Abstract
Visualization of the vasculature is becoming increasingly important for understanding many different disease states. While several techniques exist for imaging vasculature, few are able to visualize the vascular network as a whole while extending to a resolution that includes the smaller vessels1,2. Additionally, many vascular casting techniques destroy the surrounding tissue, preventing further analysis of the sample3-5. One method which circumvents these issues is micro-Computed Tomography (μCT). μCT imaging can scan at resolutions <10 microns, is capable of producing 3D reconstructions of the vascular network, and leaves the tissue intact for subsequent analysis (e.g., histology and morphometry)6-11. However, imaging vessels by ex vivo μCT methods requires that the vessels be filled with a radiopaque compound. As such, the accurate representation of vasculature produced by μCT imaging is contingent upon reliable and complete filling of the vessels. In this protocol, we describe a technique for filling mouse coronary vessels in preparation for μCT imaging.
Two predominate techniques exist for filling the coronary vasculature: in vivo via cannulation and retrograde perfusion of the aorta (or a branch off the aortic arch) 12-14, or ex vivo via a Langendorff perfusion system 15-17. Here we describe an in vivo aortic cannulation method which has been specifically designed to ensure filling of all vessels. We use a low viscosity radiopaque compound called Microfil which can perfuse through the smallest vessels to fill all the capillaries, as well as both the arterial and venous sides of the vascular network. Vessels are perfused with buffer using a pressurized perfusion system, and then filled with Microfil. To ensure that Microfil fills the small higher resistance vessels, we ligate the large branches emanating from the aorta, which diverts the Microfil into the coronaries. Once filling is complete, to prevent the elastic nature of cardiac tissue from squeezing Microfil out of some vessels, we ligate accessible major vascular exit points immediately after filling. Therefore, our technique is optimized for complete filling and maximum retention of the filling agent, enabling visualization of the complete coronary vascular network – arteries, capillaries, and veins alike.
Keywords: Medicine, Issue 60, Vascular biology, heart, coronary vessels, mouse, micro Computed Tomography (μCT) imaging, Microfil
Protocol
1. Preparations before starting
Fill each side of the pressure perfusion apparatus with Vasodilator buffer (4mg/L Papaverine + 1g/L Adenosine in PBS) or 4% Paraformaldehyde (PFA) in PBS, respectively.
Prepare a 1/2cc Insulin Syringe (with a permanently attached 29G ½" needle) by filling it with 0.1 ml of 1:100 Heparin (5000U/ml stock) and bending the needle to ~120 degree angle with the bevel up. Do the same with a 1 ml syringe (with a 26G ½" needle) filled with 0.3 ml saturated KCl solution.
2. Exposing the heart and cannulating the aorta
Anesthetize the mouse using your anesthetic of choice. (We use an overdose of a Ketamine/Xylazine mixture: IP injection of 130 mg/kg Ketamine and 8.8 mg/kg Xylazine in saline.)
Pin the anesthetized mouse onto the dissecting tray, ventral side up. Open the abdominal cavity with a midline incision and retract the skin to expose the organs. Move the intestines to one side to expose a region of the Posterior Vena Cava (PVC).
Inject Heparin solution into the PVC. As you extract the needle, cover the needle hole with a cotton-tipped applicator to prevent leaking and hold it for a few seconds until the PVC wall clots and seals. Wait 2-3 minutes for Heparin to disperse throughout the mouse circulation.
Dissect the diaphragm and rib cage so you can observe the beating heart. Slowly inject KCl solution in the PVC until the heart arrests.
Remove all organs below the diaphragm and excise the posterior portion of the mouse, leaving the region anterior of the diaphragm intact. Remove the diaphragm, being careful to cut the PVC near the diaphragm so the portion proximal to the heart is easy to locate in subsequent steps.
Locate the cut end of aorta. Place one long length of 6-0 braided silk suture underneath the aorta a few millimeters anterior from the cut end such that the suture is doubled back on itself. Cut this longer suture in half so there are 2 pieces of suture under the aorta. Insert the angiocatheter into the cut end of the aorta (Fig 1A, B) and tie each suture with a double-knot to hold the angiocatheter in place and prevent any back-pressure within the aorta from leaking out.
3. Perfusion and Microfil injection
Connect the angiocatheter to the pressure perfusion apparatus (Fig 2) and begin perfusing the vessels with vasodilator buffer (Fig 1C) by pumping the perfusion apparatus to a driving pressure of 100-110 mmHg. Double check that buffer is perfusing through the coronaries by ensuring liquid is exiting from the PVC. Continue to perfuse for at least 3 minutes or until the fluid exiting the PVC is clear. (Continue with the next steps while perfusing.)
Dissect the ribs and pin back (or remove) the ribcage to expose the heart. Once exposed, be careful not to let the heart dry out by squeezing drops of buffer onto the heart from a buffer-soaked piece of gauze. Clear away the thymus to expose the aortic arch. Ligate the three major aortic branches using 6-0 braided silk suture to ensure fluid is diverted through the coronaries rather than through these larger, low resistance vessels (Fig 1D).
Perfuse the heart with fixative for 15 minutes, then rinse with Vasodilation buffer for at least 2 minutes. Meanwhile, ligate both Anterior Vena Cavae to prevent Microfil from leaking out of the heart after injection (Fig 1E). Place sutures around the PVC and the aorta but do not tighten them until after filling.
Prepare the Microfil (as specified in table of reagents) and load it into a 1 ml syringe. Fill the dissection tray with enough water to cover the catheter (so as to prevent the introduction of air bubbles when switching from perfusion tubing to the Microfil syringe). Disconnect the perfusion apparatus from the catheter and connect the prepared Microfil syringe.
Inject the Microfil into the aorta until good filling of the coronary arteries is evident (Figs 1F, 3A): the arteries will fill first, and then the Microfil will "spill" into the capillaries as the tissue flushes with the color of the Microfil. Once on the venous side, the hydrophobic nature of the Microfil causes it to initially appear as independent spheres as it emerges from the smaller vessels. Continue to inject the Microfil until a continuous column fills the veins. Complete filling will be evident when the Microfil is continuous within the vessels, and it is exiting through the PVC.
After filling is complete, quickly tighten the sutures that were previously placed around the PVC and aorta to prevent the elastic nature of the cardiac tissue from squeezing the Microfil out of the vessels.
Cover the heart with wet gauze (soaked with water from the dissecting tray) to prevent its drying out, and let it sit for approximately 1 hour at room temperature until the Microfil has polymerized. Avoid any external pressures on the heart during the polymerization process, such as lifting or turning the heart in an attempt to get an early view of the filled vessels in the back of the heart. This may squeeze Microfil from some vessels into a more elastic area of the heart, causing breaks in the Microfil.
Remove the heart and post-fix it in 4% PFA overnight at 4°C. Then store in 70% ethanol at 4 °C. The heart vasculature is now ready for μCT imaging.
4. Representative Results
Vessels which are effectively perfused by Microfil will have continuous, unbroken Microfil throughout the vessels (Fig. 3A). The extent of filling of the coronary vessels can be judged by eye; veins are epicardially located18, and can be easily observed (Fig 3A, arrowhead); arteries, which are more intramyocardial18, are also visible through the surface of the heart (Fig 3A, arrow). Capillary filling is also evident, as cardiac tissue has a very high density of capillaries, and therefore, when the capillaries fill, the cardiac tissue will flush with the color of the Microfil (Fig. 3A, star). Thus, any vascular networks that failed to fill will be noticeable due to the lack of Microfil (Fig. 3B, C).
Discontinuities in the Microfil (asterisks in Fig 3B) often appear because the hydrophobic nature of the Microfil will cause it to contract into itself and cause "breaks" within filled vessels. These "breaks" can be reduced if pressure within the vessels is maintained through proper tie-offs of the vascular exit points from the heart. Other discontinuities can be caused by air bubbles within the microfil. To prevent the introduction of air, make sure the angiocatheter is fully submerged in water when switching from the perfusion apparatus to the Microfil syringe. If an air bubble is introduced, it can often be removed simply by continuing the Microfil perfusion until the bubble has been pushed through and out of the coronary vessels.
Vascular networks may not fill completely if a portion of the vascular bed is blocked (Fig. 3B, arrow). While Heparin inhibits the formation of blood clots, occasional blockages may still occur due to incomplete Heparin perfusion prior to beginning the procedure, or due to other unknown factors. If a blockage occurs, there is, to our knowledge, no method for dislodging the blockage to complete the vascular fill. Incomplete filling can also result if too little pressure is used during filling, as the Microfil will not be forced into all the vascular beds and capillary networks (Fig. 3C). Conversely, too much pressure can cause the capillaries to burst and extravasate Microfil into the surrounding tissue (Fig. 3D).
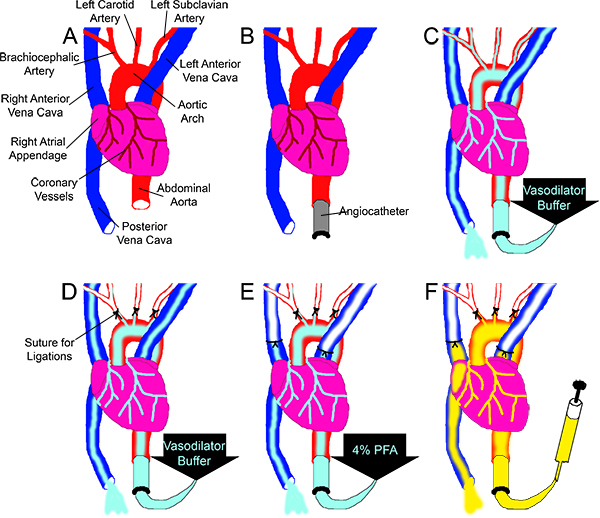 Figure 1. Overview of the Microfil perfusion scheme. (A) The aorta and the PVC are cut at approximately the level of the diaphragm. (B) The ascending aorta is cannulated with an angiocatheter. (C) Vasodilation buffer is perfused through the vessels, driven by the pressure perfusion apparatus (not pictured), while (D) the three main branches off the aortic arch are ligated. (E) 4% PFA is perfused through the coronaries while both Anterior Vena Cavas are ligated. (F) Using a syringe, Microfil is perfused through the coronaries until it is observed exiting from the PVC.
Figure 1. Overview of the Microfil perfusion scheme. (A) The aorta and the PVC are cut at approximately the level of the diaphragm. (B) The ascending aorta is cannulated with an angiocatheter. (C) Vasodilation buffer is perfused through the vessels, driven by the pressure perfusion apparatus (not pictured), while (D) the three main branches off the aortic arch are ligated. (E) 4% PFA is perfused through the coronaries while both Anterior Vena Cavas are ligated. (F) Using a syringe, Microfil is perfused through the coronaries until it is observed exiting from the PVC.
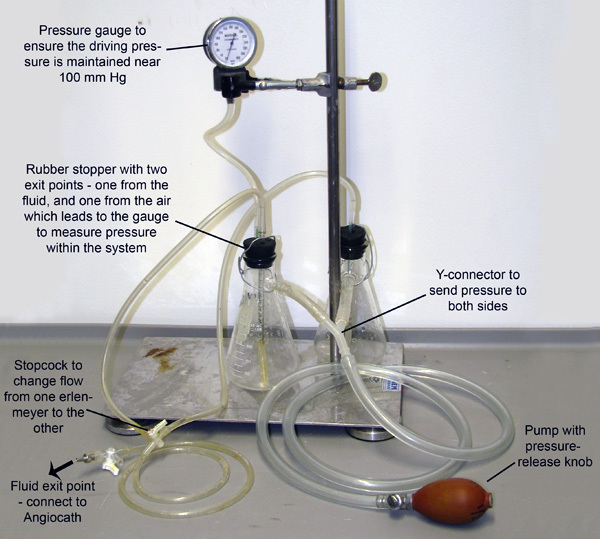 Figure 2. Perfusion Apparatus. Two Erlenmeyer flasks, each filled with either Vasodilation buffer or 4% PFA, are joined and pressurized through tubes connected to their sidearms. The system is pressurized through manual pumping of the bulb, and a pressure gauge is connected to one of the flasks to allow monitoring and maintenance of pressure. Small tubes extend through rubber stoppers and down into the fluid in each flask. Pressure entering from the sidearms pumps the fluid from each flask out these smaller tubes. The tubes then merge at a stopcock which only allows fluid to flow from one flask at a time.
Figure 2. Perfusion Apparatus. Two Erlenmeyer flasks, each filled with either Vasodilation buffer or 4% PFA, are joined and pressurized through tubes connected to their sidearms. The system is pressurized through manual pumping of the bulb, and a pressure gauge is connected to one of the flasks to allow monitoring and maintenance of pressure. Small tubes extend through rubber stoppers and down into the fluid in each flask. Pressure entering from the sidearms pumps the fluid from each flask out these smaller tubes. The tubes then merge at a stopcock which only allows fluid to flow from one flask at a time.
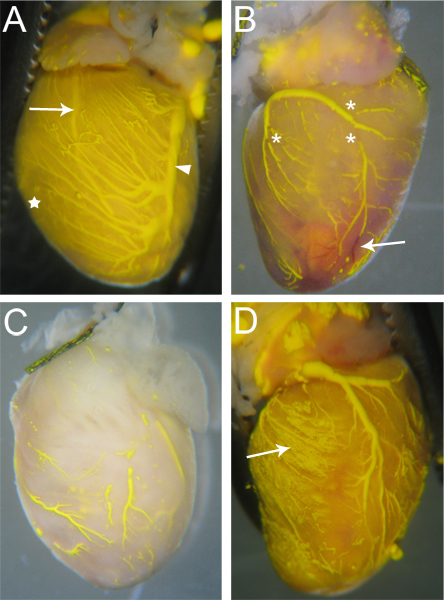 Figure 3. Sample Microfilled hearts. (A) Vessels that are filled well will have few (if any) breaks in the Microfil, and the heart tissue will be tinged the color of the Microfil due to the filled capillaries (star, and compare with C). Both arteries (arrow – Left Anterior Descending Artery) and veins (arrowhead – Left Coronary Vein) are visible through the heart surface. (B) A heart with breaks in the microfil (asterisks) as well as blockages in some vessels that prevented complete Microfil penetration. The blocked vessels remain red (arrow), as the blood was not flushed out during the perfusion process. (C) A heart with vessels that were incompletely filled. Notice the tissue has not taken on the yellow color of the Microfil, indicating the Microfil did not penetrate into the capillaries. (D) A heart where the capillaries burst during filling, causing the Microfil to leak into the surrounding tissue (arrow).
Figure 3. Sample Microfilled hearts. (A) Vessels that are filled well will have few (if any) breaks in the Microfil, and the heart tissue will be tinged the color of the Microfil due to the filled capillaries (star, and compare with C). Both arteries (arrow – Left Anterior Descending Artery) and veins (arrowhead – Left Coronary Vein) are visible through the heart surface. (B) A heart with breaks in the microfil (asterisks) as well as blockages in some vessels that prevented complete Microfil penetration. The blocked vessels remain red (arrow), as the blood was not flushed out during the perfusion process. (C) A heart with vessels that were incompletely filled. Notice the tissue has not taken on the yellow color of the Microfil, indicating the Microfil did not penetrate into the capillaries. (D) A heart where the capillaries burst during filling, causing the Microfil to leak into the surrounding tissue (arrow).
Discussion
Cardiac tissue has a very high metabolic demand, and therefore requires a constant supply of nutrients and oxygen from the blood delivered by the coronary vasculature. Diseases of the coronary vessels, which decrease coronary function due to vessel stenosis and blockage, can lead to tissue hypoxia and ischemia, and put affected patients at risk for myocardial infarction and irreparable damage to the heart muscle. A better understanding of the diseased state of these vessels is necessary, and critical to our ability to study coronary vessels is visualization of the vasculature. Here, we present a method for preparing murine coronary vasculature for ex vivo imaging by filling the vasculature with a radiopaque material. This protocol was specifically designed to ensure complete filling, and subsequently visualization, of all coronary vessels including capillaries.
To ensure complete filling of all capillaries, the filling agent, Microfil, must be injected into a partially closed system that will force the Microfil into the smaller, higher resistance vessels within the vascular network. To create this partial closure within our in vivo filling system, we ligate the three larger, low resistance arteries branching from the aortic arch. While this does not exclude all other potential "leakage" points, the remaining vessels (principally the intercostal arteries) are sufficiently small that any pressure lost through them does not interfere with complete filling of the coronary vascular system. Once the Microfil has perfused all the vessels in the heart, the innate elastic nature of the cardiac and vascular tissue will squeeze the Microfil out of some vessels. To prevent this loss of Microfil, we ligate all large and accessible exit points, namely, both superior vena cavae, the posterior vena cava, and the aorta, after the coronary vasculature is completely perfused. In this way, pressure is maintained in the heart until the Microfil polymerizes, allowing the Microfil to conform to the vessel structure under normal physiological blood pressure.
Alternatively, if visualization of the capillaries is not required, it is also possible to fill only the arterial or only the venous vascular beds. More viscous versions of Microfil can be mixed using a high viscosity diluent (available from FlowTech). The more viscous perfusate is unable to penetrate the capillaries, and therefore allows visualization of only the arteries, or only the veins if perfused from the venous side. In addition, the protocol presented here can easily be adapted to other species or non-adult mice. Scaling the procedure to appropriately match the size of the animal simply requires that the catheter and the perfusion tubing are properly sized to the animal's aorta so as to minimize leaking and prevent stretching or breaking. The volumes of fluids injected (i.e. heparin, saturated KCl, and the Microfil) must also be appropriately scaled.
Our protocol was specifically designed for injection of Microfil and imaging by μCT, however, it can easily be adapted for other filling agents, either for μCT analysis, or other ex vivo imaging techniques. When looking for μCT compatible fillers, there are several options of radiopaque dyes, as many substances used for filling and studying vasculature via other imaging methods (e.g. acrylic) can be infused with radio opaque material, such as a lead pigment9 or an osmium solution3. Regardless of the filling agent utilized, μCT imaging offers the advantage that the results can be reconstructed into a 3D model to provide vascular measurements as well as structural information about the branching pattern of the filled coronary vessels 6,7,14,19. In addition, imaging by μCT preserves the surrounding tissue, thus allowing for additional analyses after the scan. Thus, filled and scanned hearts can be processed for histological analysis, and sections stained for various markers can be aligned with μCT data to correlate arterial/venous identity, the presence of smooth muscle coats, or additional histological indices.
Other common vascular imaging techniques also require vascular filling and our protocol can easily be adapted for perfusing the coronaries with any of these other filling agents. Scanning Electron Microscopy (SEM) requires filling the vessels and then dissolving the soft tissue away from the established vascular cast in a process called corrosion casting. In order to maintain the shape of the vessels without the support of the surrounding soft tissue, the filling agent must be strong and non-brittle: often an acrylic resin (e.g. Mercox, Batson's)3,20,21. While SEM provides scanning resolutions vastly superior to that of μCT imaging 22, the corrosion casting procedure destroys the tissue, preventing any additional tissue analysis. Another method of ex vivo imaging of the coronary vasculature, Optical Projection Tomography (OPT), can detect visible or near-visible light, and thus allows for the detection of fluorescent signals in addition to chromogenic precipitates such as the purple precipitate produced by alkaline phosphatase conversion of BCIP/NBT (5-bromo-4-chloro-3-indolyl phosphate/4-nitro blue tetrazolium)23-25. Visualization of vessels, therefore, can be accomplished either by filling with a fluorescent substance (e.g. PU4ii: a polyurethane resin 3, or fluorescein infused dextran26), or through non-filling methods, such as whole-mount immunodetection via either fluorescence or a histochemical chromogenic precipitate (e.g. BCIP/NBT) 23. OPT imaging can achieve resolutions slightly better than that of μCT (to around 1 micron); however, for both the filling and the immunodetection methods the surrounding soft tissue must be chemically cleared, which may disrupt some antigens for histological analysis post-scanning.
There are also several methods for imaging the coronary vasculature that do not require vascular filling or immunodetection, and as such can be performed in vivo. One technique, Contrast Enhanced High Resolution Ultrasound (CEHRUS), utilizes gas filled microbubbles as a contrast agent. Injection of these microbubbles into the blood stream allows for visualization of the flow of blood with real-time flow measurements down to the capillary level, but it does not provide a 3D view of the imaged vessels 2,27-31. Another method, Magnetic Resonance Angiography (MRA) has also been used to image coronary vessels 32-34, and recent advances in MRA have extended its imaging capabilities to obtain real-time blood flow measurements 35,36. While MRA can produce 3D reconstructions of the vessels imaged, the resolution of MRA is currently limited to around 100 microns, and therefore fails to identify smaller vessels (capillaries, arterioles and venules).
Since both CEHRUS and MRA can be performed on live animals, they offer the advantage of repeatedly and non-invasively monitoring blood flow and vascular development. However, the relatively low resolution of MRA and the lack of 3D capabilities from CEHRUS preclude imaging of the coronary network as a whole. Thus, the ex vivo imaging techniques which require vascular filling agents or immunodetection are important for obtaining high resolution 3D information of the coronary vascular system, while the in vivo techniques provide valuable information regarding functionality of the vascular network (i.e., flow data) over time. Combining in vivo time course analysis with end point ex vivo imaging provides a powerful system for study of the coronary vasculature.
Disclosures
Mice were handled with methods approved by the Institutional Animal Care and Use Committee of the University of Washington and in accordance with the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85-23, revised 1996).
Acknowledgments
We thank Dr. Kelly Stevens for initial trials of the protocol, Dr. Michael Simons, Dr. Kip Hauch, and members of both of their labs for general discussion.
This work is support by NIH grants HL087513 and P01 HL094374.
References
- Couffinhal T, Dufourcq P, Barandon L, Leroux L, Duplaa C. Mouse models to study angiogenesis in the context of cardiovascular diseases. Front. Biosci. 2009;14:3310–3325. doi: 10.2741/3454. [DOI] [PubMed] [Google Scholar]
- Zagorchev L, Mulligan-Kehoe MJ. Molecular imaging of vessels in mouse models of disease. Eur. J. Radiol. 2009;70:305–311. doi: 10.1016/j.ejrad.2009.01.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krucker T, Lang A, Meyer EP. New polyurethane-based material for vascular corrosion casting with improved physical and imaging characteristics. Microsc. Res. Tech. 2006;69:138–147. doi: 10.1002/jemt.20263. [DOI] [PubMed] [Google Scholar]
- Murakami T. Blood flow patterns in the rat pancreas: a simulative demonstration by injection replication and scanning electron microscopy. Microsc. Res. Tech. 1997;37:497–508. doi: 10.1002/(SICI)1097-0029(19970601)37:5/6<497::AID-JEMT12>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Icardo JM, Colvee E. Origin and course of the coronary arteries in normal mice and in iv/iv mice. J. Anat. 2001;199:473–482. doi: 10.1046/j.1469-7580.2001.19940473.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beighley PE, Thomas PJ, Jorgensen SM, Ritman EL. 3D architecture of myocardial microcirculation in intact rat heart: a study with micro-CT. Adv. Exp. Med. Biol. 1997;430:165–175. doi: 10.1007/978-1-4615-5959-7_14. [DOI] [PubMed] [Google Scholar]
- Bentley MD, Ortiz MC, Ritman EL, Romero JC. The use of microcomputed tomography to study microvasculature in small rodents. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2002;282:R1267–R1279. doi: 10.1152/ajpregu.00560.2001. [DOI] [PubMed] [Google Scholar]
- Jorgensen SM, Demirkaya O, Ritman EL. Three-dimensional imaging of vasculature and parenchyma in intact rodent organs with X-ray micro-CT. Am. J. Physiol. 1998;275:H1103–H1114. doi: 10.1152/ajpheart.1998.275.3.H1103. [DOI] [PubMed] [Google Scholar]
- Marxen M. MicroCT scanner performance and considerations for vascular specimen imaging. Med. Phys. 2004;31:305–313. doi: 10.1118/1.1637971. [DOI] [PubMed] [Google Scholar]
- Zagorchev L. Micro computed tomography for vascular exploration. J. Angiogenes. Res. 2010;2:7–7. doi: 10.1186/2040-2384-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinzer S. Hierarchical microimaging for multiscale analysis of large vascular networks. Neuroimage. 2006;32:626–636. doi: 10.1016/j.neuroimage.2006.03.043. [DOI] [PubMed] [Google Scholar]
- Dedkov EI. Synectin/syndecan-4 regulate coronary arteriolar growth during development. Dev. Dyn. 2007;236:2004–2010. doi: 10.1002/dvdy.21201. [DOI] [PubMed] [Google Scholar]
- Gossl M. Functional anatomy and hemodynamic characteristics of vasa vasorum in the walls of porcine coronary arteries. Anat. Rec. A. Discov. Mol. Cell. Evol. Biol. 2003;272:526–537. doi: 10.1002/ar.a.10060. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Porcel M. Altered myocardial microvascular 3D architecture in experimental hypercholesterolemia. Circulation. 2000;102:2028–2030. doi: 10.1161/01.cir.102.17.2028. [DOI] [PubMed] [Google Scholar]
- Bell RM, Mocanu MM, Yellon DM. Retrograde heart perfusion: The Langendorff technique of isolated heart perfusion. J. Mol. Cell. Cardiol. 2011;50:940–950. doi: 10.1016/j.yjmcc.2011.02.018. [DOI] [PubMed] [Google Scholar]
- Skrzypiec-Spring M, Grotthus B, Szelag A, Schulz R. Isolated heart perfusion according to Langendorff---still viable in the new millennium. J. Pharmacol. Toxicol. Methods. 2007;55:113–126. doi: 10.1016/j.vascn.2006.05.006. [DOI] [PubMed] [Google Scholar]
- Toyota E. Vascular endothelial growth factor is required for coronary collateral growth in the rat. Circulation. 2005;112:2108–2113. doi: 10.1161/CIRCULATIONAHA.104.526954. [DOI] [PubMed] [Google Scholar]
- Lavine KJ, Long F, Choi K, Smith C, Ornitz DM. Hedgehog signaling to distinct cell types differentially regulates coronary artery and vein development. Development. 2008;135:3161–3171. doi: 10.1242/dev.019919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheema AN. Adventitial microvessel formation after coronary stenting and the effects of SU11218, a tyrosine kinase inhibitor. J. Am. Coll. Cardiol. 2006;47:1067–1075. doi: 10.1016/j.jacc.2005.08.076. [DOI] [PubMed] [Google Scholar]
- Lametschwandtner A, Lametschwandtner U, Weiger T. Scanning electron microscopy of vascular corrosion casts--technique and applications: updated review. Scanning Microsc. 1990;4:889–941. [PubMed] [Google Scholar]
- Schneider P. Simultaneous 3D visualization and quantification of murine bone and bone vasculature using micro-computed tomography and vascular replica. Microsc. Res. Tech. 2009;72:690–701. doi: 10.1002/jemt.20720. [DOI] [PubMed] [Google Scholar]
- Manelli A, Sangiorgi S, Binaghi E, Raspanti M. 3D analysis of SEM images of corrosion casting using adaptive stereo matching. Microscopy Research and Technique. 2007;70:350–354. doi: 10.1002/jemt.20417. [DOI] [PubMed] [Google Scholar]
- Alanentalo T. Tomographic molecular imaging and 3D quantification within adult mouse organs. Nat. Meth. 2007;4:31–33. doi: 10.1038/nmeth985. [DOI] [PubMed] [Google Scholar]
- Quintana L, Sharpe J. Optical projection tomography of vertebrate embryo development. Cold Spring Protoc; 2011. pp. 586–594. [DOI] [PubMed] [Google Scholar]
- Walls JR, Coultas L, Rossant J, Henkelman RM. Three-Dimensional Analysis of Vascular Development in the Mouse Embryo. PLoS ONE. 2008;3:e2853–e2853. doi: 10.1371/journal.pone.0002853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalothorn D, Clayton JA, Zhang H, Pomp D, Faber JE. Collateral density, remodeling, and VEGF-A expression differ widely between mouse strains. Physiol. Genomics. 2007;30:179–191. doi: 10.1152/physiolgenomics.00047.2007. [DOI] [PubMed] [Google Scholar]
- Behm CZ. Molecular Imaging of Endothelial Vascular Cell Adhesion Molecule-1 Expression and Inflammatory Cell Recruitment During Vasculogenesis and Ischemia-Mediated Arteriogenesis. Circulation. 2008;117:2902–2911. doi: 10.1161/CIRCULATIONAHA.107.744037. [DOI] [PubMed] [Google Scholar]
- Carr CL, Lindner JR. Myocardial perfusion imaging with contrast echocardiography. Curr. Cardiol. Rep. 2008;10:233–239. doi: 10.1007/s11886-008-0039-8. [DOI] [PubMed] [Google Scholar]
- Leong-Poi H. Assessment of Endogenous and Therapeutic Arteriogenesis by Contrast Ultrasound Molecular Imaging of Integrin Expression. Circulation. 2005;111:3248–3254. doi: 10.1161/CIRCULATIONAHA.104.481515. [DOI] [PubMed] [Google Scholar]
- Villanueva FS. Microbubbles Targeted to Intercellular Adhesion Molecule-1 Bind to Activated Coronary Artery Endothelial Cells. Circulation. 1998;98:1–5. doi: 10.1161/01.cir.98.1.1. [DOI] [PubMed] [Google Scholar]
- Wei K. Quantification of Myocardial Blood Flow With Ultrasound-Induced Destruction of Microbubbles Administered as a Constant Venous Infusion. Circulation. 1998;97:473–483. doi: 10.1161/01.cir.97.5.473. [DOI] [PubMed] [Google Scholar]
- Beckmann N, Stirnimann R, Bochelen D. High-Resolution Magnetic Resonance Angiography of the Mouse Brain: Application to Murine Focal Cerebral Ischemia Models. Journal of Magnetic Resonance. 1999;140:442–450. doi: 10.1006/jmre.1999.1864. [DOI] [PubMed] [Google Scholar]
- Kobayashi H. 3D MR angiography of intratumoral vasculature using a novel macromolecular MR contrast agent. Magnetic Resonance in Medicine. 2001;46:579–585. doi: 10.1002/mrm.1230. [DOI] [PubMed] [Google Scholar]
- Nezafat R. B1-insensitive T2 preparation for improved coronary magnetic resonance angiography at 3 T. Magn. Reson. Med. 2006;55:858–864. doi: 10.1002/mrm.20835. [DOI] [PubMed] [Google Scholar]
- Wagner S, Helisch A, Ziegelhoeffer T, Bachmann G, Schaper W. Magnetic resonance angiography of collateral vessels in a murine femoral artery ligation model. NMR in Biomedicine. 2004;17:21–27. doi: 10.1002/nbm.859. [DOI] [PubMed] [Google Scholar]
- Cochet H. In vivo MR angiography and velocity measurement in mice coronary arteries at 9.4 T: assessment of coronary flow velocity reserve. Radiology. 2010. pp. 254–441. [DOI] [PubMed]


