Abstract
Chemotherapy-induced neurotoxicity is a serious consequence of cancer treatment, which occurs with some of the most commonly used chemotherapies1,2. Chemotherapy-induced peripheral neuropathy produces symptoms of numbness and paraesthesia in the limbs and may progress to difficulties with fine motor skills and walking, leading to functional impairment. In addition to producing troubling symptoms, chemotherapy-induced neuropathy may limit treatment success leading to dose reduction or early cessation of treatment. Neuropathic symptoms may persist long-term, leaving permanent nerve damage in patients with an otherwise good prognosis3. As chemotherapy is utilised more often as a preventative measure, and survival rates increase, the importance of long-lasting and significant neurotoxicity will increase.
There are no established neuroprotective or treatment options and a lack of sensitive assessment methods. Appropriate assessment of neurotoxicity will be critical as a prognostic factor and as suitable endpoints for future trials of neuroprotective agents. Current methods to assess the severity of chemotherapy-induced neuropathy utilise clinician-based grading scales which have been demonstrated to lack sensitivity to change and inter-observer objectivity4. Conventional nerve conduction studies provide information about compound action potential amplitude and conduction velocity, which are relatively non-specific measures and do not provide insight into ion channel function or resting membrane potential. Accordingly, prior studies have demonstrated that conventional nerve conduction studies are not sensitive to early change in chemotherapy-induced neurotoxicity4-6. In comparison, nerve excitability studies utilize threshold tracking techniques which have been developed to enable assessment of ion channels, pumps and exchangers in vivo in large myelinated human axons7-9.
Nerve excitability techniques have been established as a tool to examine the development and severity of chemotherapy-induced neurotoxicity10-13. Comprising a number of excitability parameters, nerve excitability studies can be used to assess acute neurotoxicity arising immediately following infusion and the development of chronic, cumulative neurotoxicity. Nerve excitability techniques are feasible in the clinical setting, with each test requiring only 5 -10 minutes to complete. Nerve excitability equipment is readily commercially available, and a portable system has been devised so that patients can be tested in situ in the infusion centre setting. In addition, these techniques can be adapted for use in multiple chemotherapies.
In patients treated with the chemotherapy oxaliplatin, primarily utilised for colorectal cancer, nerve excitability techniques provide a method to identify patients at-risk for neurotoxicity prior to the onset of chronic neuropathy. Nerve excitability studies have revealed the development of an acute Na+ channelopathy in motor and sensory axons10-13. Importantly, patients who demonstrated changes in excitability in early treatment were subsequently more likely to develop moderate to severe neurotoxicity11. However, across treatment, striking longitudinal changes were identified only in sensory axons which were able to predict clinical neurological outcome in 80% of patients10. These changes demonstrated a different pattern to those seen acutely following oxaliplatin infusion, and most likely reflect the development of significant axonal damage and membrane potential change in sensory nerves which develops longitudinally during oxaliplatin treatment10. Significant abnormalities developed during early treatment, prior to any reduction in conventional measures of nerve function, suggesting that excitability parameters may provide a sensitive biomarker.
Keywords: Neuroscience, Issue 62, Chemotherapy, Neurotoxicity, Neuropathy, Nerve excitability, Ion channel function, Oxaliplatin, oncology, medicine
Protocol
1. Patient Preparation
Patients are referred from the Department of Medical Oncology for baseline nerve excitability testing prior to commencement on chemotherapy.
Patient suitability for excitability testing must be determined. Patients should be excluded if they have a history of or baseline neurophysiological evidence of peripheral neuropathy, have received prior neurotoxic chemotherapy treatment or there are any contra-indications for excitability testing.
2. Axonal Excitability Procedures
Undertake sensory and motor excitability protocols on the median nerve, using the semi-automated computerized system QTracS (Institute of Neurology, Queen Square, UK), an isolated linear bipolar constant current stimulator (Digitimer, Welwyn Garden City, UK) and an amplifier (Sapphire IIA, Medelec, UK).
Prepare the skin surface at the wrist and forearm with an abrasive gel or pad to reduce skin resistance, followed by application of an alcohol wipe.
Prepare the recording site for motor recordings- with non-polarizable electrodes placed on the muscle belly of abductor pollicis brevis and a reference electrode 4cm distal to record compound motor action potentials (CMAPs).
Prepare the recording site for sensory recordings - using ring electrodes placed at the proximal and distal interphalangeal joints for recording and reference electrodes respectively, to record compound sensory action potentials (CSAPs).
Place an electrosurgical neutral earth plate in the palm, with conductive gel.
Electrical noise in the recording setup should be removed as much as possible, using a Humbug 50/60 Hz Noise eliminator (Quest Scientific Instruments, North Vancouver, Canada).
Stimulate the median nerve at the wrist. Stimulation site should be selected as the site of lowest threshold, using a repositionable bipolar electrode and subsequently a non-polarizable electrode.
The anode electrode should be placed 10 cm proximal from the stimulating electrode over bone.
Monitor temperature at the site of stimulation throughout the test and ensure that the temperature is greater than 32 °C.
3. Axonal Excitability Protocols
Record a stimulus-response curve by incrementally increasing the stimulus until the response is maximal and does not augment when stimulus intensity is further increased.
The target amplitude for threshold tracking is set automatically to 30%-40% of maximal amplitude, corresponding to the area of steepest slope on the stimulus-response curve.
As per the method of Bostock et al., 1998, changes in threshold current required to achieve the target amplitude are tracked online.
Record multiple excitability parameters, including threshold electrotonus (TE), recovery cycle (RC) and current-threshold (I/V) relationship as described in Kiernan et al., 2000 and Kiernan et al., 2001.
Threshold electrotonus is assessed using 100ms subthreshold polarizing currents, with polarizing current set to ± 40% of control threshold (Fig. 1). The change in threshold current required to maintain target response amplitude following both de- and hyper-polarization is recorded. Threshold electrotonus provides an assessment of internodal conductances and membrane potential, with responses in the hyperpolarizing direction at the end of the polarizing pulse (90-100 ms) strongly associated with membrane potential.
The recovery cycle is assessed using a paired pulse paradigm (Fig. 2), with an initial supramaximal conditioning stimulus followed at different intervals by a test stimulus (from 2.5 ms to 200 ms). Following the supramaximal stimulus, it is more difficult to generate a subsequent response, termed 'refractoriness', reflecting the inactivation of voltage-gated Na+ channels. Following the refractory period, a period of facilitation known as superexcitability occurs.
Current-threshold relationship is assessed using polarizing currents of 200 ms which vary in strength from +50% to -100% of threshold.
4. Patient Assessment
Using these techniques, patients are assessed both acutely and longitudinally across chemotherapy treatment. To assess acute neurotoxicity, patients return for post-chemotherapy assessment within 48 hours of receiving treatment.
To examine chronic neurotoxicity, assessments taken prior to chemotherapy infusion are compared longitudinally across treatment cycles.
In addition to axonal excitability testing, conventional clinical grading scales should be used to assess chemotherapy-induced neurotoxicity, including the National Cancer Institute - Common Criteria for Adverse Events Neuropathy Sensory Subscale, Total Neuropathy Score and patient-reported outcome assessment.
5. Analysis and Interpretation
To identify acute neurotoxicity, results are compared pre- and post-chemotherapy treatment. To assess the development of longitudinal changes in nerve function, results are compared across treatment. Key parameters for assessment include refractoriness, superexcitability, extent of threshold change in threshold electrotonus (hyperpolarizing 90-100 ms), in addition to conventional parameters such as peak amplitude and latency.
To assess overall change in excitability parameters across treatment, a composite excitability score is calculated. The change in three parameters - superexcitability, refractoriness and threshold electrotonus (hyperpolarizing 90-100 ms) - is summed from initial to final treatments to give an overall marker of change.
6. Representative Results
Examples of excitability results in a patient treated with oxaliplatin are provided. Immediately post-oxaliplatin infusion, acute changes in both sensory and motor excitability develop, suggestive of the development of a functional Na+ channelopathy10 -13. However, significant change in multiple excitability parameters develops progressively across oxaliplatin treatment only in sensory axons, with motor axons unaffected (Fig. 3), reflecting widespread sensory axonal damage and membrane potential change. This pattern matches the clinical expression of symptoms in chronic oxaliplatin-induced neurotoxicity. Excitability changes in sensory axons precedes reductions in peak amplitude as assessed using conventional nerve conduction techniques, and suggest that axonal excitability techniques may provide a sensitive assessment tool for early oxaliplatin-induced neurotoxicity.
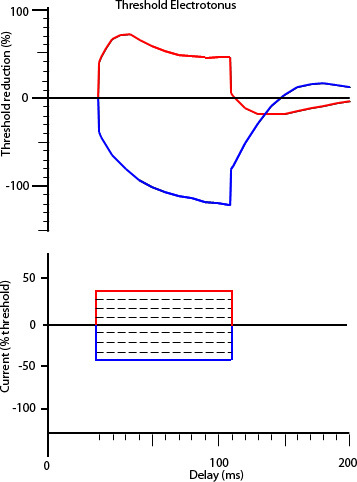 Figure 1. Threshold electrotonus, depicting waveforms in response to prolonged subthreshold polarizing current (100 ms), with hyperpolarizing direction plotted in the bottom quadrant (blue) and depolarizing direction plotted in the upper quadrant (red). Below is the stimulus waveform applied to generate the threshold electrotonus response.
Figure 1. Threshold electrotonus, depicting waveforms in response to prolonged subthreshold polarizing current (100 ms), with hyperpolarizing direction plotted in the bottom quadrant (blue) and depolarizing direction plotted in the upper quadrant (red). Below is the stimulus waveform applied to generate the threshold electrotonus response.
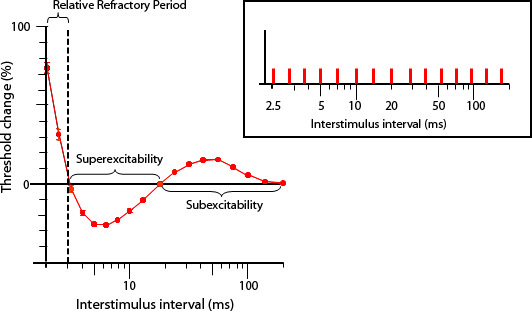 Figure 2. Recovery cycle of excitability, demonstrating the characteristic sequence of excitability changes following impulse conduction, with a period of reduced excitability (refractoriness) up to 3 ms following a supramaximal stimulus, followed by a period of increased excitability (superexcitability) peaking at 5-7 ms and subsequently reduced excitability (subexcitability). The paired pulse paradigm stimulus protocol is inset.
Figure 2. Recovery cycle of excitability, demonstrating the characteristic sequence of excitability changes following impulse conduction, with a period of reduced excitability (refractoriness) up to 3 ms following a supramaximal stimulus, followed by a period of increased excitability (superexcitability) peaking at 5-7 ms and subsequently reduced excitability (subexcitability). The paired pulse paradigm stimulus protocol is inset.
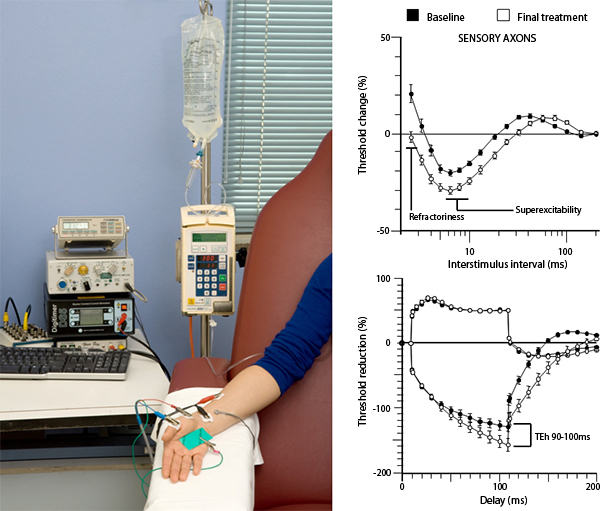 Figure 3. Excitability changes in sensory axons oxaliplatin-treated patients, with baseline recordings shown in black and post-treatment recordings shown in white, following 4-6 months of oxaliplatin treatment. These changes are thought to reflect widespread axonal damage and membrane potential change. A picture of the excitability set-up in the oncology setting is shown at left. Click here to view larger image.
Figure 3. Excitability changes in sensory axons oxaliplatin-treated patients, with baseline recordings shown in black and post-treatment recordings shown in white, following 4-6 months of oxaliplatin treatment. These changes are thought to reflect widespread axonal damage and membrane potential change. A picture of the excitability set-up in the oncology setting is shown at left. Click here to view larger image.
Discussion
Chemotherapy-induced neuropathy is a serious side effect of cancer treatment, which may affect treatment course and produce long-lasting patient disability. There is a lack of sensitive and objective assessment measures to specifically measure nerve dysfunction in chemotherapy treated patients. The clinical development of axonal excitability techniques has provided useful and predictive information for the assessment of chemotherapy-induced neurotoxicity. By providing information about ion channel function, resting potential, and axonal membrane function, these techniques enable insight into the pathophysiological processes underlying axonal dysfunction in cancer patients treated with chemotherapy. In addition, axonal excitability techniques have been demonstrated to be feasible in the clinical oncology setting, and a single test may be completed in 5-10 minutes.
In oxaliplatin-treated patients, axonal excitability techniques provide a sensitive biomarker which enables early identification of patients at risk of severe neurotoxicity. In comparison to conventional nerve conduction studies which identify oxaliplatin-induced nerve damage only after axonal loss has already occurred, axonal excitability studies provide predictive markers of nerve dysfunction prior to axonal loss. As such, axonal excitability studies may be utilised to provide assessment of nerve function in clinical trials of potential neuroprotective strategies, to objectively determine neuroprotective efficacy.
Disclosures
We have nothing to disclose.
References
- Hausheer FH, Schilsky RL, Bain S, Berghorn EJ, Lieberman F. Diagnosis, management, and evaluation of chemotherapy-induced peripheral neuropathy. Semin. Oncol. 2008;33:15–49. doi: 10.1053/j.seminoncol.2005.12.010. [DOI] [PubMed] [Google Scholar]
- Park SB, Krishnan AV, Lin CS, Goldstein D, Friedlander M, Kiernan MC. Mechanisms underlying chemotherapy-induced neurotoxicity and the potential for neuroprotective strategies. Curr. Med. Chem. 2008;15:3081–3094. doi: 10.2174/092986708786848569. [DOI] [PubMed] [Google Scholar]
- Park SB, Lin CS, Krishnan AV, Goldstein D, Friedlander ML, Kiernan MC. Long-term Neuropathy after Oxaliplatin Treatment: Challenging the Dictum of Reversibility? The Oncologist. 2012. Forthcoming. [DOI] [PMC free article] [PubMed]
- Postma TJ, Heimans JJ. Grading of chemotherapy-induced peripheral neuropathy. Ann. Oncol. 2000;11:509–513. doi: 10.1023/a:1008345613594. [DOI] [PubMed] [Google Scholar]
- Cascinu S, Catalano V, Cordella L, Labianca R, Giordani P, Baldelli AM, Beretta GD, Ubiali E, Catalano G. Neuroprotective effect of reduced gluthathione on oxaliplatin-based chemotherapy in advanced colorectal cancer: a randomized, double-blind, placebo-controlled trial. J. Clin. Oncol. 2002;20:3478–3483. doi: 10.1200/JCO.2002.07.061. [DOI] [PubMed] [Google Scholar]
- Lehky TJ, Leonard GD, Wilson RH, Grem JL, Floeter MK. Oxaliplatin-induced neurotoxicity: acute hyperexcitability and chronic neuropathy. Muscle Nerve. 2004;29:387–392. doi: 10.1002/mus.10559. [DOI] [PubMed] [Google Scholar]
- Bostock H, Cikurel K, Burke D. Threshold tracking techniques in the study of human peripheral nerve. Muscle Nerve. 1998;21:137–158. doi: 10.1002/(sici)1097-4598(199802)21:2<137::aid-mus1>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- Burke D, Kiernan MC, Bostock H. Excitability of human axons. Clin. Neurophysiol. 2001;112:1575–1585. doi: 10.1016/s1388-2457(01)00595-8. [DOI] [PubMed] [Google Scholar]
- Krishnan AK, Lin CS, Park SB, Kiernan MC. Axonal ion channels from bench to bedside: a translational neuroscience perspective. Prog. Neurobiol. 2009;89:288–313. doi: 10.1016/j.pneurobio.2009.08.002. [DOI] [PubMed] [Google Scholar]
- Park SB, Lin CS, Krishnan AV, Goldstein D, Friedlander M, Kiernan MC. Oxaliplatin-induced neurotoxicity: changes in axonal excitability precede development of neuropathy. Brain. 2009;132:2712–2723. doi: 10.1093/brain/awp219. [DOI] [PubMed] [Google Scholar]
- Park SB, Goldstein D, Lin CS, Krishnan AV, Friedlander ML, Kiernan MC. Acute abnormalities of sensory nerve function associated wtih oxaliplatin-induced neurotoxicity. J. Clin. Oncol. 2009;27:1243–1249. doi: 10.1200/JCO.2008.19.3425. [DOI] [PubMed] [Google Scholar]
- Krishnan AV, Goldstein D, Friedlander M, Kiernan MC. Oxaliplatin-induced neurotoxicity and the development of neuropathy. Muscle Nerve. 2005;32:51–60. doi: 10.1002/mus.20340. [DOI] [PubMed] [Google Scholar]
- Krishnan AV, Goldstein D, Friedlander M, Kiernan MC. Oxaliplatin and axonal Na+ channel function in vivo. Clin. Cancer Res. 2006;12:4481–4484. doi: 10.1158/1078-0432.CCR-06-0694. [DOI] [PubMed] [Google Scholar]


