Abstract
Background:
The evaluation of prosthetic valves is very difficult with two-dimensional transthoracic echocardiography alone. Doppler and color flow imaging as well as transesophageal echocardiography are more reliable to detect prosthetic valve dysfunction. However, Doppler study sometimes tends to be misleading due to the load-depending characteristics of peak and mean pressure gradients. The peak-to-mean pressure decrease ratio is a load-independent measure, which was previously used for the detecting and grading of aortic valve stenosis. We assessed the usefulness of this method for the evaluation of aortic valve prosthesis obstruction.
Methods:
One hundred fifty-four patients with aortic valve prostheses were included in this study. Transthoracic and transesophageal echocardiographic examinations were performed in all the patients. Peak velocity and velocity time integral of the aortic valve and left ventricular outflow tract, peak and mean aortic valve pressure gradients, peak-to-mean pressure gradient ratio, and time velocity integral (TVI) index were measured.
Results:
There was a significant relation between the TVI index (p value < 0.001) and aortic prosthesis obstruction. A TVI index < 0.2 had a sensitivity of 71% and specificity of 100% for the detection of aortic valve prosthesis obstruction. However, no significant relation was found between the peak-to-mean pressure ratio and aortic valve prosthesis obstruction (p value = 0.09).
Conclusion:
Although the peak-to-mean pressure gradient (PG/MG) ratio is a simple, quick, and load-independent method which may be useful for the grading of aortic valve stenosis, it is poorly associated with aortic valve prosthesis obstruction. The TVI index is a useful measure for the detection of aortic prosthesis obstruction.
Keywords: Aortic valve; Diagnosis; Echocardiography, Doppler
Introduction
The evaluation of prosthetic valves via two-dimensional (2D) transthoracic echocardiography (TTE) alone is very difficult. Doppler and color flow imaging as well as transesophageal echocardiography (TEE) are more reliable to detect prosthetic valve dysfunction.
The incidence of prosthetic valve obstruction has been estimated at 0.1% to 0.4% per year, depending on the valve size, type, and location as well as the adequacy of anticoagulation.1 Whereas the obstruction of a mitral mechanical prosthesis is caused more frequently by thrombus, the obstruction of an aortic mechanical prosthesis is created more frequently by pannus formation.2 When a prosthetic valve becomes obstructed, the motion of the disk, ball, or leaflets decreases. Be that as it may, it is difficult to visualize and yet more difficult to quantify the restriction of the excursion with TTE.3
TEE may be essential in the evaluation of mitral and tricuspid valves, but it is relatively low sensitive for detecting the dysfunction of aortic prostheses.3 Gross abnormalities such as large thrombi or vegetations can be identified using 2D echocardiography, but assessing the functional significance of such changes is difficult.4 Thus, most of the diagnostic information related to aortic prostheses depends on a thorough and quantitative Doppler study.4
The range of normal Doppler values depends primarily on the size of the prosthesis.4
It is important to remember that increased flow velocity itself does not always indicate prosthetic obstruction. The velocity can be increased without stenosis in a high output state or presence of severe prosthetic regurgitation.
The ratio of the left ventricular outflow tract (LVOT) to aortic valve prosthesis (AVP) velocity or time velocity integral (TVI) is helpful in differentiating increased flow velocity across an aortic prosthesis due to prosthetic obstruction (the ratio < 0.2) from increased velocity due to other causes (the ratio remains normal > 0.3).3 Recently, Chambers et al. reported that the relation of trans aortic peak (PG) and mean gradients (MG), i.e. the PG/MG ratio, is a useful parameter to evaluate the severity of aortic stenosis.5
The purpose of this study was to evaluate the statistical efficacy (sensitivity, specificity, positive and negative predictive values, and accuracy and probability rates in case of a positive or negative result) of the PG/MG ratio to predict aortic valve prosthesis obstruction and to compare it with the TVI ratio.
Methods
From February 2007 to January 2008, we retrospectively analyzed the Doppler echocardiograms of 154 consecutive patients (mean age: 49 years, range: 18–79 years, 52% male) with aortic valve prosthesis evaluated for several clinical indications.
The exclusion criteria were inadequate echocardiographic images, rhythm other than sinus rhythm, paravalvular regurgitation, aortic bioprosthesis, and significant mitral valve disease.
Echocardiographic examinations were performed with the subject in the left lateral decubitus position. Commercially available ultrasonography instruments equipped with 2.0 to 3.5-MHZ transthoracic probes and 2.0 MHz “non-imaging” (Pedoff) transducers were utilized from the left and right parasternal, apical, suprasternal, and sub-xyphoid windows (GE Medical Systems, Vivid 3). TEE was performed using a commercial 5.0-/3.5-MHz multi-plane probe. Complete 2D, M-mode, pulsed Doppler, continuous, and color studies were performed in all the patients in accordance with the recommendations of the American society of echocardiography.
Pulsed wave signal of the left ventricular outflow tract (LVOT) and continuous wave signal of the aortic valve (AV) prosthesis were obtained using the apical 5-chamber view, with the the sample volume placed 5 mm below the aortic annulus.
The following echocardiographic variables were measured and calculated from the average of 3-5 consecutive beats:
Peak velocity (Vmax)
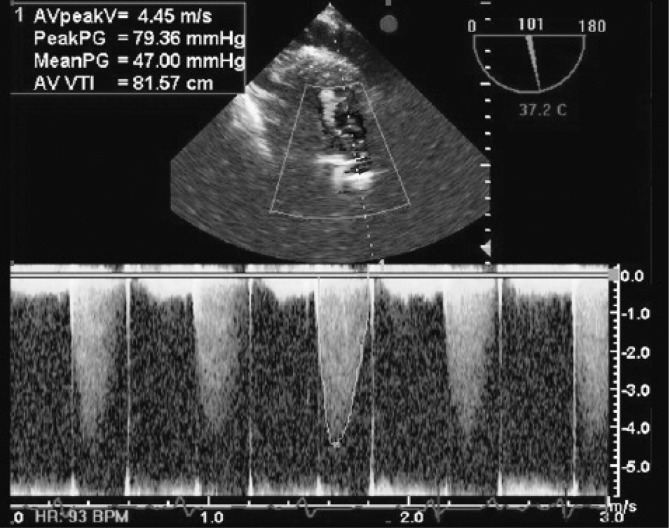
Peak gradient (PG) was calculated as 4 × (Vmax)2 and mean gradient (MG) with the algorithm incorporated to the ultrasound equipment (Figure 1)
Time velocity integral (TVI)
TVI index (LVOTTVI / AVTVI)
Figure 1.
Deep transgastric view of an obstructed aortic prosthesis. Continuous Doppler echocardiography showed significant increase in peak and mean pressure gradient through the aortic prosthesis
AV peak V, Aortic valve peak velocity; Peak PG, Peak pressure gradient; Mean PG, Mean pressure gradient; AV VTI, Aortic valve velocity time integral
TEE: aortic valve prosthesis was evaluated on 0, 45, and 120 degrees in the mid esophageal and in deep transgastric view for the detection of the thrombus or pannus formation.
Cinefluoroscopy was done in all the patients to assess the valve leaflet (s) motion. Cinefluoroscopy is superior to echocardiography in identifying disc motion, whilst Doppler study allowed the measurement of gradients and areas. A significant increase in trans-prosthesis pressure gradient along with a decreased TVI index through Doppler echocardiography and decreased leaflet (s) motion (more than 25 ± 5 degrees)6 using cinefluoroscopy was defined as prosthetic valve obstruction.
All the data are expressed as mean ± SD. Crude associations between the PG/MG ratio and the other variables were determined via the independent sample t-test and Mann-Whitney U test for the categorical data and bivariate linear regression models for the interval data. Multivariate analysis was performed using a multiple linear regression model to determine adjusted associations. A p value < 0.05 was considered statistically significant. SPSS 15 (SPSS Corporation, Chicago, Illinois, USA) was used for statistical analysis.
Results
The clinical and echocardiographic characteristics of the patients are summarized in Tables 1 and 2. Time to valve replacement surgery was 10±8 years (range from 1 to 36 years).
Table 1.
Patients’ characteristics and their comparisons in two groups of patients (n=154)
| Total (n=154)
|
AVP Obstruction
|
p value
|
||
|---|---|---|---|---|
| Yes (n=71)
|
No (n=83)
|
|||
| Age (y) (mean±SD) | 49±13.0 | 48±13.9 | 50±13.6 | 0.364 |
| Female/Male | 75/79 | 42/29 | 33/50 | 0.02 |
| Time from operation (y) (mean±SD) | 10±8.0 | 13.3±7.2 | 7±6.8 | <0.001 |
| Type of mechanical valve (%) | 0.011 | |||
| Mono-leaflet | 41 (26.6) | 21 (29.6) | 12 (14.5) | |
| Bi-leaflets | 113 (73.4) | 37 (70.4) | 60 (85.5) | |
| Referral reason (%) | 0.019 | |||
| AVR | 63 (40.9) | 22 (31) | 41 (49.4) | |
| AVP malfunction | 52 (33.8) | 29 (40.8) | 23 (27.7) | |
| Infective endocarditis | 13 (8.4) | 3 (4.2) | 10 (12.1) | |
| Cardiac source of systemic emboli | 22 (14.2) | 15 (21.2) | 7 (8.4) | |
| Syncope | 4 (2.7) | 2 (2.8) | 2 (2.4) | |
| LVEF (%) (mean±SD) | 45±10.0 | 48±9.8 | 43±12.5 | 0.072 |
AVR, Aortic valve replacement; AVP, Aortic valve prosthesis; LVEF, Left ventricular ejection fraction
Table 2.
Patients> Doppler echocardiographic findings*
| Total (n=154)
|
AVP Obstruction
|
p value
|
||
|---|---|---|---|---|
| Yes (n=71)
|
No (n=83)
|
|||
| AV peak velocity (m/s) | 2.90±1.5 | 3.40±2 | 2.50±0.60 | <0.001 |
| AV peak PG (mmHg) | 35±20 | 44.5±22.8 | 27±12.70 | <0.001 |
| AV mean PG (mmHg) | 20±14 | 25.2±14.2 | 16±13 | <0.001 |
| AV TVI (cm) | 50.70±18 | 58.3±19.9 | 43.90±13.70 | <0.001 |
| LVOT TVI (cm) | 20±7 | 20±7 | 20.20±7.10 | 0.79 |
| LVOT TVI / AV TVI | 0.43±0.15 | 0.37±0.14 | 0.48±0.15 | <0.001 |
| Normally functioning AV | 0.44±0.15 | 0.38±0.14 | 0.48±0.15 | <0.001 |
| Abnormal motion of AV | 0.33±0.13 | 0.30±0.10 | 0.51±0.15 | 0.18 |
| PG/MG ratio | 1.80±0.27 | 1.80±0.19 | 1.90±0.32 | 0.26 |
| Normally functioning AV | 1.80±0.33 | 1.80±0.17 | 1.90±0.32 | 0.85 |
| Abnormal motion of AV | 1.80±0.18 | 1.80±0.26 | 1.80±0.35 | 0.50 |
Data are presented as mean±SD
AV, Aortic valve; PG, Pressure gradient; TVI, Time velocity integral; LVOT, Left ventricular outflow tract; PG/MG ratio, The ratio of peak gradient to mean gradient; AVP, Aortic valve prosthesis
TEE showed thrombus, pannus, and mixed thrombus with pannus in 26.7%, 31%, and 12% of the patients, respectively. Nonetheless, cinefluoroscopy revealed decreased leaflet motion only in 7.8% of the patients.
There was an inverse correlation between the PG/MG ratio and MG (β = − 0.010, r = − 0.54, p value < 0.001), but there was no correlation between the PG/MG ratio and the TVI index (β = 0.09, r = 0.053; p value = 0.52). Additionally, there was a significant negative correlation between the PG/MG ratio and the Vmax. (β = − 0.03, r = − 0.165, p value = 0.04).
The logistic regression analysis showed no significant relation between the peak-to-mean pressure ratio and aortic valve prosthesis obstruction (B = 1.25, p value = 0.09, OR = 0.29, 95% CI: 0.07–1.23, but a significant relation was found between the TVI index and aortic valve prosthesis obstruction (B = 5.69, p value < 0.001, OR = 0.003, 95% CI: 0.0002–0.0490.
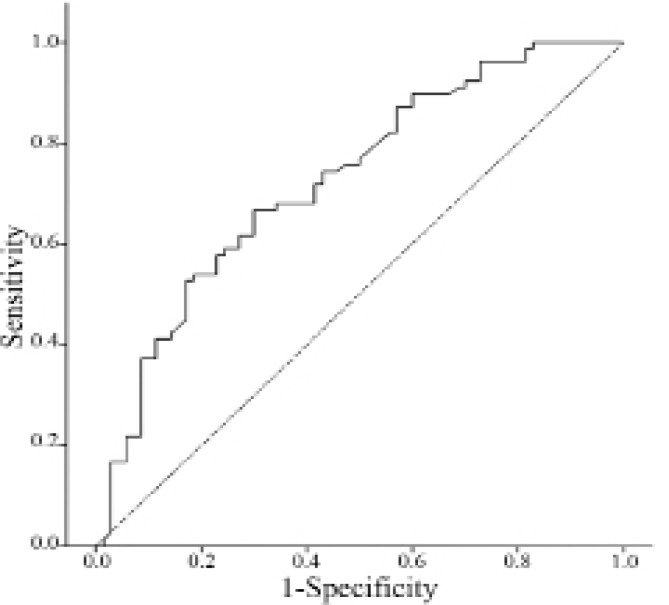
The receiver operating characteristic (ROC) curve showed that the TVI index was an accurate (AUC = 0.73 ± 0.041, 95% CI: 0.65–0.81) method for the evaluation of AVP obstruction (Figure 2). The VTI index<0.2 had a sensitivity of 71%, specificity of 100%, positive likelihood ratio of 100%, and negative likelihood ratio of 54.5% for the prediction of AVP obstruction.
Figure 2.
ROC curve of the TVI index for the diagnosis of aortic valve prosthesis obstruction according to fluoroscopy
The probability of obstruction was twice higher in the monoleaflet prosthesis in comparison with the bileaflet prosthesis (OR: 2.8, 95% CI: 0.15–0.79). Furthermore, aortic valve prosthesis obstruction was more frequent in the female gender (OR: 2.1, 95% CI: 0.24–0.89); it was not, however, affected by the patient’s age and time duration from valve surgery (table 3).
Table 3.
Logistic regression analysis between PG/MG ratio and multiple variables
| Coefficient
|
SE
|
PV
|
Odds Ratio
|
95% CI for OR
|
||
|---|---|---|---|---|---|---|
| Sex | −1.004 | 0.496 | 0.430 | 0.366 | 0.139 | 0.969 |
| Age | 0.001 | 0.017 | 0.938 | 1.001 | 0.969 | 1.034 |
| Time to surgery | 0.125 | 0.043 | 0.400 | 1.1133 | 1.041 | 1.233 |
| Valve Type | 0.570 | 0.709 | 0.422 | 1.768 | 0.440 | 7.096 |
| Valve Size | −0.072 | 0.099 | 0.468 | 0.930 | 0.766 | 1.131 |
| PG/MG ratio | −0.276 | 0.802 | 0.731 | 0.759 | 0.157 | 3.655 |
| TVI index | −5.318 | 1.830 | 0.004 | 0.005 | 0.000 | 0.177 |
| Constant | 2.357 | 3.016 | 0.435 | 10.560 | - | - |
PG, Peak pressure gradient; MG, Mean pressure gradient; TVI, Time velocity integral; SE, Standard error; PV, Probability value; CI, Confidence interval; OR, Odds ratio
Discussion
Obstruction of the AV prosthesis is an important clinical entity. It can occur by thrombus formation, pannus ingrowths, or infective endocarditis.
TTE has limited value for the evaluation of AVP obstruction3 and has a low sensitivity for the detection of its dysfunction.4 Whereas the detection of obstruction and assessment of the functional significance of obstruction is difficult by 2D echocardiography, Doppler study can help to evaluate AVP abnormality.4 Doppler study can help to diagnose AVP obstruction by measuring peak velocity, peak and mean pressure gradients, and TVI index, but load dependency can sometimes misguide physicians.
The peak-to-mean pressure ratio was previously used to evaluate aortic valve stenosis. This parameter is flow independent.7 Opinions about this variable is controversial. For example, Volbery et al. reported a weak correlation between the PG/MG ratio and aortic valve area.5 They found marked overlap in the PG/MG ratio values in patients with aortic stenosis of variable severity. The sensitivity, specificity, and accuracy of the PG/MG ratio for the diagnosis of severe stenosis in their study were fair. In a study by Chambers et al., this variable was shown to be related to the aortic valve area (1.75 in mild stenosis, 1.66 in moderate stenosis, 1.56 in severe stenosis and 1.57 in severe aortic stenosis with left ventricular ejection fraction less than 40%).5
In the present study, we assessed the usefulness of the PG/MG ratio as a parameter proposed for the diagnosis of AVP obstruction. This parameter has the advantage, compared to the other available ones, of being independent of flows such as Vmax, and MG, which represents and advantage over the indices that require flow correction. We compared the PG/MG ratio with Vmax MG and TVI index, which are the three criteria most often used for the diagnosis of AVP obstruction.
Using multiple statistical analysis methods, we did not find a significant relation between the PG/MG ratio and AVP obstruction; although the logistic regression method did not rule out this association strongly (p value = 0.09). We presumed that it might be secondary to the triangular shape of the CW Doppler flow profile in the aortic valve prosthesis, which would cause the prosthetic valve mean pressure gradient to not follow the classic formula (mean PG = 2.4 × V2). We, therefore, calculated the mean gradient mathematically by applying this formula and compared them with the previous automatically measured mean gradients. There was an insignificant difference between the automatically and mathematically derived measurements (16.5 versus 17.49 mmHg, respectively); nevertheless, the linear regression analysis showed a significant correlation between the two methods (correlation coefficient = 0.96, regression coefficient of mean pressure gradient = 0.918, p value < 0.001).
This study showed that the TVI index had a strong relation with AVP obstruction. Using several analysis methods, we found that the TVI index < 0.2 had a specificity of 100% for the prediction of significant obstruction. The PG/MG ratio had a low clinical impact for the diagnosis of AVP obstruction; be that as it may, further studies are required to evaluate the PG/MG ratio as a parameter for the diagnosis of AVP obstruction.
The greatest limitation of this study is that the criteria for AVP obstruction, considered to be “standard”, Vmax, MG, and TVI index, are all parts of the PG/MG ratio; consequently, there is contamination between the parameters. This limitation is also shared by Chambers and Volberg et al. Another limitation is the lack of direct anatomic confirmation at surgery or post-mortem examinations of abnormalities such as thrombus or pannus. Furthermore, we did not follow the patients during a long-term period, so the clinical relevance of the non-invasive abnormalities needs to be established.
Conclusion
The PG/MG ratio is a simple, quick, and load-independent method, but the present study showed that the PG/MG ratio correlated weakly with the AVP obstruction. Although this correlation was insignificant, it was not ruled out strongly. There was also a marked overlap between the PG/MG ratio values among patients with AVP obstruction of variable severities. The sensitivity, specificity, and accuracy of the PG/MG ratio for the diagnosis of AVP obstruction were fair. In the population studied, the predictive values of the PG/MG ratio for the diagnosis of AVP obstruction were modest (0.09). Moreover, the analysis of the probability rates in the case of a positive or negative result showed that the PG/MG ratio had a low clinical impact for the diagnosis of AVP obstruction. Finally, we found the TVI index a useful measure for detecting aortic prosthesis obstruction.
Acknowledgments
This study was supported by Iran University of Medical Sciences. We wish to thank all the nursing staff involved in the echocardiography and angiography departments at Shaheed Rajaei Cardiovascular, Medical and Research Center.
References
- 1.Cannegieter SC, Torn M, Rosendual FR. Oral anticoagulant treatment in patients with mechanical heart valves: how to reduce the risk of thromboembolic and bleeding complications. J Inter Med. 1999;245:369–374. doi: 10.1046/j.1365-2796.1999.00460.x. [DOI] [PubMed] [Google Scholar]
- 2.Girad SE, Miller FA, Jr, Orszulak TA, Mullany CJ, Montgomery S, Edwards WD, Tazelaar HD, Malouf JF, Tajik AJ. Reoperation for prosthetic aortic valve obstruction in the era of echocardiography: trends in diagnostic testing and comparison with surgical findings. J Am Coll Cardiol. 2001;37:579–584. doi: 10.1016/s0735-1097(00)01113-x. [DOI] [PubMed] [Google Scholar]
- 3.OH Jk, Seward JB, Tajik AJ. Prosthetic valve evaluation. In: OH Jk, Seward JB, Tajik AJ., editors. The Echo Manual. 3rd ed. Philadelphia, Baltimore, New york, London, Buenos Aires, Hong Kong, Sydney, Tokyo: Lippincott Williams & Wilkins; 2007. pp. 226–242. [Google Scholar]
- 4.Feigenbaum H, Armstrong W, Ryan T. Prosthetic valves. In: Feigenbaum H, Armstrong W, Ryan T, editors. Feigenbaum’s Echocardiography. 6th ed. Philadelphia, Baltimore, New york, London, Buenos Aires, Hong Kong, Sydney, Tokyo: Lippincott Williams & Wilkins; 2005. pp. 399–436. [Google Scholar]
- 5.Chambers J, Rajani R, Hankins M, Cook R. The peak to mean pressure decrease ratio: a new method of assessing aortic stenosis. J Am Soc Echocardiogr. 2005;18:674–678. doi: 10.1016/j.echo.2004.09.028. [DOI] [PubMed] [Google Scholar]
- 6.Cianciulli TE, Lax JA, Beck MA, Cerruti FE, Gigena GE, Saccheri MC, Fernández E, Dorelle AN, Leguizamón JH, Prezioso HA. Cinefluoroscopic assessment of mechanical disc prostheses: its value as a complementary method to echocardiography. J Heart Valve Dis. 2005;14:664–673. [PubMed] [Google Scholar]
- 7.Volberg VI, Berensztein CS, Ber MG, Lanosa G, Lerman J, Pineiro DJ. Efficacy of the peak to mean pressure decrease ratio for the assessment of aortic stenosis severity. Rev Argent Cardiol. 2006;74:123–128. [Google Scholar]