Abstract
A 55-year-old woman consulted our hospital for an epulis-like small mass in the anterior region of the mandible. A biopsy of the tumor was performed. Histological analysis showed that the tumor consisted of spindle-shaped and polygonal cells with hyperchromatic nuclei, and intracytoplasmic vacuoles and mitotic figures were scattered. Immunohistochemical staining revealed that the tumor cells were positive for factor VIII-related antigen, CD31, αSMA, and vimentin, but negative for pancytokeratins, S100 protein, neuron-specific enolase, and CD56. The Ki-67 labeling index was more than 50%. Based on these findings, a final pathological diagnosis of angiosarcoma was made. The tumor did not invade into the surrounding tissue. The operation was performed with about a 20-mm surgical margin that was negative for tumor invasion. After a 4-year follow-up, no metastatic lesions were found, and the primary site was covered with a partial denture.
Keywords: Gingival angiosarcoma, mandible, gingiva, epulis-like shape, immunohistochemistry
Introduction
Angiosarcoma is a rare malignant mesenchymal tumor that arises from the vascular endothelium. Angiosarcomas constitute less than 1% of all malignant mesenchymal lesions [1]. Although angiosarcoma can occur in any location, the most common sites are soft tissue and skin [2]. Angiosarcoma of the oral cavity is extremely rare; the existing literature consists of only a few case reports [3-5] and case series [6]. Here, we report a small epulis-like angiosarcoma of the gingival mucosa of the mandible.
Case report
A 55-year-old woman was clinically diagnosed with epulis of the gingiva of the mandible. The epulis was a soft exophytic nodular mass, with well-defined limits and a maximum diameter of 10 mm (Figure 1). The tumor was soft, white-pink in color, with easy bleeding. Histological analysis of serial sections revealed different microscopic aspects which confirmed that the lesion was pleomorphic. We observed large areas with distinctive vascular lumens, sometimes anastomosed. A biopsy of the tumor was performed. The tumor consisted of spindle-shaped and polygonal cells with hyperchromatic nuclei with conspicuous nucleoli while intracytoplasmic vacuoles and mitotic figure were scattered (Figures 2A and 2B). Immunohistochemical staining revealed that the tumor cells were positive for factor VIII-related antigen (Figure 2C), CD31, αSMA (Figure 2D), and vimentin, but negative for pancytokeratins, S100 protein (Figure 2E), neuron-specific enolase, and CD56. The Ki-67 labeling index was more than 50% (Figure 2F). A summary of our findings is shown in Table 1. A standard uptake value of 5.5 was observed during a PET examination (Figure 3). CT and MRI were not informative because of small size of the mass. Based on these findings, our initial pathological diagnosis was angiosarcoma.
Figure 1.
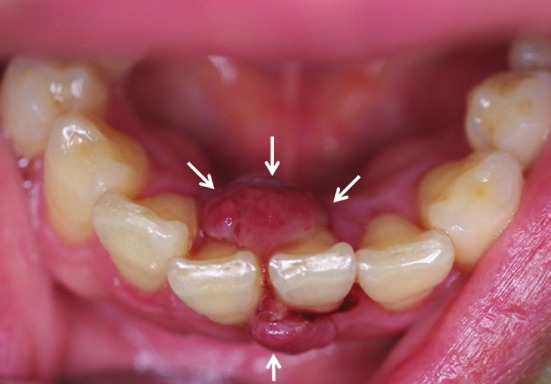
An epulis-like small mass (white arrows) was present in the anterior region of the mandible. The mass was soft and well-defined with white-red color. However, it was easy to bleeding. The maximum diameter of the tumor was 10mm.
Figure 2.
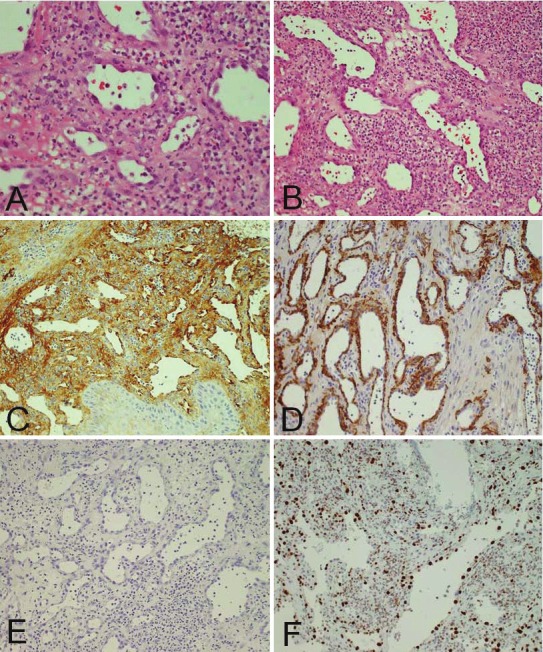
A and B: H & E staining of the tumor observed under magnification ×400 and ×200, respectively, C: Immunohistochemical staining for Factor VIII (×200), D: αSMA (× 200), E: S100 (× 200), and F: Ki-67.
Table 1.
Immunohistochemical reagents and results
| Factor VIII | CD31 | αSMA | vimentin | pancytokeratins | S100 | NSE | CD56 |
|---|---|---|---|---|---|---|---|
| + | + | + | + | - | - | - | - |
Figure 3.
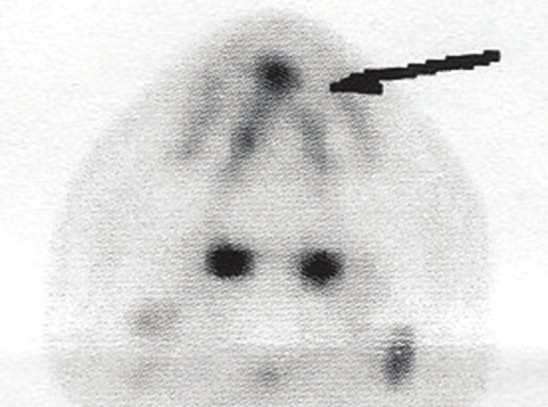
PET examination of the tumor showed a standard uptake value of 5.5.
The operation was performed with about a 20-mm surgical margin that was negative for tumor invasion. The postoperative course was uneventful. So far, after a 4-year follow-up, no metastatic lesions have been found, and the primary site is covered with a partial denture (Figures 4A and 4B).
Figure 4.
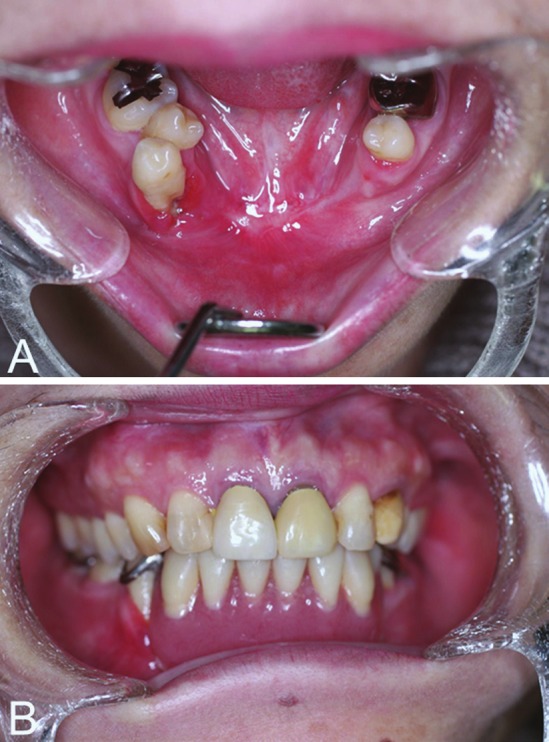
A: A follow-up after 4 years showed absence of local recurrence of the tumor. B: The defect was covered by a partial denture.
Discussion
In this case of angiosarcoma, the vascular structures exhibited zones with hardly visible lumens that resembled broad vascular spaces and were frequently filled with erythrocytes. Some of the vessels showed thickening of walls and a narrow lumen filled with homogenous hyaline eosinophilic material. The endothelium that lined the vessels was flattened, almost like normal epithelium, but at some places with big, hyperchromatic, crowded nuclei, showing mitotic activity. In some areas, the atypical endothelia showed heterogeneous intraluminal papillary proliferation. These aspects suggested the existence of a vascular tumor despite the relatively benign vascular proliferation. The neoplastic cells had round or polygonal shape, were tall, with intense eosinophilic cytoplasm, and round-ovoid polymorphous nuclei with frequent atypical mitosis. The aspect of the cells simulated the aspect of the epithelial-like cells. Based on this, the patient was diagnosed with angiosarcoma. In the interior part of the neoplastic proliferation, we observed blood vessels mostly with a small lumen or branched vascular spaces, delimitated by atypical endothelia, and containing some red cells.
Immunohistochemical analysis was done to ascertain the origin of the neoplastic proliferation-whether it was vascular, carcinoma-like, or sarcoma-like. Immunostaining revealed intense CD31 staining in large zones in different area of the tumor, independent of the morphology of the neoplastic cells both in the cells that outlined the vascular structures and between the solid neoplastic areas (Figure 2). The tumor cells were also positive for factor VIII-related antigen, αSMA, vimentin, but negative for pancytokeratins, S100 protein, neuron-specific enolase, and CD56.
Generally, angiosarcoma is a very aggressive tumor. Angiosarcoma of the oral cavity may occur in various tissues, such as oral soft tissue, minor salivary glands, and bones [3-6]. The present case occurred in the gingiva in the oral cavity. Fanburg-Smith et al. [6] reported 22 cases of primary angiosarcoma of the oral and salivary glands. The sites of the 22 cases included 9 in the tongue, 4 in the parotid gland, 4 in the lip, 3 in the submandibular gland, and 1 in the palate [6]. Men and women were equally affected [6]. The symptoms are tumor mass bleeding. In this case, the mass was also bleeding easily. The size ranged from 0.8 to 7.0cm. Histological analysis showed that all tumors were vasoformative, 86% had solid areas, and 17% had papillary areas. F-VIII-RA expression was observed in 19/21, CD31 in 16/19, and CD34 in 7/12 cases [6]. The survival differed depending on locations, and ranged from 1 year to 20 years with an average of 7.3 years. The survival was longer in low-grade angiosarcoma than in high-grade angiosarcoma [6]. Angiosarcomas mainly occur in elderly patients, are aggressive, tend to recur locally, spread wide, and have a high rate of lymph node and systemic metastases, as well as tumor related-death [7-10]. There is general agreement that the poor prognosis of angiosarcoma of the oral cavity is not influenced by the histologic grade and mitotic activity, as is the case with angiosarcoma in other anatomic regions [8,9]. In the current case study, the small mass was detected early because of the patient’s timely visit to the hospital. The time of the tumor detection could be one of the prognostic factors of this disease.
Acknowledgement
This work was supported by grants from the Japanese Ministry of Education, Culture, Sports, Science and Technology (Japanese Government Study Program) to T Sumida.
References
- 1.Enzinger FM, Weiss SW. Malignant vascular tumors. In: Enzinger FM, Weiss SW, editors. Soft tissue tumors. 3rd ed. St Louis: Mosby; 1995. pp. 641–677. [Google Scholar]
- 2.Terada T. Angiosarcoma of the Oral Cavity. Head Neck Pathol. 2011;5:67–70. doi: 10.1007/s12105-010-0211-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abdullah BH, Yahya HI, Talabani NA, Alash NI, Mirza KB. Gingival and cutaneous angiosarcoma. J Oral Pathol Med. 2000;29:410–412. doi: 10.1034/j.1600-0714.2000.290807.x. [DOI] [PubMed] [Google Scholar]
- 4.Loudon JA, Billy ML, DeYoung BR, Allen CM. Angiosarcoma of the mandible: a case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:471–476. doi: 10.1016/s1079-2104(00)70127-2. [DOI] [PubMed] [Google Scholar]
- 5.Favia G, Lo Muzio L, Serpico R, Maiorano E. Angiosarcoma of the head and neck with intraoral presentation: a clinico-pathological study of four cases. Oral Oncol. 2002;38:757–762. doi: 10.1016/s1368-8375(02)00045-3. [DOI] [PubMed] [Google Scholar]
- 6.Fanburg-Smith JC, Furlong MA, Childers EL. Oral and salivary gland angiosarcoma: a clinicopathlogic study of 29 cases. Mod Pathol. 2003;16:263–271. doi: 10.1097/01.MP.0000056986.08999.FD. [DOI] [PubMed] [Google Scholar]
- 7.Jones EW. Malignant vascular tumours. Clin Exp Dermatol. 1976;1:287–312. doi: 10.1111/j.1365-2230.1976.tb01435.x. [DOI] [PubMed] [Google Scholar]
- 8.Maddox JC, Evans HL. Angiosarcoma of skin and soft tissue: a study of forty-four cases. Cancer. 1981;48:1907–1921. doi: 10.1002/1097-0142(19811015)48:8<1907::aid-cncr2820480832>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 9.Mackenzie IJ. Angiosarcoma of the face. Arch Dermatol. 1985;121:549–550. [PubMed] [Google Scholar]
- 10.Holden CA, Spittle MF, Jones EW. Angiosarcoma of the face and scalp, prognosis and treatment. Cancer. 1987;59:1046–1057. doi: 10.1002/1097-0142(19870301)59:5<1046::aid-cncr2820590533>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]


