Abstract
Background
Socioeconomically disadvantaged women are at greater risk for gestational weight gain and postpartum weight retention compared to socioeconomically advantaged women. This study examines the effect of gestational weight gain on body mass index (BMI) transitions 5 years after pregnancy in socioeconomically disadvantaged women.
Methods
Gestational weight gain was assessed in 2136 postpartum women participating in the Fragile Families and Child Well-being study who experienced full-term, singleton gestations. Longitudinal BMI transitions were defined as a change or stability in BMI category between two time points: BMI before the index pregnancy and BMI 5 years after the index pregnancy. Logistic regression models estimated the association between gestational weight gain and longitudinal BMI transitions, controlling for health before the index pregnancy, pregnancy history, and sociodemographic characteristics.
Results
Excessive gestational weight gain was related to transitioning to a higher BMI category 5 years after the index pregnancy. Compared to white women, black and Hispanic women were more likely to transition or maintain a higher BMI category. Pregnancy history (i.e., parity at index pregnancy, interim pregnancy) and public assistance participation were associated with transitioning to a higher BMI category.
Conclusions
Among socioeconomically disadvantaged women, excessive gestational weight gain is related to transitioning to, but not maintaining, a higher weight category 5 years after the index pregnancy. Black and Hispanic women who are also socioeconomically disadvantaged and overweight or obese before conception may benefit from preconception or postpartum counseling about the long-term effect of gaining excessive weight during pregnancy and in the years immediately after childbirth.
Introduction
In 2007–2008, 64% of all U.S. women were overweight or obese (with 36% being obese). Among reproductive-aged women between the ages of 20 and 39, 34% were obese in 2007–2008 compared to 28% in 1999–2000.1 Consequently, more women are entering pregnancy overweight or obese; 53% of women enter pregnancy overweight, and 48% of women gain greater amounts of weight than recommended by the Institute of Medicine (IOM).2 Overweight and obese women are at greater risk of retaining gestational weight or gaining more weight after pregnancy compared to women with normal body mass indices (BMI).3,4 Retention of gestational weight or gaining of additional weight places obese women at greater risk for further negative health consequences associated with obesity, such as diabetes, high blood pressure, high cholesterol levels, asthma, and arthritis.5
The high rates of obesity among socioeconomically disadvantaged women and black and Hispanic women place these women at greater risk for gaining excessive weight during pregnancy and retaining the weight compared to socioeconomically advantaged women and white women.5–7 Among a sample of low-income women, women with excessive gestational weight gain are at greater risk of retaining gestational weight and gaining more weight 1 year postpartum.8,9 Further, black women are more likely to retain greater amounts of weight after pregnancy compared to white women regardless of socioeconomic status (SES).10,11
The research on gestational weight gain and postpartum weight retention recognizes that excessive weight gain during pregnancy is associated with being heavier in both the short term (<2 years postpartum) and long term (2 years postpartum).12 However, most of this research has focused on white and black women and women who are socioeconomically advantaged; fewer studies have focused on gestational weight gain and weight development 5 years after pregnancy among socioeconomically disadvantaged and ethnic minority samples of women that include Hispanic women.13 Including Hispanic samples of women in studies is especially important considering that more than half of the growth in the U.S. population between 2000 and 2010 was related to the increase in the Hispanic population.14 Further, studies have focused on the association between gestational weight gain and long-term weight gain or prevalence of overweight/obesity. The association between gestational weight gain and weight maintenance over time has rarely been investigated.
Using a sample of socioeconomically disadvantaged and predominantly black and Hispanic women, the current study explores the relationship of gestational weight gain and maternal BMI transitions 5 years after the index pregnancy. Specifically, the study controls for health before pregnancy, pregnancy history, and sociodemographic characteristics to explore how gestational weight gain relates to (1) transitioning to a higher BMI category or (2) maintaining a higher BMI category. Findings have the opportunity to provide a better understanding of gestational weight gain and weight status patterns over time among socioeconomically disadvantaged women. Specifically, the findings will provide insight into the relationship between gestational weight gain and weight patterns over time among socioeconomically disadvantaged Hispanic women in relation to their white peers.
Materials and Methods
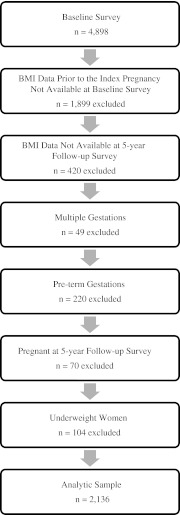
The Fragile Families and Child Well-being Study (FFCW) is a longitudinal study that examines the conditions and capabilities of a socioeconomically disadvantaged cohort of 4898 women who gave birth between 1998 and 2000 in 20 U.S. cities. The baseline survey interviews, which occurred in hospitals between 1998 and 2000, coincided with the index birth. Follow-up interviews occurred at 1, 3, and 5 years after the index birth. As shown in Figure 1, data for this analysis come from women who had complete BMI data before the index pregnancy (which was available at the baseline survey) and who had 5-year survey data (n=2579). Women with complete 5-year survey data were more likely than women with incomplete data to have had a normal or obese BMI before the index pregnancy, were younger, were black, had health insurance, and had more interim pregnancies during the 5-year study period. There were no differences in gestational weight gain between women who participated in the 5-year follow-up survey and women who did not. Information on sampling and design of the study has been reported previously.15 The study was approved by the Institutional Review Board at the Pennsylvania State University.
FIG. 1.
Characteristics of the analytic sample, n=2136. BMI, body mass index.
Analytic sample
A total of 2579 women had prepregnancy BMI data available at the baseline survey and were interviewed at the 5-year follow-up survey. The analytic sample was further restricted to women whose pregnancies resulted in full-term (220 women excluded), singleton births (49 women excluded) to exclude women with lower gestational weight gain due to preterm birth. In addition, the sample was also restricted to women who were not pregnant at the time of the 5-year follow-up survey (70 women excluded). Because of relatively few underweight women (n=104), these women were excluded from analysis. The final analytic sample consisted of 2136 women.
Measures
BMI transitions
To assess change and stability in BMI, BMI was captured at two time points: BMI before the index pregnancy and BMI at the year 5 follow-up survey. BMI before the index pregnancy was obtained from the hospital medical record data at the time of the baseline survey. At the year 5 survey, women reported their height in feet and inches and weight in pounds, from which BMI was calculated. Among reproductive-aged women, self-reported height and weight have been found to represent BMI extracted from medical records adequately.16 At both time points, the continuous BMI measurements were categorized into the reference criteria for adults outlined by the Centers for Disease Control and Prevention (CDC).17 The BMI categories were then used to create five dichotomous dependent variables. Each of the five dependent variables captured women with particular categorical BMI transition patterns; thus, not all women in the analytic sample are included in each of the five dependent variables.
Three of the five dependent variables captured women who transitioned to a higher BMI category between the two time points in comparison to women who maintained the corresponding initial BMI category at both time points: (1) transitioned from normal weight (BMI=18.5-24.9 kg/m2) before the index pregnancy to overweight (BMI=25.0–29.9 kg/m2) at year 5 (vs. maintained normal weight at both time points),17 (2) transitioned from overweight before the index pregnancy to obese (BMI ≥30.0 kg/m2)17 at year 5 (vs. maintained overweight at both time points), and (3) transitioned from normal weight before the index pregnancy to obese at year 5 (vs. maintained normal weight at both time points).
Two of the five dependent variables captured women who maintained a higher BMI category at the two time points in comparison to women who transitioned to a lower BMI category at year 5: (1) maintained overweight before the index pregnancy and at year 5 (vs. transitioned to normal weight at year 5) and (2) maintained obese before the index pregnancy and at year 5 (vs. transitioned to overweight at year 5). Less than 1% of obese women before the index pregnancy transitioned to normal weight at year 5 (n=16). For this reason, the comparison of maintaining obesity at both time points vs. transitioning to normal weight at year 5 was not investigated as a dependent variable.
Independent variables
Gestational weight gain
Gestational weight gain in pounds was obtained from medical record data at the baseline survey. The 2009 IOM pregnancy weight gain guidelines18 were used to categorize women as having gained less than the recommended weight gain, the recommended weight gain, or greater than the recommended weight gain during pregnancy based on women's BMI before the index pregnancy. Recommended weight gain was used as the reference category in multivariate regression models.
Covariates
Covariates were chosen that were hypothesized to be associated with long-term weight gain based on current literature. These covariates are defined below.
Health before the index pregnancy
Medical record data captured women's preexisting health status before the index pregnancy. Preexisting health conditions that have known associations with overweight and obesity were included: cardiac disease, hypertension, and chronic diabetes. Because of a low prevalence of each individual condition, a variable was included to indicate whether or not any of these preexisting health conditions were present (1=yes, 0=no).
Pregnancy history
Weight is known to increase with increasing number of pregnancies.3,19,20 Therefore, any live births before the index pregnancy (1=yes, 0=no) were included in the regression model. To control for pregnancies that occurred in the 5 years after the index pregnancy, three variables controlling for interim pregnancies were included in the regression models: between index pregnancy and year 1 (1=yes, 0=no), between year 1 and year 3 (1=yes, 0=no), and between year 3 and year 5 (1=yes, 0=no).
Sociodemographic characteristics
All sociodemographic characteristics were collected at the baseline survey and reported by the women in the sample. Variables include woman's age (years), marital status (1=married, 0=not married), race (non-Hispanic white [reference], Hispanic, and non-Hispanic black), education (1=high school graduate or more, 0=less than high school education), and household income based on the Federal Poverty Line (FPL) threshold (1=≥200% FPL, 0=<200% of FPL). Participation in public assistance programs (1=yes, 0=no) was included in the regression models, as public assistance programs, specifically the Supplemental Nutrition and Assistance Program, have been associated with elevating women's weight status,21,22 although current research indicates that the effect may be small.23 Minority individuals and individuals of low SES are more likely to have reduced access to care,24 and reduced access to care minimizes assistance provided by clinicians to manage weight. Health insurance coverage served as a proxy for access to care (private, public, none [reference]).
Statistical analyses
Descriptive analysis and multivariate logistic regression analyses were conducted using STATA version 10.0 statistical software (StataCorp LP, College Station, TX). Before conducting the multivariate logistic regression models, multiple imputation techniques were used to impute missing data. Specifically, missing values on the independent variables and eight covariates (1.0% of values) were imputed using switching regression, an interactive multivariable regression imputation technique. The multiple imputation technique created five imputed datasets. The strength of multiple imputation is that all relevant cases are kept in the analyses for accurate parameter estimates and the standard errors (SE) are corrected for the amount of missing information. This is in comparison to listwise deletion, which results in a sample that no longer represents the population.25,26
Multivariate logistic regression models were then conducted on the imputed data to predict longitudinal BMI transitions. The odds ratio (OR) coefficients in the final models represent the estimates of the five pooled datasets. For each of the five dichotomous dependent variables, the dependent variable was regressed onto gestational weight gain, controlling for health status before the index pregnancy and pregnancy history, as well as sociodemographic characteristics.
Results
Sample description
The characteristics for the full analytic sample are shown in Table 1. Over half of the sample entered the pregnancy overweight (27%) or obese (26%). Further, 51% of the sample gained greater than recommended weight during pregnancy, and 19% gained less weight than recommended. Women who transitioned to a higher BMI category over the 5-year period experienced between a 19% and 36% increase in weight, whereas women who transitioned to a lower BMI category over the 5-year period experienced an approximately 9%–14% decrease in weight (Table 2). Women who maintained a steady weight over the 5-year period experienced an approximately 3%–6% increase in weight.
Table 1.
Characteristics of Women in Analytic Sample, n=2136
| Gestational weight gain | |
| Greater than recommended | 1081 (51%) |
| Recommended | 612 (29%) |
| Less than recommended | 402 (19%) |
| Unknown | 41 (<2%) |
| Health before index pregnancy | |
| BMI before index pregnancy | |
| Normal BMI | 1018 (47%) |
| Overweight | 570 (27%) |
| Obese | 548 (26%) |
| Preexisting health conditions before index pregnancy | |
| Preexisting conditions | 158 (7%) |
| No preexisting conditions | 1978 (93%) |
| Pregnancy history | |
| Parity at index pregnancy | |
| 0 births | 799 (37%) |
| ≥1 births | 1331 (62%) |
| Unknown | 6 (<1%) |
| Interim pregnancy between index pregnancy and year 1 | |
| No | 1893 (89%) |
| Yes | 106 (5%) |
| Unknown | 137 (6%) |
| Interim pregnancy between year 1 and year 3 | |
| No | 1503 (70%) |
| Yes | 493 (23%) |
| Unknown | 140 (7%) |
| Interim pregnancy between year 3 and year 5 | |
| No | 1931 (90%) |
| Yes | 205 (10%) |
| Sociodemographic characteristics | |
| Woman's age at index pregnancy, mean years (SD) | 25.18 (6.05) |
| Marital status at index pregnancy | |
| Married | 537 (25%) |
| Not married | 1599 (75%) |
| Race and ethnicity | |
| Non-Hispanic white | 456 (21%) |
| Hispanic | 639 (30%) |
| Non-Hispanic black | 1036 (49%) |
| Unknown | 5 (<1%) |
| Education | |
| Less than high school graduate | 716 (34%) |
| High school graduate or more | 1417 (66%) |
| Unknown | 3 (<1%) |
| Household poverty | |
| <200% of FPL | 1315 (62%) |
| ≥200% of FPL | 821 (38%) |
| Public assistance participation | |
| No participation | 1358 (64%) |
| Participation | 758 (35%) |
| Unknown | 20 (<1%) |
| Health insurance | |
| Private health insurance | 621 (29) |
| Public health insurance | 1368 (64) |
| Uninsured | 118 (6) |
| Unknown | 29 (<2%) |
Descriptives based on nonimputed data.
BMI, body mass index; FPL, Federal Poverty Line; SD, standard deviation.
Table 2.
Average Percent Change in Weight over 5-Year Study Period, by Body Mass Index Transition Group
| Transitioned to higher BMI category | ||
| Normal weight→overweight | Overweight→obese | Normal weight→obese |
| +19.34% | +21.21% | +36.33% |
| (n=266) | (n=201) | (n=70) |
| Transitioned to lower BMI category | ||
| Overweight→normal weight | Obese→overweight | |
| −8.62% | −14.35% | |
| (n=57) | (n=60) | |
| Maintained BMI category | ||
| Normal weight→normal weight | Overweight→overweight | Obese→obese |
| +5.93% | +2.91% | +4.02% |
| (n=577) | (n=259) | (n=399) |
Calculations for percent change in weight are based on nonimputed data at two time points: (1) weight in pounds before index pregnancy and (2) weight in pounds 5 years after index pregnancy.
BMI, body mass index.
Multivariate results
The results of the multivariate logistic regression models predicting longitudinal BMI transitions are displayed in Tables 3 and Table 4. Gaining greater than recommended weight during pregnancy is related to women transitioning to a higher weight category (Table 3) but not related to women maintaining a higher weight category (Table 4). There were several covariates that were significant as well. Women who experienced an interim pregnancy between year 3 and year 5 had approximately two times the odds to transition from normal BMI to overweight during the 5-year period. Older women at the index pregnancy and women with a high school education or more were at lower odds of transitioning from overweight to obesity. Women who had experienced at least one pregnancy before the index pregnancy in the study had approximately two times the odds to transition from normal weight to obesity during the 5-year period. Women with preexisting health conditions before the index pregnancy had over two times the odds of maintaining their obesity status during the 5-year period than transition to overweight status. Hispanic and black women compared to white women were more likely to transition to a higher BMI category as well as maintain a higher BMI category over the 5-year period.
Table 3.
Multivariate Regression Analyses Predicting Higher Weight Category Transitions 5 Years After Index Pregnancy
| Normal weight to overweight vs. stable normal weight (n=843) | Overweight to obese vs. stable overweight (n=460) | Normal weight to obese vs. stable normal weight (n=647) | |
|---|---|---|---|
| Gestational weight gain | |||
| Greater than recommended | 1.10 (0.77-1.56) | 1.79 (1.11-2.88)* | 2.39 (1.28-4.45)** |
| Recommended (Reference) | 1.00 | 1.00 | 1.00 |
| Less than recommended | 0.94 (0.63-1.42) | 0.88 (0.41-1.90) | 0.65 (0.29-1.46) |
| Health before index pregnancy | |||
| Preexisting health conditions before index pregnancy | |||
| Preexisting conditions | 1.02 (0.55-1.88) | 1.37 (0.62-3.03) | 0.32 (0.07-1.43) |
| No preexisting conditions (Reference) | 1.00 | 1.00 | 1.00 |
| Pregnancy history | |||
| Parity at index pregnancy | |||
| 0 births (Reference) | 1.00 | 1.00 | 1.00 |
| ≥1 births | 1.21 (0.87-1.69) | 1.39 (0.86-2.25) | 1.95 (1.05-3.60)* |
| Interim pregnancy between index pregnancy and year 1 | |||
| No (Reference) | 1.00 | 1.00 | 1.00 |
| Yes | 0.55 (0.24-1.29) | 0.89 (0.36-2.22) | 2.20 (0.91-5.33) |
| Interim pregnancy between year 1 and year 3 | |||
| No (Reference) | 1.00 | 1.00 | 1.00 |
| Yes | 1.28 (0.90-1.82) | 1.19 (0.74-1.91) | 1.72 (0.93-3.18) |
| Interim pregnancy between year 3 and year 5 | |||
| No (Reference) | 1.00 | 1.00 | 1.00 |
| Yes | 1.85 (1.11-3.08)* | 1.04 (0.54-1.98) | 0.39 (0.11-1.31) |
| Sociodemographic characteristics | |||
| Woman's age at index pregnancy | 0.99 (0.96-1.03) | 0.94 (0.90-0.98)** | 0.96 (0.89-1.02) |
| Marital status at index pregnancy | |||
| Married | 0.96 (0.63-1.48) | 0.91 (0.51-1.62) | 0.93 (0.39-2.19) |
| Not married (Reference) | 1.00 | 1.00 | 1.00 |
| Race and ethnicity | |||
| Non-Hispanic white (Reference) | 1.00 | 1.00 | 1.00 |
| Hispanic | 2.17 (1.37-3.46)** | 2.13 (1.13-4.04)* | 3.55 (1.23-10.23)* |
| Non-Hispanic black | 2.16 (1.40-3.34)** | 2.04 (1.12-3.73)* | 4.64 (1.69-12.72)** |
| Education | |||
| Less than high school graduate (Reference) | 1.00 | 1.00 | 1.00 |
| High school graduate or more | 0.90 (0.63-1.29) | 0.52 (0.33-0.81)** | 0.60 (0.33-1.07) |
| Household poverty | |||
| <200% of FPL (Reference) | 1.00 | 1.00 | 1.00 |
| ≥200% of FPL | 1.04 (0.71-1.51) | 1.22 (0.74-2.02) | 0.51 (0.25-1.03) |
| Public assistance participation | |||
| No participation (Reference) | 1.00 | 1.00 | 1.00 |
| Participation | 1.72 (1.20-2.46)** | 0.87 (0.55-1.37) | 0.89 (0.49-1.64) |
| Health insurance | |||
| Private health insurance | 0.94 (0.50-1.76) | 0.70 (0.26-1.87) | 0.59 (0.18-1.87) |
| Public health insurance | 0.92 (0.51-1.64) | 0.75 (0.29-1.92) | 1.05 (0.41-2.68) |
| Uninsured (Reference) | 1.00 | 1.00 | 1.00 |
Results are based on imputed data.
Results are given as odds ratio (95% confidence interval).
p<0.001; **p<0.01; *p<0.05.
Table 4.
Multivariate Regression Analyses Predicting Maintaining Higher Weight Category 5 Years After Index Pregnancy
| Stable overweight vs. overweight to normal weight (n=316) | Stable obese vs. obese to overweight (n=459) | |
|---|---|---|
| Gestational weight gain | ||
| Greater than recommended | 1.00 (0.50-2.01) | 0.80 (0.37-1.76) |
| Recommended (Reference) | 1.00 | 1.00 |
| Less than recommended | 0.80 (0.30-2.16) | 0.48 (0.20-1.14) |
| Health before index pregnancy | ||
| Preexisting health conditions before index pregnancy | ||
| Preexisting conditions | 1.43 (0.30-6.88) | 1.66 (0.60-4.63) |
| No preexisting conditions (Reference) | 1.00 | 1.00 |
| Pregnancy history | ||
| Parity at index pregnancy | ||
| 0 births (Reference) | 1.00 | 1.00 |
| ≥1 births | 0.99 (0.49-2.03) | 1.35 (0.66-2.77) |
| Interim pregnancy between index pregnancy and year 1 | ||
| No (Reference) | 1.00 | 1.00 |
| Yes | 1.24 (0.25-6.29) | 1.06 (0.29-3.90) |
| Interim pregnancy between year 1 and year 3 | ||
| No (Reference) | 1.00 | 1.00 |
| Yes | 0.71 (0.35-1.41) | 1.18 (0.58-2.40) |
| Interim pregnancy between year 3 and year 5 | ||
| No (Reference) | 1.00 | 1.00 |
| Yes | 1.29 (0.40-4.17) | 1.09 (0.39-3.00) |
| Sociodemographic characteristics | ||
| Woman's age at index pregnancy | 1.00 (0.94-1.06) | 1.00 (0.94-1.05) |
| Marital status at index pregnancy | ||
| Married | 0.87 (0.38-1.97) | 1.11 (0.49-2.53) |
| Not married (Reference) | 1.00 | 1.00 |
| Race and ethnicity | ||
| Non-Hispanic white (Reference) | 1.00 | 1.00 |
| Hispanic | 1.04 (0.47-2.31) | 2.43 (1.09-5.39)* |
| Non-Hispanic black | 2.83 (1.23-6.50)* | 3.92 (1.86-8.39)** |
| Education | ||
| Less than high school graduate (Reference) | 1.00 | 1.00 |
| High school graduate or more | 1.04 (0.49-2.22) | 0.85 (0.43-1.69) |
| Household poverty | ||
| <200% of FPL (Reference) | 1.00 | 1.00 |
| ≥200% of FPL | 1.35 (0.59-3.05) | 1.62 (0.74-3.56) |
| Public assistance participation | ||
| No participation (Reference) | 1.00 | 1.00 |
| Participation | 0.91 (0.44-1.87) | 0.80 (0.40-1.60) |
| Health Insurance | ||
| Private health insurance | 0.93 (0.17-5.17) | 0.28 (0.05-1.61) |
| Public health insurance | 0.80 (0.15-4.34) | 0.32 (0.06-1.79) |
| Uninsured (Reference) | 1.00 | 1.00 |
Results are based on imputed data.
Results an given as odds ratio (95% confidence interval).
p<0.001; **p<0.01; *p<0.05.
Discussion
This study examined the association between gestational weight gain and longitudinal BMI transitions among socioeconomically disadvantaged women. Similar to previous research that found that low-income women's postpartum weight status is at risk when excess weight is gained during pregnancy,8,9 the current study found excessive gestational weight gain to be associated with transitioning to a higher BMI category. Women who transitioned to a higher weight status experienced a significant amount of weight change (i.e., 19%–36%) over the 5-year study period. Although the study was able to control for the timing of subsequent pregnancies, it was unable to control for the amount of weight gained in subsequent pregnancies or other factors that could be contributing to weight gain, such as lack of physical activity. Engaging in physical activity has been associated with reducing pregnancy-related weight gain.27,28 In addition, recent research indicates that women with normal BMI and lower physical activity levels (i.e., <30 minutes most days) are more likely to transition to overweight status 2 years later.29 Thus, subsequent pregnancies and other weight gain-related factors could be contributing to the higher weight status, but the results suggest that excessive gestational weight gain acts as a catalyst for transitioning to a higher weight status over a 5-year period.
Interestingly, excessive gestational weight gain does not contribute to maintaining a higher weight status 5 years after the index pregnancy among a sample of socioeconomically disadvantaged women. Although the majority of the women gained more than the recommended amount of weight during pregnancy, the women who maintained a higher weight category (either overweight or obese) experienced a weight change of approximately only 3%–4% over the 5-year period. Thus, the association between gaining excessive gestational weight and maintaining a higher weight status 5 years postindex pregnancy does not appear to function in the same manner as gaining excessive gestational weight and transitioning to a higher weight category 5 years postindex pregnancy.
Similar to previous research that has focused on the white-black comparison in postpartum weigh change,10,30 black women were more likely to transition to a higher BMI category or maintain a higher BMI category over time compared to their white peers. This study also provided insight into the relationship between gestational weight gain and weight patterns over time among socioeconomically disadvantaged Hispanic women in relation to their white peers. Similar to the black-white comparison, Hispanic women were more likely to transition to a higher BMI category or maintain a higher BMI category over time compared to their white peers. As previously mentioned, the study was unable to control for physical activity; however, prior research has indicated that Latina women are less likely to meet the American College of Obstetricians and Gynecologists (ACOG) recommendations for moderate physical activity during pregnancy compared to non-Latina white women.31 This relationship is further exacerbated among lower-income Latina women.32 The confluence of physical activity deficiency and obesity trends among the Hispanic population suggest that interventions focusing on reducing the weight status among Hispanic women of reproductive age before pregnancy is needed. It has been observed that interventions geared toward reducing excessive gestation weight that have been implemented early in pregnancy have been successful among low-income women,33 especially women with a normal prepregnancy BMI.34 Among ethnic and race minority women who are also socioeconomically disadvantaged and are overweight or obese before conception, however, encouraging them to engage in weight-modifying interventions before conception may be needed in order to promote adequate gestational weight gain and prevent long-term obesity. In addition, these women may benefit from counseling about the long-term effects of gaining excessive weight during pregnancy.
Pregnancy history and participation in public assistance were related to women transitioning to higher BMI category 5 years after the index pregnancy. In line with previous research,3,19,20 women who had given birth before the index birth in the study were more likely to transition from normal weight to obese in the 5-year period. Likewise, women who had an interim pregnancy in the 2 years prior to the 5-year survey were also at greater odds of transitioning from normal weight to overweight. Thus, there is a need to continue to counsel socioeconomically disadvantaged women on the short-term and long-term effects of pregnancy on weight gain.
For women with a normal BMI before the index pregnancy, participation in public assistance was related to transitioning to overweight status 5 years after the index pregnancy; in other words, women with a greater need of financial assistance are also at greater risk of transitioning to a higher BMI category over time. Although the current study did not control for selection bias toward participation in public assistance programs and was not able to identify which public assistance programs the women used, some studies have found a positive association between participation in the Supplemental Nutrition Assistance Program (SNAP) and higher BMI status in women.21,35–37 It has been suggested that families who are at risk of experiencing food insecurity have limited cash assistance to spend on food at the end of the month because the majority of SNAP benefits are used within the first 3 days of the month when SNAP benefits are distributed.38 The sharp decline in cash benefits toward the end of the month leads to a reduction in food consumption among mothers, perhaps even starving themselves so that their children can have sufficient food to eat.39 As a result, an irregular food consumption pattern emerges that may contribute to women's metabolism slowing down,40,41 influencing weight gain.42
Limitations regarding BMI measurement
There are several measurement concerns about BMI and how BMI was obtained for the current study. A general concern is that although BMI is highly correlated with body fat, it is not a direct measure of adiposity, and it does not differentiate between lean body mass and fat mass.43 Further, the percentage of adiposity and the distribution of adiposity for a given BMI level vary by race and ethnic groups among women.44–46 In addition, higher musculoskeletal mass has been found among black women compared to white women, which may lead to a body fat misclassification if BMI is used as an index.47 This has led to some discussion of whether BMI should be ethnic specific rather than country specific.48 Although such measurement concerns are valid, the percent of weight change among the sample population was significant, and the increased weight puts these women at risk for negative health consequences associated with obesity, such as diabetes, high blood pressure, and high cholesterol.5
BMI data was obtained from two different sources in the current study, both of which led to the concern that overweight and obesity were underreported. In the current study, BMI before the index pregnancy was based on medical records, and the use of medical record data has been questioned. Research focusing on the reliability and validity of birth certificate data to obtain prepregnancy weight and height among low-income samples of women has found the prevalence of obesity to be underestimated, yet the difference was considered to be negligible and limited the impact on reporting bias.49
BMI at the 5-year follow-up was based on self-reported measures of height and weight. Self-reported measures of height and weight present the possibility of underreporting or overreporting of height or weight, which could lead to misclassification of the BMI category. Research has indicated that women are more likely than men to underestimate their height and weight,50 resulting in underestimates of overweight and obesity in women. Despite this concern, self-reported height and weight have been used in various epidemiologic studies, and there is consensus that self-reported height and weight are sufficient quality predictors of actual height and weight.51
In addition to the concern of underreporting because of the use of two different sources to obtain BMI data, the use of two sources also introduces the possibility for inconsistent bias to be present. The inconsistency in reporting could contribute to changes in BMI status. As mentioned previously, women who transitioned to a higher or lower BMI category over the 5-year period had their weight change substantially compared to women who stayed within a BMI category. The substantial change in weight contributes to the change in BMI category and suggests that the different sources of BMI data were not driving the findings in the analyses. A factor that could be driving the analyses that the current study lacked information about, is excessive weight gain from an interim pregnancy or pregnancies. Future studies are needed to replicate the current study and to take into account any weight changes that could have occurred as a result of excessive weight gain from interim pregnancies between the index pregnancy and the 5-year follow-up.
Conclusions
The study used longitudinal data to investigate the relationship between gestational weight gain and BMI transitions 5 years after the index pregnancy among a sample of socioeconomically disadvantaged women who are primarily black and Hispanic. Excessive gestational weight gain is related to transitioning to a higher BMI category but not related to maintaining a higher BMI category. Further, black and Hispanic women are more likely to transition or maintain a higher BMI over the 5-year period than are white women. The study's focus on socioeconomically disadvantaged and primarily black and Hispanic women makes the results not generalizeable to other populations, yet the focus on the restricted population sheds light on the risk factors that contribute to the health disparities among socioeconomically disadvantaged women of reproductive age. The risk factors (e.g., race and ethnicity, pregnancy history, public assistance participation, overweight before pregnancy) can be used by physicians and nurses to target specific socioeconomically disadvantaged women of reproductive age who may benefit from preconception or postpartum counseling. The counseling would need to emphasize the importance of staying within the new IOM recommended pregnancy weight gain guidelines as a way to gain the appropriate amount of weight during pregnancy and to decrease the risk of postpartum weight retention and obesity within the first 5 years after childbirth. Additional research is needed on the contextual and physiologic mechanisms that foster increases in BMI or maintenance of adverse BMI after excessive gestational weight gain. Identifying contextual and physiologic mechanisms may provide suggestions as to possible risk factors that could be modified through weight loss interventions, which include physical activity and nutrition planning.
Acknowledgments
This research was funded, in part, by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (K12 HD055882). In addition, the author thanks participants of the Pennsylvania State University Building Interdisciplinary Research Careers in Women's Health Seminar, along with Drs. Leann Birch, Cynthia Chuang, and Marianne Hillemeier for their comments on preliminary drafts.
Disclosure Statement
No competing financial interests exist.
References
- 1.Flegal K. Carroll M. Ogden C. Curtin L. Prevalence and trends in obesity among U.S. adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Center for Disease Control and Prevention. 2009 Pregnancy Nutrition Surveillance: Maternal health indicators by race/ethnicity, age, or education. Pediatric and Pregnancy Nutrition Surveillance System. 2010. www.cdc.gov/pednss/pnss_tables/pdf/national_table9.pdf. [Feb 7;2011 ]. www.cdc.gov/pednss/pnss_tables/pdf/national_table9.pdf
- 3.Gunderson EP. Murtaugh MA. Lewis CE. Quesenberry CP. West DS. Sidney S. Excess gains in weight and waist circumference associated with childbearing: The Coronary Artery Risk Development in Young Adults Study (CARDIA) Int J Obes. 2004;28:525–535. doi: 10.1038/sj.ijo.0802551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosenberg L. Palmer JR. Wise LA. Horton NJ. Kumanyika SK. Adams-Campbell LL. A prospective study of the effect of childbearing on weight gain in African-American women. Obesity. 2003;11:1526–1535. doi: 10.1038/oby.2003.204. [DOI] [PubMed] [Google Scholar]
- 5.Mokdad AH. Ford ES. Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–79. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- 6.Laitinen J. Power C. Jarvelin MR. Family social class, maternal body mass index, childhood body mass index, and age at menarche as predictors of adult obesity. Am J Clin Nutr. 2001;74:287–294. doi: 10.1093/ajcn/74.3.287. [DOI] [PubMed] [Google Scholar]
- 7.Wang Y. Beydoun MA. The obesity epidemic in the United States—Gender, age, socioeconomic, racial/ethnic, and geographic characteristics: A systematic review and meta-regression analysis. Epidemiol Rev. 2007;59:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 8.Rothberg BEG. Magriples U. Kershaw TS. Rising SS. Ickovics JR. Gestational weight gain and subsequent postpartum weight loss among young, low-income, ethnic minority women. Am J Obstet Gynecol. 2011;204:e1–11. doi: 10.1016/j.ajog.2010.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olson CM. Strawderman MS. Hinton PS. Pearson TA. Gestational weight gain and postpartum behaviors associated with weight change from early pregnancy to 1 year postpartum. Int J Obes. 2003;27:117–127. doi: 10.1038/sj.ijo.0802156. [DOI] [PubMed] [Google Scholar]
- 10.Boardley DJ. Sargent RG. Coker AL. Hussey JR. Sharpe PA. The relationship between diet, activity, and other factors, and postpartum weight change by race. Obstet Gynecol. 1995;86:834–838. doi: 10.1016/0029-7844(95)00283-W. [DOI] [PubMed] [Google Scholar]
- 11.Parker JD. Abrams B. Differences in postpartum weight retention between black and white mothers. Obstet Gynecol. 1993;81:768–774. [PubMed] [Google Scholar]
- 12.Siega-Riz AM. Viswanathan M. Moos MK, et al. A systematic review of outcomes of maternal weight gain according to the Institute of Medicine recommendations: Birthweight, fetal growth, and postpartum weight retention. Am J Obstet Gynecol. 2009;201:339–343. doi: 10.1016/j.ajog.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 13.Institute of Medicine. Influence of pregnancy weight on maternal and child health: Workshop report. Washington, DC: National Academy of Sciences; 2007. [Google Scholar]
- 14.Ennis S. Rois-Vargas M. Albert NG. The Hispanic population: 2010. U.S. Census Bureau; 2011. [Google Scholar]
- 15.Reichman NE. Teitler JO. Garfinkel I. McLanahan SS. Fragile families: Sample and design. Child Youth Serv Rev. 2001;23:303–326. [Google Scholar]
- 16.Huber LRB. Validity of self-reported height and weight in women of reproductive age. Matern Child Health J. 2007;11:137–144. doi: 10.1007/s10995-006-0157-0. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Assessing your weight—About BMI for adults. Healthy weight—It's not a diet, it's a lifestyle! www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html. [Jun 24;2011 ]. www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html
- 18.Institute of Medicine. Weight gain during pregnancy: Re-examining the guidelines. Washington, DC: National Academy of Sciences; 2009. [Google Scholar]
- 19.Billewicz WZ. Thomson AM. Body weight in parous women. Br J Prev Soc Med. 1970;24:97–104. doi: 10.1136/jech.24.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smith DE. Lewis CE. Caveny JL. Perkins LL. Burke GL. Bild DE. Longitudinal changes in adiposity associated with pregnancy: The CARDIA study. JAMA. 1994;271:1747–1751. [PubMed] [Google Scholar]
- 21.Gibson D. Food stamp program participation is positively related to obesity in low income women. J Nutr. 2003;133:225–231. doi: 10.1093/jn/133.7.2225. [DOI] [PubMed] [Google Scholar]
- 22.Gibson D. Long-term food stamp program participation is positively related to simultaneous overweight in young daughters and obesity in mothers. J Nutr. 2006;136:1081–1085. doi: 10.1093/jn/136.4.1081. [DOI] [PubMed] [Google Scholar]
- 23.Baum CL. The effects of food stamps on obesity. South Econ J. 2011;77:623–651. [Google Scholar]
- 24.Agency for Healthcare Research and Quality. National healthcare disparities report. 2010.
- 25.Graham JW. Missing data analysis: Making it work in the real world. Annu Rev Psychol. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- 26.Graham JW. Schafer JL. On the performance of multiple imputation for multivariate data with small sample size. In: Hoyle RH, editor. Statistical strategies for small sample research. Thousand Oaks, CA: Sage; 1999. pp. 1–27. [Google Scholar]
- 27.Ohlin A. Rossner S. Trends in eating patterns, physical activity and socio-demographic factors in relation to postpartum body weight development. Br J Nutr. 1994;71:457–470. doi: 10.1079/bjn19940155. [DOI] [PubMed] [Google Scholar]
- 28.Rooney BL. Schauberger CW. Excess pregnancy weight gain and long-term obesity: One decade later. Obstet Gynecol. 2002;100:245–252. doi: 10.1016/s0029-7844(02)02125-7. [DOI] [PubMed] [Google Scholar]
- 29.Hillemeier MM. Weisman CS. Chuang C. Downs DS. McCall-Hosenfeld J. Camacho F. Transition to overweight or obesity among women of reproductive age. J Womens Health. 2011;20:703–710. doi: 10.1089/jwh.2010.2397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Davis E. Olson C. Obesity in pregnancy. Prim Care Clin Office Pract. 2009;36:341–356. doi: 10.1016/j.pop.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 31.Petersen AM. Leet TL. Brownson RC. Correlates of physical activity among pregnant women in the United States. Med Sci Sports Exerc. 2005;37:1748–1753. doi: 10.1249/01.mss.0000181302.97948.90. [DOI] [PubMed] [Google Scholar]
- 32.Chasan-Taber L. Schmidt MD. Pekow P. Sternfeld B. Manson JA. Markenson G. Correlates of physical activity in pregnancy among Latina women. Matern Child Health J. 2007;11:353–363. doi: 10.1007/s10995-007-0201-8. [DOI] [PubMed] [Google Scholar]
- 33.Olson CM. Strawderman MS. Reed RG. Efficacy of an intervention to prevent excessive gestational weight gain. Am J Obstet Gynecol. 2004;191:530–536. doi: 10.1016/j.ajog.2004.01.027. [DOI] [PubMed] [Google Scholar]
- 34.Polley BA. Wing RR. Sims CJ. Randomized controlled trial to prevent excessive weight gain in pregnant women. Int J Obes. 2002;26:1494–1502. doi: 10.1038/sj.ijo.0802130. [DOI] [PubMed] [Google Scholar]
- 35.Baum C. The effects of food stamps on obesity. Washington, DC: U.S. Department of Agriculture, Economic Research Service; 2007. p. 34. [Google Scholar]
- 36.Chen Z. Yen ST. Eastwood DB. Effects of food stamp participation on body weight and obesity. Am J Agric Econ. 2005;87:1167–1173. [Google Scholar]
- 37.Jones SJ. Frongillo EA. The modifying effects of food stamp program participation on the relation between food insecurity and weight change in women. J Nutr. 2006;136:1091–1094. doi: 10.1093/jn/136.4.1091. [DOI] [PubMed] [Google Scholar]
- 38.Wilde PE. Ranney CK. The monthly food stamp cycle: Shopping frequency and food intake decisions in an endogenous switching regression framework. Am J Agric Econ. 2000;82:200–213. [Google Scholar]
- 39.Wilde PE. Ranney CK. A monthly cycle in food expenditure and intake by participants in the U.S. food stamp program. Madison, WI: Institute for Research on Poverty; 1998. [Google Scholar]
- 40.Gingras JR. Harber V. Field CJ. McCargar LJ. Metabolic assessment of female chronic dieters with either normal or low resting energy expenditures. Am J Clin Nutr. 2000;71:1413–1420. doi: 10.1093/ajcn/71.6.1413. [DOI] [PubMed] [Google Scholar]
- 41.Manore MM. Berry TE. Skinner JS. Carroll SS. Energy expenditure at rest and during exercise in nonobese female cyclical dieters and in nondieting control subjects. Am J Clin Nutr. 1991;54:41–46. doi: 10.1093/ajcn/54.1.41. [DOI] [PubMed] [Google Scholar]
- 42.Townsend MS. Peerson J. Love B. Achterberg C. Murphy SP. Food insecurity is positively related to overweight in women. J Nutr. 2001;131:1738–1745. doi: 10.1093/jn/131.6.1738. [DOI] [PubMed] [Google Scholar]
- 43.Hu FB. Measures of adiposity and body composition. In: Hu FB, editor. Obesity epidmiology. New York: Oxford University Press; 2008. pp. 53–83. [Google Scholar]
- 44.Casas YG. Schiller BC. DeSouza CA. Seals DR. Total and regional body composition across age in healthy Hispanic and white women of similar socioeconomic status. Am J Clin Nutr. 2001;73:13–18. doi: 10.1093/ajcn/73.1.13. [DOI] [PubMed] [Google Scholar]
- 45.Fernandez JR. Heo M. Heymsfield SB, et al. Is percentage body fat differentially related to body mass index in Hispanic Americans, African Americans, and European Americans? Am J Clin Nutr. 2003;77:71–75. doi: 10.1093/ajcn/77.1.71. [DOI] [PubMed] [Google Scholar]
- 46.Rahman M. Temple JR. Breitkopf CR. Berenson AB. Racial differences in body fat distribution among reproductive-aged women. Metabolism. 2009;58:1329–1337. doi: 10.1016/j.metabol.2009.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Aloia JF. Vaswani A. Mikhail M. Flaster ER. Body composition by dual-energy x-ray absorptiometry in black compared with white women. Osteoporos Int. 1999;10:114–119. doi: 10.1007/s001980050204. [DOI] [PubMed] [Google Scholar]
- 48.Stevens J. Ethnic-specific cutpoints for obesity vs country-specific guidelines for action. Int J Obes. 2003;27:287–288. doi: 10.1038/sj.ijo.0802255. [DOI] [PubMed] [Google Scholar]
- 49.Park S. Sappenfield WM. Bish C. Bensyl DM. Goodman D. Menges J. Reliability and validity of birth certificate prepregnancy weight and height among women enrolled in prenatal WIC program: Florida, 2005. Matern Child Health J. 2009 doi: 10.1007/s10995-009-0544-4. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 50.Yun S. Zhu BP. Black W. Brownson RC. A comparison of national estimates of obesity prevalence from the Behavioral Risk Factor Surveillance System and the National Health and Nutrition Examination Survey. Int J Obes. 2005;30:164–170. doi: 10.1038/sj.ijo.0803125. [DOI] [PubMed] [Google Scholar]
- 51.Cawley J. The impact of obesity on wages. J Hum Resource. 2004;39:451–474. [Google Scholar]