Abstract
While there is accumulating evidence to suggest that therapies using mindfulness and acceptance-based approaches have benefits for improving the symptoms of insomnia, it is unclear how these treatments work. The goal of this paper is to present a conceptual framework for the cognitive mechanisms of insomnia based upon mindfulness and acceptance approaches. The existing cognitive and behavioral models of insomnia are first reviewed and a two-level model of cognitive (primary) and metacognitive (secondary) arousal is presented in the context of insomnia. We then focus on the role of metacognition in mindfulness and acceptance-based therapies, followed by a review of these therapies in the treatment of insomnia. A conceptual framework is presented detailing the mechanisms of metacognition in the context of insomnia treatments. This model proposes that increasing awareness of the mental and physical states that are present when experiencing insomnia symptoms and then learning how to shift mental processes can promote an adaptive stance to one’s response to these symptoms. These metacognitive processes are characterized by balanced appraisals, cognitive flexibility, equanimity, and re-commitment to values and are posited to reduce sleep-related arousal, leading to remission from insomnia. We hope that this model will further the understanding and impact of mindfulness and acceptance-based approaches to insomnia.
Keywords: Insomnia, Mindfulness, Acceptance and Commitment Therapy, Sleep, Treatment Mechanisms
Novel treatments using mindfulness and acceptance-based approaches are a wave of rapidly emerging therapies. Many treatment studies and meta-analyses have demonstrated the benefits of these therapies on mental and physical health. A subset of these studies has examined the impact of mindfulness and acceptance-based therapies on sleep disturbance, collectively referred to here as metacognitive therapies for insomnia (MCTI). While there is accumulating evidence to suggest that MCTIs have benefits for improving sleep, a conceptual model to explain their potential common mechanisms is lacking.
This paper proposes a conceptual framework for the cognitive mechanisms of insomnia based upon mindfulness and acceptance approaches. First, we review the existing cognitive and behavioral models of insomnia and present a re-conceptualization of sleep-related arousal to include metacognitive processes in addition to the cognitive processes that have been previously described. Second, we examine the literature on mindfulness and acceptance which has identified metacognitive processes as a potential target for emotion regulation and reducing second order distress. Third, we present a treatment model to explain how MCTIs target secondary distress and lead to remission from an insomnia disorder. Studies that support psychopathological processes relevant to the components of the model are presented along with clinical implications for assessment and intervention. Finally, we discuss potential implications of this model and offer an agenda for future research. We hope that these concepts provide a framework that can stimulate empirical testing of the treatment mechanisms in MCTIs.
Cognitive and Behavioral Models of Insomnia: A Historical Context
Conceptualizations of insomnia have consistently focused on the notion that sleep disruptions are caused by elevated arousal. It has even been argued that insomnia is a disorder of hyperarousal that causes sleep disruption (Bonnet & Arand, 1997). Consequently, the early wave of behavioral treatments, delivered as a single component, had behavioral targets that directly or indirectly reduced arousal. Examples include progressive muscle relaxation (Jacobson, 1938) and biofeedback (Hauri, 1981) to reduce physiological arousal, paradoxical intention for reducing arousal that stems from performance anxiety (Ascher & Efran, 1978; Ascher & Turner, 1979; Turner & Ascher, 1979), stimulus control for reducing a conditioned arousal response to the bed (Bootzin, 1972), and sleep restriction therapy (Spielman, Sasky, & Thorpy, 1987), which restricts time in bed to mobilize the homeostatic drive to sleep, thus offsetting hyperarousal. Integrating these concepts into a diathesis-stress-response model, Spielman and colleagues (1987) conceptualized chronic insomnia as involving predisposing, precipitating, and perpetuating factors. Perpetuating factors include behaviors that individuals enact in an effort to cope with sleep disturbances (e.g., staying in bed to gain more sleep), but which inadvertently create arousal and perpetuate the problem.
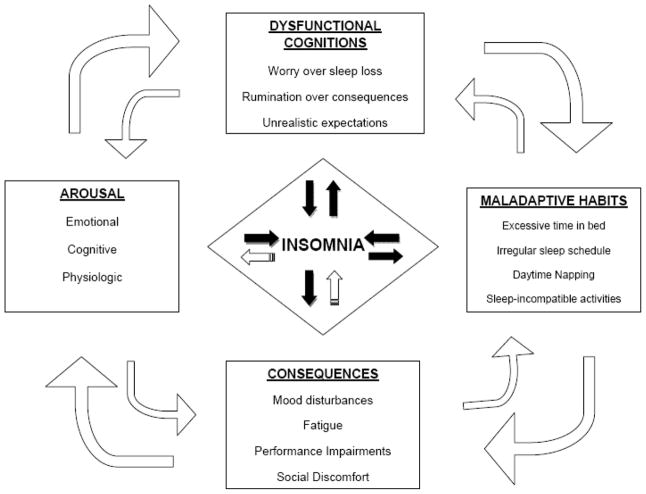
Emerging from a focus on cognitive arousal, the second wave of treatments targeted sleep-related cognitions. Investigation into sleep interfering cognitions revealed that people with insomnia hold maladaptive beliefs and attitudes about sleep (Morin, Stone, Trinkle, Mercer, & Remsberg, 1993). Based on these findings, Morin presented an integrated conceptualization of insomnia, whereby emotional, cognitive, and physiologic hyperarousal were identified as the central mediating features of insomnia (Morin, 1993). He posited that both maladaptive behaviors and arousal-producing cognitions are dysfunctional responses to poor sleep and daytime fatigue and that these responses maintain the disorder by creating a vicious cycle of insomnia (Figure 1). Morin proposed to add cognitive therapy strategies to the existing behavioral interventions in order to help patients modify their dysfunctional beliefs and attitudes about sleep. He emphasized targeting two common cognitive errors among individuals with insomnia – catastrophizing and probability over estimation (Morin, 1993). This combination of cognitive and behavioral components is now known as cognitive-behavior therapy for insomnia (CBTI) and includes stimulus control, sleep restriction, education about sleep hygiene, and cognitive therapy to address cognitive errors.
Figure 1.
Morin’s Cognitive-Behavioral Model of Insomnia, depicting the role of arousal, cognitions, behaviors, and perceived consequences in creating a cycle of insomnia.
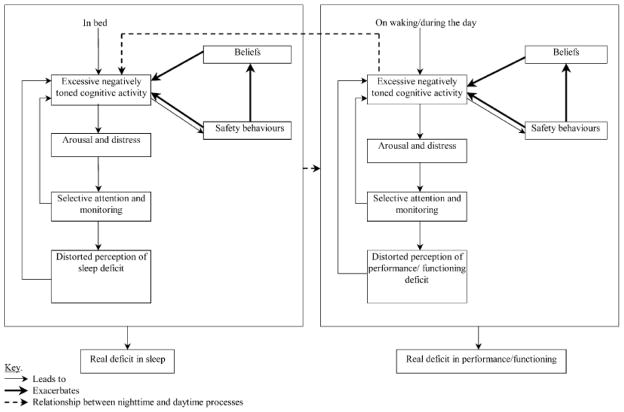
More recently, Espie (2002) has proposed a psychobiological inhibition model of insomnia that centers on the failure to de-arouse. In his model, a central process in insomnia is the loss of automaticity (i.e., sleep comes effortlessly) and plasticity (i.e., sleep is flexible) which are characteristic of good sleepers. Good sleepers are able to de-arouse at night, which facilitates the process of falling asleep. In contrast, people with insomnia have selective attention for sleep-related cues, make explicit intention to sleep, and have increased effort to sleep. This approach to sleep is maladaptive. It leads to a failure to de-arouse at night and thus inhibits the homeostatic and circadian processes that regulate sleep. Espie’s model also considers how daytime factors could contribute to insomnia. For example, inaccurate attributions of impaired daytime functioning to poor sleep may increase sleep effort and lead to performance anxiety and worse sleep. Similar to Espie, Harvey (2002) applied cognitive theories of anxiety to a model of insomnia that recognizes cognitive processes at night and during the day that could contribute to increased arousal and interfere with sleep (see Figure 2). These include worry, selective attention monitoring, misperception of sleep, unhelpful beliefs, and safety behaviors. Moreover, Harvey posits that these processes can occur with or without real deficits in sleep or daytime functioning but can lead to actual deficits in sleep and daytime function through increased arousal. Harvey has proposed and tested the use of “behavioral experiments” as a way to help people with insomnia test these sleep-related arousal inducing cognitions (Harvey, Sharpley, Ree, Stinson, & Clark, 2007). Maintaining a focus on the cognitive processes of insomnia, Lundh and Broman (2000) have proposed a theoretical model based on two cognitive processes: sleep-interfering processes and sleep-interpreting processes. They argue that most theories of insomnia (described above) focus on the sleep-interfering processes, which consist of worries, negative emotions, and thoughts related to stressful events that lead to arousal and thus interfere with sleep. Lundh and Broman (2000) argue that sleep-interfering processes alone are insufficient for explaining insomnia and that sleep-interpreting processes (i.e., thoughts, perceptions, and attributions about sleep and its consequences) might combine and interact with sleep-interfering processes to produce insomnia.
Figure 2.
Harvey’s Cognitive Model of Insomnia. This model describes how worry, selective attention monitoring, misperception of sleep, unhelpful beliefs, and safety behaviors at night and during the daytime are involved in insomnia.
A two-level model of arousal
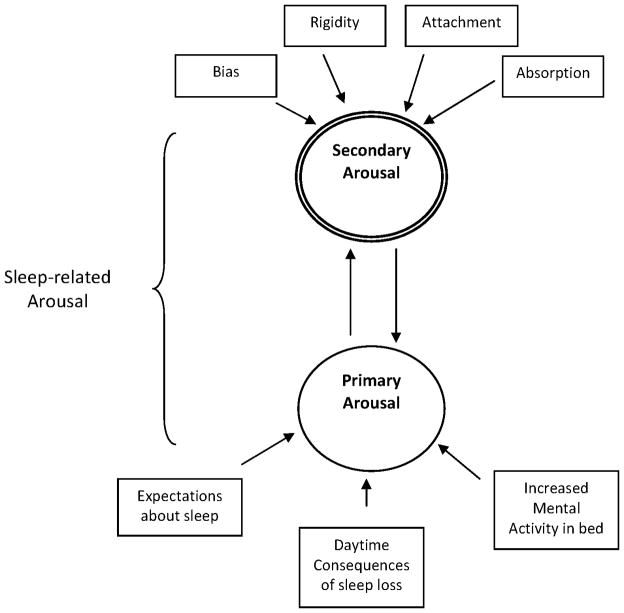
We propose further refinement of the existing concepts of cognitive arousal by introducing a two-level model of sleep-related arousal that includes metacognitive processes in addition to cognitive processes (see Figure 3). Metacognition is an awareness or knowledge of one’s own cognitive process (Flavell, 1976). This has also been referred to as “thinking about thinking” or a meta-level governing of thoughts and beliefs. In distinguishing metacognitions from cognitions, we conceptualize two levels of sleep-related cognitive arousal. Primary arousal consists of the cognitive activity directly related to the inability to sleep. This includes the thoughts that interfere with sleep and the beliefs about daytime consequences of poor or insufficient sleep. Secondary arousal consists of how one relates to thoughts about sleep. This includes the emotional valence one assigns to those thoughts, the degree of attachment one has to them, and the meaning of those thoughts in relation to one’s values (interpretive value). Therefore, secondary cognitive arousal tends to amplify the negative emotional valence and/or create a bias in the attention to and perception of sleep-related thoughts at the primary level. For example, the thought, “I need eight hours of sleep to function well the next day” can create primary arousal when the individual is lying in bed unable to sleep. A rigid attachment to this thought interferes with serious consideration of alternative beliefs and can amplify the valence, or degree of negative affect, associated with the thought, thereby creating secondary arousal. The degree to which one accepts thoughts as facts determines the valence these thoughts generate. Without the flexibility to allow competing thoughts to be considered (e.g., “I can find other ways to cope if I get less than 8 hours”), secondary arousal becomes a mechanism by which insomnia is perpetuated. Together, both primary and secondary arousal are seen as factors that promote and maintain the insomnia disorder.
Figure 3.
Two-level model of sleep-related arousal. Primary arousal refers to the cognitive content and activity that is directly related to the inability to sleep. Secondary arousal refers to the attention and emotional bias towards sleep-related thoughts, the degree of attachment one has in believing these thoughts, and the interpretive value of the sleep-related thoughts.
Rather than proposing a new model of insomnia, we consider this reformulation of sleep-related cognitive arousal to fit with existing models of insomnia described above. Metacognitive processes are closely related to the sleep-interpreting process in the Lundh and Broman (2000) model, reflecting an interpretation of the immediate experience of thoughts and feelings about insomnia. Lundh (2005) also presented the idea that mindfulness and acceptance skills might facilitate “cognitive deactivation” which is similar to the concept of reducing secondary arousal. However, this model conceptualizes sleep-interpreting processes as consisting of the content of specific interpretive thoughts as well as personality factors, whereas we conceptualize metacognitions as not directly involving the content of thoughts or personality. Metacognitive processes are also implicit in other models of insomnia, including the loss of automaticity described by Espie (2002), the selective attention given to sleep described by Harvey (2002), and the interpretive value of negative beliefs and attitudes about sleep discussed in Morin’s model (1993). However, metacognitive processes do not form an explicitly distinct component of these models. We believe that the construct of metacognitions and secondary arousal provides greater specificity and offers a way to connect cognitive arousal with treatments that include a cognitive component (CBTI, mindfulness and acceptance approaches). This formulation is consistent with recent work illuminating the role of metacognitions in mindfulness and acceptance based treatments for other psychological disorders as discussed below.
Evolution of Behavior Therapy: The Rise of Third Wave Therapies and Metacognitions
The evolution of behavioral treatments for insomnia has paralleled a trend of incorporating mindfulness and acceptance-based approaches into psychotherapy for other disorders, including mood and anxiety disorders. These are sometimes referred to as the “Third Wave” of behavior therapy (Hayes, 2004) and include Acceptance and Commitment Therapy (ACT), Mindfulness-Based Cognitive-Therapy (MBCT), and Dialectical Behavior Therapy (DBT). These Third Wave therapies have challenged the conceptualization of some forms of psychopathology and the method or target of change that is needed to return to wellness. In describing this wave of therapies, Hayes asserts that the “new behavior therapies carry forward the behavioral therapy tradition, but they (1) abandon a sole commitment to first-order change, (2) adopt more contextualistic assumptions, (3) adopt more experiential and indirect change strategies in addition to direct strategies, and (4) considerably broaden the focus of change (pg. 6, Hayes, 2004).” In that vein, mindfulness and acceptance based interventions adopt experiential and indirect (second order) change strategies, such as observing and noticing the thoughts, and considerably broaden the focus of change. These interventions directly target metacognitive processes rather than the content of cognitions. Specifically, they are aimed at creating a shift in the lens through which first order cognitions are viewed. Although the first and second order changes are seen as distinct processes, the two processes interact and guide one another.
The importance of metacognitive processes (second order) in regulating emotional distress can be traced back to the Buddhist influence on mindfulness-based interventions. Impermanence is a central theme in Buddhism and is related to the polarization of attraction and aversion in which all things come and go; the attachment to desired outcomes is what leads to suffering. From this perspective, psychological distress is directly related to the extent to which one is attached to certain outcomes or the way things “ought to be” (the degree of non-acceptance). This attachment leads to rigidity and restricted range in one’s psychological and physiological responses to distress that may be ineffective and therefore could lead to mood dysregulation, physiological dysregulation, and other negative consequences of prolonged stress.
Interventions using mindfulness meditation are based upon the idea that cultivating intentional awareness of the present moment, self-compassion, and non-attachment to outcomes (acceptance of present state) can enhance one’s ability to respond to mental and physical states with a wider range of options rather than reacting to them, often in an automatic and ineffective manner, and aid in alleviating mental and physical distress. Rather than changing the environment or source of stress, mindfulness meditation promotes changing the relationship with stress. In this way, there is a metacognitive shift from an outcome-oriented approach (actions to relieve stress) to a process-oriented approach (“I observe that I am stressed”).
In his seminal paper on the role of metacognition and mindfulness in mood disorders, Teasdale (1999) presents the conceptual basis for the role of metacognitive insight and mindfulness meditation in the prevention of depressive relapse. Shapiro and colleagues (2006) followed with the IAA model of mindfulness in which intention, attention, and attitude (IAA) are seen as an interwoven processes that can lead to “re-perceiving” experiences. Segal and colleagues (2002) introduced the concept of decentering as the ability to “step outside of one’s immediate experience, thereby changing the very nature of that experience” and is seen as a similar process to re-perceiving in Shapiro’s model (2006). These metacognitive models promote a shift in mental processes (second order) rather than a direct change of the mental contents or behaviors (first order). This shift in perspective (stance) enhances self-regulation and promotes an adaptive response (action), rather than maladaptive stress reactivity (reaction). Recently, Garland and colleagues (Garland, Gaylord, & Park, 2009) have provided a metacognitive framework for understanding how mindfulness can facilitate the reappraisal of stressful events and distressing thoughts. Using a stress and coping model, the authors propose that a mode of mindfulness allows one to “decenter” from the primary, or initial, stress appraisal and that this facilitates reappraisal with a different perspective that can promote more positive attributes. This new mindful reappraisal is hypothesized to attenuate the stress reaction (e.g., activation of the HPA axis) and to cultivate positive emotions rather than to suppress negative emotions. Therefore, mindfulness might potentiate the capacity for positive reappraisal as an active coping strategy.
Metacognitive Therapies for Insomnia
As part of the third wave of behavior therapy, mindfulness and acceptance-based approaches for the treatment of insomnia (i.e., MCTIs) are also emerging, with a growth of studies in the literature over the past decade. Early empirical studies using metacognitive therapies examined the impact of mindfulness meditation on sleep disturbance associated with other conditions. One study examined the impact of MBSR on sleep among women with breast cancer and found no differences between the MBSR and the control group on sleep quality and sleep efficiency, but did report a positive relationship between the practice of mindfulness techniques and feeling refreshed after sleep for the MBSR group (Shapiro, Bootzin, Figueredo, Lopez, & Schwartz, 2003). In a series of studies, Carlson and colleagues found evidence that MBSR leads to improvements in sleep quality among those with breast and prostate cancer (Carlson, Speca, Patel, & Goodey, 2004) as well as a heterogeneous group of cancer patients (Carlson & Garland, 2005). Another study added a mindfulness component to CBT for insomnia in adolescents with a substance abuse history and sleep complaints and revealed evidence for improvements in sleep and reductions in relapse of substance use for completers (Bootzin & Stevens, 2005). A more recent study reported improvement on the PSQI following MBCT for individuals suffering from poor sleep related to an anxiety disorder (Yook et al., 2008).
Another group of studies have examined the efficacy of MCTIs to specifically treat insomnia. Uncontrolled pilot studies on primary insomnia using MBSR (Britton, Shapiro, Penn, & Bootzin, 2003) and MBCT (Heidenreich, Tuin, Pflug, Michal, & Michalak, 2006) demonstrated improvements in self-reported wake after sleep onset and total sleep time along with reductions in cognitions related to rumination and worry. A pilot study combining mindfulness meditation with behavior therapy for insomnia (Ong, Shapiro, & Manber, 2008) found that half of the sample experienced a 50% or greater reduction in self-reported total wake time, and all but two participants no longer had clinically significant insomnia (based on Insomnia Severity Index scores) at the end of treatment. Consistent with the hypothesis that mindfulness reduces arousal, there was a significant correlation between the total number of meditation sessions during treatment and reduction on the Hyperarousal Scale. Follow-up data revealed that 61% of participants had no relapse of insomnia during the 12 months following treatment, supporting the long-term benefits of this treatment (Ong, Shapiro, & Manber, 2009). A similar approach has also been taken combining ACT with CBTI (Dalrymple, Fiorentino, Politi, & Posner, 2010). This case study reported on the successful treatment of an individual with insomnia using behavioral strategies with acceptance-based strategies. While promising, these small studies did not use control groups and did not include objective measures of sleep.
To date, two controlled trials have been conducted using mindfulness meditation with objective measures of sleep. One study compared MBSR with eszopiclone for individuals with chronic primary insomnia (Gross et al., 2011). There were significant improvements from baseline to post-treatment in both groups on a number of sleep parameters. Within the MBSR group, significant improvements were found on actigraphy-measured sleep onset latency and diary-measured sleep onset latency, total sleep time, and sleep efficiency. Although there were no significant between group differences the study was not sufficiently powered to provide definitive evidence of equivalent efficacy. Unfortunately, the authors did not examine potential mediators or mechanisms of treatment effects. Britton and colleagues compared MBCT with a wait-list control for individuals with depression and insomnia (Britton, Haynes, Fridel, & Bootzin, 2010). Participants in both groups reported reductions in sleep onset latency on diaries, and more time spent in meditation practice was associated with less self-reported time awake after sleep onset. However, data from polysomnography found that at the end of treatment, participants in the MBCT group had significantly more awakenings and Stage 1 sleep and decreased Slow-Wave Sleep (Stages 3 and 4) relative to controls. The authors interpreted these findings as indications that participants in the MBCT condition had greater cortical arousal than controls. Furthermore, the amount of time spent in mindfulness meditation practice was positively correlated with cortical arousals. This counter-intuitive finding indicates that the observed improvement in subjective sleep does not translate to reductions in cortical arousal and highlights the need to re-examine the mechanism by which mindfulness-based treatments improve subjective sleep. The collective literature provides a glimpse of efficacy for MCTIs across a number of sleep measures, but it would appear that a conceptual model is needed to guide testing of treatment mechanisms.
A Metacognitive Model for Insomnia
The proposed metacognitive treatment model builds upon the conceptualization of sleep-related cognitive arousal that was presented earlier (see Figure 3). It also fits with existing models of insomnia that conceptualize hyperarousal and failure to deactivate as central to the development and maintenance of insomnia. In the proposed model both primary and secondary arousal are seen as key factors in the development and maintenance of an insomnia disorder. The distinction between primary and secondary arousal discussed earlier parallels the distinction between first and second order metacognitive processes. Using these concepts, we propose a unifying framework in which the metacognitive processes of observing and noticing thoughts are an important therapeutic element and that treatments aimed at shifting these metacognitive processes would be expected to reduce secondary arousal.
The model posits that through the specific use of mindfulness and acceptance-based principles, MCTIs directly aim to reduce secondary arousal with downstream effects on reducing primary arousal, leading to the clinical outcome of remission from insomnia. As a group, MCTIs share the common aim of increasing awareness of the mental and physical states that arise when experiencing insomnia symptoms and learning how to shift mental processes to promote an adaptive stance in responding to these symptoms. This stance is characterized by balanced appraisals of sleep expectations and the causes of daytime dysfunction, increased cognitive flexibility in approaching nocturnal and daytime symptoms of insomnia, non-attachment to sleep-related outcomes, and committing to values that are important to the individual. A shift in these metacognitive processes is posited to reduce secondary arousal and prevent the perpetuation of negative emotions and behaviors that fuel the cycle of chronic insomnia. The metacognitive process is illustrated in Table 1 and each of the three central metacognitive processes (awareness, shifting, and stance) are discussed below with examples of clinical applications from MCTIs.
Table 1.
Metacognitive Treatment Model for Insomnia
| Elements of secondary arousal | Shift to adaptive stance | Reduction in secondary arousal |
|---|---|---|
| Attention and emotional bias towards sleep-seeking or sleep-aversive thoughts and behaviors | Balance | Allow the state of sleepiness to guide sleep-related behavior |
| Rigidity in sleep-related behaviors and beliefs | Flexibility | Adjusting intentionally to changing conditions |
| Attachment to sleep-related needs and expectations | Equanimity | Calmness stemming from non- striving and patience about sleep |
| Absorption in solving the sleep problem | Commitment to Values | Pursuit of valued living in the context of the range of thoughts and emotions |
Metacognitive Awareness
Increasing metacognitive awareness involves the cultivation of non-judging, present-focused awareness. Many individuals with chronic insomnia are stuck in a cycle of insomnia because they have difficulty viewing the problem from an objective perspective. They are typically not aware of their own maladaptive cognitive, emotional, and behavioral reactions to sleep disturbance; when they are aware, they often fail to adopt an objective stance. Many people with insomnia also show poor awareness of time. Several studies have found that people with insomnia tend to be poor estimators of total sleep time (Manconi et al., 2010; Tang & Harvey, 2005) and this deficit does not appear to be the result of a diminished ability to estimate time (Fichten, Creti, Amsel, Bailes, & Libman, 2005; Tang & Harvey, 2005). At the extreme are people with paradoxical insomnia, an insomnia sub-type characterized by a marked discrepancy between the subjective perception of sleep and objective measurement of sleep. In clinical evaluations, people with paradoxical insomnia report sleeping only one or two hours but objective measurement through polysomnography reveals that the actual total sleep time is within the normal range. People with insomnia also tend to focus on the potential short or long-term negative consequences of poor sleep and their responses are directed at avoiding such consequences. Many no longer use internal cues of sleepiness as a guide for going to bed and instead use external cues (e.g., “I should go to bed before midnight”) or avoidance of a negative emotional state (e.g., “I had a bad day and just want to go to bed”) to decide when to go to bed, even if it is incongruent with their current physiological state. These behaviors are outcome driven (i.e., “all I want is to get a good night’s sleep”) with past or future-oriented thinking. The increase in effort for sleep, reactivity to sleep disturbance, and attachment to satisfying immediate sleep needs are manifestations of secondary arousal (see Figure 3). Moreover, there is a shift towards “mindlessness”-a state of being too tired to be fully awake, yet too aroused to fall asleep.
In MCTIs, awareness is developed through the practice of meditation or engagement in an activity that focuses attention to the present moment without judgment. In MBSR and MBCT, guided meditations are conducted in every session. The cultivation of mindfulness allows one to see the problem of insomnia with a clear lens that is not clouded by the desire for and effort to sleep. By attending to the present moment, one is taking an objective perspective and is able to separate the experience of not sleeping (primary arousal) from the emotional attachment to seeking sleep (secondary arousal). For example, one might observe without judgment and without a need to change the situation, the experiences of annoyance when waking prior to the alarm clock or negative affect related to low energy during the day. Such mindful observation could lead to the insight that much of the suffering is due to being absorbed in the frustration (secondary arousal), rather than not sleeping itself (primary arousal). Through objective, non-attached observations one might also become aware of internal sensations when considering a daytime nap and notice a state of hyperarousal but not sleepiness or fatigue. Awareness of this distinct state can guide appropriate behavioral action: if sleepy then go to sleep, if fatigued then rest, and if in a state of high arousal focus on reducing arousal. These are examples of how metacognitive awareness provides a means to “awaken” the individual to their sleep related experiences and facilitate insight to the problem. This, in turn, can halt the perpetuation of the problem, which occurs with mindless automatic reactions. Indeed, a recent study revealed that scores on the Kentucky Inventory of Mindfulness Skills were negatively correlated with ratings of daytime sleepiness, such that greater mindfulness skills were associated with less sleepiness (Ong et al., 2009).
Metacognitive Shifting
Metcognitive shifting involves changing the “relationship with” as opposed to the “content of” cognitions. Instead of changing a thought or behavior, greater awareness promotes a metacognitive shift towards a more objective, non-judging stance. This is similar to previously describe concepts of re-perceiving (Shapiro et al., 2006) and de-centering (Segal et al., 2002). The shift that follows the insight gained from metacognitive awareness allows one to have greater equanimity about the problem rather than trying to immediately change what is undesirable. Equanimity provides a platform to stand and observe mental events as they are without trying to fix them. In the case of insomnia, metacognitive shifting involves a shift in one’s relationship with his/her sleep-related thoughts (i.e., the assigned degree of importance, meaning, and/or value of sleep). This represents de-arousal at the secondary level. MCTIs include tools to facilitate metacognitive shifts. For example, meditation is an MCTI tool to promote the practice of observing and acknowledging sleep-interfering thoughts, rather than engaging in these thoughts. Short exercises (e.g., nine-dot exercise, Chinese fingertrap) can be used as metaphors to teach the importance of shifting perspectives and letting go of effort to sleep.
New Metacognitive Stance
The process of metacognitive awareness and shifting leads to adoption of a new stance. This is not a linear process, but rather it is an iterative process involving frequent iterations of movement form awareness to shifting to adopting new stances. By embodying the principles of mindfulness and acceptance, each new stance is characterized by balance, flexibility, equanimity, and a commitment to values. An adaptive stance is posited to reduce arousal and prevent the perpetuation of insomnia. In contrast, an avoidant stance, such as the one described in Harvey’s Cognitive Model of Insomnia (Harvey, 2002) often consists of safety behaviors and rigidity. Instead of trying to gain control of sleep by examining the accuracy of and modifying cognitions, adopting a new metacognitive stance involves working out of the territory of an insomnia disorder (i.e., both nighttime and daytime symptoms) by shifting to a new stance through mindfulness and acceptance. The key elements of an adaptive stance are described below and summarized in Table 1.
Balance
Having balance is a key component of adopting a new stance. The framework of mindfulness meditation is founded on the Buddhist view that all mental content, including thoughts and emotions, fall into one of three categories: aversion, attraction, or indifference. Thoughts and emotions that are polarizing can lead to suffering by pulling one towards attraction or aversion. As applied to insomnia, a balanced stance involves managing the attraction and aversion to sleep. In assessing patients with insomnia, many will report a tendency to seek sleep, meaning there is an imbalance in thoughts and behaviors related to sleep, such as striving to go to sleep or “clinging” to the bed in hopes of getting more sleep. People with insomnia have been found to exhibit increased physiological reactions to positive sleep-related stimuli that are consistent with the concept of craving sleep (Baglioni et al., 2010). On the other hand, some individuals with insomnia, such as those with Post-Traumatic Stress Disorder (PTSD) have an aversive relationship with sleep. For these individuals, the state of letting go and falling asleep competes with the perceived need to maintain awareness and vigilance of their surroundings at all times. In a study of Veterans of the Iraq and Afghanistan Wars presenting to a primary care clinic within one year of returning from deployment, fear of lost vigilance was found to be an independent predictor of sleep quality (Pietrzak, Morgan, and Southwick, 2010). At each extreme, there is an imbalance in the relationship with sleep, which tends to perpetuate insomnia. There is also evidence supporting an attentional bias towards sleep-related cues among people with insomnia (Jones, Macphee, Broomfield, Jones, & Espie, 2005; Marchetti, Biello, Broomfield, Macmahon, & Espie, 2006). For example, monitoring the clock while in bed, is common among individuals with insomnia, which may serve to heighten sleep-related worry (Tang, Anne Schmidt, & Harvey, 2007). In this context, adopting a balanced stance might involve broadening the attention so that the focus is not exclusively on sleep-related cues, thus preventing biased perceptions about sleep. A balanced stance could also be taken to the time getting into and out of bed. Recent findings have revealed that people with insomnia report highly variable time in bed (Buysse et al., 2010; Sanchez-Ortuno, Carney, Edinger, Wyatt, & Harris, 2011; Suh et al., 2012). This can serve as a maladaptive response to poor sleep and can increase sleep-related arousal. Rather overcompensating for sleep deprivation, one can focus on the internal cues related to sleepiness as a guide of when to go to bed and when to wake up. This can enhance self-efficacy by aligning sleep-related behaviors with internal cues of sleepiness.
Flexibility
Flexibility in stance is also an important component, consisting of openness, a willingness to adopt a beginner’s mind, and acceptance of a wide range of cognitive and emotional phenomena. In a recent study, the roles of acceptance and experiential avoidance were evaluated in relation to insomnia complaints among chronic pain patients (McCracken, Williams & Tang, 2011). Measures of acceptance, mindfulness, and experiential avoidance were evaluated collectively as a proxy for psychological flexibility. Findings showed that psychological inflexibility was a significant predictor of insomnia severity, problems with sleep and rest, low sleep efficiency, and fatigue. Another study found that increased frequency of avoidance behaviors is directly linked to objective measures of sleep disturbances (Hall et al, 2007). People with insomnia also tend to be very rigid in their thinking and behaviors. In assessing sleep-related cognitions, people with insomnia tend to hold onto fairly rigid beliefs about sleep (Morin et al., 1993). Attempts to control or suppress unwanted thoughts have been found to prolong sleep onset latency (Harvey, 2003). Safety behaviors (Harvey (2002) are specific routines or rituals that must be done in order to fall asleep or to limit the consequences of poor sleep. Examples of these safety behaviors include avoidance of social functions and, increasing time in bed in an effort to avoid the fear of not sleeping or the consequences of not sleeping. Safety behaviors reflect unwillingness to accept sleeplessness and its consequences. Ironically, attempts to control sleep have the paradoxical effect of perpetuating sleeplessness, particularly when the sleeplessness persists beyond the acute stress stage. This is consistent with the ironic processes theory of mental control (Wegner, 1994) and it has been demonstrated in normal sleepers under high mental load, that trying to fall asleep quickly is associated with longer sleep onset latency (Ansfield, Wegner & Bowser, 1996). Thus, adopting an inflexible orientation towards sleep in which only a single outcome is acceptable can exacerbate poor sleep.
Flexibility increases one’s ability to let go of the change agenda and decreases the secondary arousal stemming from lost sleep. By maintaining flexibility in thoughts and behaviors related to sleep, one is adopting an open and accepting stance. Acceptance techniques are intended to facilitate awareness of an unworkable change agenda that the individual uses in order to eliminate sleeplessness and the thoughts, emotions, and sensations that accompany this undesirable state. In MBSR, poems such as The Guest House by Rumi (Barks, 2004) are discussed to help illustrate the concept of acceptance and flexibility. This poem describes how different emotions (e.g., joy, depression) might be considered guests and that these guests should all be welcomed and entertained. Discussion of this poem can illustrate the importance of accepting both positive and negative emotions.
Another way to promote flexibility is through the beginner’s mind approach. Approaching both the nighttime and daytime with a beginner’s mind involves letting go of the contingencies based upon expectations about the previous night’s sleep or worries about the following day and allowing the present day or night to unfold. For example, remaining in bed after waking in the morning is a common strategy employed by those with insomnia; yet this strategy usually does not result in getting more sleep. Persistent use of this ineffective strategy reflects a strong allegiance to the change agenda, when in fact the change agenda is the problem. In other words, the unwillingness to accept sleeplessness results in the very suffering that they are attempting to alleviate by causing secondary arousal. Using beginner’s mind, an insomnia patient would be asked to approach each day and night with openness to the range of experiences without pre-determined outcomes or contingencies based on past experiences or future expectations. This approach can be used when reviewing sleep diaries. If the patient presents diaries that have virtually identical patterns across days or states, “every day is the same”, he or she would be asked to provide more details about each day or to describe the events of a particular night to illuminate the concept that every day is unique.
Equanimity
Equanimity refers to a stance without attachment or aversion to sleep-related stimuli. For example, one’s reactions to the thoughts “I am having trouble sleeping” and “I am sleeping well” would be much less disparate from a stance of equanimity. This stance would outwardly evince relative calmness and composure in response to sleep-related cues. As noted earlier, models of insomnia have hypothesized that both elevated arousal (Morin, 1993) and failure to de-arouse (Espie, 2002) are involved in the pathophysiology of insomnia. During clinical evaluations, patients with insomnia often report strong emotional reactions to various sleep-related stimuli. In addition to attention bias discussed earlier, people with insomnia also demonstrate an emotional bias in the appraisal and perception of sleep-related stimuli. For example, studies have found that individuals with insomnia not only demonstrate more cognitive activity at night, but that emotional tone, or valence, of the thoughts are more negative when compared to good sleepers (Kuisk, Bertelson, & Walsh, 1989). Another study that used a two-dimensional approach to assessing affect revealed that compared to good sleepers, poor sleepers report more negative emotional valence during the daytime and nighttime while reporting more arousal at nighttime but not during the daytime (Ong, Carde, Gross, & Manber, 2011). Using a similar affective rating system, people with insomnia were found to rate sleep-related negative stimuli (e.g., picture of person laying in bed awake) and non-sleep related negative stimuli as equally unpleasant while good sleepers rated only non-sleep related negative stimuli as unpleasant (Baglioni et al., 2010). This suggests that the negative bias in rating sleep-related stimuli is specific to people with insomnia. When compared to good sleepers, people with insomnia are also more likely to appraise stressful events as negative despite no differences in the frequency of stressful events (Morin, Rodrigue, & Ivers, 2003; Friedman, Brooks, Yesavage, Bliwise, & Wicks, 1995).
A stance with equanimity in metacognitions can help to reduce the bias in attention and emotion that develops during the course of insomnia. With equanimity, one is adopting a stance of non-attachment to sleep outcomes, which facilitates improved emotion regulation in the face of insufficient sleep and fatigue. This stance refers to actively letting go of the desire to get sleep or the expectation of meeting certain sleep needs. It also refers to letting go of the strong belief in contingencies between sleep and daytime functioning, such as the need to get eight hours of sleep in order to function well during the daytime. People with insomnia are often driven towards sleep-seeking behaviors because of messages from the media emphasizing the consequences of sleep debt. This belief can increase sleep effort or increase time spent in bed when sleep goals are not achieved. Rather than facilitating sleep, this set of cognitions and behaviors is counterproductive and serves to increase primary and secondary arousal.
The shift towards equanimity is a shift from outcome-oriented thinking to process-oriented thinking, and is similar to the shift in paradoxical intention described earlier (Ascher & Efran, 1978). However, paradoxical intention involves a shift from one outcome (trying to sleep) to another outcome (trying to stay awake). With equanimity and detachment, the shift is from the outcome (sleep) to the process (present moment). It is important to note that this shift is an active strategy and does not involve suppression of thoughts. It is not a passive strategy nor a defense mechanism. Non-attachment from this perspective does not imply a lack of feelings or emotions, but rather it suggests creating a space between a stimulus and the reaction to the stimulus. For example, letting go of the need to sleep eight hours per night does not mean that one should no longer have thoughts about sleep needs. Rather, these thoughts shift towards how one feels at the present moment, and the recognition that thoughts about sleep are just that; thoughts about sleep, and nothing more, allowing the secondary arousal to dissipate. During meditation practices, patients are taught to practice equanimity when the sensation of sleepiness arises. Rather than rushing to bed at night or resisting the urge to sleep during the day, a stance with equanimity can cultivate calmness in response to sleepiness, thus reducing secondary arousal and rediscovering the process of falling asleep.
Commitment to values
Individuals experiencing chronic insomnia may lose sight of some of their life values as their focus becomes more directed towards control of sleeplessness. Whereas the impetus for seeking treatment is commitment to the value of well-being, insomnia patients often acknowledge making concessions to other values in the service of symptom management as their anxiety about sleep increases over time. For example, an individual who values health may forgo the morning exercise regimen to compensate for lost sleep on the previous day by “sleeping in.” In this case, an important value (heart health) is sacrificed at the expense of a short-term gain (better work performance today). Similarly, when patients do not complete sleep logs or do not adhere to treatment recommendations, they ignore the connection between adherent behaviors and their stated values.
From this perspective, a commitment to personal values can provide the direction in which one is purposefully headed. Values are not attainable targets, but value-consistent goals can be attained. When asked to state their values, patients will often respond with a goal rather than a value. Increased awareness of non-sleep values can enhance willingness to enact behavioral recommendations for improving sleep, such as getting out of bed at the same time every day and letting go of ineffective and maladaptive strategies for dealing with insomnia (e.g., variable rise time depending on perception of sleep quality and quantity). Awareness of values can be a reference for developing values-consistent goals, and for determining if individual actions are consistent with values. For example, individuals who are suffering from insomnia are more likely than good sleepers to cancel social obligations following a night of poor sleep (Carney & Edinger, 2006). In many cases, the decision to cancel obligations is based on strongly-held beliefs about the negative consequences of poor or insufficient sleep. The individual experiencing insomnia pays greater attention to the mind’s prediction about performance following a poor night of sleep than to the value of the obligation.
In using a value-based approach, MCTIs encourage people to commit to actions in the service of their stated values, such as engaging in an activity rather than canceling it, even in the context of thoughts and feelings that promote avoidance. ACT includes tools for identifying values, such as the Life Compass (Dahl & Lundgren, 2006) which requires one to rate the importance of various life domains (e.g., family, friendships, work, spirituality, etc.). Once values are identified, therapists can help a patient realize the cost of a behavior (e.g., canceling a social engagement because of poor sleep the previous night) in terms of a linked value (e,g, staying connected with people). In that way changing a behavior is promoted by commitment to values. Barriers to enacting values-based behavior change are addressed through other components of the model, such as flexibility and equanimity. Rather than being absorbed by the distress of the immediate experience, one can de-center or re-perceive to connect with the stated values. In this way, people can see the “big picture” (living a valued life) despite the perception of “losing battles” (i.e., getting less than ideal sleep) on any particular night.
Clinical and Research Implications of the Metacognitive Model
As a deeper understanding of the cognitive processes involved in insomnia is being gained, the treatments aimed at addressing these processes can improve. Thus, an important research agenda is to move towards identifying the treatment mechanisms involved in mindfulness and acceptance-based therapies for insomnia and to develop a testable model that can elucidate the specific treatment effects. Given the early stage of research in this area, much work is needed to further the understanding and impact of MCTIs. Measuring secondary arousal can be a methodological challenge and might require creative assessment techniques. To meet this challenge, new measures may need to be developed. For example, a measure that can capture shifts from a narrow focus on sleep-related issues to a more broad focus on values and life issues would be important when assessing changes in metacognition. Based upon a different theoretical background, Adrian Wells has described a similar distinction between cognitions and metacognitions in developing a novel set of metacognitive therapies for anxiety disorders (e.g., Wells, 1999; Wells & Mathews, 1994; Wells & Sembi, 2004; Wells et al, 2010). Using this metacognitive model, one paper has reported on a metacognitive questionnaire for insomnia (MCQ-I) (Waine, Broomfield, Banham, & Espie, 2009). While this measure has yet to be used in studies on MCTI, it serves as an example that might lead to future directions. Longitudinal designs with frequent measurement of sleep-related arousal could provide a way to study the relative order of change in these measures relative to insomnia symptoms during MCTI. One might expect to see change in secondary arousal (e.g., change in the perception that poor sleep quality impairs function during the day) before or even in absence of a significant improvement in sleep. These investigations could also provide insight into the relative importance of primary arousal compared to secondary arousal.
Further work also remains to examine issues related to the delivery of MCTIs and to compare and contrast these approaches with other cognitive and behavioral approaches. It has been suggested elsewhere that mindfulness and acceptance-based approaches are compatible with CBT and should be considered under the family of CBT rather than a new wave of treatments (Hofmann, Sawyer, & Fang, 2010). We argue that MCTIs have elements that are distinct from CBTI and the focus on secondary arousal rather than primary arousal is unique. However, there is overlap between these two approaches and studies comparing the differences between MCTI and CBTI can aid in further specifying the common and unique elements. It is unclear if MCTIs should be delivered independent of other techniques or if they can be combined or integrated with existing approaches. Future studies could also examine the timing (morning versus evening) and dosing (e.g., 10, 30, or 45 minutes) of formal meditations that would be needed to have an impact on secondary arousal. Also, the possibility that the practice of mindfulness meditation or acceptance techniques might result in side effects or adverse events has not been carefully examined. Once a better understanding of MCTIs is available, movement can be made towards training and dissemination of specific techniques either alone or in treatment packages.
Another direction for investigation is to examine the connection between the proposed model and physiological mechanisms. For example, a brain imaging study by Holzel and colleagues (2010) found that participation in a mindfulness-based stress reduction program was associated with increased gray matter concentration in the hippocampus, posterior cingulate cortex, cererbellum, and the tempro-parietal junction when compared to a wait-list control group. These findings are consistent with involvement of brain functions involved in emotion regulation and perspective taking that could be considered metacognitive processes. Meanwhile, Nofzinger and colleagues (2004) found that patients with insomnia as compared to healthy subjects showed a smaller decline in relative metabolism in wake-promoting regions of the brain when comparing waking to sleep states and reduced relative metabolism in the prefrontal cortex while awake. In both studies, brain regions related to arousal, emotion-regulation, and cognitive systems were found to be involved. Further research should consider these brain regions as a potential link for understanding the biological correlates of metacognitive processes involved in insomnia.
Conclusions
The concept of metacognition has a long tradition, but the application of metacognitive techniques to disorder-specific interventions, including insomnia, is an emerging trend in behavior therapy. The application of metacognition to insomnia is compatible with the rich and growing literature on cognitive processes in the development and maintenance of insomnia. We propose a model that extends and refines the existing literature on cognitive hyperarousal to include secondary arousal. Our model describes specific metacognitive process and provides a theoretical framework for future empirical work on metacognitive therapies for insomnia.
Highlights.
A two-level model of cognitive (primary) and metacognitive (secondary) arousal is presented in the context of insomnia.
A conceptual framework is presented detailing the mechanisms of metacognition in the context of insomnia treatments.
Mechanisms include awareness of mental and physical states, shifting mental processes, and promoting an adaptive stance.
A stance with balanced appraisals, cognitive flexibility, equanimity, and commitment to values reduces secondary arousal.
Acknowledgments
Preparation of this manuscript was supported in part by a grant from the National Institutes of Health awarded to the first author (K23AT003678) and a Department of Veterans Affairs HSR&D Career Development Award (CDA 09-218) awarded to the second author. The authors would like to thank Michael Lederman and Christina Khou for assistance with preparation of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jason C. Ong, Department of Behavioral Sciences, Rush University Medical Center
Christi S. Ulmer, Durham VA Medical Center, Duke University Medical Center
Rachel Manber, Stanford University School of Medicine.
References
- Ansfield ME, Wegner DM, Bowser R. Ironic effects of sleep urgency. Behaviour Research and Therapy. 1996;34(7):523–531. doi: 10.1016/0005-7967(96)00031-9. [DOI] [PubMed] [Google Scholar]
- Ascher LM, Efran JS. Use of paradoxical intention in a behavioral program for sleep onset insomnia. J Consult Clin Psychol. 1978;46(3):547–550. doi: 10.1037//0022-006x.46.3.547. [DOI] [PubMed] [Google Scholar]
- Ascher LM, Turner R. Paradoxical intention and insomnia: an experimental investigation. Behav Res Ther. 1979;17(4):408–411. doi: 10.1016/0005-7967(79)90015-9. [DOI] [PubMed] [Google Scholar]
- Baglioni C, Lombardo C, Bux E, Hansen S, Salveta C, Biello S, Espie CA. Psychophysiological reactivity to sleep-related emotional stimuli in primary insomnia. Behaviour Research and Therapy. 2010;48(6):467–475. doi: 10.1016/j.brat.2010.01.008. [DOI] [PubMed] [Google Scholar]
- Barks C. The Essential Rumi. New York: HarperCollins; 2004. The Guest House; p. 109. [Google Scholar]
- Bonnet MH, Arand DL. Hyperarousal and insomnia. Sleep Medicine Reviews. 1997;1(2):97–108. doi: 10.1016/s1087-0792(97)90012-5. [DOI] [PubMed] [Google Scholar]
- Bootzin RR. Stimulus control treatment for insomnia. Paper presented at the 80th Annual Convention of the American Psychological Association.1972. [Google Scholar]
- Bootzin RR, Stevens SJ. Adolescents, substance abuse, and the treatment of insomnia and daytime sleepiness. Clin Psychol Rev. 2005;25(5):629–644. doi: 10.1016/j.cpr.2005.04.007. [DOI] [PubMed] [Google Scholar]
- Britton WB, Haynes PL, Fridel KW, Bootzin RR. Polysomnographic and subjective profiles of sleep continuity before and after mindfulness-based cognitive therapy in partially remitted depression. Psychosom Med. 2010;72(6):539–548. doi: 10.1097/PSY.0b013e3181dc1bad. [DOI] [PubMed] [Google Scholar]
- Britton WB, Shapiro SL, Penn PE, Bootzin RR. Treating insomnia with mindfulness-based stress reduction. Sleep. 2003;26:A309. [Google Scholar]
- Buysse DJ, Cheng Y, Germain A, Moul DE, Franzen PL, Fletcher M. Night-to-night sleep variability in older adults with and without chronic insomnia. Sleep Med. 2010;11(1):56–64. doi: 10.1016/j.sleep.2009.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson LE, Garland SN. Impact of mindfulness-based stress reduction (MBSR) on sleep, mood, stress and fatigue symptoms in cancer outpatients. Int J Behav Med. 2005;12(4):278–285. doi: 10.1207/s15327558ijbm1204_9. [DOI] [PubMed] [Google Scholar]
- Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004;29(4):448–474. doi: 10.1016/s0306-4530(03)00054-4. [DOI] [PubMed] [Google Scholar]
- Carney CE, Edinger JD. Identifying critical beliefs about sleep in primary insomnia. Sleep. 2006;29(3):342–350. doi: 10.1093/sleep/29.3.342. [DOI] [PubMed] [Google Scholar]
- Dahl J, Lundgren T. In: Acceptance and Commitment Therapy (ACT) in the Treatment of Chronic Pain. Baer Ruth., editor. Elsevier; Burlington, MA: 2006. pp. 285–306. [Google Scholar]
- Dalrymple KL, Fiorentino L, Politi MC, Posner D. Incorporating principles from acceptance and commitment therapy into cognitive-behavioral therapy for insomnia: A case example. Journal of Contemporary Psychotherapy. 2010;40(4):209–217. [Google Scholar]
- Espie CA. Insomnia: conceptual issues in the development, persistence, and treatment of sleep disorder in adults. Annu Rev Psychol. 2002;53:215–243. doi: 10.1146/annurev.psych.53.100901.135243. [DOI] [PubMed] [Google Scholar]
- Flavell JH. Metacognitive aspects of problem solving. In: Resnick LB, editor. The nature of intelligence. Hillsdale, NJ: Erlbaum; 1976. pp. 231–236. [Google Scholar]
- Fichten CS, Creti L, Amsel R, Bailes S, Libman E. Time estimation in good and poor sleepers. J Behav Med. 2005;28(6):537–553. doi: 10.1007/s10865-005-9021-8. [DOI] [PubMed] [Google Scholar]
- Friedman L, Brooks JO, Yesavage JA, Bliwise DL, Wicks DS. Perceptions of life stress and chronic insomnia in older adults. Psychology and Aging. 1995;10:352–357. doi: 10.1037//0882-7974.10.3.352. [DOI] [PubMed] [Google Scholar]
- Garland E, Gaylord S, Park J. The role of mindfulness in positive reappraisal. Explore (NY) 2009;5(1):37–44. doi: 10.1016/j.explore.2008.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross CR, Kreitzer MJ, Reilly-Spong M, Wall M, Winbush NY, Patterson R. Mindfulness-based stress reduction versus pharmacotherapy for chronic primary insomnia: a randomized controlled clinical trial. Explore (NY) 2011;7(2):76–87. doi: 10.1016/j.explore.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall M, Thayer JF, Germain A, Moul D, Vasko R, Puhl M, Buysse DJ. Psychological stress is associated with heightened physiological arousal during NREM sleep in primary insomnia. Behavioral Sleep Medicine. 2007;5(3):178–193. doi: 10.1080/15402000701263221. [DOI] [PubMed] [Google Scholar]
- Harvey AG. A cognitive model of insomnia. Behav Res Ther. 2002;40(8):869–893. doi: 10.1016/s0005-7967(01)00061-4. [DOI] [PubMed] [Google Scholar]
- Harvey AG. The attempted suppression of presleep cognitive activity in insomnia. Cognitive Therapy and Research. 2003;27(6):593–602. [Google Scholar]
- Harvey AG, Sharpley AL, Ree MJ, Stinson K, Clark DM. An open trial of cognitive therapy for chronic insomnia. Behav Res Ther. 2007;45(10):2491–2501. doi: 10.1016/j.brat.2007.04.007. [DOI] [PubMed] [Google Scholar]
- Hauri P. Treating psychophysiologic insomnia with biofeedback. Arch Gen Psychiatry. 1981;38(7):752–758. doi: 10.1001/archpsyc.1981.01780320032002. [DOI] [PubMed] [Google Scholar]
- Hayes SC. Acceptance and commitment therapy and the new behaviour therapies: Mindfulness, acceptance, and relationship. In: Hayes SC, Follette VM, Linehan MM, editors. Mindfulness and Acceptance: Expanding the cognitive-behavioral tradition. New York: The Guilford Press; 2004. pp. 1–29. [Google Scholar]
- Heidenreich T, Tuin I, Pflug B, Michal M, Michalak J. Mindfulness-based cognitive therapy for persistent insomnia: a pilot study. Psychother Psychosom. 2006;75(3):188–189. doi: 10.1159/000091778. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Fang A. The empirical status of the “New wave” of cognitive behavioral therapy. Psychiatric Clinics of North America. 2010;33(3):701–710. doi: 10.1016/j.psc.2010.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holzel BK, Carmody J, Vangel M, Congleton C, Yerramsetti SM, Gard T. Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Res. 2010;191(1):36–43. doi: 10.1016/j.pscychresns.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson E. You Can Sleep Well. New York, NY: McGraw-Hill Book Company, Inc; 1938. [Google Scholar]
- Jones BT, Macphee LM, Broomfield NM, Jones BC, Espie CA. Sleep-related attentional bias in good, moderate, and poor (primary insomnia) sleepers. J Abnorm Psychol. 2005;114(2):249–258. doi: 10.1037/0021-843X.114.2.249. [DOI] [PubMed] [Google Scholar]
- Kuisk LA, Bertelson AD, Walsh JK. Presleep cognitive hyperarousal and affect as factors in objective and subjective insomnia. Percept Mot Skills. 1989;69(3 Pt 2):1219–1225. doi: 10.1177/00315125890693-228. [DOI] [PubMed] [Google Scholar]
- Lundh LG. The role of acceptance and mindfulness in the treatment of insomnia. Journal of Cognitive Psychotherapy. 2005;19:29–39. [Google Scholar]
- Lundh LG, Broman JE. Insomnia as an interaction between sleep-interfering and sleep-interpreting processes. Journal of Psychosomatic Research. 2000;49(5):299–310. doi: 10.1016/s0022-3999(00)00150-1. [DOI] [PubMed] [Google Scholar]
- Manconi M, Ferri R, Sagrada C, Punjabi NM, Tettamanzi E, Zucconi M. Measuring the error in sleep estimation in normal subjects and in patients with insomnia. J Sleep Res. 2010;19(3):478–486. doi: 10.1111/j.1365-2869.2009.00801.x. [DOI] [PubMed] [Google Scholar]
- Marchetti LM, Biello SM, Broomfield NM, Macmahon KM, Espie CA. Who is pre-occupied with sleep? A comparison of attention bias in people with psychophysiological insomnia, delayed sleep phase syndrome and good sleepers using the induced change blindness paradigm. J Sleep Res. 2006;15(2):212–221. doi: 10.1111/j.1365-2869.2006.00510.x. [DOI] [PubMed] [Google Scholar]
- McCracken LM, Williams JL, Tang NK. Psychological flexibility may reduce insomnia in persons with chronic pain: A preliminary retrospective study. Pain Medicine. 2011;12(6):904–912. doi: 10.1111/j.1526-4637.2011.01115.x. [DOI] [PubMed] [Google Scholar]
- Morin CM. Insomnia: Psychological Assessment and Management. New York: The Guilford Press; 1993. [Google Scholar]
- Morin CM, Rodrigue S, Ivers H. Role of stress, arousal, and coping skills in primary insomnia. Psychosomatic Medicine. 2003;65(2):259–267. doi: 10.1097/01.psy.0000030391.09558.a3. [DOI] [PubMed] [Google Scholar]
- Morin CM, Stone J, Trinkle D, Mercer J, Remsberg S. Dysfunctional beliefs and attitudes about sleep among older adults with and without insomnia complaints. Psychol Aging. 1993;8(3):463–467. doi: 10.1037//0882-7974.8.3.463. [DOI] [PubMed] [Google Scholar]
- Nofzinger EA, Buysse DJ, Germain A, Price JC, Miewald JM, Kupfer DJ. Functional neuroimaging evidence for hyperarousal in insomnia. Am J Psychiatry. 2004;161(11):2126–2128. doi: 10.1176/appi.ajp.161.11.2126. [DOI] [PubMed] [Google Scholar]
- Ong JC, Carde NB, Gross JJ, Manber R. A two-dimensional approach to assessing affective states in good and poor sleepers. Journal of Sleep Research. 2011;20(4):606–610. doi: 10.1111/j.1365-2869.2011.00907.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong JC, Shapiro SL, Manber R. Combining mindfulness meditation with cognitive-behavior therapy for insomnia: a treatment-development study. Behav Ther. 2008;39(2):171–182. doi: 10.1016/j.beth.2007.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong JC, Shapiro SL, Manber R. Mindfulness meditation and cognitive behavioral therapy for insomnia: a naturalistic 12-month follow-up. Explore (NY) 2009;5(1):30–36. doi: 10.1016/j.explore.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, Morgan CA, Southwick SM. Sleep quality in treatment-seeking veterans of Operations Enduring Freedom and Iraqi Freedom: the role of cognitive coping strategies and unit cohesion. Journal of Psychosomatic Research. 2010;69(5):441–448. doi: 10.1016/j.jpsychores.2010.07.002. [DOI] [PubMed] [Google Scholar]
- Sanchez-Ortuno MM, Carney CE, Edinger JD, Wyatt JK, Harris A. Moving beyond average values: assessing the night-to-night instability of sleep and arousal in DSM-IV-TR insomnia subtypes. Sleep. 2011;34(4):531–539. doi: 10.1093/sleep/34.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York: The Guilford Press; 2002. [Google Scholar]
- Shapiro SL, Bootzin RR, Figueredo AJ, Lopez AM, Schwartz GE. The efficacy of mindfulness-based stress reduction in the treatment of sleep disturbance in women with breast cancer: An exploratory study. Journal of Psychosomatic Research. 2003;(54):85–91. doi: 10.1016/s0022-3999(02)00546-9. [DOI] [PubMed] [Google Scholar]
- Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of Mindfulness. Journal of Clinical Psychology. 2006;62(3):373–386. doi: 10.1002/jclp.20237. [DOI] [PubMed] [Google Scholar]
- Spielman AJ, Caruso LS, Glovinsky PB. A behavioral perspective on insomnia treatment. Psychiatr Clin North Am. 1987;10(4):541–553. [PubMed] [Google Scholar]
- Spielman AJ, Sasky P, Thorpy MJ. Treatment of chronic insomnia by restriction of time in bed. Sleep. 1987;10(1):45–56. [PubMed] [Google Scholar]
- Suh S, Nowakowski S, Bernert RA, Ong JC, Siebern AT, Dowdle CL. Clinical significance of night-to-night sleep variability in insomnia. Sleep Med. 2012;13(5):469–475. doi: 10.1016/j.sleep.2011.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang NK, Harvey AG. Time estimation ability and distorted perception of sleep in insomnia. Behav Sleep Med. 2005;3(3):134–150. doi: 10.1207/s15402010bsm0303_2. [DOI] [PubMed] [Google Scholar]
- Tang NKY, Anne Schmidt D, Harvey AG. Sleeping with the enemy: Clock monitoring in the maintenance of insomnia. Journal of Behavior Therapy and Experimental Psychiatry. 2007;38(1):40–55. doi: 10.1016/j.jbtep.2005.07.004. [DOI] [PubMed] [Google Scholar]
- Teasdale JD. Metacognition, Mindfulness and the Modification of Mood Disorders. Clinical Psychology and Psychotherapy. 1999;6(2):146–155. [Google Scholar]
- Turner RM, Ascher LM. Controlled comparison of progressive relaxation, stimulus control, and paradoxical intention therapies for insomnia. J Consult Clin Psychol. 1979;47(3):500–508. doi: 10.1037//0022-006x.47.3.500. [DOI] [PubMed] [Google Scholar]
- Waine J, Broomfield NM, Banham S, Espie CA. Metacognitive beliefs in primary insomnia: Developing and validating the metacognitions questionnaire--insomnia (MCQ-I) Journal of Behavior Therapy and Experimental Psychiatry. 2009;40(1):15–23. doi: 10.1016/j.jbtep.2008.03.002. [DOI] [PubMed] [Google Scholar]
- Wegner DM. Ironic processes of mental control. Psychol Rev. 1994;101(1):34–52. doi: 10.1037/0033-295x.101.1.34. [DOI] [PubMed] [Google Scholar]
- Wells A. A metacognitive model and therapy for Generalized Anxiety Disorder. Clinical Psychology and Psychotherapy. 1999;6:86–95. [Google Scholar]
- Wells A, Matthews G. Attention and Emotion: A Clinical Perspective. Hove, UK: Erlbaum; 1994. [Google Scholar]
- Wells A, Sembi S. Metacognitive therapy for PTSD: A preliminary investigation of a new brief treatment. Journal of Behavior Therapy and Experimental Psychiatry. 2004;35(4):307–318. doi: 10.1016/j.jbtep.2004.07.001. [DOI] [PubMed] [Google Scholar]
- Wells A, Welford M, King P, Papageorgiou C, Wisely J, Mendel E. A pilot randomized trial of metacognitive therapy vs applied relaxation in the treatment of adults with generalized anxiety disorder. Behaviour Research and Therapy. 2010;48:429–434. doi: 10.1016/j.brat.2009.11.013. [DOI] [PubMed] [Google Scholar]
- Yook K, Lee SH, Ryu M, Kim KH, Choi TK, Suh SY. Usefulness of mindfulness-based cognitive therapy for treating insomnia in patients with anxiety disorders: a pilot study. J Nerv Ment Dis. 2008;196(6):501–503. doi: 10.1097/NMD.0b013e31817762ac. [DOI] [PubMed] [Google Scholar]