Abstract
In an effort to self-medicate psychological distress stemming from exposure to traumatic life events, at-risk youth may be likely to seek intoxication via substance use. Concomitantly, self-medication with psychoactive substances is theorized to confer risk of developing future psychiatric and substance use disorders. The present study employed structural equation modeling to examine self-medication among a sample of 723 youth in residential treatment for antisocial behavior via recursive and non-recursive relationships between trauma history, substance misuse, and psychological distress. Results supported study hypotheses that: (a) the effects of trauma history on psychological distress are partially mediated by substance misuse, and (b) exposure to traumatic life events drives a feedback loop between substance misuse and psychological distress. Findings from this large-scale survey of adolescents exhibiting behavioral dysfunction suggest that identification of self-medication processes among traumatized youth may be crucial for developing targeted prevention and treatment initiatives.
Keywords: Self-medication, Substance abuse, Youth at-risk, Trauma, Psychiatric, Allostasis, Stress
Introduction
Exposure to traumatic life events often results in adverse psychological symptoms, including intrusive cognitions, images, memories, and emotions associated with the original trauma (Brewin et al., 2010; Bryant et al., 2011; Ehlers et al., 2002; Holmes et al., 2005). These post-traumatic symptoms may promote maladaptive or self-destructive behavior, including substance misuse. Individuals exposed to trauma are especially at-risk for developing substance use disorders (Jacobsen et al., 2001). Adults diagnosed with posttraumatic stress disorder (PTSD) exhibit substantially higher rates of substance abuse and dependence than persons without PTSD (i.e., 21.6–43.0 % vs. 8.1–24.7 %), respectively (Breslau et al., 1991; Kessler et al., 1995). Kilpatrick et al. (2000) found that youth who experience traumatic events also have an increased risk of substance misuse. Although the causal mechanism linking trauma, substance misuse, and psychological symptoms remains uncertain, psychoactive substances may be used to self-medicate the dysphoric mood, intrusive cognitions, and somatic sequelae of trauma (Khantzian, 1997; Leeies et al., 2010; Robinson et al., 2011).
The risk chain underlying self-medication of trauma symptoms may involve positive feedback loops between stress appraisal, emotion dysregulation, physiological arousal, compulsive behavior, and palliative coping with substances (Garland et al., 2011). Specifically, traumatic stress results in pathogenic activation of the hypothalamic pituitary adrenal (HPA) axis and the autonomic nervous system (Kaye & Lightman, 2005) coupled with perseverative cognition, the process of ruminating on a cognitive representation of the traumatic event in the absence of implementing adaptive coping behaviors (Brosschot et al., 2006). Prolonged or repeated stress activation subsequent to trauma exposure may lead to an a chronic deviation of self-regulatory mechanisms from their normal mode of operation that leads to heightened stress sensitivity, vulnerability to future stressors, and the eventual development of mood disorders (McEwen, 1998, 2003).
In turn, psychosocial stress and negative mood evoke craving and addiction-related cognitive biases towards drug-related cues (Field & Powell, 2007), leading to increased motivation to acquire and consume drugs which is then sustained through negative reinforcement conditioning (Baker et al., 2004). Stress-dysregulated affect and other psychiatric symptoms often co-occur with substance dependence and may play an etiological role through psychological, neurobiological, and genetic pathways (Sinha, 2007; Zimmermann et al., 2007; Garland et al., 2011). Indeed, chronic, negative emotional states may dysregulated stress and reward neurocircuitry within the extended amygdala, inducing an overall affective balance where dysphoric mood predominates (Koob & Le Moal, 2001). Elevated negative affect may then elicit increased consumption of psychoactive substances as a means of self-medication. Yet, the use of drugs and alcohol to cope with negative emotion can cause further alterations in the extended amygdala, amplifying affective dysregulation and dysphoric mood, and increasing the drive to self-medicate (Koob & Le Moal, 2001). Triggered by traumatic stress, the feedback loop between substance use and psychiatric symptomatology is self-perpetuating and may ultimately lead to the development serious addictive behaviors and/or substance dependence.
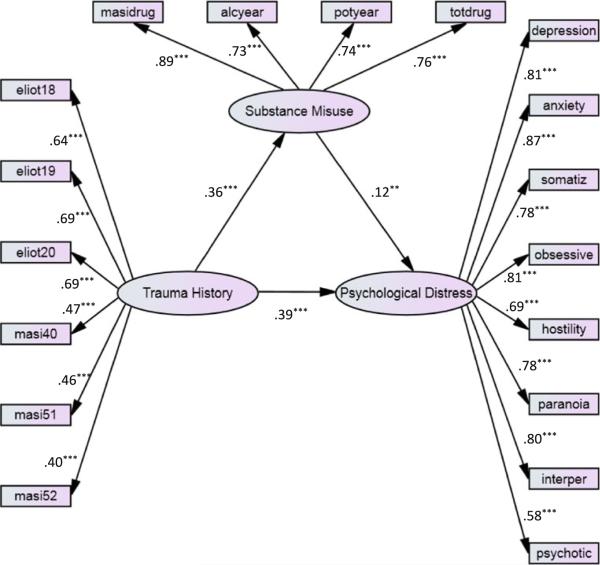
The purpose of the present investigation was to test relationships among trauma history, substance use, and psychological symptoms. We hypothesized that (1) the positive relationship between trauma and psychological distress will be partially mediated by substance misuse and (2) trauma initiates a feedback loop between psychological distress and substance misuse, such that changes in substance misuse lead to alterations in substance use patterns which then reciprocate in further changes in psychological distress. Path diagrams of the conceptual frameworks articulated in hypothesis one and two are depicted in Fig. 1a, b.
Fig. 1.
a The self-medication (partial mediation) model. b A feedback model of self-medication
Structural equation modeling (SEM) was used to test the proposed mediational and feedback effects in a sample of youth in residential treatment for antisocial behavior. Antisocial youth have high rates of trauma and substance misuse (Kilpatrick et al., 2000, 2003; Buka et al., 2001; Abram et al., 2004), tend to escalate substance use over time (Stice et al., 1998), and have increased odds of being diagnosed with psychiatric and substance use disorders in adulthood (Brook et al., 1998; Hofstra et al., 2002). Thus, the study of self-medication within this sample of youth with a history of behavioral problems may provide insight into how this process operates within a population at risk for developing serious psychosocial dysfunction in the future. The advantage of SEM as an analytic technique is that can assess relationships between latent variables instead of single item indicators, thus allowing for potentially more robust and valid measurement of complex constructs such as trauma, substance misuse, and psychiatric symptoms.
Methods
Participants
Adolescent residents of the Missouri division of youth services (DYS) were sampled for this investigation. DYS provides residential rehabilitation services to adjudicated residents ages 13–17 at 27 facilities statewide. Approximately 97.7 % of DYS resident youth (N = 723) were available to be interviewed and agreed to complete the interview. Thus, the present study is nearly a census of the population of Missouri DYS residents at the time the study was undertaken and a large, representative sample of DYS annual residents. Of these youth, 693 (96 % of the total sample) had no missing data on the measures of interest.
Interviews were conducted over a 3-month period and were 30–90 min long, depending on the extensiveness of the respondent's substance use history. Confidential one-on-one interviews were conducted by graduate social work student interviewers in large rooms at each facility in private areas. Youth received $10.00 in their facility monetary accounts as remuneration for their participation. Informed consent and study protocols were approved by the Missouri DYS IRB, Washington University Human Studies Committee IRB, and federal Office of Human Research Protection. The confidentiality of study data was protected by a Certificate of Confidentiality issued by the National Institute on Drug Abuse.
Measures
Frequency of alcohol and marijuana use
Two items assessed how frequently youth had used marijuana and alcohol in the year before entering into DYS custody (once, 2–4, 5–10 times, once a month, every 2–3 weeks, once a week, 2–3 times a week, once a day, and 2–3 times a day).
Polysubstance use
The total number of psychoactive drug classes used was computed by summing the number of affirmative responses to questions assessing lifetime use of 20 different types of psychoactive substances (e.g., cocaine, heroin, barbiturates, amphetamines, etc.).
Substance-related problems
Extent of lifetime substance misuse problems was measured with the total composite score from the 8-item alcohol/drug use problems scale of the Massachusetts youth screening instrument—2nd version (MAYSI-2, Grisso & Barnum, 2000) developed for use with juvenile justice populations. Youth responded “yes” or “no” to questions about whether they had ever been drunk or high at school, had used alcohol and drugs at the same time, had ever been so drunk or high they couldn't remember what happened, used alcohol or drugs to help them feel better, had gotten into trouble while high or drinking, (if yes) whether or not that trouble had been fighting, had done anything they wished they hadn't while drunk or high, or did their parents think they drink too much. Scores could range from 0 to 8.
Trauma history
Lifetime exposure to trauma was measured with the 4-item traumatic experiences scale adapted from the MAYSI-2. Youth were asked to report whether or not they had ever seen someone severely injured or killed in person (not in the movies or on TV), had a lot of bad thoughts or dreams about a bad or scary event that happened to them, and had ever been badly hurt, or been in danger of getting badly hurt or killed. In addition, three items from the victimization index of the self-report of delinquency (SRD, Elliott et al., 1989) were used to assess frequency of personal experiences of criminal victimization (i.e., been hit by someone trying to hurt them, had someone use a weapon or force to get money or things from them, or been attacked by someone with a weapon or by someone trying to seriously hurt or kill them) in the year prior to entering residential treatment.
Psychological distress
All participants completed the brief symptom inventory (BSI), comprised of 53 questions measuring the extent to which youth were distressed (0 = not at all; 4 = extremely) by a wide range of cognitive, emotional, behavioral, and somatic symptoms “over the last 7 days including today.” The BSI consists of items tapping eight primary symptom dimensions for which separate, valid subscale total scores can be calculated; factor analysis confirmed the construct validity of the subscales across samples of adults and adolescents (Derogatis & Melisaratos, 1983). For this study scores were calculated for eight symptom dimensions theoretically linked to trauma: depression, anxiety, somatization, obsessive compulsiveness, interpersonal sensitivity, psychoticism, paranoia, and hostility.
Data analysis
Structural equation modeling (SEM) was conducted with Mplus 6.11 (Muthén & Muthén, 2010); SPSS 17.0 was used for data management purposes. Of the 723 youth sampled, 30 cases (4 %) had missing values. Given that data were missing at random, missing data were handled using full information maximum likelihood estimation (FIML) in Mplus, an approach found to be superior to mean substitution and listwise and pairwise deletion approaches to handling missing data (Little & Rubin, 2002; Wothke, 1998). FIML constructs optimal first and second order missing estimates using all available data points (Wothke, 1998). An initial two-step approach was used for model specification (Kline, 1998). The objective of step one was to determine whether the specified model was a good measurement model. Using the final measurement model, we proceeded with step two and ran the general SEM.
The goodness-of-fit of the measurement model was established before analyzing the general SEM. A congeneric measurement model was developed, loading theoretically related indicators onto their respective latent factors. For each latent variable, we constrained one path coefficient to be one to assign a metric to the variable in question. Confirmatory factor analysis was used to assess how well the measured variables reflected the latent variables and to establish a solid measurement model. We used the maximum likelihood parameter estimates with SEs (MLM) estimator because of its ability to accommodate nonnormal data (Muthén & Muthén 2010). Three fit indices were used to assess the model according to widely accepted cut-offs as reviewed in Kline (1998) (a) the comparative fit index (CFI)—values >.90 were considered a good fit, (b) Tucker Lewis-index (TLI) relative fit index—values >.90 were considered a good fit, and (c) The root mean square error of approximation (RMSEA)—values lower than .08 and the upper bound of its 90 % confidence interval <1 were considered an acceptable model.
After constructing a measurement model with adequate fit, we used SEM to estimate path coefficients. This latent variable approach accounts for measurement error and assigns values to model-implied parameters based on observed data (Kline, 1998). In light of the potential non-normality of the data and the use of ordinal-level indicator variables, structural equation models were estimated using the MLM estimator in Mplus. The MLM estimator uses the Satorra–Bentler (S–B) correction to generate maximum likelihood parameter estimates with SEs and a mean-adjusted χ2 test statistic that are robust to non-normality. The computation of the S–B correction accounts for sample kurtosis values, the estimation method, and the model itself (Byrne, 2012). Prior research indicates that this correction produces reliable test statistics to evaluate mean and covariance structure models under a variety of sample sizes and distributions (Curran et al., 1996; Hu et al., 1992), and yields maximum likelihood parameter estimates and fit indices that are robust to nonormality and the presence of ordinal level variables (Muthén & Muthén, 2010).
We tested the two hypothesized models: (a) a partially mediated recursive model in which trauma has direct effects on substance misuse and indirect effects on substance misuse mediated through psychological distress and (b) a non-recursive model in which trauma drives a feedback loop between psychological distress and substance misuse. For both models, we controlled for the influence of gender by treating this variable as a covariate. The aforementioned fit indices were used to assess goodness-of-fit. To further assess the appropriateness and stability of the specified models, we randomly selected half of the sample and reran the model with the randomly selected subsample. We found no significant differences in path coefficients and model fit between the randomly selected subsample and the full study sample. Thus, findings are reported below only for the full study sample.
Results
Descriptive statistics
A substantial majority (87.0 %, n = 629) of youth in the sample were male. The racial composition of the sample was 32.9 % (n = 238) African American, 55.3 (n = 400) Caucasian, 3.9 % (n = 28) Latino/Latina, 6.2 % (n = 45) biracial, and 1.5 % (n = 11) other. Approximately 39.8 % (n = 288) of youth came from families receiving public assistance. Descriptive statistics of sample variables are reported in Table 1, and zero-order correlations are reported in Table 2.
Table 1.
Descriptive statistics for trauma history, substance misuse, and psychological distress variables
| Variable | M (SD) or N (%) |
|---|---|
| Trauma history variables | |
| Have you ever seen someone severely injured or killed in person? | 471 (65.1 %) |
| Have you had a lot of bad thoughts/dreams about a scary event that happened to you? | 324 (45.1 %) |
| Have you ever been badly hurt or been in danger of being badly hurt or killed? | 467 (64.6 %) |
| How many times in the past 12 months have you been hit by someone trying to hurt you?a | 2.36 (2.31) |
| How many times in the past 12 months have you had someone use a weapon or force or get money or things from you?a | .84 (1.61) |
| How many times in the past 12 months have you been attacked by someone with a weapon or by someone trying to seriously hurt or kill you?a | 1.19 (1.81) |
| Substance misuse variables | |
| Frequency of marijuana use in the year prior to entering residential treatmentb | 5.66 (3.63) |
| Frequency of alcohol use in the year prior to entering residential treatmentb | 3.91 (3.01) |
| Total lifetime number of psychoactive drug types used | 4.09 (2.83) |
| Lifetime substance-related problemsc | 3.94 (2.37) |
| Psychological distress variables | |
| BSI somatization scored | 3.61 (4.34) |
| BSI depression scored | 4.77 (5.06) |
| BSI anxiety scored | 4.36 (4.71) |
| BSI hostility scored | 6.16 (4.99) |
| BSI paranoid ideation scored | 6.28 (4.70) |
| BSI psychoticism scored | 3.65 (3.86) |
| BSI obsessive compulsiveness total scored | 6.63 (5.40) |
| BSI interpersonal sensitivity scored | 2.87 (3.40) |
Scored from 0 to 8 on a Likert-type scale (0 = never, 1 = 1–2 times in the last year, 2 = 1 time every 2–3 months, 3 = 1 time a month, 4 = 1 time every 2–3 weeks, 5 = 1 time a week, 6 = 2–3 times/week, 7 = 1 time a day, 8 = 2–3 times a day)
Scored from 0 to 9 on a Likert-type scale (0 = never, 1 = 1 time, 2 = 2–4 times, 3 = 5–10 times, 4 = 1 time a month, 5 = every 2–3 weeks, 6 = 1 time a week, 7 = 2–3 times a week, 8 = 1 time a day, 9 = 2–3 times a day)
Summary of affirmative responses to 8 dichotomous items tapping substance-related problems
Scored from 0 to 4 on a Likert-type scale (0 = not at all, 4 = extremely)
Table 2.
Correlation matrix of study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. ELIOT 18 | 1.00 | |||||||||||||||||
| 2. ELIOT 19 | .453 | 1.00 | ||||||||||||||||
| 3. ELIOT 20 | .492 | .556 | 1.00 | |||||||||||||||
| 4. SOMATIZ | .171 | .267 | .235 | 1.00 | ||||||||||||||
| 5. OBSESSIVE | .203 | .255 | .190 | .621 | 1.00 | |||||||||||||
| 6. INTERPER | .123 | .188 | .164 | .633 | .633 | 1.00 | ||||||||||||
| 7. DEPRESSION | .161 | .195 | .148 | .600 | .665 | .667 | 1.00 | |||||||||||
| 8. ANXIETY | .169 | .229 | .185 | .719 | .715 | .703 | .699 | 1.00 | ||||||||||
| 9. HOSTILITY | .194 | .260 | .285 | .528 | .558 | .536 | .529 | .595 | 1.00 | |||||||||
| 10. PARANOIA | .193 | .285 | .205 | .560 | .641 | .639 | .643 | .630 | .621 | 1.00 | ||||||||
| 11. PSYCHOTIC | .107 | .165 | .133 | .450 | .452 | .490 | .517 | .479 | .367 | .481 | 1.00 | |||||||
| 12. MAYSIDRUG | .224 | .167 | .168 | .151 | .315 | .099 | .201 | .222 | .199 | .227 | .123 | 1.00 | ||||||
| 13. POTYEAR | .127 | .138 | .132 | .022 | .179 | −.025 | .074 | .078 | .133 | .132 | .031 | .666 | 1.00 | |||||
| 14. ALCYEAR | .244 | .176 | .174 | .104 | .234 | .089 | .171 | .164 | .150 | .175 | .108 | .645 | .552 | 1.00 | ||||
| 15. TOTDRUG | .182 | .156 | .170 | .177 | .340 | .114 | .244 | .259 | .196 | .206 | .194 | .674 | .546 | .563 | 1.00 | |||
| 16. MASI52T | .219 | .268 | .198 | .100 | .123 | .057 | .056 | .081 | .124 | .144 | .112 | .167 | .177 | .154 | .124 | 1.00 | ||
| 17. MASI51T | .281 | .231 | .223 | .349 | .345 | .307 | .309 | .362 | .311 | .363 | .292 | .218 | .078 | .151 | .214 | .259 | 1.00 | |
| 18. MASI40T | .257 | .242 | .270 | .211 | .207 | .166 | .187 | .190 | .275 | .260 | .197 | .233 | .143 | .179 | .230 | .371 | .363 | 1.00 |
ELIOT 18 = “how many times in the past 12 months have you been hit by someone trying to hurt you?”, ELIOT 19 = “how many times in the past 12 months have you had someone use a weapon or force or get money or things from you?”, ELIOT 20 = “how many times in the past 12 months have you been attacked by someone with a weapon or by someone trying to seriously hurt or kill you?”, SOMATIZ = BSI somatization total score, OBSESSIVE = BSI obsessive–compulsive total score, INTERPER = BSI interpersonal sensitivity total score, DEPRESSION = BSI depression total score, ANXIETY = BSI anxiety total score, HOSTILITY = BSI hostility total score, PARANOIA = BSI paranoid ideation total score, PSYCHOTIC = BSI psychoticism total score, MAYSIDRUG = lifetime substance-related problems, POTYEAR = frequency of marijuana use in the year prior to entering residential treatment, ALCYEAR = frequency of alcohol use in the year prior to entering residential treatment, TOTDRUG = total lifetime number of psychoactive drug types used, MASI52T = “have you ever seen someone killed in person?”, MASI51T = “have you had a lot of nightmares about a frightening event?”, MASI40T = “have you ever been badly hurt or been in danger of being badly hurt or killed?”
Overall, the sample reported high rates of traumatic experiences. More than 9 out of 10 (91.4 %, n = 661) youth in the sample reported having had at least one traumatic experience in their lifetime. Specifically, 65.1 % (n = 471) of the total sample reported ever having seen someone severely injured or killed in person, 45.1 % (n = 324) reported ever having negative thoughts or nightmares about a frightening event that happened to them, and 64.6 % (n = 467) reported ever having been badly hurt or having been in danger of being badly hurt or killed. Similarly, youth reported having been physically assaulted in various ways multiple times in the year prior to treatment. The majority of participants had been battered: a cumulative total of 77.2 % (n = 558) had been hit by someone trying to hurt them at least once or twice in the past year, a cumulative total of 35.8 % (n = 259) had been hit at least once a month, and a cumulative total of 19.5 % (n = 141) had been hit at least once a week. In addition, a cumulative total of 7.6 % (n = 55) had been hit at least once a day. Robberies were also common: a cumulative total of 35.2 % of participants (n = 255) had someone use a weapon or force to get money or things from them at least once or twice in the past year, a cumulative total of 11.2 % (n = 81) had been robbed at least once a month, and a cumulative total of 5.5 % (n = 40) had been robbed at least once a week. One-half of participants had been a victim of aggravated assault: a cumulative total of 50.3 % (n = 364) had been attacked by someone with a weapon or by someone trying to seriously hurt or kill them at least once or twice in the past year, a cumulative total of 15.2 % (n = 110) had been assaulted at least once a month, and a cumulative total of 8.2 % (n = 59) had been assaulted at least once a week. With regard to gender differences in trauma history, males were significantly more likely to report having seen someone severely injured or killed (p = .03), whereas females were significantly more likely to report having negative thoughts or nightmares about a traumatic event (p = .009). Similarly, males had been robbed significantly more often than females (p = .03).
Recurrent substance use and polydrug use among the sample was also common. During the year before their incarceration, a cumulative total of 57.3 % of participants (n = 414) smoked marijuana at least 2–3 times a week, and 36.2 % (n = 262) of participants smoked marijuana 2–3 times a day. Similarly, during the year before their incarceration, a cumulative total of 25.6 % of participants (n = 185) drank alcohol at least 2–3 times a week, and 7 % (n = 52) of participants drank alcohol two to three times a day. On average, adolescents in the sample had used 4.1 (SD = 2.8) classes of psychoactive drugs during their lifetime. Moreover, participants reported having experienced an average 4.1 (SD = 4.3) substance-related problems, including impaired psychosocial functioning and the use of substances to self-medicate negative affect. With regard to gender differences in substance misuse, females in this sample exhibited significantly more polydrug use (p = .009) and significantly more frequent use of alcohol (p = .009) than males.
The average psychological profile of the adolescents sampled was marked by a wide range of psychologically distressing symptoms. Females exhibited significantly higher levels of depression, anxiety, phobic anxiety, somatization, interpersonal sensitivity, somatization, and obsessive compulsive symptoms than males (p's < .03–<.001).
Measurement model
The theoretically-specified measurement model was comprised of three latent factors, trauma, substance misuse, and psychological distress. The following variables loaded onto the latent psychological distress factor: depression (β = .81), anxiety (β = .87), somatization (β = .78), obsessive compulsiveness (β = .81), interpersonal sensitivity (β = .80), psychoticism (β = .58), paranoia (β = .78), and hostility (β = .69). The following variables loaded onto the latent substance misuse factor: frequency of marijuana use in the year prior to entering treatment (β = .74), frequency of alcohol use in the year prior to entering treatment (β = .73), frequency of total lifetime substance use (β = .76), and substance-related problems (β = .89). The following variables loaded onto the trauma factor: seen injured or killed (.40), dreams about scary event (β = .46), been badly hurt or at risk of (β = .47), hit by someone in last year (β = .64), used weapon or force against you in last year (β = .69), and attacked with weapon in past year (β = .69). All factor loadings were statistically significant (p < .001) with no cross-loadings. The specified measurement model evidenced acceptable goodness-of-fit, RMSEA = .06 (90 % CI = .05, .06); CFI = .93; TLI = .92, and there were no statistical or theoretical reasons to suggest that changes to the specified model were needed. Therefore, we used this model as final measurement model in subsequent SEM.
Structural equation models
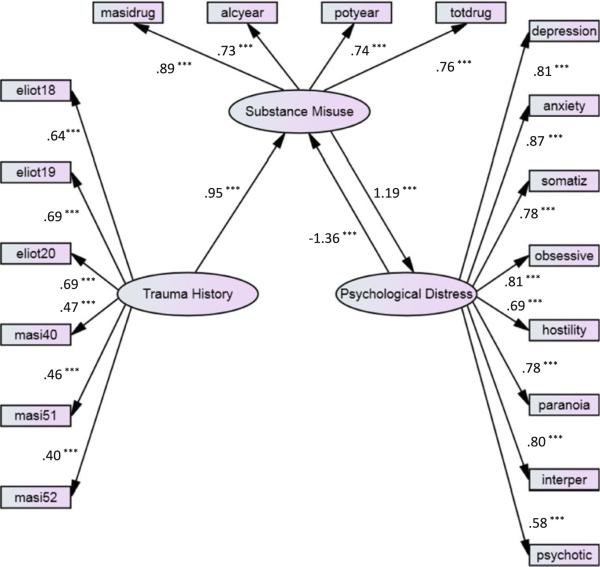
Partial mediation model
The standardized solution for the partial mediation model is presented in Fig. 2. This model exhibited good fit: RMSEA = .06 (90 % CI: .05, .06); TLI = .92; CFI = .93. In this model, trauma history was significantly positively associated with substance misuse (β = .36, p < .001) and psychological distress (β = .39, p < .001). In turn, substance misuse was associated with psychological distress (β = .12, p < .01). The Sobel test for the indirect effect confirmed the first study hypothesis: the effect of trauma on substance misuse was significantly statistically mediated through its indirect effect on psychiatric symptoms (p = .01).
Fig. 2.
SEM of the partial mediation model of self-medication among traumatized youth
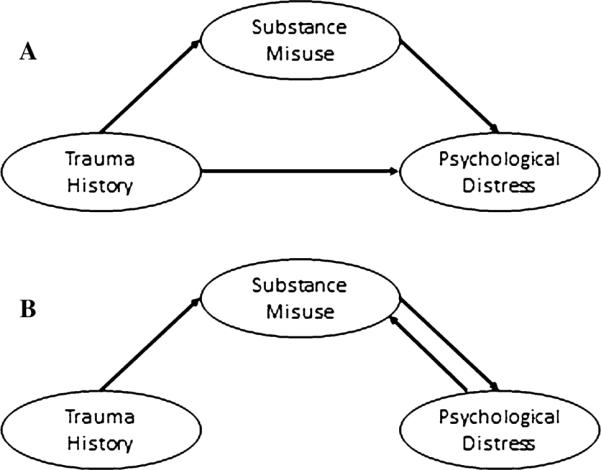
Non-recursive model
The standardized solution for the non-recursive model is presented in Fig. 3. The non-recursive model also fit the data well: RMSEA = .06 (90 % CI: .05, 06); TLI = .92; CFI = .93. In this model, trauma history was significantly positively associated with substance misuse (β = .95, p < .001). In turn, significant pathways from substance misuse to psychological distress (β = 1.12, p < .001) and from psychological distress back to substance misuse (β = −1.36, p < .001) constituted a self-attenuating feedback loop.
Fig. 3.
SEM of the feedback model of self-medication among traumatized youth
Model comparison
The AIC was consulted as a means of comparing the partial mediation model to the non-recursive model (Kline, 1998). AIC of the non-recursive model was larger than that of the partial mediation model (53,478.20 compared to 53,467.39, respectively), indicating that the partial mediation model was more parsimonious than the non-recursive model.
Discussion
As hypothesized, among this relatively large sample of at-risk adolescents, exposure to traumatic experiences was significantly associated with substance misuse and psychiatric symptoms indicative of psychological distress. Specifically, findings lent support to hypothesis one: substance misuse was found to statistically mediate the effect of trauma history on psychological distress. In support of hypothesis two, trauma history was found to be significantly associated with a feedback loop between psychological distress and substance misuse.
Findings related to our first hypothesis suggest that compared to adolescents with limited exposure to traumatic events, youth with extensive trauma histories tend to engage in more extreme patterns of substance misuse, which partially accounts for their more severe psychiatric symptoms. Plausibly, in an attempt to self-medicate psychological distress resulting from exposure to violent and terrifying events, traumatized youth in this study may have engaged in comparatively frequent use of alcohol and marijuana, sought intoxication from a wide array of psychoactive substances, and experienced serious substance-related problems in psychosocial functioning. To the extent that such youth engaged in substance misuse behaviors, this predicted current psychological distress as manifested in symptoms of depression, anxiety, hostility, paranoia, and psychoticism, among others. These findings converge with those of a recent longitudinal study, which found that self-medication of anxiety symptoms significantly predicted the development of incident substance use disorders and anxiety disorders up to 3 years later (Robinson et al., 2011).
Exposure to repeated stressors such as traumatic experiences of violence or abuse during critical developmental periods predicts future susceptibility to mood disorders and substance use (Anda et al., 2006). Trauma may confer risk of developing substance misuse and psychiatric symptoms through multiple pathways. Children exposed to early life trauma exhibit heightened stress reactivity (Bremne & Vermetten, 2001). The experience of recurrent stress is thought to lead to allostatic load on brain structures such as the prefrontal cortex and amygdala (McEwen, 2007), resulting in a host of deleterious effects, including executive function impairments (Liston et al., 2009) and dysphoric mood (McEwen, 2003). Moreover, traumatic brain injury sustained during childhood (such as what might be incurred by blows to the head during incidents of physical abuse) is predictive of cerebral atrophy, impairments in executive function, and impulsivity observed an average of 4 years after the original trauma (Slawik et al., 2009), and focal lesions in the PFC are associated with later risk taking (Floden et al., 2008). Thus, exposure to traumatic experiences may motivate an executively impaired adolescent to impulsively pursue intoxication via psychoactive substance use as a means of self-medicating negative affect.
In our model, substance misuse explained a significant portion of the association between trauma history and current psychological distress. Although the mechanism by which self-medication of trauma with psychoactive substances promotes psychiatric symptoms cannot be directly assessed with the present dataset, Koob and LeMoal's allostatic model of addiction (2001, 2008) provides an explanation for this phenomena. This model posits that the use of substances to compensate for dysphoria results in an opponent process that leads to neurobiological sensitization in the extended amygdala to stress and intensified negative affect, while decreasing sensitivity to reward (Koob & Le Moal, 2001). This upward shift in reward threshold may then elicit increased consumption of psychoactive substances as a means of achieving a hedonic equilibrium (Koob, 2003). Ironically, this attempt to reach a hedonic state comes with a cost: the continued use of substances further increases the reward set point in the brain, making the individual increasingly insensitive to naturally-rewarding experiences while becoming increasingly sensitive to punishment and other aversive states (Koob & Le Moal, 2001). Thus, allostatic load incurred from prior trauma and enhanced by the pharmacological effects of psychoactive substances promotes neuroadaptation to drug effects, modulates sensitization to rewards and punishment, and intensifies negative mood states. This cyclic process then elicits further substance use as a means of countering dysphoric mood. Study findings pertaining to our second hypothesis are consistent with this allostatic conceptualization. Indeed, exposure to traumatic events was significantly associated with substance misuse, which predicted psychiatric symptom severity. In turn, psychiatric symptom severity was significantly associated with substance misuse via a feedback process, a finding that would be predicted by the allostatic model.
Although the data suggest the presence of an allostatic process, non-recursive modeling in SEM is founded on a steady state assumption, which holds that the effects of any changes in a feedback system have already been manifested and thus the system is in equilibrium (Kline, 1998). However, in biological systems, steady states are only temporary, and often yield to positive feedback loops or runaway states, such as that which may be observed in the disease process of cancer (McEwen & Wingfield, 2003). Indeed, the allostatic model (Koob & Le Moal, 2001, 2008) depicts addiction as a positive feedback loop in which the set point of sensitivity to rewards and stressors continually shifts in the direction of an ever-deepening downward spiral of dysregulated affect and compulsive, appetitive behavior. The present analytic approach and cross-sectional nature of the dataset cannot directly test the long-term predictions specified by the allostatic model of addiction. On the other hand, the allostatic model predicts that in the short-term, drug use results in transient increases in reward and decreases in antireward systems in the brain. These initial homeostatic adaptations may be depicted in the non-recursive model reported in this paper. Future studies should employ measures of stress physiology (e.g., cortisol, heart rate variability, amygdala function) and appetitive motivations (e.g., craving) as a means of directly testing allostatic hypotheses among traumatized youth.
It should be noted that substance misuse often results in accidents, health problems, legal issues, and other stressors that can cause or exacerbate anxiety, depression, and other psychiatric symptoms (Brook et al., 2009; Garland & Howard, 2011; Hodgins et al., 2009). Thus, in addition to allostatic processes, real life stressors typically accompany substance misuse.
The present study is limited by the cross-sectional nature of the dataset and use of self-report measures, which may be susceptible to social desirability and recall biases. SEM was able to account for the error inherent in measuring latent variables of interest. Although our measurement model exhibited good fit, indicators variables reflecting victimization in the past-year loaded higher on the trauma history latent variable than the lifetime trauma indicator variables. In contrast, indicators of the psychological distress and substance misuse latent variables evidenced more robust loadings. Measures with greater temporal resolution, such as ecologic momentary assessment, would have been better able to examine the dynamic interaction between traumatic life events, substance use behaviors, and psychological distress. The present study was also limited by a lack of measures of chronic stress exposure, stress sensitization, post-traumatic stress symptoms, sexual trauma, alcohol consumption, and substance use motivations which may have elucidated relationships between the latent variables under investigation. Yet, the victimization variables assessed may serve as a rough proxy for severity of stress exposure, and so our structural model may have partially accounted for this factor. Regardless, the absence of experimental design in the present study precludes any causal inferences. Future research should use experimental methods to directly examine the effect of self-medication on the development of psychiatric symptoms. The fact that the sample was comprised mostly of males may limit the generalizability of study findings. Similarly, study results may not be generalizable to populations other than youth in residential treatment for antisocial behavior.
Despite these limitations, the present investigation had a number of strengths, including a relatively large sample size, a low refusal rate, scant missing values, and near-population level data. This study provides a multivariate statistical evaluation of self-medication processes in a large-scale survey of adolescents exhibiting behavioral dysfunction. As such, study findings have several implications for clinical practice. First, study findings suggest that practitioners working with traumatized youth should be aware of their heightened risk for substance misuse, especially during times when adolescent clients are experiencing significant psychological distress. Second, practitioners should be attuned to the potential feedback loop between psychiatric symptoms and substance use behaviors by recognizing that shifts in one of these variables may be likely to result in changes in the other. Lastly, interventions should be designed to disrupt links in the risk chain between adverse life experiences, psychological distress, and psychoactive substance misuse (Garland et al., 2011). For instance, when treating adolescents with extensive trauma histories for substance use disorders, psychotherapeutic techniques designed to facilitate regulation of negative emotion and appetitive processes (e.g., mindfulness training, see Garland et al., 2010; Garland & Roberts-Lewis, 2011) should be used in tandem with more traditional forms of addictions treatment like motivational interviewing or cognitive behavioral therapy. Targeting such critical factors in the treatment of at-risk youth who have been exposed to trauma may mitigate the development of substance use disorders and increase the probability of achieving positive clinical outcomes.
References
- Abram KM, Teplin LA, Charles DR, Longworth SL, McClelland GM, Dulcan MK. Posttraumatic stress disorder and trauma in youth in juvenile detention. Archives of General Psychiatry. 2004;61:403. doi: 10.1001/archpsyc.61.4.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, et al. The enduring effects of abuse and related adverse experiences in childhood—A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience. 2006;256:174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Bremne JD, Vermetten E. Stress and development: Behavioral and biological consequences. Developmental Psychopathology. 2001;13:473–489. doi: 10.1017/s0954579401003042. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Archives of General Psychiatry. 1991;48:216–222. doi: 10.1001/archpsyc.1991.01810270028003. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Gregory JD, Lipton M, Burgess N. Intrusive images in psychological disorders: Characteristics, neural mechanisms, and treatment implications. Psychological Review. 2010;117:210–232. doi: 10.1037/a0018113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant RA, Friedman MJ, Spiegel D, Ursano R, Strain J. A review of acute stress disorder in DSM-5. Depression and Anxiety. 2011;28:802–817. doi: 10.1002/da.20737. [DOI] [PubMed] [Google Scholar]
- Brook JS, Cohen P, Brook DW. Longitudinal study of co-occurring psychiatric disorders and substance use. Journal of American Academy of Child and Adolescent Psychiatry. 1998;37:322–330. doi: 10.1097/00004583-199803000-00018. [DOI] [PubMed] [Google Scholar]
- Brook JS, Katten NS, Zhang C, Brook DW. Psychosocial antecedents and adverse health consequences resulting from tobacco use, alcohol, and other drug-related problems. American Journal of Public Health. 2009;99:563. doi: 10.2105/AJPH.2007.127225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brosschot JF, Gerin W, Thayer JF. The perseverative cognition hypothesis: A review of worry, prolonged stress-related physiological activation, and health. Journal of Psychosomatic Research. 2006;60:113–124. doi: 10.1016/j.jpsychores.2005.06.074. [DOI] [PubMed] [Google Scholar]
- Buka SL, Stichick TL, Birdthistle I, Earls FJ. Youth exposure to violence: Prevalence, risks, and consequences. American Journal of Orthopsychiatry. 2001;71:298–310. doi: 10.1037/0002-9432.71.3.298. [DOI] [PubMed] [Google Scholar]
- Byrne BM. Structural equation modeling with Mplus. Routledge; New York: 2012. [Google Scholar]
- Curran PJ, West SG, Finch JF. The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychological Methods. 1996;1:16–29. [Google Scholar]
- Derogatis LR, Melisaratos N. The brief symptom inventory: An introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- Ehlers A, Hackmann A, Steil R, Clohessy S, Wenninger K, Winter H. The nature of intrusive memories after trauma: The warning signal hypothesis. Behavior Research and Therapy. 2002;40:995–1002. doi: 10.1016/s0005-7967(01)00077-8. [DOI] [PubMed] [Google Scholar]
- Elliott DS, Huizinga D, Menard S. Multiple problem youth: Delinquency, substance use, and mental health problems. Springer; New York: 1989. [Google Scholar]
- Field M, Powell H. Stress increases attentional bias for alcohol cues in social drinkers who drink to cope. Alcohol and Alcoholism. 2007;42:560–566. doi: 10.1093/alcalc/agm064. [DOI] [PubMed] [Google Scholar]
- Floden D, Alexander MP, Kubu CS, Katz D, Stuss DT. Impulsivity and risk-taking behavior in focal frontal lobe lesions. Neuropsychologia. 2008;46:213–223. doi: 10.1016/j.neuropsychologia.2007.07.020. [DOI] [PubMed] [Google Scholar]
- Garland EL, Howard MO. Adverse consequences of acute inhalant intoxication. Experimental and Clinical Psycho-pharmacology. 2011;19:134. doi: 10.1037/a0022859. [DOI] [PubMed] [Google Scholar]
- Garland EL, Roberts-Lewis A. Differential roles of dispositional mindfulness and thought suppression in post-traumatic stress symptoms and craving. Addictive Behaviors. 2011 doi: 10.1016/j.addbeh.2012.02.004. doi:10.1016/j.bbr.2011.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Gaylord SA, Boettiger CA, Howard MO. Mindfulness training modifies cognitive, affective, and physiological mechanisms implicated in alcohol dependence: Results from a randomized controlled pilot trial. Journal of Psychoactive Drugs. 2010;42:177–192. doi: 10.1080/02791072.2010.10400690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Boettiger CA, Howard MO. Targeting cognitive-affective risk mechanisms in stress-precipitated alcohol dependence: An integrated, biopsychosocial model of allostasis, automaticity, and addiction. Medical Hypotheses. 2011;76:745–754. doi: 10.1016/j.mehy.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grisso T, Barnum R. Massachusetts youth screening instrument-second version: User's manual and technical reports. University of Massachusetts Medical School; Boston, MA: 2000. [Google Scholar]
- Hodgins S, Larm P, Molero-Samuleson Y, Tengström A, Larsson A. Multiple adverse outcomes over 30 years following adolescent substance misuse treatment. Acta Psychiatrica Scandinavica. 2009;119:484–493. doi: 10.1111/j.1600-0447.2008.01327.x. [DOI] [PubMed] [Google Scholar]
- Hofstra MB, Van Der Ende J, Verhulst FC. Child and adolescent problems predict DSM-IV disorders in adulthood: A 14-year follow-up of a Dutch epidemiological sample. Journal of American Academy of Child and Adolescent Psychiatry. 2002;41:182–189. doi: 10.1097/00004583-200202000-00012. [DOI] [PubMed] [Google Scholar]
- Holmes EA, Grey N, Young KA. Intrusive images and “hotspots” of trauma memories in posttraumatic stress disorder: An exploratory investigation of emotions and cognitive themes. Journal of Behavioral Therapy and Experimental Psychiatry. 2005;36:3–17. doi: 10.1016/j.jbtep.2004.11.002. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM, Kano Y. Can test statistics in covariance structure analysis be trusted? Psychological Bulletin. 1992;112:351–362. doi: 10.1037/0033-2909.112.2.351. [DOI] [PubMed] [Google Scholar]
- Jacobsen LK, Southwick SM, Kosten TR. Substance use disorders in patients with posttraumatic stress disorder: A review of the literature. American Journal of Psychiatry. 2001;158:1184–1190. doi: 10.1176/appi.ajp.158.8.1184. [DOI] [PubMed] [Google Scholar]
- Kaye JM, Lightman SL. Psychological stress and endocrine axes. In: Vedhara K, Irwin M, editors. Human Psychoneuroimmunology. Oxford University Press; New York: 2005. [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry. 1997;4:231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Saunders B, Resnick HS, Best CL, Schnurr PP. Risk factors for adolescent substance abuse and dependence: Data from a national sample. Journal of Consulting and Clinical Psychology. 2000;68:692–700. doi: 10.1037//0022-006x.68.1.19. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the national survey of adolescents. Journal of Consulting and Clinical Psychology. 2003;71:692. doi: 10.1037/0022-006x.71.4.692. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. Guilford Press; NY, USA: 1998. [Google Scholar]
- Koob GF. Alcoholism: Allostasis and beyond. Alcoholism, Clinical and Experimental Research. 2003;27:232–243. doi: 10.1097/01.ALC.0000057122.36127.C2. [DOI] [PubMed] [Google Scholar]
- Koob GF, Le Moal M. Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacology. 2001;24:97–129. doi: 10.1016/S0893-133X(00)00195-0. [DOI] [PubMed] [Google Scholar]
- Koob GF, Le Moal M. Addiction and the brain antireward system. Annual Review of Psychology. 2008;59:29–53. doi: 10.1146/annurev.psych.59.103006.093548. [DOI] [PubMed] [Google Scholar]
- Leeies M, Pagura J, Sareen J, Bolton JM. The use of alcohol and drugs to self-medicate symptoms of posttraumatic stress disorder. Depression and Anxiety. 2010;27:731–736. doi: 10.1002/da.20677. [DOI] [PubMed] [Google Scholar]
- Liston C, McEwen BS, Casey BJ. Psychosocial stress reversibly disrupts prefrontal processing and attentional control. Proceedings of the National Academy of Science USA. 2009;106:912–917. doi: 10.1073/pnas.0807041106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RJA, Rubin DA. Statistical analysis with missing data. 2nd ed. Wiley; New York: 2002. [Google Scholar]
- McEwen BS. Stress, adaptation, and disease: Allostasis and allostatic load. Annals of New York Academy of Sciences. 1998;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Mood disorders and allostatic load. Biological Psychiatry. 2003;54:200–207. doi: 10.1016/s0006-3223(03)00177-x. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Physiology and neurobiology of stress and adaptation: Central role of the brain. Physiological Review. 2007;87:873–904. doi: 10.1152/physrev.00041.2006. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Wingfield JC. The concept of allostasis in biology and biomedicine. Hormones and Behavior. 2003;43:2–15. doi: 10.1016/s0018-506x(02)00024-7. [DOI] [PubMed] [Google Scholar]
- Muthén B, Muthén L. Mplus user's guide. 6th ed. Muthén and Muthén; Los Angeles, CA: 2010. [Google Scholar]
- Robinson J, Sareen J, Cox BJ, Bolton JM. Role of self-medication in the development of comorbid anxiety and substance use disorders: A longitudinal investigation. Archives of General Psychiatry. 2011;68:800. doi: 10.1001/archgenpsychiatry.2011.75. [DOI] [PubMed] [Google Scholar]
- Sinha R. The role of stress in addiction relapse. Current Psychiatry Reports. 2007;9:388–395. doi: 10.1007/s11920-007-0050-6. [DOI] [PubMed] [Google Scholar]
- Slawik H, Salmond CH, Taylor-Tavares JV, Williams GB, Sahakian BJ, Tasker RC. Frontal cerebral vulnerability and executive deficits from raised intracranial pressure in child traumatic brain injury. Journal of Neurotrauma. 2009;26:1891–1903. doi: 10.1089/neu.2009.0942. [DOI] [PubMed] [Google Scholar]
- Stice E, Myers MG, Brown SA. A longitudinal grouping analysis of adolescent substance use escalation and de-escalation. Psychology of Addictive Behaviors. 1998;12:14–27. [Google Scholar]
- Wothke W. Longitudinal and multi-group modeling with missing data. In: Little TD, Schnabel KU, Baumert J, editors. Modeling longitudinal and multiple group data: Practical issues, applied approaches and specific examples. Lawrence Erlbaum Associates; Mahwah, NJ: 1998. [Google Scholar]
- Zimmermann US, Blomeyer D, Laucht M, Mann KF. How gene-stress-behavior interactions can promote adolescent alcohol use: The roles of predrinking allostatic load and childhood behavior disorders. Pharmacology, Biochemistry and Behavior. 2007;86:246–262. doi: 10.1016/j.pbb.2006.09.024. [DOI] [PubMed] [Google Scholar]