Abstract
Aims
Among patients with substance dependence and comorbid major depressive disorder (MDD) receiving treatment in a controlled trial, we examined if group differences in depression were mediated by 12-step involvement, and if the effects of 12-Step involvement on future alcohol and drug use were mediated by reductions in depression.
Design
Controlled trial of Twelve-Step Facilitation (TSF) and Integrated Cognitive Behavioral Therapy (ICBT), delivered in outpatient groups for 6 months with adjunct pharmacotherapy.
Setting
Outpatient dual diagnosis clinic in Veteran’s Affairs Healthcare Center.
Participants
Veterans (N = 209) diagnosed with alcohol, stimulant, or marijuana dependence and substance-independent MDD.
Measurements
Twelve-step attendance and affiliation, depression severity, percent days drinking, and percent days using drugs assessed at baseline and Months 3, 6, and 9.
Findings
In multilevel analyses greater 12-step meeting attendance predicted lower depression and mediated the superior depression outcomes of the TSF group, explaining 24.3% of the group difference in depression. Independent of treatment group, lower depression severity predicted lower future alcohol use and mediated the effects of 12-step meetings, explaining 15.7% of their effects on future drinking. Controlled, lagged models indicated these effects were not confounded by current substance use, suggesting that depression had unique associations with 12-step meeting attendance and future drinking.
Conclusions
For patients with substance dependence and MDD, attendance at 12-step meetings is associated with mental health benefits that extend beyond substance use, and reduced depression could be a key mechanism whereby 12-step meetings reduce future drinking in this population.
Introduction
Compared to the general population, mood and anxiety disorders occur at higher rates among individuals with substance use disorders (SUDs), and major depression (MDD) is the most common comorbid Axis I psychiatric disorder [1]. Comorbid MDD is associated with a more chronic and prolonged course of SUDs [2], higher rates of disability [3], greater treatment costs [4, 5] and elevated risk of suicide [6, 7]. The prevalence is even greater among those who receive SUD treatment; in some clinical settings over half of patients have MDD [8, 9]. These patients often have greater severity of problems at intake [10] and poorer outcomes from alcohol or drug treatment [11–15]. Despite high prevalence and evidence that treatment is less effective, few studies have examined treatment processes within this population. Recent research in SUD interventions has increasingly focused on mechanisms of change, defined as the factors that explain how and why treatments work [16]. Studies of mediators, or variables that account for the association between a predictor and outcome [17], are a core element of this research [18]. However, these factors have rarely been investigated in patients with SUD and comorbid MDD, which hinders the advancement of interventions for this patient population.
Some of the most frequently-studied mediators of SUD treatment have been variables related to 12-step involvement, including attendance at 12-step meetings and participation in 12-step activities (e.g., having a sponsor, reading literature). In general SUD samples these variables are consistently associated with reduced alcohol and drug use [19, 20] and mediated the effects of 12-step psychotherapies in clinical trials [21, 22]. However, among patients with comorbidity studies of 12-step involvement have yielded inconsistent findings. In some studies, patients with psychiatric comorbidity attended similar levels of 12-step meetings [9] and experienced similar benefits as those without psychiatric conditions [23], but others found reduced benefits of 12-step involvement for patients with comorbid MDD [24]. Issues inherent to some community meetings, such as attitudes about psychiatric medication, could interfere with participation [25]. In light of the limited existing research, further studies are needed to evaluate the utility of 12-step involvement in this population.
A more complete understanding of 12-step variables may be achieved by examining mediators of therapeutic effects. Among patients with MDD one potential mediating variable is depressive symptoms. Affect regulation is frequently described in the 12-step literature [26], and 12-step involvement may increase exposure to common therapeutic factors that could reduce depressive symptoms [27]. Therapeutic changes in mood could play a key role in substance use outcomes, as negative affect is often implicated in relapse [28] and reductions in depression over time are associated with reduced alcohol and drug use [29–31]. In a secondary analysis of Project MATCH (Matching Alcoholism Treatment to Client Heterogeneity), lower depression explained the effects of Alcoholics’ Anonymous (AA) attendance on future drinking, but this was mostly attributable to AA’s effects on current drinking [32]. The relative role of depression in mediating 12-step involvement could be greater for patients with comorbid MDD. Depressive symptoms are a prevalent precipitant of relapse for these patients [33], and prior research with this sample found strong correlations between individual changes in depression and substance use [34]. Thus, improvement in depressive symptoms linked to 12-step involvement could be a key process in the reduction of substance use for patients with SUD and MDD.
The goal of this study was to examine relations between 12-step involvement, depression, and substance use in patients receiving treatment for comorbid SUD and MDD. Veterans with alcohol or drug dependence and MDD received antidepressant pharmacotherapy and 6 months of group psychotherapy with either Twelve-Step Facilitation (TSF) or Integrated Cognitive-Behavioral Therapy (ICBT), a cognitive-behavioral treatment that focused jointly on depression and substance use [35]. In previously published studies of this sample, the TSF group had greater 12-step affiliation [36] and greater reductions in depression compared to ICBT during treatment, while substance use outcomes were similar between groups [37]. For the current study we hypothesized that the superior depression outcomes in the TSF group would be mediated by greater 12-step attendance and affiliation. Furthermore, we predicted that the effects of 12-step attendance and affiliation on future alcohol and drug use would be mediated by depressive symptoms. As depression often decreases with initial abstinence [38], we controlled for past alcohol and drug use in longitudinal models, to test whether the hypothesized relations were independent of prior substance use.
Methods
Subjects
The current study involves secondary analyses of 209 veterans who participated in a trial of outpatient group psychotherapy for comorbid SUD-MDD [35, 37]. Demographics of the sample are presented in Table 1. Participants met DSM-IV criteria for: (1) lifetime dependence on alcohol, cannabis, or stimulants with use in the past 90 days, and (2) major depressive disorder with ≥ 1 lifetime episode occurring independent of substance use, assessed via the Composite International Diagnostic Interview [39]. Exclusion criteria included opiate dependence with intravenous administration, bipolar disorder or psychotic disorder, living more than 50 miles from the facility, or severe memory impairment interfering with assessment.
Table 1.
Baseline demographic and clinical characteristics of veterans with substance dependence and major depression (N = 209).
| TSF n =97 |
ICBT n =112 |
|
|---|---|---|
| Male | 90.9 % | 88.7 % |
| Caucasian | 70.7 % | 76.3 % |
| Mean age (SD) | 49.6 (7.6) | 48.8 (7.8) |
| Mean years of education (SD) | 13.6 (2.2) | 13.4 (2.1) |
| Employed | 21.2 % | 15.0 % |
| Married | 17.2 % | 8.9 % |
| Post-traumatic stress disorder | 38.4% | 41.6% |
| Alcohol dependence | 87.0 % | 92.2 % |
| Stimulant dependence | 54.4 % | 54.2 % |
| Cannabis dependence | 27.8 % | 30.8 % |
Note. TSF: Twelve-Step Facilitation; ICBT: Integrated Cognitive-Behavioral Therapy
Procedures
The trial was approved by the University of California, San Diego and VA San Diego Healthcare System (VASDHS) Institutional Review Boards. Research staff obtained referrals from the VASDHS dual diagnosis clinic, briefly screened individuals for eligibility, and met with eligible veterans to explain study procedures and obtain informed consent. Participants consented to group psychotherapy, video recording of sessions, monthly psychotropic medication visits, random toxicology screens, and research assessments at baseline and every 3 months. Veterans agreed to participate only in the assigned form of treatment (except pharmacotherapy and 12-step meetings) for the duration of group psychotherapy. Rates of prescription antidepressant utilization during the group psychotherapy phase were high for both treatment conditions (TSF = 94%, ICBT = 90%).
Group Treatments
Group psychotherapy was initiated via a rolling admission procedure, with start dates scheduled every 2 weeks and alternating assignment of patients to the condition with the next start date. Group sessions occurred twice/week for the first 3 months and weekly for the next 3 months. Session attendance was not significantly different (M = 22 of 36 sessions) across groups. Both interventions were co-delivered by senior clinicians and doctoral students trained to criterion via manual review, direct observation, and weekly supervision. Therapists rotated across treatment conditions every 6–12 months and treatment adherence was assessed via client report of content and videotape review. The TSF and ICBT groups did not differ significantly on the demographic and clinical characteristics assessed at baseline (see Table 1).
For the TSF condition we modified TSF [40] from Project MATCH [41] to allow focus on multiple substances and group delivery. The three core modules of the TSF protocol covered Steps 1–3, general Twelve-Step topics and literature, and Steps 4–5. Sessions involved discussions of 12-step readings and recovery tasks (e.g., talking to sponsor). Depression was only discussed in the context of 12-Step themes. For ICBT, material was adapted from two empirically-validated treatments: group cognitive-behavioral treatment of depression [42] and cognitive-behavioral therapy from Project MATCH [43]. The three core modules of ICBT were Thoughts (e.g., challenging cognitions), Activities (e.g., increasing positive activities), and Interpersonal (e.g., communication and assertiveness training).
Measures
All measures were obtained at intake, mid-treatment (Month 3), end-of-treatment (Month 6), and 3-month follow-up (Month 9). Follow-up rates were high (Month 3 = 99%, Month 6 = 94%, Month 9 = 89%). Summary statistics for the following measures, by treatment group and time, are presented in Table 2.
Table 2.
12-step variables, depression, alcohol use, and drug use at each wave by treatment condition.
| Month | |||||
|---|---|---|---|---|---|
| Intake | 3 | 6 | 9 | ||
| M (SD) | M (SD) | M (SD) | M (SD) | ||
| Past month | TSF | 0.50 (.33) | 0.49 (.31) | 0.44 (.30) | - |
| 12-step attendance a | ICBT | 0.48 (.31) | 0.34 (.31) | 0.25 (.27) | - |
| Past month | TSF | 2.26 (1.33) | 2.56 (1.33) | 2.55 (1.38) | - |
| 12-step affiliationb | ICBT | 2.15 (1.19) | 2.06 (1.34) | 1.78 (1.33) | - |
| HAMDc | TSF | 27.81 (11.55) | 23.99 (12.81) | 19.00 (10.90) | - |
| ICBT | 29.19 (10.08) | 26.04 (12.57) | 24.92 (13.5) | - | |
| Percent Days | TSF | 26.36 (24.82) | 6.90 (16.50) | 8.71 (20.08) | 11.78 (23.98) |
| Drinking | ICBT | 21.61 (22.49) | 8.54 (17.53) | 12.35 (23.49) | 11.45 (21.19) |
| Percent Days | TSF | 11.58 (21.26) | 3.15 (13.21 ) | 4.16 (11.84) | 3.60 (13.18) |
| Using Drugs | ICBT | 10.78 (20.26) | 2.88 (9.14) | 3.94 (12.85) | 4.94 (15.27) |
Note. TSF: Twelve-Step Facilitation; ICBT: Integrated Cognitive-Behavioral Therapy; HAMD: Hamilton Depression Rating Scale.
Ordinal scale (0 = “None”, .25 = “1 to 10”, .50 = “11–20”, .75 = “21 to 30”, 1 = “More than 30”).
Range = 0–4 affiliation behaviors.
Range = 0–60.
12-step meeting attendance and affiliation
The Alcoholics Anonymous Affiliation Scale [45] was used to measure 12-step meeting attendance and affiliation in the past month. Attendance at 12-step meetings was captured by one ordinal item measuring the number of meetings attended (0 = “None”, .25 = “1 to 10”, .50 = “11–20”, .75 = “21 to 30”, 1 = “More than 30”). Affiliation with 12-step (e.g., having a sponsor, doing service, reading literature, having a spiritual awakening) was measured by a summary score of four binary items (Range 0–4). Given prior differences between 12-step attendance and affiliation in predicting substance use [44], we examined these constructs separately, utilizing the 12-step variables from intake, Month 3, and Month 6.
Depressive symptoms
The Hamilton Depression Rating Scale [46], a structured clinical interview previously validated with MDD [47] and SUD populations [48] was used to assess depressive symptoms in the past week. Reliability of the HAMD ranged from .78 to .85 across all assessments. This study used the HAMD total score (Range 0–60) from intake, Month 3, and Month 6.
Frequency of alcohol and drug use
Alcohol and drug use was assessed with the Timeline Follow-Back (TLFB [49]), a calendar-assisted interview with documented reliability and validity [50]. We used the TLFB to separately measure the frequency of alcohol and drug use. The primary outcome variables were percent days drinking (PDD) and percent days using drugs (PDDRG) during the previous 90 days. PDD and PDDRG from intake and Months 3, 6, and 9 were utilized in analyses.
Statistical methods
Multilevel analyses
We employed hierarchical linear models (HLMs) to examine the relations between treatment condition, 12-step variables, depression, and alcohol/drug use in multilevel mediation analyses [51]. The use of HLM allows inclusion of multiple time points nested within individuals and both static and time-varying covariates. By examining associations between sets of time-varying predictors and outcomes, these analyses were akin to running multiple models for multiple time points and averaging their effects. We included all available data via maximum likelihood estimation, a preferred method of estimation when the data contain information that is assumed missing-at-random [52]. Analyses revealed no differences on any study variables between individuals with complete data and those with any missing data, supporting this assumption.
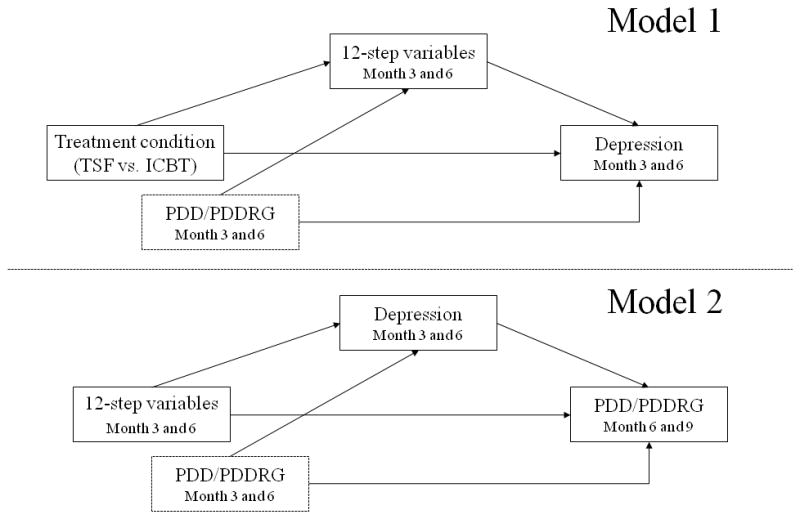
Separate HLMs were conducted in Stata 10.1 [53] to examine individual paths in each mediation model (see Figure 1). Covariates for each HLM included treatment group, time, baseline level of outcome, demographics (age, gender, ethnicity, level of education) and post-traumatic stress disorder (PTSD), as these covariates have previously predicted substance use in this sample [54] or others [55]. Repeated variables were treated as time-varying covariates, with PDD and PDDRG as time-varying covariates in the final HLMs to determine if effects were independent of current alcohol and drug use. Finally, in Model 2 all time-varying covariates were lagged, with prior variables predicting future (3 months later) alcohol and drug use.
Figure 1.
Statistical test of mediation
Consistent with current conventions in mediation analysis [17], formal tests to estimate the magnitude, statistical significance, and effect sizes of mediated effects were computed using products-of-coefficients with asymmetric 95% confidence limits, which has more accurate Type I error rates and greater power to detect mediated effects than alternate approaches [56]. Estimates of mediated effects and confidence limits were obtained using the PRODCLIN program [57] by importing coefficients and standard errors from the HLMs. Mediated effect size was reported with the proportion of the direct effect explained by the mediated effect [17].
Results
Relations between treatment condition, 12-step variables, and depression
Effects of treatment condition on depression and 12-step variables
Separate HLMs examined the effect of treatment group on depression and 12-step variables during active treatment, controlling for covariates. No covariates significantly predicted 12-step attendance, affiliation, or depression. Consistent with prior reports of this sample [37], TSF had significantly lower levels of depression during active treatment as compared to ICBT (see Table 3). The TSF group also had greater 12-step meeting attendance (b = 0.14, p < 0.001) and affiliation (b = 0.54, p < 0.001).
Table 3.
Hierarchical linear modeling results for 12-step variables (Month 3/6) predicting depression (Month 3/6).
| Direct effect model | Mediator model | Mediator model controlling for substance use | |
|---|---|---|---|
|
| |||
| b (SE) | b (SE) | b (SE) | |
| Baseline HAMD | 0.56 (0.06)*** | 0.54 (0.07)*** | 0.53 (0.06)*** |
| Treatment group | −3.30 (1.39)* | −2.19 (1.48) | −2.29 (1.42) |
| Month | −0.94 (0.31)** | −0.86 (0.32)** | −0.90 (0.33)** |
| 12-step attendance | - | −6.16 (2.51)* | −5.69 (2.08)** |
| 12-step affiliation | - | −.38 (.61) | -a |
| PDD | - | - | 0.09 (0.03)* |
| PDDRG | - | - | 0.12 (0.06)* |
Note. HAMD: Hamilton Depression Rating Scale; PDD: percent days drinking; PDDRG: percent days using drugs. Non-significant covariates included age, gender, ethnicity, level of education, and post-traumatic stress disorder (coefficients not shown).
Predictor was not retained in final model.
p < .05,
p < .01,
p < .001.
Effects of 12-step variables on depression
Separate HLMs examined the effects of 12-step attendance and affiliation on depression at Months 3 and 6, controlling for treatment condition, baseline depression, time, and other covariates (see Table 3). Greater 12-step attendance (b = −7.06, p = 0.001) and greater 12-step affiliation (b = −1.23, p = 0.014) both predicted lower depression, and the effect of treatment condition was no longer statistically significant. When examining the 12-step variables simultaneously, only 12-step meeting attendance independently predicted depression (p = 0.014), thus further analyses did not include 12-step affiliation.
A final model included current (Month 3 and 6) PDD and PDDRG as time-varying predictors of depression, to determine if the effects of 12-step meetings on depression were independent of current alcohol and drug use. Lower PDD and PDDRG both significantly predicted lower depression (see Table 3). Controlling for these effects, greater 12-step meeting attendance still predicted lower depression (p = 0.006), indicating that relations between meeting attendance and depression were independent of current drinking and drug use.
Multilevel mediation test
To assess the statistical and clinical significance of mediation we obtained an estimate of the mediated effect with asymmetric 95% confidence intervals. In Model 1 this refers to the specific portion of the group difference (TSF vs. ICBT) on depression that is mediated through 12-step meeting attendance. These results (b = − 0.80, 95% CI [−1.59, − 0.20], p < 0.05) indicated that the effect of TSF on depression was mediated through 12-step meeting attendance, with the mediated effect explaining 24.3% of the direct effect of TSF on depression.
Relations between 12-step attendance, depression, and substance use
Effects of 12-step attendance on future alcohol and drug use
Lagged measures of 12-step attendance at Months 3 and 6 were used to predict future (Month 6 and 9) frequency of drinking and drug use, controlling for covariates, none of which significantly predicted drinking or drug use in the subsequent HLMs. As shown in Table 4, greater 12-step meeting attendance significantly predicted lower future PDD ( p = 0.029) but not future PDDRG (p = 0.18). This indicated individuals with greater 12-step meeting attendance had lower future drinking frequency, but 12-step attendance was not significantly related to future drug use.
Table 4.
Hierarchical linear modeling results for lagged 12-step attendance and depression (Month 3/6) predicting future alcohol and drug use (Month 6/9).
| Direct effect model | Mediator model | Mediator model controlling for substance use | |
|---|---|---|---|
|
| |||
| b (SE) | b (SE) | b (SE) | |
| Post-treatment drinking | |||
| Baseline PDD | 0.12 (0.06)* | 0.13 (0.05)* | - |
| Treatment group | −0.33 (2.76) | 0.53 (2.69) | 1.12 (2.11) |
| Month | 0.76 (0.44) | 0.94 (0.46)* | 0.73 (0.54) |
| Lagged 12-step attendance | −7.22 (3.39)* | −4.75 (3.43) | −2.50 (3.27) |
| Lagged HAMD | - | 0.31 (0.08 )*** | 0.19 (0.08 )* |
| Lagged PDD | 0.49 (0.06)*** | ||
| Post-treatment drug use | |||
| Baseline PDDRG | 0.03 (0.05) | 0.03 (0.05) | - |
| Treatment group | 0.74 (1.94) | 0.82 (1.97) | −0.75 (1.74) |
| Month | 1.50 (1.03) | 1.50 (1.07) | 0.36 (0.39) |
| Lagged 12-step attendance | −3.38 (2.50) | −3.60 (2.60) | −3.34 (2.52) |
| Lagged HAMD | - | −.02 (0.06) | −.03 (0.06) |
| Lagged PDDRG | 0.39 (0.08)*** | ||
Note. HAMD: Hamilton Depression Rating Scale; PDD: percent days drinking; PDDRG: percent days using drugs. Non-significant covariates included age, gender, ethnicity, level of education, and post-traumatic stress disorder (coefficients not shown).
p < .05,
p < .01,
p < .001.
Effects of depression on future alcohol and drug use
Support for the predictor-to-mediator path in Model 2 (12-step attendance predicting depression) was previously established in Model 1. To complete Model 2 analyses, we examined the mediator-to-outcome path by testing whether depression at Month 3 and 6 predicted future (Month 6 and 9) alcohol and drug use, controlling for the effects of the predictor (12-step attendance). As shown in Table 4, lower lagged depression significantly predicted lower future PDD (p < .001) but not future PDDRG (p = .75). The effects of 12-step attendance were no longer statistically significant (p = .17).
Given that effects of depression on future drinking could be confounded by current drinking, our final model controlled for the effects of lagged PDD. As shown in Table 4, prior PDD was significantly and strongly related to future PDD (p < .001), but lagged depression was still significantly predictive of future PDD (p = .017). In other words, lower month 3 and 6 depression uniquely predicted lower drinking at months 6 and 9, above and beyond the effects of prior drinking.
Multilevel mediation test
In Model 2 the mediated effect refers to the specific portion of the relationship between 12-step meeting attendance and future drinking that is mediated through depressive symptoms. Results (b = − 1.16, 95% CI [−2.57, −0.18], p < 0.05) indicated that the effect of 12-step meeting attendance on future drinking was significantly mediated through depression, explaining 15.7% of the direct effect.
Discussion
In our original trial of ICBT and TSF for adults with SUD and MDD, the ICBT group was expected to have superior reductions in depression symptoms during treatment, but the results were contrary to these expectations [35, 37]. The current study utilized mediation analyses to examine whether greater engagement in 12-step resources explained lower within-treatment depression for the TSF condition. Greater attendance at community-based 12-step meetings was associated with lower depression and mediated the group difference in depression, providing preliminary evidence for 12-step attendance as a therapeutic mechanism for reductions in depressive symptoms. Others have noted that general therapeutic factors inherent to self-help groups (e.g., social contact) may be especially helpful for SUD patients with psychiatric conditions [58], and patients in TSF likely gained greater exposure to such therapeutic factors through greater community 12- step meeting attendance. Greater meeting attendance could also signal greater behavioral activation, a component of effective psychotherapy for depression [59]. While interpersonal and behavioral coping skills were also targeted in ICBT, our findings suggest 12-step meetings could be an important and readily accessible vehicle for general symptom reduction in patients with SUD and MDD. While the ICBT group had less reduction in depression during treatment, our prior report revealed superior post-treatment depressive symptoms and substance use for ICBT [37], and future studies of this sample may provide insight into the unique vs. common mechanisms that explain differential patterns of symptom change in these alternative treatments.
Consistent with prior studies [32, 60] greater 12-step meeting attendance predicted lower future drinking. However, our study was unique in finding this effect was mediated by depression, even when controlling for current drinking. In a similar study of Project MATCH, depressive symptoms were not uniquely related to meeting attendance or future drinking when current drinking was controlled [32]. This discrepancy suggests that changes in depressive symptoms linked to 12-step meeting attendance may be an especially critical therapeutic process for patients with comorbid MDD. Other studies suggest negative affect has a large role in the maintenance of substance use for these patients. Individual changes in depression and substance use were highly correlated in this sample [34], and SUD patients with MDD are more likely to experience depressed mood prior to relapse [33]. The importance of negative affect was also confirmed in recent work with Project MATCH [61], in which the mediating effects of depression were significant and independent of other process variables (e.g., social networks, self-efficacy, spirituality) in the aftercare sample, who may be more representative of patients enrolled in our study. In our sample 12-step meeting attendance no longer predicted future drinking when accounting for the mediating effects of depressive symptoms. This suggests that even when treatment processes focus explicitly on substance use, ancillary effects on mood may be an important mechanism of change for patients with comorbid MDD. Conversely, patients with depressive symptoms that persist despite continued abstinence and frequent 12-step meeting attendance may need additional interventions to control depression and prevent future relapse.
Two aspects of our hypotheses were not confirmed and merit discussion. When examined concurrently, 12-step affiliation did not predict depression independent of 12-step meeting attendance. While 12-step meetings may be more instrumental in reducing depressive symptoms due to the positive effects of social interaction and behavioral activation, the lack of effects for affiliation here could also be due to statistical and methodological limitations. The two 12-step variables were highly correlated (.65-.69) at each wave, and this multicollinearity could have biased regression coefficients [62]. Our measure of 12-step affiliation was brief and basic, and other measures may capture detailed components of affiliation [63] more predictive of depression. Secondly, future drug use was not predicted by 12-step attendance or depression. We had less power to detect this effect, because fewer patients were drug-dependent or using drugs at intake. Still, the effects of 12-step meetings could be stronger for patients who primarily use alcohol, possibly due to greater availability of specific meetings (e.g., AA). The effects of 12-step meetings have differed between alcohol and drug users in prior research [64], so the lack of effects on drug use in this study may be important and deserving of further exploration.
This study has limitations, most notably in the sample’s restricted demographic characteristics which limit the generalizability of findings. These results may be applicable to a large proportion of SUD patients due to the high prevalence of comorbid MDD in clinical settings [8, 9], but replication in other samples is needed. Importantly, factors other than 12-step meeting attendance (e.g., antidepressants, psychotherapy content) could have accounted for better initial depression response in TSF, but the groups had similar attendance at group therapy sessions and similar rates of antidepressant medication use. Temporal precedence between 12-step attendance and depression was not explicitly tested here, and more rigorous models could examine lagged effects of 12-step attendance on future depression. Also, our measure of 12-step attendance did not differentiate between different meetings (e.g., AA vs. NA), which may have helped investigate the lack of effects on drug use. Finally, while we controlled for the effects of comorbid PTSD on all outcomes, we did not explore more intricate (e.g., moderating) effects that may be of interest due to the high prevalence of PTSD in this population.
Our study provides preliminary evidence that among patients with SUD and MDD receiving TSF, reduction in depression is mediated by greater 12-step meeting attendance, and that reductions in depression related to 12-step attendance can also occur for patients receiving other (e.g., cognitive-behavioral) forms of therapy. Importantly, reductions in depressive symptoms appear to mediate the effects of 12-step meeting attendance on future drinking outcomes among patients with SUD and MDD, regardless of treatment condition. Because our lagged analyses controlled for prior substance use, this study provides strong initial support for reduced depression as a mechanism through which 12-step attendance influences future drinking in adults with SUD and comorbid MDD.
Acknowledgments
This research was funded by Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Clinical Sciences Research & Development Merit Review Awards to Dr. Sandra A. Brown and Dr. Susan R. Tate. Preparation of this manuscript was supported by National Institute on Drug Abuse fellowship grant (F31DA030861) awarded to Matthew J. Worley. Portions of this research were presented at the 2011 Meeting of the Research Society on Alcoholism (RSA) and the 2011 RSA Mechanisms of Behavior Change pre-conference satellite meeting.
Footnotes
Clinical trials registration: Clinicaltrials.gov identifiers NCT00108407 and NCT00018655.
Declarations of interest: Research funded by Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Clinical Sciences Research & Development Merit Review Awards to Dr. Sandra A. Brown and Dr. Susan R. Tate, and by National Institute on Drug Abuse fellowship grant (F31DA030861) awarded to Matthew J. Worley.
Contributor Information
Matthew J. Worley, San Diego State University/University of California, San Diego Joint Doctoral Program in Clinical Psychology
Susan R. Tate, San Diego Veterans Affairs Healthcare System
Sandra A. Brown, University of California, San Diego
References
- 1.Grant BF, Stinson FS, Dawson DA, Chou P, Dufour MC, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 2.Hasin D, Liu X, Nunes E, McCloud S, Samet S, et al. Effects of major depression on remission and relapse of substance dependence. Archives of General Psychiatry. 2002;59:375–80. doi: 10.1001/archpsyc.59.4.375. [DOI] [PubMed] [Google Scholar]
- 3.Wilk J, West JC, Rae DS, Regier DA. Relationship of comorbid substance and alcohol use disorders to disability among patients in routine psychiatric practice. American Journal on Addictions. 2006;15:180–185. doi: 10.1080/10550490500528799. [DOI] [PubMed] [Google Scholar]
- 4.Curran GM, Sullivan G, Williams K, Han XT, Collins K, et al. Emergency department use of persons with comorbid psychiatric and substance abuse disorders. Annals of Emergency Medicine. 2003;41:659–667. doi: 10.1067/mem.2003.154. [DOI] [PubMed] [Google Scholar]
- 5.O’Toole TP, Pollini RA, Ford DE, Bigelow G. The effect of integrated medical-substance abuse treatment during an acute illness on subsequent health services utilization. Medical Care. 2007;45:1110–1115. doi: 10.1097/MLR.0b013e318127142b. [DOI] [PubMed] [Google Scholar]
- 6.Bolton JM, Pagura J, Enns MW, Grant B, Sareen J. A population-based longitudinal study of risk factors for suicide attempts in major depressive disorder. Journal of Psychiatric Research. 2010;44:817–26. doi: 10.1016/j.jpsychires.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glasner-Edwards S, Mooney LJ, Marinelli-Casey P, Hillhouse M, Ang A, et al. Risk factors for suicide attempts in methamphetamine-dependent patients. American Journal on Addictions. 2008;17:24–7. doi: 10.1080/10550490701756070. [DOI] [PubMed] [Google Scholar]
- 8.Lynskey MT. The comorbidity of alcohol dependence and affective disorders: treatment implications. Drug and Alcohol Dependence. 1998;52:201–9. doi: 10.1016/s0376-8716(98)00095-7. [DOI] [PubMed] [Google Scholar]
- 9.Chi FW, Satre DD, Weisner C. Chemical dependency patients with cooccurring psychiatric diagnoses: service patterns and 1-year outcomes. Alcoholism: Clinical and Experimental Research. 2006;30:851–9. doi: 10.1111/j.1530-0277.2006.00100.x. [DOI] [PubMed] [Google Scholar]
- 10.Leventhal AM, Mooney ME, DeLaune KA, Schmitz JM. Using addiction severity profiles to differentiate cocaine-dependent patients with and without comorbid major depression. American Journal on Addictions. 2006;15:362–9. doi: 10.1080/10550490600860148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Curran GM, Flynn HA, Kirchner J, Booth BM. Depression after alcohol treatment as a risk factor for relapse among male veterans. Journal of Substance Abuse Treatment. 2000;19:259–265. doi: 10.1016/s0740-5472(00)00107-0. [DOI] [PubMed] [Google Scholar]
- 12.Ilgen M, Moos R. Deterioration Following Alcohol-Use Disorder Treatment in Project MATCH. Journal of Studies on Alcohol. 2005;66:517–525. doi: 10.15288/jsa.2005.66.517. [DOI] [PubMed] [Google Scholar]
- 13.Gamble SA, Conner KR, Talbot NL, Yu Q, Tu XM, et al. Effects of pretreatment and posttreatment depressive symptoms on alcohol consumption following treatment in Project MATCH. Journal of Studies on Alcohol and Drugs. 2010;71:71–7. doi: 10.15288/jsad.2010.71.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levin FR, Bisaga A, Raby W, Aharonovich E, Rubin E, et al. Effects of major depressive disorder and attention-deficit/hyperactivity disorder on the outcome of treatment for cocaine dependence. Journal of Substance Abuse Treatment. 2008;34:80–89. doi: 10.1016/j.jsat.2006.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Glasner-Edwards S, Marinelli-Casey P, Hillhouse M, Ang A, Mooney LJ, et al. Depression Among Methamphetamine Users Association With Outcomes From the Methamphetamine Treatment Project at 3-Year Follow-Up. Journal of Nervous and Mental Disease. 2009;197:225–231. doi: 10.1097/NMD.0b013e31819db6fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Longabaugh R. The search for mechanisms of change in behavioral treatments for alcohol use disorders: a commentary. Alcoholism: Clinical and Experimental Research. 2007;31:21s–32s. doi: 10.1111/j.1530-0277.2007.00490.x. [DOI] [PubMed] [Google Scholar]
- 17.MacKinnon DP. Introduction to statistical mediation analysis. New York: Lawrence Erlbaum Associates; 2008. [Google Scholar]
- 18.Longabaugh R, Magill M. Recent Advances in Behavioral Addiction Treatments: Focusing on Mechanisms of Change. Current Psychiatry Reports. 2011;13(5):382–389. doi: 10.1007/s11920-011-0220-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ouimette PC, Moos RH, Finney JW. Influence of outpatient treatment and 12-step group involvement on one-year substance abuse treatment outcomes. Journal of Studies on Alcohol. 1998;59:513–22. doi: 10.15288/jsa.1998.59.513. [DOI] [PubMed] [Google Scholar]
- 20.Tonigan JS, Toscova R, Miller WR. Meta-analysis of the literature on Alcoholics Anonymous: sample and study characteristics moderate findings. Journal of Studies on Alcohol. 1996;57:65–72. doi: 10.15288/jsa.1996.57.65. [DOI] [PubMed] [Google Scholar]
- 21.Subbaraman MS, Kaskutas LA, Zemore S. Sponsorship and service as mediators of the effects of Making Alcoholics Anonymous Easier (MAAEZ), a 12-step facilitation intervention. Drug and Alcohol Dependence. 2011;116:117–24. doi: 10.1016/j.drugalcdep.2010.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Walitzer KS, Dermen KH, Barrick C. Facilitating involvement in Alcoholics Anonymous during out-patient treatment: a randomized clinical trial. Addiction. 2009;104:391–401. doi: 10.1111/j.1360-0443.2008.02467.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bogenschutz MP, Geppert CM, George J. The role of twelve-step approaches in dual diagnosis treatment and recovery. American Journal on Addictions. 2006;15:50–60. doi: 10.1080/10550490500419060. [DOI] [PubMed] [Google Scholar]
- 24.Kelly JF, McKellar JD, Moos R. Major depression in patients with substance use disorders: Relationship to 12-Step self-help involvement and substance use outcomes. Addiction. 2003;98:499–508. doi: 10.1046/j.1360-0443.2003.t01-1-00294.x. [DOI] [PubMed] [Google Scholar]
- 25.Noordsy DL, Schwab B, Fox L, Drake RE. The role of self-help programs in the rehabilitation of persons with severe mental illness and substance use disorders. Community Mental Health Journal. 1996;32:71–81. doi: 10.1007/BF02249369. [DOI] [PubMed] [Google Scholar]
- 26.Alcoholics-Anonymous. Twelve steps and Twelve Traditions. New York, NY: Alcoholics Anonymous Publishing; 1953. [Google Scholar]
- 27.Laudet AB, Cleland CM, Magura S, Vogel HS, Knight EL. Social support mediates the effects of dual-focus mutual aid groups on abstinence from substance use. American Journal of Community Psychology. 2004;34:175–85. doi: 10.1007/s10464-004-7413-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zywiak WH, Connors GJ, Maisto SA, Westerberg VS. Relapse research and the Reasons for Drinking Questionnaire: a factor analysis of Marlatt’s relapse taxonomy. Addiction. 1996;91(Suppl):S121–30. [PubMed] [Google Scholar]
- 29.Witkiewitz K, Villarroel NA. Dynamic association between negative affect and alcohol lapses following alcohol treatment. Journal of Consulting and Clinical Psychology. 2009;77:633–644. doi: 10.1037/a0015647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jaffe A, Shoptaw S, Stein JA, Reback CJ, Rotheram-Fuller E. Depression ratings, reported sexual risk behaviors, and methamphetamine use: Latent growth curve models of positive change among gay and bisexual men in an outpatient treatment program. Experimental and Clinical Psychopharmacology. 2007;15:301–307. doi: 10.1037/1064-1297.15.3.301. [DOI] [PubMed] [Google Scholar]
- 31.Stulz N, Crits-Christoph P, Thase ME, Gallop R. Psychosocial treatments for cocaine dependence: The role of depressive symptoms. Drug and Alcohol Dependence. 2011;114:41–48. doi: 10.1016/j.drugalcdep.2010.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kelly JF, Stout RL, Magill M, Tonigan JS, Pagano ME. Mechanisms of behavior change in alcoholics anonymous: does Alcoholics Anonymous lead to better alcohol use outcomes by reducing depression symptoms? Addiction. 2010;105:626–36. doi: 10.1111/j.1360-0443.2009.02820.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tomlinson KL, Tate SR, Anderson KG, McCarthy DM, Brown SA. An examination of self-medication and rebound effects: Psychiatric symptomatology before and after alcohol or drug relapse. Addictive Behaviors. 2006;31:461–474. doi: 10.1016/j.addbeh.2005.05.028. [DOI] [PubMed] [Google Scholar]
- 34.Worley MJ, Tate SR, Brown SA. Mediational Relations between 12-step Meeting Attendance, Depression, and Substance Use during and after Treatment for Comorbidity. (in press) [Google Scholar]
- 35.Brown SA, Glasner-Edwards SV, Tate SR, McQuaid JR, Chalekian J, et al. Integrated cognitive behavioral therapy versus twelve-step facilitation therapy for substance-dependent adults with depressive disorders. Journal of Psychoactive Drugs. 2006;38:449–460. doi: 10.1080/02791072.2006.10400584. [DOI] [PubMed] [Google Scholar]
- 36.Glasner-Edwards S, Tate SR, McQuaid JR, Cummins K, Granholm E, et al. Mechanisms of action in integrated cognitive-behavioral treatment versus twelve-step facilitation for substance-dependent adults with comorbid major depression. Journal of Studies on Alcohol and Drugs. 2007;68:663–72. doi: 10.15288/jsad.2007.68.663. [DOI] [PubMed] [Google Scholar]
- 37.Lydecker KP, Tate SR, Cummins KM, McQuaid J, Granholm E, et al. Clinical outcomes of an integrated treatment for depression and substance use disorders. Psychology of Addictive Behaviors. 2010;24:453–65. doi: 10.1037/a0019943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brown SA, Vik PW, Patterson TL, Grant I, Schuckit MA. Stress, vulnerability and adult alcohol relapse. Journal of Studies on Alcohol. 1995;56:538–45. doi: 10.15288/jsa.1995.56.538. [DOI] [PubMed] [Google Scholar]
- 39.Robins LN, Wing J, Wittchen HU, Helzer JE, Babor TF, et al. The Composite International Diagnostic Interview. An epidemiologic Instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiatry. 1988;45:1069–77. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- 40.Nowinski J, Baker S, Carroll K. Twelve step facilitation therapy manual : a clinical research guide for therapists treating individuals with alcohol abuse and dependence. Rockville, Md: U.S. Dept. of Health and Human Services, Public Health Service, National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism; 2007. [Google Scholar]
- 41.Project Match Research Group. Matching Alcoholism Treatments to Client Heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- 42.Muñoz RF, Ying Y-W. The Prevention of Depression: Research and Practice. Baltimore: Johns Hopkins University Press; 1993. [Google Scholar]
- 43.Kadden RM. Cognitive-behavioral coping skills therapy manual : a clinical research guide for therapists treating individuals with alcohol abuse and dependence. Rockville, Md: U.S. Dept. of Health and Human Services, Public Health Service, National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism; 1995. [Google Scholar]
- 44.Weiss RD, Griffin ML, Gallop RJ, Najavits LM, Frank A, et al. The effect of 12-step self-help group attendance and participation on drug use outcomes among cocaine-dependent patients. Drug and Alcohol Dependence. 2005;77:177–84. doi: 10.1016/j.drugalcdep.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 45.Humphreys K, Kaskutas LA, Weisner C. The Alcoholics Anonymous Affiliation Scale:Development, reliability, and norms for diverse treated and untreated populations. Alcoholism: Clinical and Experimental Research. 1998;22:974–8. doi: 10.1111/j.1530-0277.1998.tb03691.x. [DOI] [PubMed] [Google Scholar]
- 46.Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Knesevich JW, Biggs JT, Clayton PJ, Ziegler VE. Validity of the Hamilton Rating Scale for depression. Br J Psychiatry. 1977;131:49–52. doi: 10.1192/bjp.131.1.49. [DOI] [PubMed] [Google Scholar]
- 48.Willenbring ML. Measurement of depression in alcoholics. Journal of Studies on Alcohol. 1986;47:367–72. doi: 10.15288/jsa.1986.47.367. [DOI] [PubMed] [Google Scholar]
- 49.Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: Psychosocial and biochemical methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- 50.Maisto SA, Sobell LC, Sobell MB. Comparison of alcoholics’ self-reports of drinking behavior with reports of collateral informants. Journal of Consulting and Clinical Psychology. 1979;47:106–112. [PubMed] [Google Scholar]
- 51.Krull JL, MacKinnon DP. Multilevel modeling of individual and group level mediated effects. Multivariate Behavioral Research. 2001;36:249–277. doi: 10.1207/S15327906MBR3602_06. [DOI] [PubMed] [Google Scholar]
- 52.Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–77. [PubMed] [Google Scholar]
- 53.StataCorp. Stata Statistical Software: Release 10. College Station, TX: StataCorp LP; 2007. [Google Scholar]
- 54.Norman SB, Tate SR, Wilkins KC, Cummins K, Brown SA. Posttraumatic stress disorder’s role in integrated substance dependence and depression treatment outcomes. J Subst Abuse Treat. 2010;38:346–55. doi: 10.1016/j.jsat.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 55.Adamson SJ, Sellman JD, Frampton CM. Patient predictors of alcohol treatment outcome: a systematic review. J Subst Abuse Treat. 2009;36:75–86. doi: 10.1016/j.jsat.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 56.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.MacKinnon DP, Fritz MS, Williams J, Lockwood CM. Distribution of the product confidence limits for the indirect effect: program PRODCLIN. Behavioral Research Methods. 2007;39:384–9. doi: 10.3758/bf03193007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Moos RH. Active ingredients of substance use-focused self-help groups. Addiction. 2008;103:387–96. doi: 10.1111/j.1360-0443.2007.02111.x. [DOI] [PubMed] [Google Scholar]
- 59.Dimidjian S, Barrera M, Martell C, Munoz RF, Lewinsohn PM. The Origins and Current Status of Behavioral Activation Treatments for Depression. Annual Review of Clinical Psychology. 2011;7:1–38. doi: 10.1146/annurev-clinpsy-032210-104535. [DOI] [PubMed] [Google Scholar]
- 60.McCrady BS, Epstein EE, Kahler CW. Alcoholics anonymous and relapse prevention as maintenance strategies after conjoint behavioral alcohol treatment for men: 18-month outcomes. Journal of Consulting and Clinical Psychology. 2004;72:870–8. doi: 10.1037/0022-006X.72.5.870. [DOI] [PubMed] [Google Scholar]
- 61.Kelly JF, Hoeppner B, Stout RL, Pagano M. Determining the relative importance of the mechanisms of behavior change within Alcoholics Anonymous: a multiple mediator analysis. Addiction. 2012;107:289–99. doi: 10.1111/j.1360-0443.2011.03593.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Raudenbush SW, Bryk AS. Hierarchical linear models : Applications and data analysis methods. Thousand Oaks: Sage Publications; 2002. [Google Scholar]
- 63.Klein AA, Slaymaker VJ, Kelly JF. The 12 Step Affiliation and Practices Scale: Development and initial validation of a measure assessing 12 step affiliation. Addictive Behaviors. 2011;36:1045–51. doi: 10.1016/j.addbeh.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tonigan JS, Beatty GK. Twelve-step program attendance and polysubstance use: interplay of alcohol and illicit drug use. Journal of Studies on Alcohol and Drugs. 2011;72:864–71. doi: 10.15288/jsad.2011.72.864. [DOI] [PMC free article] [PubMed] [Google Scholar]


