Abstract
Background
Discharge against medical advice (DAMA) is a relatively common problem worldwide. We sought to determine the prevalence of and reasons for DAMA among inpatients of our cardiac center.
Methods:
From a total of 20289 discharges from our cardiac teaching hospital, 992 (4.9%) patients at a minimum age of 18 years were cases of DAMA. After excluding 49 cases due to missing data, we retrospectively analyzed our prospectively collected data from 943 patients, who were DAMA cases. Patients’ characteristics, including demographic details, reason for discharge, insurance status, and length of stay before discharge, were examined.
Results:
The mean age of the study patients was 60.7 ± 13.0 (range, 18–94 years) with a male-to-female ratio of 2.1/1. Lack of consent to surgery or other invasive procedures was the reason cited for DAMA in 31% of the patients, followed by personal or family issues (17%). No reason for DAMA was reported in 26 (2.8%) of the patients. Women compared to men were more likely to cite “lack of consent to surgery or invasive procedures” as the reason for DAMA (p value = 0.005), whereas men more prevalently stated “personal or family issues” as the reason for DAMA (18.7% vs. 12.7%, p value = 0.022).
Conclusion:
The most frequent self-reported reason for DAMA in our cardiac patients was lack of consent to surgery or invasive procedures. This may be because of fear of undergoing invasive procedures such as revascularization. Explaining the stages of a given invasive procedure to patients and comparing its risks versus benefits may lessen impulsive decision-making and DAMA.
Keywords: Patient discharge, Heath care surveys, Heart diseases, Iran
Introduction
The instance of a patient already in hospital wishing to leave against clinicians’ advice is referred to as self-discharge or discharge against medical advice (DAMA). DAMA is a relatively common problem of health care systems, accounting for as many as 2% of all hospital discharges.1, 2 Because lengths of stay (LOS) are commonly several days, these patients often remain acutely ill at the time of self-discharge, and they may remain exposed to the risk of inappropriately treated medical problem, resulting in the need for readmission.3–5 It is not surprising that DAMA poses a major problem for many clinicians who treat inpatients,6, 7 particularly those with heart trouble because incomplete therapy in conditions such as ischemic heart disease may exert a negative impact on health outcome. Additionally, consequent care will be probably associated with more challenges and higher overall costs over time.8, 9 Avoiding DAMA is, thus, likely to be beneficial for both patients and health systems.
DAMA occurs for a variety of reasons.10, 11 Green et al. found that the majority of the their DAMA cases were in consequence of personal reasons, financial problems, and legal issues such as a court date.11 A good understanding of patients’ reasons for DAMA may assist health care providers in averting some of these premature discharges.
Patients’ consideration of DAMA may be influenced by race/ethnicity and cultural factors or other contextual factors, including differences in the health care system, relationship between primary care physicians and hospital-based physicians, insurance coverage, and styles of communication between physicians and patients.7 While there are several studies available from dominantly western countries regarding the prevalence of DAMA,7 to the best of our knowledge, there is only one study on DAMA among emergency-admitted patients in Iran,12 and no such published data exist in hospitalized patients. We, therefore, sought to determine the prevalence of and also the reasons for DAMA in an Iranian sample of cardiac patients.
Methods
Between September 2008 and November 2009, this study was conducted over a 14-month period at Tehran Heart Center, a major referral and educational hospital dedicated to cardiac patients and affiliated to Tehran University of Medical Sciences. Tehran Heart Center comprises 4 intensive care units (ICUs) (74 beds), 5 cardiac care units (CCUs) (72 beds), 7 post-CCUs) (178 beds), and 5 surgical wards (120 beds) and boasts full-time accomplished specialists, well-trained nurses, and state-of-the-art diagnostic and therapeutic equipment. The center provides diagnostic and treatment services at much lower costs than do hospitals in the private sector. The hospital has considerable patient loads from Tehran (capital city) and other large and small cities and towns. On average, 8500 coronary angiographic procedures, 3500 surgical operations, and 1500 percutaneous coronary intervention (PCI) procedures are performed in this hospital per annum.
We identified 20289 discharges of consecutive hospitalized patients at a minimum age of 18 years after excluding the patients who had expired in the hospital (n = 342). Of these, 992 patients were cases of DAMA. After the exclusion of those with missing data (n = 49), the remaining 943 patients formed the study population.
According to the policies of Tehran Heart Center, a request for DAMA is considered only when a related form is completed and signed by the patient or his/her legal custodian. The “DAMA form” was designed on the basis of the reasons cited by patients in the past for self-discharge and the potential reasons reported in prior studies. A list of reasons are provided in this form including lack of consent to surgery or invasive procedures, personal or family issues, feeling well, financial problems, transfer to another hospital, no noticeable improvements, requesting temporary leave from hospital stay during public or extended holidays, dissatisfaction with hospital services/facilities, seeking consultation elsewhere, delay in the delivery of health care services, dissatisfaction with the staff’s behavior, and other reasons. Patients should then list, in order of importance, the reason(s) for DAMA. In case patients cite more than one reason for DAMA, the principal reason is considered the one appearing first on the list. Other data are filled out by the nursing staff.
In the present study, data on the discharge dates, reason(s) provided for DAMA by the patients, hospitalization ward, and the patients’ file numbers were obtained from these forms. These data were thereafter merged with the hospital registration database using the patients’ file number to obtain the other variables of the patients, including insurance status, demographic characteristics, and LOS before DAMA. Demographic information was comprised of such biological characteristics as age, gender, and race/ethnicity. Insurance status was categorized as uninsured, Social Security Organization (SSO), Medical Service Insurance Organization (MSIO), complementary insurance, and others. Finally, the prospectively collected data were analyzed.
The data are presented as mean ± SD (standard deviation) for the quantitative variables and are summarized by absolute frequencies and percentages for the categorical variables. The categorical variables were compared using the two-sided Pearson chi-square test or the Fisher exact test (as appropriate). The continuous variables were compared using the student t-test or nonparametric Mann-Whitney U test when the presumption of normality was disrupted by the Kolmogorov-Smirnov test.
For the statistical analyses, the statistical software SPSS version 16.0 for Windows (SPSS Inc., Chicago, IL) was employed. All the p values were two-tailed, with statistical significance defined by a p value ≤ 0.05.
Results
Over the 14-month study period, there were 20289 discharges, of which 992 (4.9%) were cases of DAMA. Analysis was conducted in 943 patients after the exclusion of 49 patients due to missing data. Modes of admission were the emergency department in 380 (40.3%) patients, hospital transfer in 13 (1.4%), and routine or elective in 550 (58.3%). The most prevalent type of procedure cited by the study population as the principal reason for DAMA was cardiac surgery (54%), followed by PCI (15.4%), and coronary angiography (11.5%). Medical therapy was recommended in the remaining 180 patients with DAMA (19.1%).
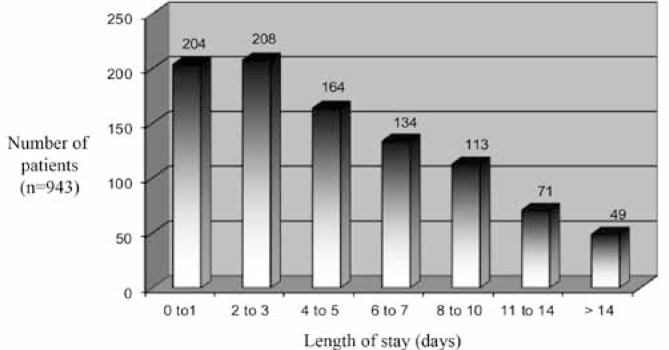
The baseline characteristics of the DAMA cases, for men and women separately, are depicted in Table 1. The mean age of the study patients was 60.7 ± 12.0 (range = 18–94 years) with a male-to-female ratio of 643/300. Nearly one third of the study patients were in the age group of 61–70 years. The most common age group was 51–60 years in the men and 61–70 years in the women. In our DAMA cases, the male patients were younger and more educated than were the female patients. As is shown in Table 1, the mean LOS in hospital was 5.5 ± 5.3 days for the whole population (range = 1–55 days), and over 60% of the patients had stayed for 5 days or less prior to DAMA. This variable was significantly different between the men and women (5.1 ± 4.7 vs. 6.3 ± 6.4, p value = 0.002). There was no statistically significant difference between the men and women with regard to the other baseline variables. Figure 1 demonstrates the frequency distribution of LOS in hospital before DAMA.
Table 1.
Baseline characteristics of the study population stratified by gender*
| All (n=943) | Men (n=643) | Women (n=300) | P value** | |
|---|---|---|---|---|
| Age (y) | 60.68±13.00 | 59.56±13.08 | 63.08 ±12.51 | <0.001 |
| Age category (y) | <0.001 | |||
| 18–40 | 57 (6.0) | 41 (6.4) | 16 (5.3) | |
| 41–50 | 157 (16.6) | 121 (18.8) | 36 (12.0) | |
| 51–60 | 222 (23.5) | 172 (26.7) | 50 (16.7) | |
| 61–70 | 275 (29.2) | 162 (25.2) | 113 (37.7) | |
| 71–80 | 192 (20.4) | 119 (18.5) | 73 (24.3) | |
| > 80 | 40 (4.2) | 28 (4.4) | 12 (4.0) | |
| Education (y) | 7.46±5.70 | 8.75±5.50 | 4.66±5.09 | <0.001 |
| LOS before self-discharge (d) | 5.49±5.31 | 5.13±4.69 | 6.27±6.39 | 0.002 |
| Marital status | 0.772 | |||
| Single | 109 (11.6) | 73 (11.4) | 36 (12.0) | |
| Married | 834 (88.4) | 570 (88.6) | 264 (88.0) | |
| Domicile | 0.205 | |||
| Tehran city | 662 (70.2) | 438 (68.1) | 224 (74.7) | |
| Tehran province | 115 (12.2) | 86 (13.4) | 29 (9.7) | |
| Neighboring provinces | 88 (9.3) | 64 (10.0) | 24 (8.0) | |
| Other provinces | 78 (8.3) | 55 (8.6) | 23 (7.7) | |
| Ethnicity | 0.234 | |||
| Fars | 598 (63.4) | 418 (65.0) | 180 (60.0) | |
| Tork | 155 (16.4) | 95 (14.8) | 60 (20.0) | |
| Shomali | 118 (12.5) | 80 (12.4) | 38 (12.7) | |
| Other | 72 (7.6) | 50 (7.8) | 22 (7.3) | |
| Health insurance | 907 (96.2) | 615 (95.6) | 297 (97.3) | 0.207 |
| SSO | 438 (48.3) | 301 (48.9) | 137 (46.9) | |
| MSIO | 392 (43.2) | 262 (42.6) | 130 (44.5) | |
| Others | 77 (8.5) | 52 (8.5) | 25 (8.6) | |
| Complementary health insurance | 155 (16.4) | 96 (14.9) | 59 (19.7) | 0.068 |
| Hospital ward | 0.065 | |||
| CCU | 197 (20.9) | 122 (19.0) | 75 (25.0) | |
| Post-CCU | 616 (65.3) | 435 (67.7) | 181 (60.3) | |
| Surgery | 130 (13.8) | 86 (13.4) | 44 (14.7) |
Data are presented as mean±SD or n (%)
P values for men vs. women
LOS, Length of stay; SSO, Social security organization; MSIO, Medical service insurance organization; CCU, Cardiac care unit
Figure 1.
Frequency distribution of length of stay in hospital before self-discharge
Reasons given for DAMA as stated by the patients or their companions are listed in Table 2. The most frequently cited reason was lack of consent to surgery or other invasive procedures (31%), followed by personal or family issues (17%). The next three most commonly reasons stated for DAMA were feeling well (13%), financial problems (11%), and desire to be transferred to another hospital (10%). No reason for DAMA was reported in 26 (2.8%) of the patients. The women compared to the men were more likely to cite “lack of consent to surgery or invasive procedures” as the reason for self-discharge (p value = 0.005), whereas the men more prevalently stated “personal or family issues” as the reason for DAMA (18.7% vs. 12.7%, p value = 0.022).
Table 2.
Self-reported reasons by the 943 hospitalized cardiac patients for leaving the hospital against medical advice*
| All (n=943) | Men (n=643) | Women (n=300) | P value** | |
|---|---|---|---|---|
| Lack of consent to surgery or invasive procedures | 290 (30.8) | 179 (27.8) | 111 (37.0) | 0.005 |
| Personal or family issues | 158 (16.8) | 120 (18.7) | 38 (12.7) | 0.022 |
| Feeling well | 122 (12.9) | 86 (13.4) | 36 (12.0) | 0.558 |
| Financial problems | 105 (11.1) | 75 (11.7) | 30 (10.0) | 0.449 |
| Desire to be transferred to another hospital | 95 (10.1) | 69 (10.7) | 26 (8.7) | 0.327 |
| No noticeable improvements | 56 (5.9) | 34 (5.3) | 22 (7.3) | 0.216 |
| Requesting temporary leave from hospital stay during public or extended holidays | 27 (2.9) | 18 (2.8) | 9 (3.0) | 0.863 |
| No reason mentioned | 26 (2.8) | 20 (3.1) | 6 (2.0) | 0.322 |
| Dissatisfaction with hospital services/facilities | 22 (2.3) | 12 (1.9) | 10 (3.3) | 0.165 |
| Seeking consultation elsewhere | 13 (1.4) | 9 (1.4) | 4 (1.3) | 0.999 |
| Delay in delivery of health care services | 8 (0.8) | 7 (1.1) | 1 (0.3) | 0.447 |
| Dissatisfaction with the staff’s behavior | 7 (0.7) | 3 (0.5) | 4 (1.3) | 0.218 |
| Other reasons | 14 (1.5) | 11 (1.7) | 3 (1.0) | 0.566 |
Data are presented n (%)
P values for men vs. women
Eighty-three (8.8%) patients cited more than one reason for opting for DAMA. The most common second reasons for DAMA were personal or family issues (29%), financial problems (18%), feeling well (15%), and desire to be transferred to another hospital (15%).
Among the 943 DAMA cases in the analysis, 183 (19.4%) were readmitted within the study period: 95 (51.9%) of them returned to the hospital within 15 days, 73 (39.9%) within 16–90 days, and the remaining 15 (8.2%) more than 90 days following DAMA. The mean time interval to readmission was 32.8 days in this subgroup; the interval to readmission was 18.0 days longer for the women than that for the men (45.8 vs. 27.8 days, p value = 0.028).
Discussion
DAMA creates a challenge for physicians and other health care providers, in part due to the association of premature self-discharge with multiple readmissions. As is reported in the literature, DAMA has been a universal problem for more than half a century troubling both general medicine and psychiatric hospitals. However, most of the early studies were performed on the psychiatric patients in the USA.13, 14
The present study found a DAMA rate of 4.9%. This rate is similar to that reported among hospitalized patients with asthma4 but higher than that for medical admissions (typically less than 4%).15 Yet, it is lower than the rate among patients hospitalized for human immunodeficiency virus (HIV) infections (13%),16 substance abuse (23%),17 and psychiatric problems (typically more than 20%).18 Based on the patient population and the type of therapy, the rate of DAMA differs widely, and as was previously suggested by Baptist et al.,4 patients with chronic medical conditions may be at a higher risk for DAMA.
In line with earlier studies,10, 19, 20 our DAMA cases were more frequently men. Higher involvement of the 61–70-year-old age group in this study could be explained by the nature of cardiac diseases, which are more common in the elderly.
Exploring the reasons for DAMA, we observed a reasonable number of forms (2.8%) that had no reason documented. Contrary to a previous report from a general hospital,21 our analysis of the reasons stated by our DAMA cases revealed that a medical factor (reluctance to undergo an invasive therapeutic procedure), rather than social factors (e.g., personal or family issues), was the most common reason for DAMA among the study population. One reason for that could be the different study groups with different cultures and backgrounds. The fact that reluctance to undergo an invasive therapeutic procedure was the most frequent reason for DAMA may be due to the patients’ fear of undergoing such invasive procedures as revascularization. Explaining the stages of a given invasive procedure and its risks and benefits to patients may reduce impulsive decision-making and DAMA by such patients.
Chiming in with some previously conducted research,10, 20, 22 we found that financial problems were among the major reasons for DAMA. There are also some reports that hospital stays may be longer than it is necessary regardless of the severity of illness and without necessarily influencing the patient’s outcome.23, 24 Therefore, longer LOS may be a contributing factor for increasing the rate of DAMA in the patients with a desire to do so.25 We, however, observed a mean LOS of 5.5 days and more than 60% of our cases requested DAMA within 5 days. This may be due to the fact that such patients are much less likely to be transferred or to undergo cardiac procedures such as revascularization.
Another reason for DAMA on the part of patients is disagreement with the physician’s judgment of their health status. In our study, 12.9% of the patients cited feeling well as the reason to leave the hospital, which is far less than that reported by another Iranian study on patients admitted to the emergency department.12
Reducing the rates of DAMA requires, first and foremost, an awareness of patients’ rationales for taking this particular route. In this study, five factors that contributed to our patients’ opting for DAMA were lack of consent to surgery or other invasive procedures, personal or family issues, feeling well, financial problems, and desire to be transferred to another hospital. We found that many of our patients had decided on DAMA in order to refuse invasive procedures.
The concept of respect is of great importance in the Iranian culture. Iranian physicians are liable to deem it disrespectful if patients ask too many questions or doubt their professional opinions. On the other hand, many patients feel that a second professional opinion will enable them to make a better informed decision about their course of treatment. In our experience, Iranian heart specialists and surgeons are less likely to take the time to explain the reason for procedures to their patients. This ineffective physician-patient communication more often than not, leaves the patient with insufficient information about his or her illness and its treatment modalities; hence the fear of the medical procedures on the part of the patient. This may in part explain why so many patients refuse to be subjected to invasive procedures.
The main limitation of this study is the lack of a control group to compare DAMA patients with those who are discharged normally. The comparisons between men and women are also undercut by the absence of multivariable adjustment and a denominator: without knowing the denominator, it is not possible to know whether sex-related differences in DAMA reflect true differences by sex or simply the characteristics of the patients admitted. Still, similar to the USA, the mean age of Iranian cardiac patients is higher among women than among men, which reflects the earlier age of heart disease onset in men.26 This may explain why the female DAMA cases were older than their male counterparts in our study population. The current study has three other limitations of note as well. First, using self-report forms is often biased due to a tendency among people to give socially desirable answers. To address this inherent shortcoming, we asked the patients or their companions to complete the form only minutes before they left the hospital so that a patient dissatisfied with the care provided by the hospital would not worry about the possibility of the staff regarding him or her as ungrateful. Second, we were unable to follow up all the patients to determine the outcome of DAMA, i.e. whether they were re-admitted to our hospital or other hospitals or whether they died. And finally, some of the reasons cited for DAMA by our patient population, e.g. transfer to another hospital or seeking consultation elsewhere, seem to overlap with the others.
It is deserving of note that although all the patients were from a single center, the conclusions of the present study may be generalizable to other hospitals in Iran because ours is a tertiary referral centre receiving patients from all over the country.
Conclusion
The most frequent self-reported reasons for DAMA in a sample of Iranian cardiac patients included lack of consent to surgery or invasive procedures, personal or family issues, and feeling well, respectively. Providing strategies for decreasing the rate of DAMA by analyzing the current circumstances and developing effective interventions may benefit both patients (improving their health) and health care systems (decreasing unnecessary readmissions). We believe that qualitative research (e.g. semi-structured interviews with patients and perhaps physicians and hospital staff) is likely to be beneficial.
Acknowledgments
This study was supported by Tehran Heart Center, affiliated to Tehran University of Medical Sciences. We wish to thank the surgery data base group at Tehran Heart Center for its support.
References
- 1.Ibrahim SA, Kwoh CK, Krishnan E. Factors associated with patients who leave acute-care hospitals against medical advice. Am J Public Health. 2007;97:2204–2208. doi: 10.2105/AJPH.2006.100164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saitz R, Ghali WA, Moskowitz MA. The impact of leaving against medical advice on hospital resource utilization. J Gen Intern Med. 2000;15:103–107. doi: 10.1046/j.1525-1497.2000.12068.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hwang SW, Li J, Gupta R, Chien V, Martin RE. What happens to patients who leave hospital against medical advice? CMAJ. 2003;168:417–420. [PMC free article] [PubMed] [Google Scholar]
- 4.Baptist AP, Warrier I, Arora R, Ager J, Massanari RM. Hospitalized patients with asthma who leave against medical advice: characteristics, reasons, and outcomes. J Allergy Clin Immunol. 2007;119:924–929. doi: 10.1016/j.jaci.2006.11.695. [DOI] [PubMed] [Google Scholar]
- 5.Fiscella K, Meldrum S, Barnett S. Hospital discharge against advice after myocardial infarction: deaths and readmissions. Am J Med. 2007;120:1047–1053. doi: 10.1016/j.amjmed.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 6.Taqueti VR. Leaving against medical advice. N Engl J Med. 2007;357:213–215. doi: 10.1056/NEJMp078046. [DOI] [PubMed] [Google Scholar]
- 7.Alfandre DJ. “I’m going home”: discharges against medical advice. Mayo Clin Proc. 2009;84:255–260. doi: 10.4065/84.3.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Udvarhelyi IS, Goldman L, Komaroff AL, Lee TH. Determinants of resource utilization for patients admitted for evaluation of acute chest pain. J Gen Intern Med. 1992;7:1–10. doi: 10.1007/BF02599092. [DOI] [PubMed] [Google Scholar]
- 9.Pennycook AG, McNaughton G, Hogg F. Irregular discharge against medical advice from the accident and emergency department--a cause for concern. Arch Emerg Med. 1992;9:230–238. doi: 10.1136/emj.9.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Akiode O, Musa AA, Shonubi AM, Salami BA, Oyelekan AA. Trends of discharges against medical advice in a suburban surgical practice in Nigeria. Trop Doct. 2005;35:51–52. [PubMed] [Google Scholar]
- 11.Green P, Watts D, Poole S, Dhopesh V. Why patients sign out against medical advice (AMA): factors motivating patients to sign out AMA. Am J Drug Alcohol Abuse. 2004;30:489–493. doi: 10.1081/ada-120037390. [DOI] [PubMed] [Google Scholar]
- 12.Shirani F, Jalili M, Asl-E-Soleimani H. Discharge against medical advice from emergency department: results from a tertiary care hospital in Tehran, Iran. Eur J Emerg Med. 2010;17:318–321. doi: 10.1097/MEJ.0b013e3283334ef1. [DOI] [PubMed] [Google Scholar]
- 13.Daniels RS, Margolis PM, Carson RC. Hospital discharges against medical advice. I. Origin and prevention. Arch Gen Psychiatry. 1963;8:120–130. doi: 10.1001/archpsyc.1963.01720080010003. [DOI] [PubMed] [Google Scholar]
- 14.Schlauch RW, Reich P, Kelly MJ. Leaving the hospital against medical advice. N Engl J Med. 1979;300:22–24. doi: 10.1056/NEJM197901043000106. [DOI] [PubMed] [Google Scholar]
- 15.Smith DB, Telles JL. Discharges against medical advice at regional acute care hospitals. Am J Public Health. 1991;81:212–215. doi: 10.2105/ajph.81.2.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anis AH, Sun H, Guh DP, Palepu A, Schechter MT, O’Shaughnessy MV. Leaving hospital against medical advice among HIV-positive patients. CMAJ. 2002;167:633–637. [PMC free article] [PubMed] [Google Scholar]
- 17.Armenian SH, Chutuape MA, Stitzer ML. Predictors of discharges against medical advice from a short-term hospital detoxification unit. Drug Alcohol Depend. 1999;56:1–8. doi: 10.1016/s0376-8716(99)00027-7. [DOI] [PubMed] [Google Scholar]
- 18.Dalrymple AJ, Fata M. Cross-validating factors associated with discharges against medical advice. Can J Psychiatry. 1993;38:285–289. doi: 10.1177/070674379303800411. [DOI] [PubMed] [Google Scholar]
- 19.Ohanaka EC. Discharge against medical advice. Trop Doct. 2002;32:149–151. doi: 10.1177/004947550203200310. [DOI] [PubMed] [Google Scholar]
- 20.Nasir AA, Babalola OM. Clinical spectrum of discharges against medical advice in a developing country. Indian J Surg. 2008;70:68–72. doi: 10.1007/s12262-008-0018-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duno R, Pousa E, Sans J, Tolosa C, Ruiz A. Discharge against medical advice at a general hospital in Catalonia. Gen Hosp Psychiatry. 2003;25:46–50. doi: 10.1016/s0163-8343(02)00253-0. [DOI] [PubMed] [Google Scholar]
- 22.Okoromah CN, Egri-Qkwaji MT. Profile of and control measures for paediatric discharges against medical advice. Niger Postgrad Med J. 2004;11:21–25. [PubMed] [Google Scholar]
- 23.DeCoster C, Roos NP, Carriere KC, Peterson S. Inappropriate hospital use by patients receiving care for medical conditions: targeting utilization review. CMAJ. 1997;157:889–896. [PMC free article] [PubMed] [Google Scholar]
- 24.Kalant N, Berlinguet M, Diodati JG, Dragatakis L, Marcotte F. How valid are utilization review tools in assessing appropriate use of acute care beds? CMAJ. 2000;162:1809–1813. [PMC free article] [PubMed] [Google Scholar]
- 25.Katayama Y, Terashi A, Shimizu J, Suzuki S, Kashiwagi F, Kamiya T, Ashida S. Role of platelets as a factor aggravating cerebral ischemia. Jpn Circ J. 1990;54:1511–1516. doi: 10.1253/jcj.54.12_1511. [DOI] [PubMed] [Google Scholar]
- 26.Karimi A, Marzban M, Movahedi N, Salehiomran A, Sadeghian S, Goodarzynejad H. Traditional cardiac risk factors profile in Iranian patients undergoing coronary artery bypass surgery. Acta Cardiol. 2009;64:371–377. doi: 10.2143/AC.64.3.2038024. [DOI] [PubMed] [Google Scholar]