egg antigens (SEA) induces IL-4 production in basophils (27). Protease antigens such as papain and house dust mite antigens also activate basophil cytokine production (28, 29), although the underlying mechanism is not clear. Antigens from pathogens also modulate basophil functions. Helicobacter pylori-derived cecropin-like peptide (Hp(2–20)) induces basophil chemotaxis (30). HIV glycoprotein gp120 induces IL-4 and IL-13 release from human basophils through interaction with the VH3 region of IgE (31). Complement C5a induces strong IgE-independent production of cytokines and mediators from basophils (32).
Cytoplasmic signaling molecules and transcription factors that downregulate basophil activation are reported. Interferon regulatory factor 2 (IRF-2) inhibits basophil expansion. As a result, mice deficient in IRF-2 show marked basophilia and spontaneous Th2 differentiation (33). Lyn, a src kinase family member, dampens basophil expression of GATA-3 (34). Like IRF-2−/− mice, Lyn−/− mice present basophilia and constitutive Th2 effector CD4 T cells (34). SHIP, a negative regulator of the PI3K pathway, plays a key role in suppressing IL-4 production from basophils (35). Notably, Th2-prone immune responses found in these mice require both basophils and IL-4, further highlighting the importance of IL-4-dependent immune modulation by basophils. The surface antigens that negatively regulate basophil activation remain to be determined.
BASOPHIL FUNCTIONS IN VIVO
Th1 CD4 T cells mainly produce IFNγ, protecting hosts from intracellular pathogens, and factors inducing Th1 differentiation have been identified, including IL-12, IFNγ, and transcription factor T-bet (36). Th2 CD4 T cells produce IL-4, IL-5, and IL-13, protecting hosts from extracellular pathogens. IL-4 and transcription factor GATA-3 are key Th2 inducing factors. Unlike Th1 immunity, in which activated antigen-presenting DCs provide IL-12, which then program activated naïve CD4 T cells to Th1 lineage cells, the source of initial IL-4 necessary to initiate Th2 differentiation remains elusive. Studies using cytokine-reporter mice (4get or G4 mice) identified basophils as potential candidates for the role of Th2 inducers (37, 38). In vitro, stimulation of naïve CD4 T cells in the presence of basophils promotes Th2 differentiation without exogenous addition of IL-4 (39). A key mechanism of basophils that supports Th2 differentiation operates via IL-4, because basophils deficient in IL-4 or IL-4 neutralization abolish basophil-mediated Th2 differentiation (Figure 1).
Unlike CD4 T cells, CD8 T cells stimulated in the presence of basophils produce high levels of IL-10, which is not observed when T cells are stimulated by other APCs (40). Because basophils express MHC I molecules, they directly interact with and promote IL-10 production in CD8 T cells. IL-4 neutralization abolishes basophil-mediated IL-10 expression; however, recombinant IL-4 alone does not induce IL-10 in CD8 T cells, suggesting an additional factor in this process. IL-6 has a synergistic effect on CD8 T cell IL-10 expression when cocultured with IL-4, although IL-6 alone had no effect (40).
Basophils can also enhance B cell IgE production in vitro through the production of Th2 cytokines and CD40L expression (41, 42). It was recently reported that basophils efficiently capture intact antigens and enhance B cell activation, particularly B cell proliferation and Ig production (43). Both IL-4 and IL-6 produced by basophils are key cytokines that optimize CD4 T cell-dependent B cell help (43). In vivo, basophil-mediated effects on B cells are critical to mount protective humoral immunity against bacterial infection (44). In humans, circulating IgD bind to basophils, which induce B cell stimulating factors such as B cell-activating factor [BAFF; also known as B lymphocyte stimulator (BLyS)], IL-1, and IL-4 together with antimicrobial and opsonizing factors (44). Whether the IgD-mediated basophil activation pathway also operates in mice remains to be determined.
Basophil function as antigen presenting cells and the controversy
Studies show that basophils play critical roles as antigen-presenting cells during Th2 type responses (Figure 1). Basophils uptake exogenous protein antigens, process, and present them to naïve CD4 T cells via surface MHCII (45). Mice immunized with OVA protein plus protease papain developed OVA specific Th2 type immune responses. As papain injection recruits circulating basophils into the draining lymph nodes where basophils are found within T cell areas, it is suggested that basophils provide key signals (MHCII-Ag complexes plus IL-4) through which antigen-specific Th2 differentiation is optimized (45). Papain-mediated Th2 immune responses were not altered by CD11c+ DCs depletion. In fact, the transfer of antigen-pulsed basophils induces Th2 differentiation within CIITA-deficient mice, where resident APCs, including DCs, lack functional MHC II molecules (45). Basophils incubated with IL-3 plus antigen or antigen-IgE complexes induce development of antigen-specific Th2 cells and antigen-specific B cell responses in naïve mice and administration of antigen-IgE complexes induces Th2 differentiation only in the presence of endogenous basophils, suggesting basophils could function as potent antigen-presenting cells by capturing IgE complexes (24). A Trichuris muris infection model also demonstrated that DC-mediated immune priming is insufficient for the development of parasite-specific Th2 immunity using MHC II-CD11c transgenic mice in which MHC II expression is restricted to CD11c+ DCs (46). T. muris-specific Th2 immunity was substantially impaired in these mice, although Th1 differentiation was intact. Basophil depletion significantly impaired Th2 cytokine responses and parasite expulsion (46).
However, the role of basophils as Th2-inducing antigen presenting cells was recently challenged by three independent studies demonstrating that basophils are dispensable for Th2 induction (47–49). CD11c+ DC depletion dramatically reduced Th2 induction in mice challenged with schistosome egg antigens or infected with Schistosoma mansoni, but treatment with MAR-1 Ab had little or no effect on Th2 responses (47). Th2 cell differentiation was not impaired after papain/OVA immunization using basophil-deficient mice (49). In response to house dust mite (HDM) allergens, basophils play no role in Th2 immunity, but FcεRI+ CD11c+ DC subsets recruited into the draining lymph nodes were responsible for Th2 immunity (48).
The discrepancies in these studies require explanation. Experimental models may determine the contribution of basophils to subsequent T cell immunity. Basophil-independent (and DC-dependent) Th2 immunity could arise from more-complicated immunogens derived from parasites or multiple antigens, including HDM. In contrast, papain could act directly on basophils via cysteine protease activity, which then activates basophils, including antigen-presenting machineries. However, Th2 immunity raised from papain immunization requires DC-basophil cooperation (45). Alternatively, DC subsets expressing FcεRI may have been overlooked in studies using MAR-1 Ab. Thus, the defects observed following MAR-1 Ab could be due to DC depletion.
Basophil-deficient animals: new functions revealed
A transgenic mouse, Mcpt8Cre, was generated by expressing the Cre recombinase gene under the control of the Mcpt8 gene. Basophil numbers were constitutively lower in this animal, while other leukocytes such as peritoneal mast cells remained intact. In vivo Th2 responses, including alum-induced allergic lung inflammation, alum-induced humoral immune responses, and Ig-mediated passive systemic anaphylaxis, were normally induced. Furthermore, primary Th2 immune responses against intestinal nematode Nippostrongylus brasiliensis infection were not impaired without basophils (49), consistent with our recent report (50). In contrast, protective memory immune responses against secondary Nb infection were significantly impaired (49). Interestingly, lung infiltration of Th2 type CD4 T cells and eosinophils following Nb infection was not altered; instead, eosinophil recruitment into the draining mediastinal lymph node was greatly diminished without basophils, suggesting they may contribute to eosinophil recruitment (51). Karasuyama and colleagues independently generated Mcpt8DTR mice, in which basophils are conditionally depleted by transgenic expression of the human diphtheria toxin (DT) receptor under the control of the mast cell protease 8 (Mcpt8) promoter. A single injection of DT resulted in transient (yet highly efficient) depletion of basophils from the bone marrow, circulation, and spleen, while other cell types including mast cells were not affected. Using a tick infection model they demonstrated that basophil depletion resulted in loss of acquired tick resistance (7). Because Ig receptor expression on basophils, but not on mast cells, was necessary to confer protection, these results provide strong evidence supporting antibody-mediated acquired immunity by basophils against tick infection (Figure 1).
BASOPHIL MOBILIZATION: A KEY STEP FOR BASOPHIL FUNCTION IN VIVO
In steady-state conditions, the primary locations of basophils are the bone marrow and the circulation, while basophils are very-rarely found in secondary lymphoid tissues. A key step that allows basophils to contribute to Th2 immune responses is their transient mobilization into secondary lymphoid tissues. Basophils within draining lymph nodes are observed in many in vivo immune responses: immunization with protease antigens such as papain (29) and house dust mite antigens (48), and infection by Nippostrongylus brasililensis (50), Schistosoma mansoni (47), Trichuris muris (46), and ticks (7). Recruitment is only found in draining lymphoid tissues, suggesting active immune responses. IL-3 plays a crucial role in this recruitment process (50). Because IL-3 is primarily produced by activated T cells (13), antigen-induced T cell activation within local lymphoid tissues seems to be the primary underlying factor. In addition, recruitment is transient, only found between day 3 and 4 post-antigen challenge (29, 50). It is unclear how IL-3-derived basophil recruitment is tightly controlled, although IL-3-responsive cells have been shown to be bone marrow-derived cells (50). Likewise, recruited basophils are in close contact with T cells within the T cell zone (29). Basophils may function as antigen-presenting cells (24, 45, 46) and/or produce IL-4, creating an optimal microenvironment favoring Th2 differentiation. Basophils express chemokine receptors, including CCR1, CCR2, CCR3, CXCR1, CXCR3, and CXCR4 (52). Microarray study of basophils isolated from the lung of N. brasiliensis-infected mice showed that CCR2 is highly expressed on basophils (38). Whether IL-3-dependent basophil recruitment is chemokine-dependent and if so, which chemokines are involved in basophil recruitment remains to be determined.
BASOPHILS: FROM ALLERGY TO AUTOIMMUNITY
As basophils play an immunomodulatory role, provoking Th2 cell differentiation in vivo, it could be suggested that they might also play a leading role in immune diseases other than allergies. In addition to the finding of peripheral basophilia and constitutive Th2 skewing of CD4 T cells in lyn−/− mice, basophil involvement is also reported in autoimmune urticaria, where autoantibodies to the high affinity receptor FcεRIα induces basophil activation (53, 54). A Th2 component is well-described in autoimmune urticaria, and basophils contribute to the development of autoimmune symptoms through their immunomodulatory and effector responses. Reports show that, in some murine models, mast cells contribute to autoimmune arthritis (55). In this and other autoimmune diseases, mast cell effector and immunomodulatory functions initiate inflammation, while the enhancement of inflammation may be due to Th1 and Th17 cell responses. These CD4 T cell subsets are thought to be the primary effector cells involved in chronic inflammation in experimental autoimmune encephalomyelitis, a model of human multiple sclerosis, experimental autoimmune uveitis, a model of human posterior uveitis, and collagen-induced arthritis, a murine model of human rheumatoid arthritis (RA) (56).
While IgE is recognized as a human Th2 marker, some reports describe increased levels of IgE in the setting of Th1 and Th17 responses in patients with autoimmune disease (57–59). Although the significance of Th1- and Th17-driven responses in the development of autoimmunity is evident, it seems improbable that Th2 responses do not contribute to the disease. Furthermore, allergy and autoimmunity share various features such as manifestations associated with autoantibody production and circulating immune complex (CIC) formation (60). Studies report a common structure of some allergens and autoantigens (61), and suggest that numerous environmental allergens have common structural conformations with self-antigens, which could explain the development of autoimmune diseases like chronic urticaria. However, as discussed later, increased IgE levels are not associated with increased allergic disease in other autoimmune diseases, such as systemic lupus erythematosus (SLE) (57).
The recent finding that IgD-mediated basophil activation by a yet unidentified receptor is relevant to some chronic autoinflammatory diseases such as hyper IgD syndrome, tumor necrosis factor receptor-associated periodic syndrome and Muckle-Wells syndrome (44), suggests this activation could be involved in B-cell homeostasis and the production of antibodies.
SYSTEMIC LUPUS ERYTHEMATOSUS AS A PARADIGM OF AUTOIMMUNE DISEASE
SLE is characterized by functional changes in B and T cells, monocytes, plasmacytoid dendritic cells, and granulocytes, autoantibody deposition in inflammation sites, and raised circulating cytokine and chemokine levels. In lupus nephritis (LN), immune complexes deposited in glomeruli include IgG, IgM, and IgA autoantibodies, which are directed against ubiquitous nuclear antigens, especially double-stranded (ds) DNA, possibly leading to kidney failure and death (62). Mechanisms contributing to LN pathogenesis include those mediated by Th1 and Th17 cells (63).
While humoral responses produced by self-reactive antibodies act as effector mediators of LN, and IgE autoantibodies have been observed in some cases, the manner of Th2 cell and B cell activation in LN pathogenesis remains unclear (62).
Role of T-cells and cytokines in the pathogenesis of SLE and lupus nephritis
In SLE, T cells provide “excessive help” to B cells and mount inflammatory responses while producing low levels of interleukin-2 (IL-2) (63). Defective IL-2 production in T cells could explain for the known reduction in cytotoxic activity, defective regulatory T cell function and decreased activation-induced cell death in SLE patients (64). Helper CD4 T cells are vital components of immune responses in SLE; after differentiation, CD4 T cell effector functions correlate with the profile of the cytokines they secrete (65).
Amplified Th1, Th2, Th17 and follicular helper T cell responses are related to autoantibody production in murine and human SLE, and their effector cytokines may mediate target-organ inflammation. The cytokine response might reflect the primary activation pathway, which could be governed by genetic factors, and/or might reflect a specific environmental trigger (65, 66).
As mentioned, studies show a reduction in the amount and/or function of regulatory T cells in SLE patients and lupus-prone mice (67). Regulatory T cells have a reduced capacity to suppress CD4 T cell proliferation in active lupus compared with inactive lupus or healthy controls (68).
In addition to Th1, Th17 and regulatory T cells, reports suggest a role for Th2 cells in SLE (68–70). The strong humoral response in SLE indicates that there may be a Th2 component, with reports showing increased IgE and the presence of self-reactive IgE in the serum from some SLE patients, with no increase in allergy (71, 72). However, it is unclear whether Th2 cytokines, like IL-4, and IgE, contribute to SLE and which cell type may be implicated.
The presentation of LN is phenotypically and histologically heterogeneous. Diffuse proliferative glomerulonephritis (DPGN) and membranous glomerulonephritis (MGN) are, morphologically, complete opposites (73). DPGN pathogenesis is associated with a predominance of Th1 cytokines, suggesting that it occurs in a Th1-dominant immune response. Renal tissue from DPGN patients shows increased Th1 cytokine levels, including IFNγ, and the IFNγ/IL-4 production ratio correlates with the nephritic histological activity index. In contrast, the ratio is reduced in peripheral blood lymphocytes of MGN patients, suggesting that Th2-dominant cytokine responses are associated with MGN pathogenesis (74).
IgE in SLE and lupus nephritis
Studies show SLE patients without allergy have elevated total IgE and antinuclear IgE autoantibody levels, which appear to be related to disease severity (57). Likewise, the presence of IgE in glomerular immune complex deposits in renal biopsies of SLE patients and a murine model of systemic autoimmune disease suggest they play a role in LN (75). A study of antinuclear IgE antibody specificity and cytokine involvement suggests that IgE antibodies against cell autoantigens implicated in protein expression, cell proliferation, and apoptosis, are observed in SLE patients and that IL-10 may down-regulate IgE autoimmune responses in SLE. (75).
Lyn, basophils and Th2
Lyn is one of various Src-tyrosine kinases involved in B-cell activation. Aged lyn−/− mice develop autoimmune disease resembling human SLE (76). Lyn−/− mice have circulating autoantibodies to dsDNA and antinuclear antibodies (ANA). Glomerular CIC deposition in these mice results in renal damage and death.
Lyn−/− mice develop early strong, constitutive Th2 skewing and exacerbated responses to Th2 challenges (77, 78). In addition, B cells from some SLE patients express reduced levels of Lyn kinase (79). Therefore, lyn−/− mice are a likely model to study the influence of a Th2 environment on lupus-like nephritis.
The cell types causing Th2 cell differentiation are not clear. Identification of the cell types and molecules responsible for Th2 cell response dysregulation could help to control these responses (34). Although important, factors controlling basophil-mediated Th2 cell differentiation remain unknown. Lyn kinase dampens basophil expression of the transcription factor, GATA-3, and the initiation and the extent of Th2 cell differentiation. Reportedly, lyn−/− mice had marked basophilia, a constitutive Th2 cell skewing that was exacerbated by in vivo basophil challenge, produced antibodies to normally inert antigens, and did not respond appropriately to a Th1 cell-inducing pathogen. Th2 cell skewing was dependent on basophils, IgE, and IL-4, but independent of mast cells, suggesting basophil-expressed Lyn kinase exerts regulatory control on Th2 cell differentiation and function (34).
BASOPHILS, IgE, Th2 AND LUPUS NEPHRITIS
Charles et al recently investigated whether Th2 skewing in lyn−/− mice plays a role in the development of late-life lupus-like nephritis and whether similar characteristics exist in SLE patients (80). They found that the Th2 phenotype contributes to lupus-like nephritis in lyn−/− mice and is associated with LN in human SLE. Basophils and self-reactive IgE were identified as key players in renal disease. In mice, basophil depletion or a lack of IL-4 or IgE led to reduced autoantibody production and preserved renal function. Therefore, without basophils, autoantibody levels might not be sufficient to cause renal disease.
The authors studied the role played by the Th2 environment in the development of an SLE-like phenotype using mice deficient in IgE and Lyn, IL-4 and Lyn, or mast cells and Lyn, respectively. As reported (77), IgE contributes to increased mast cell levels in lyn−/− mice, suggesting it plays a role in mast cell survival (81). However, neither IL-4 nor IgE was associated with basophilia in mice and the lupus-like nephritis seen was, therefore, dependent on IgE and IL-4 but not on mast cells. Basophil depletion in lyn−/− mice aged > 32 weeks substantially decreased ANA and reduced splenic plasma cells and the renal pro-inflammatory environment. Basophils supported splenic plasma cells and enhanced the production of autoantibodies in an IL-4 and IgE-dependent manner, resulting in kidney damage.
The study also determined whether self-reactive IgE is observed in the murine circulation, whether they activate FcεRI-bearing basophils, resulting in Th2 cytokine expression, and whether IgE or IgG immune complexes stimulate basophil IL-4 production. While IgE immune complexes induced basophil IL-4 production, IgG immune complexes did not.
Circulating basophils had increased CD62L expression, which permits leukocyte homing to peripheral lymphoid tissues. A lack of IL-4 or IgE inhibited CD62L expression on circulating basophils. Large amounts of basophils were present in the spleen and lymph nodes, where the proportion of basophils was markedly reduced in IL-4- or IgE-deficient but not in mast cell-deficient settings. Lymph node basophils expressed membrane-associated BAFF, showing a possible role of lymph node basophils on B cell survival and differentiation. In addition, basophils from mice lymph nodes and spleen had a high expression of MHC II. Higher expression of MHC II and/or BAFF in the lymph nodes and spleen could permit communication with T and B cells.
SLE patients had high numbers of C1q-reactive CICs, which activate the classical complement pathway and were markedly raised in mild and active disease. SLE patients also showed high total IgE and self-reactive dsDNA-specific IgE levels, which were associated with active LN. IgGs directed against IgE were also found in sera in SLE patients, with significantly raised levels correlating with active disease.
Basophils from all SLE patients had high CD203c expression compared with healthy controls, indicating basophil activation. CD62L and HLA-DR expression was also elevated on SLE basophils and correlated with greater disease activity. Total circulating basophils were reduced in SLE patients, and were associated with immunosuppressive therapy, but not with basophil activation.
INTERPRETATION AND CAVEATS
Charles et al showed basophils contribute to self-reactive antibody production in SLE and could enhance pre-existing loss of B cell tolerance. The development of lupus-like disease in lyn−/− mice depended on the presence of IL-4 and IgE, whose absence reversed the Th2 skewing seen in these mice. IgG anti-dsDNA and ANA titers and CIC levels were also reduced in mice deficient for IgE and Lyn, and IL-4 and Lyn, respectively, demonstrating that autoantibody production in lyn−/− mice was, at least partly, reliant on the Th2 environment. Therefore, these results demonstrate the participation of basophils, IgE, and IL-4 in the maintenance of autoantibody production in lyn−/− mice and indicate that the Th2 environment contributes to the autoimmunity. They also show that, in some settings, basophils are strong inducers of Th2 cell differentiation, thus connecting the ‘allergic’ environment to the development of autoimmune diseases like SLE, although the suggestion that basophils are necessary for Th2 cell differentiation must be inferred with caution. Research is limited on this topic and the crucial test of challenging mice with a Th2 antigen in the complete lack of basophils remains to be done.
Although this study increases the understanding of LN pathogenesis, it has some limitations. IgE autoantibodies are found only in one third of SLE patients (75). Therefore, it is unlikely that the lyn−/− mouse models SLE in most patients. However, it is known that IFNγ, the primary Th1 cytokine, can negatively regulate both basophils and IL-4 production; therefore, it remains to be determined whether the 30% of SLE patients with high IgE ANA levels would respond to therapeutic basophil modulation, as suggested by this study in lyn−/− mice (65).
It is also unclear whether the reported upregulation of BAFF on basophils depends on FcεRI engagement or needs concomitant TLR9 engagement or, alternatively, if BAFF produces basophil-mediated class switching and Ig production (44). Activated basophils migrate to peripheral lymphoid organs, but the manner and site of interaction with T or B cells remains to be elucidated.
Finally, Charles et al observed a significant decrease in circulating basophils in SLE patients, which was associated with increased disease activity, findings consistent with basophil homing to the secondary lymphoid tissues. Reduced circulating basophils were not observed in lyn−/− mice, although the mice had peripheral basophilia, which was not observed in patients. In lyn−/− mice, dysregulation of basophil proliferation probably covers circulating basophil depletion after basophil homing to the secondary lymphoid tissues.
THERAPEUTIC IMPLICATIONS
This study suggests that reducing circulating levels of self-reactive IgE or dampening basophil activity could have therapeutic benefits in LN. Therefore, determining whether basophil reduction or inactivation early in the disease course could defer or rescue the early development of LN is of substantial interest.
A recent phase 3 multicenter, placebo-controlled trial in patients with active SLE found that belimumab, a monoclonal antibody against BAFF, is safe and efficacious in these patients (62, 82). Belimumab, besides affecting B cells, might deplete basophils (which contain membrane-bound BAFF), suggesting that it could be of help in some LN patients, perhaps combined with treatments suppressing IgE production.
The study showed that IgE immune complexes activate basophils, and that removing self-reactive IgEs forming functional CICs prevents renal disease. As circulating IgE levels are decreased, omalizumab, a monoclonal antibody binding to human IgE and decreasing FcεRI expression on basophils (83), may provide therapeutic benefits in SLE patients with raised IgE. This approach could be easily tested, since omalizumab is currently used to treat asthma and allergic rhinitis and seems to be well tolerated [80, 81].
FUTURE DIRECTIONS
The variety of basophil immunoregulatory activity explains why their pharmacological modulation by specific inhibitors or regulators is actively pursued, especially in allergic diseases. This approach may be utilized fairly soon in other pathologic conditions, including autoimmunity, as illustrated by the recent finding of basophil activation by anti-citrullinated protein antibodies (ACPA) in the serum of RA patients (84). Schuerwegh et al showed that IgE-bearing basophils from ACPA+ RA patients are directly activated on exposure to citrullinated antigens, probably reflecting the presence of FcεRI-bound IgE-ACPAs on basophil surfaces (84). Identification of this activation pathway mediated by IgE-ACPAs in basophils could lead to innovative therapeutic schemes in RA.
The role of basophils should also be tested in immune-mediated renal disorders other than LN. A memory-type immune response prevails in transplantation and various autoimmune diseases with the constant presence of alloantigens/autoantigens. Together with specific antibodies, these antigens may activate basophils, which may enhance ongoing humoral immune responses and further boost immunoglobulin production (85).
Although studies suggest basophils may play a role in transplant rejection, studies using consistent methods of detecting basophils and determining their activation in some renal disorders are required. Basophils should be studied in minimal-change disease and focal segmental glomerulosclerosis, where T cells and allergy/atopy are believed to play a major role, and Th2 skewed cytokine profiles have been recognized (85). Basophils, as inducers of Th2 immune responses and an important source of IL-4, could initiate disease and play a role in sustaining Th2-immune responses. Basophils should also be assessed in diseases driven by Ig directed against defined kidney structures (e.g., anti-glomerular basement membrane disease), deposited in the glomeruli (e.g., membranous nephropathy) or driven by systemic vasculitis (e.g., antineutrophil cytoplasmic antibody-associated vasculitis), in which basophils may contribute to the generation and maintenance of high levels of specific Ig and, eventually, to disease progression.
CONCLUSIONS
Although our knowledge of the immunomodulatory and effector functions of basophils remains imperfect, it can be stated that, in addition to their role in allergy and host defense against parasites, basophils can promote Th2 cell differentiation and amplify the humoral immune response. Their role in autoimmune diseases is not clear, but the studies reported here provide a persuasive argument for a role in the amplification of LN rather than disease initiation. Essential requirements are autoreactive IgE-dependent basophil activation, IL-4 production by basophils, and the promotion of Th2 cell differentiation. This does not negate the proven role of Th1, Th17, and the loss of regulatory T cell function in the development of autoimmunity but rather suggests that the robust humoral constituent of autoimmune diseases like SLE requires basophils to reach the autoantibody production levels that produce renal disease. These novel findings open the way for the study of basophils in other autoimmune and renal diseases. Future studies may also show whether basophil-mediated immune activation is linked to other SLE-prone mouse models in addition to lyn−/− mice.
Acknowledgments
Supported by NIH grant AI080908 (B.M.)
REFERENCES
- 1.Falcone FH, Zillikens D, Gibbs BF. The 21st century renaissance of the basophil? Current insights into its role in allergic responses and innate immunity. Exp Dermatol. 2006;15:855–864. doi: 10.1111/j.1600-0625.2006.00477.x. [DOI] [PubMed] [Google Scholar]
- 2.Askenase PW. Mechanisms of hypersensitivity: cellular interactions. Basophil arrival and function in tissue hypersensitivity reactions. J Allergy Clin Immunol. 1979;64:79–89. doi: 10.1016/0091-6749(79)90041-1. [DOI] [PubMed] [Google Scholar]
- 3.Brown SJ, Graziano FM, Askenase PW. Immune serum transfer of cutaneous basophil-associated resistance to ticks: mediation by 7SIgG1 antibodies. J Immunol. 1982;129:2407–2412. [PubMed] [Google Scholar]
- 4.Brown SJ, Barker RW, Askenase PW. Bovine resistance to Amblyomma americanum ticks: an acquired immune response characterized by cutaneous basophil infiltrates. Vet Parasitol. 1984;16:147–165. doi: 10.1016/0304-4017(84)90016-5. [DOI] [PubMed] [Google Scholar]
- 5.Brown SJ, Galli SJ, Gleich GJ, Askenase PW. Ablation of immunity to Amblyomma americanum by anti-basophil serum: cooperation between basophils and eosinophils in expression of immunity to ectoparasites (ticks) in guinea pigs. J Immunol. 1982;129:790–796. [PubMed] [Google Scholar]
- 6.Min B. Basophils: what they 'can do' versus what they 'actually do'. Nat Immunol. 2008;9:1333–1339. doi: 10.1038/ni.f.217. [DOI] [PubMed] [Google Scholar]
- 7.Wada T, Ishiwata K, Koseki H, Ishikura T, Ugajin T, Ohnuma N, Obata K, Ishikawa R, Yoshikawa S, Mukai K, Kawano Y, Minegishi Y, Yokozeki H, Watanabe N, Karasuyama H. Selective ablation of basophils in mice reveals their nonredundant role in acquired immunity against ticks. J Clin Invest. 2010;120:2867–2875. doi: 10.1172/JCI42680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ohnmacht C, Schwartz C, Panzer M, Schiedewitz I, Naumann R, Voehringer D. Basophils Orchestrate Chronic Allergic Dermatitis and Protective Immunity against Helminths. Immunity. 2010 doi: 10.1016/j.immuni.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 9.Ohmori K, Luo Y, Jia Y, Nishida J, Wang Z, Bunting KD, Wang D, Huang H. IL-3 induces basophil expansion in vivo by directing granulocyte-monocyte progenitors to differentiate into basophil lineage-restricted progenitors in the bone marrow and by increasing the number of basophil/mast cell progenitors in the spleen. J Immunol. 2009;182:2835–2841. doi: 10.4049/jimmunol.0802870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arinobu Y, Iwasaki H, Gurish MF, Mizuno S, Shigematsu H, Ozawa H, Tenen DG, Austen KF, Akashi K. Developmental checkpoints of the basophil/mast cell lineages in adult murine hematopoiesis. Proc Natl Acad Sci U S A. 2005;102:18105–18110. doi: 10.1073/pnas.0509148102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arinobu Y, Iwasaki H, Akashi K. Origin of basophils and mast cells. Allergol Int. 2009;58:21–28. doi: 10.2332/allergolint.08-RAI-0067. [DOI] [PubMed] [Google Scholar]
- 12.Lantz CS, Boesiger J, Song CH, Mach N, Kobayashi T, Mulligan RC, Nawa Y, Dranoff G, Galli SJ. Role for interleukin-3 in mast-cell and basophil development and in immunity to parasites. Nature. 1998;392:90–93. doi: 10.1038/32190. [DOI] [PubMed] [Google Scholar]
- 13.Shen T, Kim S, Do JS, Wang L, Lantz C, Urban JF, Le Gros G, Min B. T cell-derived IL-3 plays key role in parasite infection-induced basophil production but is dispensable for in vivo basophil survival. Int Immunol. 2008;20:1201–1209. doi: 10.1093/intimm/dxn077. [DOI] [PubMed] [Google Scholar]
- 14.Lantz CS, Min B, Tsai M, Chatterjea D, Dranoff G, Galli SJ. IL-3 is required for increases in blood basophils in nematode infection in mice and can enhance IgE-dependent IL-4 production by basophils in vitro. Lab Invest. 2008;88:1134–1142. doi: 10.1038/labinvest.2008.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Le Gros G, Ben-Sasson SZ, Conrad DH, Clark-Lewis I, Finkelman FD, Plaut M, Paul WE. IL-3 promotes production of IL-4 by splenic non-B, non-T cells in response to Fc receptor cross-linkage. J Immunol. 1990;145:2500–2506. [PubMed] [Google Scholar]
- 16.Hida S, Yamasaki S, Sakamoto Y, Takamoto M, Obata K, Takai T, Karasuyama H, Sugane K, Saito T, Taki S. Fc receptor gamma-chain, a constitutive component of the IL-3 receptor, is required for IL-3-induced IL-4 production in basophils. Nat Immunol. 2009;10:214–222. doi: 10.1038/ni.1686. [DOI] [PubMed] [Google Scholar]
- 17.Ben-Sasson SZ, Le Gros G, Conrad DH, Finkelman FD, Paul WE. Cross-linking Fc receptors stimulate splenic non-B, non-T cells to secrete interleukin 4 and other lymphokines. Proc Natl Acad Sci U S A. 1990;87:1421–1425. doi: 10.1073/pnas.87.4.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yoshimoto T, Tsutsui H, Tominaga K, Hoshino K, Okamura H, Akira S, Paul WE, Nakanishi K. IL-18, although antiallergic when administered with IL-12, stimulates IL-4 and histamine release by basophils. Proc Natl Acad Sci U S A. 1999;96:13962–13966. doi: 10.1073/pnas.96.24.13962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schneider E, Petit-Bertron AF, Bricard R, Levasseur M, Ramadan A, Girard JP, Herbelin A, Dy M. IL-33 activates unprimed murine basophils directly in vitro and induces their in vivo expansion indirectly by promoting hematopoietic growth factor production. J Immunol. 2009;183:3591–3597. doi: 10.4049/jimmunol.0900328. [DOI] [PubMed] [Google Scholar]
- 20.Smithgall MD, Comeau MR, Yoon BR, Kaufman D, Armitage R, Smith DE. IL-33 amplifies both Th1- and Th2-type responses through its activity on human basophils, allergen-reactive Th2 cells, iNKT and NK cells. Int Immunol. 2008;20:1019–1030. doi: 10.1093/intimm/dxn060. [DOI] [PubMed] [Google Scholar]
- 21.Kroeger KM, Sullivan BM, Locksley RM. IL-18 and IL-33 elicit Th2 cytokines from basophils via a MyD88- and p38alpha-dependent pathway. J Leukoc Biol. 2009;86:769–778. doi: 10.1189/jlb.0708452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fort MM, Cheung J, Yen D, Li J, Zurawski SM, Lo S, Menon S, Clifford T, Hunte B, Lesley R, Muchamuel T, Hurst SD, Zurawski G, Leach MW, Gorman DM, Rennick DM. IL-25 induces IL-4, IL-5, and IL-13 and Th2-associated pathologies in vivo. Immunity. 2001;15:985–995. doi: 10.1016/s1074-7613(01)00243-6. [DOI] [PubMed] [Google Scholar]
- 23.Wang H, Mobini R, Fang Y, Barrenas F, Zhang H, Xiang Z, Benson M. Allergen challenge of peripheral blood mononuclear cells from patients with seasonal allergic rhinitis increases IL-17RB, which regulates basophil apoptosis and degranulation. Clin Exp Allergy. 2010;40:1194–1202. doi: 10.1111/j.1365-2222.2010.03542.x. [DOI] [PubMed] [Google Scholar]
- 24.Yoshimoto T, Yasuda K, Tanaka H, Nakahira M, Imai Y, Fujimori Y, Nakanishi K. Basophils contribute to T(H)2-IgE responses in vivo via IL-4 production and presentation of peptide-MHC class II complexes to CD4+ T cells. Nat Immunol. 2009;10:706–712. doi: 10.1038/ni.1737. [DOI] [PubMed] [Google Scholar]
- 25.Sabroe I, Jones EC, Usher LR, Whyte MK, Dower SK. Toll-like receptor (TLR)2 and TLR4 in human peripheral blood granulocytes: a critical role for monocytes in leukocyte lipopolysaccharide responses. J Immunol. 2002;168:4701–4710. doi: 10.4049/jimmunol.168.9.4701. [DOI] [PubMed] [Google Scholar]
- 26.Bieneman AP, Chichester KL, Chen YH, Schroeder JT. Toll-like receptor 2 ligands activate human basophils for both IgE-dependent and IgE-independent secretion. J Allergy Clin Immunol. 2005;115:295–301. doi: 10.1016/j.jaci.2004.10.018. [DOI] [PubMed] [Google Scholar]
- 27.Schramm G, Mohrs K, Wodrich M, Doenhoff MJ, Pearce EJ, Haas H, Mohrs M. Cutting edge: IPSE/alpha-1, a glycoprotein from Schistosoma mansoni eggs, induces IgE-dependent, antigen-independent IL-4 production by murine basophils in vivo. J Immunol. 2007;178:6023–6027. doi: 10.4049/jimmunol.178.10.6023. [DOI] [PubMed] [Google Scholar]
- 28.Phillips C, Coward WR, Pritchard DI, Hewitt CR. Basophils express a type 2 cytokine profile on exposure to proteases from helminths and house dust mites. J Leukoc Biol. 2003;73:165–171. doi: 10.1189/jlb.0702356. [DOI] [PubMed] [Google Scholar]
- 29.Sokol CL, Barton GM, Farr AG, Medzhitov R. A mechanism for the initiation of allergen-induced T helper type 2 responses. Nat Immunol. 2008;9:310–318. doi: 10.1038/ni1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.de Paulis A, Prevete N, Fiorentino I, Walls AF, Curto M, Petraroli A, Castaldo V, Ceppa P, Fiocca R, Marone G. Basophils infiltrate human gastric mucosa at sites of Helicobacter pylori infection, and exhibit chemotaxis in response to H. pylori-derived peptide Hp(2–20) J Immunol. 2004;172:7734–7743. doi: 10.4049/jimmunol.172.12.7734. [DOI] [PubMed] [Google Scholar]
- 31.Patella V, Florio G, Petraroli A, Marone G. HIV-1 gp120 induces IL-4 and IL-13 release from human Fc epsilon RI+ cells through interaction with the VH3 region of IgE. J Immunol. 2000;164:589–595. doi: 10.4049/jimmunol.164.2.589. [DOI] [PubMed] [Google Scholar]
- 32.Kurimoto Y, de Weck AL, Dahinden CA. Interleukin 3-dependent mediator release in basophils triggered by C5a. J Exp Med. 1989;170:467–479. doi: 10.1084/jem.170.2.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hida S, Tadachi M, Saito T, Taki S. Negative control of basophil expansion by IRF-2 critical for the regulation of Th1/Th2 balance. Blood. 2005;106:2011–2017. doi: 10.1182/blood-2005-04-1344. [DOI] [PubMed] [Google Scholar]
- 34.Charles N, Watford WT, Ramos HL, Hellman L, Oettgen HC, Gomez G, Ryan JJ, O'Shea JJ, Rivera J. Lyn kinase controls basophil GATA-3 transcription factor expression and induction of Th2 cell differentiation. Immunity. 2009;30:533–543. doi: 10.1016/j.immuni.2009.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kuroda E, Ho V, Ruschmann J, Antignano F, Hamilton M, Rauh MJ, Antov A, Flavell RA, Sly LM, Krystal G. SHIP represses the generation of IL-3-induced M2 macrophages by inhibiting IL-4 production from basophils. J Immunol. 2009;183:3652–3660. doi: 10.4049/jimmunol.0900864. [DOI] [PubMed] [Google Scholar]
- 36.Zhu J, Yamane H, Paul WE. Differentiation of effector CD4 T cell populations (*) Annu Rev Immunol. 2010;28:445–489. doi: 10.1146/annurev-immunol-030409-101212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Min B, Prout M, Hu-Li J, Zhu J, Jankovic D, Morgan ES, Urban JF, Jr, Dvorak AM, Finkelman FD, LeGros G, Paul WE. Basophils produce IL-4 and accumulate in tissues after infection with a Th2-inducing parasite. J Exp Med. 2004;200:507–517. doi: 10.1084/jem.20040590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Voehringer D, Shinkai K, Locksley RM. Type 2 immunity reflects orchestrated recruitment of cells committed to IL-4 production. Immunity. 2004;20:267–277. doi: 10.1016/s1074-7613(04)00026-3. [DOI] [PubMed] [Google Scholar]
- 39.Oh K, Shen T, Le Gros G, Min B. Induction of Th2 type immunity in a mouse system reveals a novel immunoregulatory role of basophils. Blood. 2007;109:2921–2927. doi: 10.1182/blood-2006-07-037739. [DOI] [PubMed] [Google Scholar]
- 40.Kim S, Shen T, Min B. Basophils can directly present or cross-present antigen to CD8 lymphocytes and alter CD8 T cell differentiation into IL-10-producing phenotypes. J Immunol. 2009;183:3033–3039. doi: 10.4049/jimmunol.0900332. [DOI] [PubMed] [Google Scholar]
- 41.Gauchat JF, Henchoz S, Mazzei G, Aubry JP, Brunner T, Blasey H, Life P, Talabot D, Flores-Romo L, Thompson J, et al. Induction of human IgE synthesis in B cells by mast cells and basophils. Nature. 1993;365:340–343. doi: 10.1038/365340a0. [DOI] [PubMed] [Google Scholar]
- 42.Yanagihara Y, Kajiwara K, Basaki Y, Ikizawa K, Ebisawa M, Ra C, Tachimoto H, Saito H. Cultured basophils but not cultured mast cells induce human IgE synthesis in B cells after immunologic stimulation. Clin Exp Immunol. 1998;111:136–143. doi: 10.1046/j.1365-2249.1998.00474.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Denzel A, Maus UA, Rodriguez Gomez M, Moll C, Niedermeier M, Winter C, Maus R, Hollingshead S, Briles DE, Kunz-Schughart LA, Talke Y, Mack M. Basophils enhance immunological memory responses. Nat Immunol. 2008;9:733–742. doi: 10.1038/ni.1621. [DOI] [PubMed] [Google Scholar]
- 44.Chen K, Xu W, Wilson M, He B, Miller NW, Bengten E, Edholm ES, Santini PA, Rath P, Chiu A, Cattalini M, Litzman J, J BB, Huang B, Meini A, Riesbeck K, Cunningham-Rundles C, Plebani A, Cerutti A. Immunoglobulin D enhances immune surveillance by activating antimicrobial, proinflammatory and B cell-stimulating programs in basophils. Nat Immunol. 2009;10:889–898. doi: 10.1038/ni.1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sokol CL, Chu NQ, Yu S, Nish SA, Laufer TM, Medzhitov R. Basophils function as antigen-presenting cells for an allergen-induced T helper type 2 response. Nat Immunol. 2009;10:713–720. doi: 10.1038/ni.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Perrigoue JG, Saenz SA, Siracusa MC, Allenspach EJ, Taylor BC, Giacomin PR, Nair MG, Du Y, Zaph C, van Rooijen N, Comeau MR, Pearce EJ, Laufer TM, Artis D. MHC class II-dependent basophil-CD4+ T cell interactions promote T(H)2 cytokine-dependent immunity. Nat Immunol. 2009;10:697–705. doi: 10.1038/ni.1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Phythian-Adams AT, Cook PC, Lundie RJ, Jones LH, Smith KA, Barr TA, Hochweller K, Anderton SM, Hammerling GJ, Maizels RM, MacDonald AS. CD11c depletion severely disrupts Th2 induction and development in vivo. J Exp Med. 2010;207:2089–2096. doi: 10.1084/jem.20100734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hammad H, Plantinga M, Deswarte K, Pouliot P, Willart MA, Kool M, Muskens F, Lambrecht BN. Inflammatory dendritic cells--not basophils--are necessary and sufficient for induction of Th2 immunity to inhaled house dust mite allergen. J Exp Med. 2010;207:2097–2111. doi: 10.1084/jem.20101563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ohnmacht C, Schwartz C, Panzer M, Schiedewitz I, Naumann R, Voehringer D. Basophils orchestrate chronic allergic dermatitis and protective immunity against helminths. Immunity. 2010;33:364–374. doi: 10.1016/j.immuni.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 50.Kim S, Prout M, Ramshaw H, Lopez AF, LeGros G, Min B. Cutting edge: basophils are transiently recruited into the draining lymph nodes during helminth infection via IL-3, but infection-induced Th2 immunity can develop without basophil lymph node recruitment or IL-3. J Immunol. 2010;184:1143–1147. doi: 10.4049/jimmunol.0902447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mukai K, Matsuoka K, Taya C, Suzuki H, Yokozeki H, Nishioka K, Hirokawa K, Etori M, Yamashita M, Kubota T, Minegishi Y, Yonekawa H, Karasuyama H. Basophils play a critical role in the development of IgE-mediated chronic allergic inflammation independently of T cells and mast cells. Immunity. 2005;23:191–202. doi: 10.1016/j.immuni.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 52.Iikura M, Miyamasu M, Yamaguchi M, Kawasaki H, Matsushima K, Kitaura M, Morita Y, Yoshie O, Yamamoto K, Hirai K. Chemokine receptors in human basophils: inducible expression of functional CXCR4. J Leukoc Biol. 2001;70:113–120. [PubMed] [Google Scholar]
- 53.Grattan CE. Basophils in chronic urticaria. J Investig Dermatol Symp Proc. 2001;6:139–140. doi: 10.1046/j.0022-202x.2001.00027.x. [DOI] [PubMed] [Google Scholar]
- 54.Bischoff SC, Zwahlen R, Stucki M, Mullner G, de Weck AL, Stadler BM, Dahinden CA. Basophil histamine release and leukotriene production in response to anti-IgE and anti-IgE receptor antibodies. Comparison of normal subjects and patients with urticaria, atopic dermatitis or bronchial asthma. Int Arch Allergy Immunol. 1996;110:261–271. doi: 10.1159/000237297. [DOI] [PubMed] [Google Scholar]
- 55.Nigrovic PA, Lee DM. Synovial mast cells: role in acute and chronic arthritis. Immunol Rev. 2007;217:19–37. doi: 10.1111/j.1600-065X.2007.00506.x. [DOI] [PubMed] [Google Scholar]
- 56.Damsker JM, Hansen AM, Caspi RR. Th1 and Th17 cells: adversaries and collaborators. Ann N Y Acad Sci. 2010;1183:211–221. doi: 10.1111/j.1749-6632.2009.05133.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Atta AM, Sousa CP, Carvalho EM, Sousa-Atta ML. Immunoglobulin E and systemic lupus erythematosus. Braz J Med Biol Res. 2004;37:1497–1501. doi: 10.1590/s0100-879x2004001000008. [DOI] [PubMed] [Google Scholar]
- 58.Sekigawa I, Yoshiike T, Iida N, Hashimoto H, Ogawa H. Allergic diseases in systemic lupus erythematosus: prevalence and immunological considerations. Clin Exp Rheumatol. 2003;21:117–121. [PubMed] [Google Scholar]
- 59.Veldhoen M. The role of T helper subsets in autoimmunity and allergy. Curr Opin Immunol. 2009;21:606–611. doi: 10.1016/j.coi.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 60.Martin F, Chan AC. Pathogenic roles of B cells in human autoimmunity; insights from the clinic. Immunity. 2004;20:517–527. doi: 10.1016/s1074-7613(04)00112-8. [DOI] [PubMed] [Google Scholar]
- 61.Valenta R, Seiberler S, Natter S, Mahler V, Mossabeb R, Ring J, Stingl G. Autoallergy: a pathogenetic factor in atopic dermatitis? J Allergy Clin Immunol. 2000;105:432–437. doi: 10.1067/mai.2000.104783. [DOI] [PubMed] [Google Scholar]
- 62.Kaveri SV, Mouthon L, Bayry J. Basophils and nephritis in lupus. N Engl J Med. 2010;363:1080–1082. doi: 10.1056/NEJMcibr1006936. [DOI] [PubMed] [Google Scholar]
- 63.Crispin JC, Liossis SN, Kis-Toth K, Lieberman LA, Kyttaris VC, Juang YT, Tsokos GC. Pathogenesis of human systemic lupus erythematosus: recent advances. Trends Mol Med. 2010;16:47–57. doi: 10.1016/j.molmed.2009.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Crispin JC, Kyttaris VC, Juang YT, Tsokos GC. How signaling and gene transcription aberrations dictate the systemic lupus erythematosus T cell phenotype. Trends Immunol. 2008;29:110–115. doi: 10.1016/j.it.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 65.Davidson A, Diamond B. Activated basophils give lupus a booster shot. Nat Med. 2010;16:635–636. doi: 10.1038/nm0610-635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Singh RR, Saxena V, Zang S, Li L, Finkelman FD, Witte DP, Jacob CO. Differential contribution of IL-4 and STAT6 vs STAT4 to the development of lupus nephritis. J Immunol. 2003;170:4818–4825. doi: 10.4049/jimmunol.170.9.4818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rahman A, Isenberg DA. Systemic lupus erythematosus. N Engl J Med. 2008;358:929–939. doi: 10.1056/NEJMra071297. [DOI] [PubMed] [Google Scholar]
- 68.Valencia X, Yarboro C, Illei G, Lipsky PE. Deficient CD4+CD25high T regulatory cell function in patients with active systemic lupus erythematosus. J Immunol. 2007;178:2579–2588. doi: 10.4049/jimmunol.178.4.2579. [DOI] [PubMed] [Google Scholar]
- 69.Zeng D, Liu Y, Sidobre S, Kronenberg M, Strober S. Activation of natural killer T cells in NZB/W mice induces Th1-type immune responses exacerbating lupus. J Clin Invest. 2003;112:1211–1222. doi: 10.1172/JCI17165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pernis AB. Th17 cells in rheumatoid arthritis and systemic lupus erythematosus. J Intern Med. 2009;265:644–652. doi: 10.1111/j.1365-2796.2009.02099.x. [DOI] [PubMed] [Google Scholar]
- 71.Tiller T, Tsuiji M, Yurasov S, Velinzon K, Nussenzweig MC, Wardemann H. Autoreactivity in human IgG+ memory B cells. Immunity. 2007;26:205–213. doi: 10.1016/j.immuni.2007.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tsuiji M, Yurasov S, Velinzon K, Thomas S, Nussenzweig MC, Wardemann H. A checkpoint for autoreactivity in human IgM+ memory B cell development. J Exp Med. 2006;203:393–400. doi: 10.1084/jem.20052033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Shimizu S, Sugiyama N, Masutani K, Sadanaga A, Miyazaki Y, Inoue Y, Akahoshi M, Katafuchi R, Hirakata H, Harada M, Hamano S, Nakashima H, Yoshida H. Membranous glomerulonephritis development with Th2-type immune deviations in MRL/lpr mice deficient for IL-27 receptor (WSX-1) J Immunol. 2005;175:7185–7192. doi: 10.4049/jimmunol.175.11.7185. [DOI] [PubMed] [Google Scholar]
- 74.Masutani K, Akahoshi M, Tsuruya K, Tokumoto M, Ninomiya T, Kohsaka T, Fukuda K, Kanai H, Nakashima H, Otsuka T, Hirakata H. Predominance of Th1 immune response in diffuse proliferative lupus nephritis. Arthritis Rheum. 2001;44:2097–2106. doi: 10.1002/1529-0131(200109)44:9<2097::AID-ART360>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 75.Atta AM, Santiago MB, Guerra FG, Pereira MM, Sousa Atta ML. Autoimmune response of IgE antibodies to cellular self-antigens in systemic Lupus Erythematosus. Int Arch Allergy Immunol. 2010;152:401–406. doi: 10.1159/000288293. [DOI] [PubMed] [Google Scholar]
- 76.Yu CC, Yen TS, Lowell CA, DeFranco AL. Lupus-like kidney disease in mice deficient in the Src family tyrosine kinases Lyn and Fyn. Curr Biol. 2001;11:34–38. doi: 10.1016/s0960-9822(00)00024-5. [DOI] [PubMed] [Google Scholar]
- 77.Odom S, Gomez G, Kovarova M, Furumoto Y, Ryan JJ, Wright HV, Gonzalez-Espinosa C, Hibbs ML, Harder KW, Rivera J. Negative regulation of immunoglobulin E-dependent allergic responses by Lyn kinase. J Exp Med. 2004;199:1491–1502. doi: 10.1084/jem.20040382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Beavitt SJ, Harder KW, Kemp JM, Jones J, Quilici C, Casagranda F, Lam E, Turner D, Brennan S, Sly PD, Tarlinton DM, Anderson GP, Hibbs ML. Lyn-deficient mice develop severe, persistent asthma: Lyn is a critical negative regulator of Th2 immunity. J Immunol. 2005;175:1867–1875. doi: 10.4049/jimmunol.175.3.1867. [DOI] [PubMed] [Google Scholar]
- 79.Liossis SN, Solomou EE, Dimopoulos MA, Panayiotidis P, Mavrikakis MM, Sfikakis PP. B-cell kinase lyn deficiency in patients with systemic lupus erythematosus. J Investig Med. 2001;49:157–165. doi: 10.2310/6650.2001.34042. [DOI] [PubMed] [Google Scholar]
- 80.Charles N, Hardwick D, Daugas E, Illei GG, Rivera J. Basophils and the T helper 2 environment can promote the development of lupus nephritis. Nat Med. 2010;16:701–707. doi: 10.1038/nm.2159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Asai K, Kitaura J, Kawakami Y, Yamagata N, Tsai M, Carbone DP, Liu FT, Galli SJ, Kawakami T. Regulation of mast cell survival by IgE. Immunity. 2001;14:791–800. doi: 10.1016/s1074-7613(01)00157-1. [DOI] [PubMed] [Google Scholar]
- 82.Navarra SV, Guzman RM, Gallacher AE, Hall S, Levy RA, Jimenez RE, Li EK, Thomas M, Kim HY, Leon MG, Tanasescu C, Nasonov E, Lan JL, Pineda L, Zhong ZJ, Freimuth W, Petri MA. Efficacy and safety of belimumab in patients with active systemic lupus erythematosus: a randomised, placebo-controlled, phase 3 trial. Lancet. 2011 doi: 10.1016/S0140-6736(10)61354-2. [DOI] [PubMed] [Google Scholar]
- 83.Lin H, Boesel KM, Griffith DT, Prussin C, Foster B, Romero FA, Townley R, Casale TB. Omalizumab rapidly decreases nasal allergic response and FcepsilonRI on basophils. J Allergy Clin Immunol. 2004;113:297–302. doi: 10.1016/j.jaci.2003.11.044. [DOI] [PubMed] [Google Scholar]
- 84.Schuerwegh AJ, Ioan-Facsinay A, Dorjee AL, Roos J, Bajema IM, van der Voort EI, Huizinga TW, Toes RE. Evidence for a functional role of IgE anticitrullinated protein antibodies in rheumatoid arthritis. Proc Natl Acad Sci U S A. 2010;107:2586–2591. doi: 10.1073/pnas.0913054107. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 85.Mack M, Rosenkranz AR. Basophils and mast cells in renal injury. Kidney Int. 2009;76:1142–1147. doi: 10.1038/ki.2009.320. [DOI] [PMC free article] [PubMed] [Google Scholar]