Abstract
Objective
Children with unilateral hearing loss (UHL) have been found to have lower language scores, and increased rate of speech therapy, grade failures, or needing Individualized Education Plans (IEPs). The objective of this study was to determine whether language skills and educational performance improved or worsened over time in a cohort of children with UHL.
Study Design
Prospective longitudinal cohort study
Methods
Forty-six children with permanent UHL, ages 6 to 12 years, were studied using standardized cognitive, achievement, and language testing at yearly intervals for three years. Using standardized test scores allowed implicit comparison to norms established by national cross-sectional samples. Secondary outcomes included behavioral issues, IEPs, receipt of speech therapy, or teacher report of problems at school. Analysis utilized repeated measures ANOVA and multilevel random regression modeling.
Results
Several cognitive and language mean standardized scores increased over time. Possible predictors of increase with time included higher baseline cognitive levels and receipt of interventions through an IEP. However, standardized achievement scores and indicators of school performance did not show concomitant improvements. Rates of IEPs remained > 50% throughout, and rates of speech therapy were consistently about 20%.
Conclusions
Children with UHL demonstrated improvement in oral language and verbal IQ scores over time, but not improvements in school performance. Parents and teachers reported persistent behavioral problems and academic weaknesses or areas of concern in about 25%. The provision of IEPs for children with UHL, and acknowledging UHL as a hearing disability, may be an effective intervention to improve language skills over time.
Keywords: unilateral hearing loss, children, speech or language delay
INTRODUCTION
“Historically, the involvement of hearing health professionals in the management of children with unilateral hearing loss has been limited. The conventional approach was to identify the cause of the hearing loss and to assure the parents that there would be no handicap.”1
Unilateral hearing loss (UHL) affects an increasing number of children as they grow older, from 1 in 1000 newborns to 1 in 5 adolescents.2–5 Small studies from the late 20th century suggested that compared to peers with bilateral normal hearing (NH), children with UHL were at risk for increased rates of grade failures (24–35% vs. 3% in the NH population).6–8 Many children with UHL required additional educational assistance (12–41%) and were prone to behavioral problems at school.9 Those studies suggested several risk factors, including early age of UHL onset, perinatal and/or postnatal medical complications, severe-to-profound UHL, and right ear UHL.10 Young children with UHL in preschool were found to have delayed language development compared to their NH peers,11 but a study in older elementary students did not find similar results.12 A recent large case-control study showed that compared to siblings with NH, school-aged children with UHL had significantly lower oral language scores, 4.4 times the risk of having an Individualized Educational Plan (a sign of difficulty in school), and 2.5 times the risk of speech therapy.13 Other predictors of lower language scores included lower IQ, male sex, family income below the federal poverty level, and lower maternal education levels.
To date, only one prior study has examined longitudinal outcomes in children with UHL. Children with severe UHL at seven years of age (n=44) were evaluated again at 11 years of age.14 Although as a group, these children had a higher proportion of speech difficulties, and “backwardness in oral ability and reading,” only four children still had poor speech intelligibility at 11 years, and had similar reading scores to NH peers. However, at least 13 of the 44 children had temporary hearing loss. No longitudinal studies have been performed in older children or adolescents with UHL.
Although bilateral hearing loss in adults has been associated with decreased rates of literacy, diminished earnings, difficulty communicating at work, and diminished quality of life,15–18 whether UHL in children leads to similar problems in adulthood is not known. However, adults have complained of negative psychosocial effects of UHL. In a qualitative study of 20 adults and teenagers, participants reported that extraneous noise and distance created difficult listening situations, and that they often suffered negative feelings of embarrassment, annoyance, confusion and helplessness in communication with others.19 Using the Hearing Handicap Inventory for Adults, Newman et al reported that among 43 adults with UHL, 32% reported a mild-moderate handicap, 40% reported significant handicap, and only 28% reported no handicap.20 This variability was not related to severity of hearing loss, but hearing handicap was similar to that reported from adults with bilateral mild hearing loss.
Given the overall dearth of knowledge about the longitudinal effects of UHL in children, we sought to gain a greater understanding of the natural history of children affected by UHL. The objective of this study was to determine whether speech-language and educational performance increased or decreased over time in a cohort of children with UHL.
METHODS
Institutional Review Board approval was obtained prior to the onset of this study. All parent and child participants signed written informed consents and pediatric assents, respectively.
Participants
Children aged 6 to 8 years old were recruited from pediatric otolaryngology clinics and several regional school districts. The school districts identified children through hearing screening programs or audiologic testing, and not as a result of receiving special services.
Inclusion criteria
Children were eligible if they had UHL, defined as an average threshold of any three consecutive frequencies of ≥30 dB hearing level (HL) in the affected ear. Normal hearing in the other ear was defined as a pure tone threshold average (PTA) of 500, 1000, and 2000 Hz of <20 dB HL, and threshold at 4000 Hz <30 dB. The UHL had to be sensorineural or mixed/conductive hearing loss considered ‘permanent,’ operationally defined as not being reversible with any known medical or surgical therapy during the course of the study.
Exclusion criteria
Children were excluded if they had temporary or fluctuating conductive UHL, or had a medical diagnosis associated with cognitive impairment (e.g., Down syndrome, congenital cytomegalovirus infection) or cognitive impairment per parental report.
Demographic and baseline variables
Subject demographic information, parental socioeconomic data, subject current and past medical history, and subject educational history were obtained through parental questionnaire and interview. The percentage of federal poverty level (FPL) was calculated using family size and income.21
Longitudinal assessment
Children with UHL underwent standardized cognitive, achievement, and language testing at yearly intervals for three years, as well as an annual audiogram. Parents were asked to assess their child’s behavior and allow schools to release grades and standardized test scores from the previous year. Parents were queried through semi-structured interview about interventions, evaluations, or extra assistance that the subject received over the previous year that could possibly affect the subject’s performance.
Outcome variables
Cognitive ability was measured using the Wechsler Abbreviated Scale of Intelligence that provided Verbal, Performance, and Full Scale IQ scores.22 Achievement was measured using the Wechsler Individual Achievement Test-Second Edition-Abbreviated (WIAT-II-A), a standardized measure of reading, math and writing.23 Language was assessed with the oral portion of the Oral and Written Language Scales (OWLS),24 to measure understanding of spoken language (Listening Comprehension Scale [LC]) and the understanding and use of spoken language (Oral Expression Scale [OE]). The Oral Composite Scale (OC) combines the LC and OE scores into a single overall score. All of the standardized tests convert raw scores into scaled scores that are statistically normed by age to have a mean of 100 and a standard deviation (SD) of 15, based on cross-sectional studies in typically developing children.
Behavioral problems were measured using the Child Behavior Checklist (CBCL), considered the “gold standard” psychological instrument to assess behavior in children.25 Raw scores from the CBCL are also converted into scaled scores, where a T score of 50 is assigned to the 50th percentile, standardized by age. Clinically important problem scores for the Syndrome and DSM scales are defined as those at or above the 98th percentile. Clinically important Competency problem scores are defined as those at or below the third percentile.
Hearing outcomes were measured in a sound-treated booth. PTAs were calculated as the average of 500, 1000, 2000, and 4000 Hz. Severity of hearing loss in the worse ear was categorized as mild for PTA <40 dB HL; moderate for PTA 40–69 dB HL; severe for PTA 70–89 dB HL; and profound for PTA ≥ 90 dB HL. Word recognition scores (WRS) were obtained monaurally in quiet using Central Institute for the Deaf (CID) W-22 word lists through headphones at 40 dB above the speech reception threshold, or the participant’s most comfortable loudness level. WRS in noise using CID W-22 word lists were obtained through soundfield testing at +5 and 0 dB signal-to-noise ratios, with noise consisting of recorded 8-talker speech babble.
Secondary outcomes recorded included parent-report of speech-language delay or problems, receipt of speech-language therapy, and provision of individualized educational plans (IEPs) or section 504c accommodations for hearing disability at school. Qualitative data was obtained from the academic report cards, IEP reports, and teacher narratives.
Analysis
Bivariate analyses examined the speech-language, achievement, and behavioral outcomes associated with patient demographic, baseline clinical, and risk factor variables. Student’s t test or one-way ANOVA were used for continuous variables. Chi-square or Fisher exact tests were used for categorical variables. Logistic regression analysis of other outcomes was used to estimate the odds ratio (OR) and 95% confidence interval (CI). A two-tailed alpha level of 0.05 was considered statistically significant.
Repeated measures ANOVA, Mantel-Haenszel chi square and random effect regression (multilevel) modeling were used to evaluate change over time. All statistical analyses were performed using SAS software, version 9.2 (Cary, North Carolina).
RESULTS
Table I summarizes the demographic, selected educational history, medical history, and hearing characteristics of the 46 children with UHL who participated. Notably, 39% had received speech therapy, 54% had received an IEP, and 36% had received additional educational assistance. Approximately half of the cohort had ever tried any form of amplification: 13 (28%) had used an FM system, nine (20%) had used a conventional hearing aid, and three (7%) had used a CROS aid; none wore a BAHA. Only one additional child each had tried using an FM system and conventional hearing aid over the course of the study. The number of children who used currently amplification appeared to increase slightly from 18 in year 1, 23 in year 2 and 22 in year 3, but this was not statistically significant (Mantel-Haenszel chi square for trend, p = 0.36).
Table I.
Baseline demographic, medical history, educational, and hearing characteristics of 46 children with unilateral hearing loss (UHL).
| Characteristic | Result |
|---|---|
| Demographic | |
| Age, years (SD) | 7.5 (1.1) |
| Males, n (%) | 25 (54) |
| Race, n (%) | |
| White | 31 (67) |
| Black | 9 (20) |
| Asian | 3 (6) |
| Other | 3 (6) |
| Hispanic ethnicity, n (%) | 3 (6) |
| Insurance status, n (%) | |
| Private | 32 (70) |
| Medicaid | 12 (26) |
| Both | 1 (2) |
| None | 1 (2) |
| Adopted, n (%) | 5 (11) |
| First-born, n (%) | 22 (48) |
| 1st language not English, n (%) | 3 (6) |
| Family income, n (%) | |
| Above (>200%) FPL | 34 (74) |
| Borderline (100–200%) FPL | 5 (11) |
| Below (<100%) FPL | 7 (15) |
| Medical history | |
| Premature, n (%) | 6 (13) |
| Head trauma, n (%) | 10 (21) |
| Recurrent Otitis Media, n (%) | 12 (25) |
| ADHD, n (%) | 5 (11) |
| Takes regular meds, n (%) | 22 (48) |
| Wears glasses, n (%) | 6 (13) |
| Speech-language delay, n (%) | 6 (13) |
| Educational | |
| Repeated at least one grade, n (%) | 3 (6) |
| IEP/504C plan, n (%) | 25 (54) |
| Special educational needs, n (%) | 17 (36) |
| Received speech therapy, n (%) | 18 (39) |
| Behavioral issues identified by teacher | 16 (35) |
| Hearing | |
| Hearing severity, n (%) | |
| Mild | 4 (9) |
| Moderate | 8 (17) |
| Severe | 7 (15) |
| Profound | 28 (61) |
| Side of UHL, n (%) | |
| Right | 28 (61) |
| Left | 18 (39) |
| Ever used amplification | 22 (48) |
| Currently used amplification | 18 (39) |
SD, standard deviation; FPL, federal poverty level; ADHD, attention deficit hyperactivity disorder
The annual results of the standardized testing are displayed in Table II. Although there was no change in the achievement test mean scores, verbal and full IQ and OE and OC mean scores increased significantly over time. In addition, the vocabulary T scores showed a trend toward increase over time. Rates of IEPs, speech therapy, and behavioral issues identified by teachers did not decrease over time with rates of 51%, 22%, and 32%, respectively, in the last year of follow-up.
Table II.
Longitudinal results in a cohort of children with unilateral hearing loss, by year of testing.
| Year 1 (n=46) | Year 2 (n=46) | Year 3 (n=41) | P value* | |
|---|---|---|---|---|
| Mean age (SD) | 7.5 (1.1) | 8.6 (1.2) | 9.7 (1.3) | |
| Oral Language | ||||
| Listening comprehension | 92 (11) | 94 (12) | 95 (15) | 0. 156 |
| Oral expression | 90 (14) | 93 (15) | 97 (17) | 0. 0003 |
| Oral composite | 88 (13) | 92 (14) | 95 (16) | 0. 0016 |
| Cognition | ||||
| Performance IQ | 100 (14) | 100 (17) | 102 (17) | 0.357 |
| Verbal IQ | 99 (16) | 102 (15) | 107 (15) | 0.011 |
| Vocabulary T-score | 47 (11) | 49 (11) | 51 (12) | 0.078 |
| Full IQ | 100 (15) | 102 (16) | 105 (16) | 0.016 |
| Achievement | ||||
| Reading | 103 (13) | 104 (16) | 104 (14) | 0.741 |
| Math | 102 (14) | 103 (23) | 106 (18) | 0.475 |
| Writing | 102 (14) | 103 (23) | 106 (18) | 0.087 |
Repeated measures ANOVA
Random effect regression was used to model the role of time (level 1) on IQ, language and achievement scores, using age as the time variable (Table III). Analysis of the proportional within-person variance (pseudo R2) explained by time alone reveals that time decreased variance more than 10% for only full scale IQ (0.109), verbal IQ (0.115), OE (0.149), and OC (0.168) scores. Additional individual child-level predictors of scores over time (level 2 predictors) were sought for IQ and the oral language scores. Predictors of baseline scores (intercept) included black race (negative effect on full IQ, verbal IQ, OE and OC scores), receipt of IEP (negative effect on full and verbal IQ), and speech-language problem (negative effect on verbal IQ). Additionally, baseline verbal and full IQ were predictors of all language scores—LC, OE, and OC. Severity and side of UHL, WRS in quiet or in noise, or use of amplification (any form, FM system, hearing aid, or CROS aid) were not predictors of either baseline scores or change over time (data not shown). Predictors of change over time (slope) included speech-language problem (positive effect on verbal IQ), black race (negative effect on LC), and full IQ below 90 (negative effects on OE and OC scores). Figure 1 displays the multilevel predictive model of the effect of full IQ (dichotomized as > 90 or ≤ 90) on OC scores over time. This graph shows that although all children started with a similar OC score at age 6 years, children with an IQ > 90 increased their OC scores over time, whereas children with an IQ ≤ 90 did not. In Figure 2, the predicted effect of the receipt of an IEP on verbal IQ is displayed. This graph shows that children who received an IEP had a significantly lower baseline verbal IQ compared with those who did not. While both groups demonstrated increase of their verbal IQ over time, those who had received an IEP demonstrated a trend toward faster rate of increase, such that the predicted verbal IQ at age 12 years approaches the scores of those who did not.
Table III.
Random regression (multilevel) models of the effect of time, defined as age at testing beginning at age 6 years, in 46 children with unilateral hearing loss.
| Outcome | Initial Status (SE) | Rate of Change (SE) | Pseudo R2 |
|---|---|---|---|
| Full IQ | 97.5 (2.7)*** | 1.76 (0.59)** | 0.109 |
| Verbal IQ | 96.1 (2.9)*** | 2.48 (0.76)** | 0.115 |
| Performance IQ | 100.0 (2.7)*** | 0.34 (0.61) | 0.017 |
| Listening comprehension | 90.6 (2.4)*** | 1.04 (0.69) | 0.045 |
| Oral expression | 85.5 (2.8)*** | 2.87 (0.70)*** | 0.149 |
| Oral composite | 85.3 (2.7)*** | 2.48 (0.72)** | 0.168 |
| Reading achievement | 104.3 (2.4)*** | −0.24 (0.52) | 0 |
| Math achievement | 93.8 (2.8)*** | 0.50 (0.72) | 0 |
| Writing achievement | 99.8 (3.4)*** | 1.44 (0.93) | 0.026 |
Note: The Initial Status provides the model’s calculated mean baseline score at the age of 6 years. The Rate of Change indicates the slope of the change in scores over time (i.e., calculated change in score per year). The Pseudo R2 values provide the proportional within-person variance that is explained by the effect of time.
p<0.05,
p<0.01,
p<0.001
Figure 1.
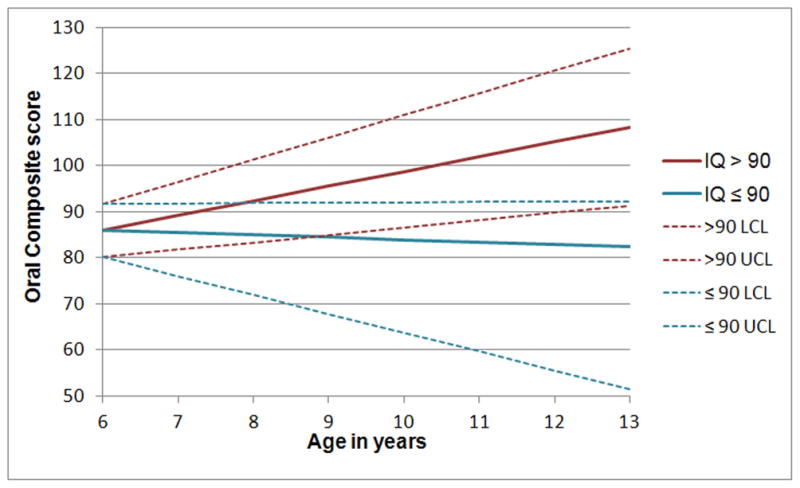
Random regression (multilevel) predictive model of the effect of full IQ on the Oral Composite language scores over time. Full IQ was dichotomized as either above 90 (> 90) or 90 and below (≤90). Oral Composite scores are standard scores with a population a mean of 100 and SD of 15. The dashed lines show the upper (UCL) and lower (LCL) 95% confidence limits.
Figure 2.
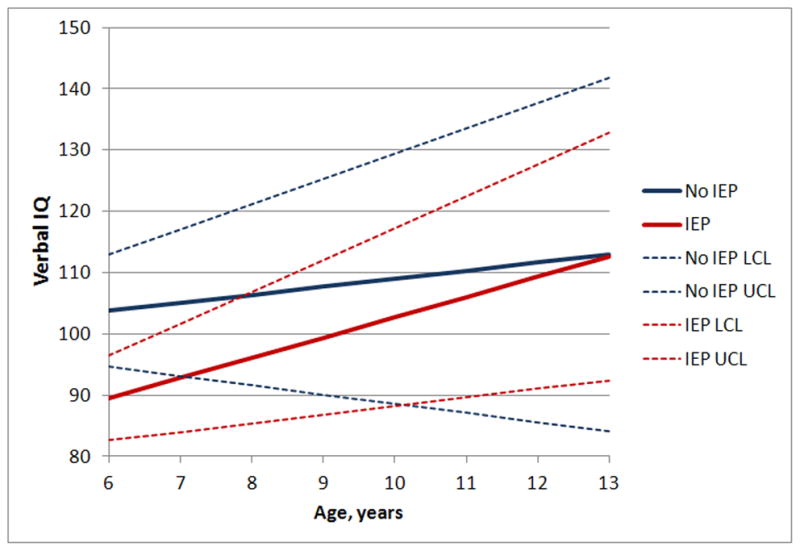
Random regression (multilevel) predictive model of the effect of receiving an Individualized Education Plan (IEP) on verbal IQ scores over time. Verbal IQ scores are standard scores with a population a mean of 100 and SD of 15. The dashed lines show the upper (UCL) and lower (LCL) 95% confidence limits.
In order to identify other possible predictors of change, children with qualitatively large positive slopes (i.e., large increases in standardized scores over time evident on visual inspection of individual trajectories) in either OE or Verbal IQ scores were identified and compared to the remainder of the longitudinal cohort. This comparison allowed us to identify other predictors of large increases in scores, and determine whether the increases in scores of the entire cohort were disproportionately influenced by this subgroup. Table IV summarizes the characteristics of this subgroup. These 10 children were older at identification of their hearing loss, came from families well above the FPL, and had higher cognitive, receptive language, reading and writing skills at baseline.
Table IV.
Comparison of 10 children with large increases in Oral Expression or Verbal IQ with the remaining 36 children in the longitudinal cohort with unilateral hearing loss.
| Characteristic | Children with large slopes | Children without large slopes | P value |
|---|---|---|---|
| Age at identification of UHL, years (SD) | 5.8 (1.4) | 4.0 (2.5) | 0.038 |
| Male sex, n (%) | 5 (50) | 20 (56) | 0.76 |
| Above federal poverty threshold, n (%) | 10 (100) | 24 (67) | 0.048* |
| Baseline scores | |||
| Full IQ (SD) | 110.1 (13.4) | 97.2 (14.4) | 0.014 |
| Listening comprehension (SD) | 97.9 (12.1) | 89.8 (10.0) | 0.036 |
| Oral expression (SD) | 94.5 (9.9) | 88.2 (14.8) | 0.21 |
| Reading (SD) | 115.0 (16.0) | 100.0 (10.5) | <0.001 |
| Writing (SD) | 113.2 (15.3) | 98.9 (12.5) | 0.004 |
| IEP/504 plans, n (%) | 5 (50) | 20 (56) | 0.75 |
| Speech therapy, n (%) | 2 (20) | 16 (44) | 0.27 |
| Behavioral issues, n (%) | 3 (30) | 13 (36) | 0.72 |
SD, standard deviation; IEP, Individualized Educational Plan
Mantel-Haenszel chi square P value
The data from the remaining 36 children without large slopes were then analyzed with multilevel random regression modeling to determine whether the IQ and language scores continued to increase significantly with time. In Table V, the scores for verbal IQ, OE and OC are shown to still increase, although the proportional within-person variance (pseudo R2) explained by time alone is greater than 10% for OE and OC scores only.
Table V.
Random regression (multilevel) models of the effect of time, defined as age at testing beginning at age 6 years, in 36 children with unilateral hearing loss who did not have qualitatively large increases of verbal IQ or Oral Expression scores.
| Outcome | Initial Status (SE) | Rate of Change (SE) | Pseudo R2 |
|---|---|---|---|
| Full IQ | 95.6 (2.7)*** | 1.20 (0.62) | 0.080 |
| Verbal IQ | 95.0 (2.9)*** | 1.65 (0.80)* | 0.078 |
| Performance IQ | 97.6 (3.0)*** | 0.29 (0.76) | 0.009 |
| Listening comprehension | 88.5 (2.8)*** | 1.20 (0.88) | 0.063 |
| Oral expression | 84.1 (2.7)*** | 2.48 (0.52)*** | 0.166 |
| Oral composite | 83.5 (3.0)*** | 2.21 (0.88)* | 0.153 |
Note: The Initial Status provides the model’s calculated mean baseline score at the age of 6 years. The Rate of Change indicates the slope of the change in scores over time (i.e., calculated change in score per year). The Pseudo R2 values provide the proportional within-person variance that is explained by the effect of time.
p<0.05,
p<0.01,
p<0.001
Parent-reported behavioral problems gleaned from the CBCL for all three years are summarized in Table VI for Syndrome, Competency, and DSM-oriented subscales. In general, the rate of clinically significant problems as assessed by the CBCL remained unchanged or decreased for most of the subscales. Parents noted clinically important attention, internalizing, externalizing and total problems, in 10% or more on the Syndrome scales during the final year. Clinically important problems on all four Competency scales affected 20% or more of the children in the final year of data collection.
Table VI.
Rates of children with unilateral hearing loss who had clinical problems on the Child behavioral checklist (CBCL), as reported by parents. Clinical problem for the Syndrome and DSM subscales is defined as those at or above the 98th percentile for the age group. Clinical problem for Competency subscales is defined as those at or below the third percentile for the age group.
| Year 1 n = 46 | Year 2 n = 46 | Year 3 n = 41 | P value* | |
|---|---|---|---|---|
| Syndrome subscales | ||||
| Anxious and depressed, n (%) | 5 (11) | 5 (11) | 2 (5) | 0.21 |
| Withdrawn and depressed, n (%) | 4 (9) | 1 (2) | 2 (5) | 0.35 |
| Somatic complaints, n (%) | 6 (14) | 5 (11) | 2 (5) | 0.23 |
| Social problems, n (%) | 8 (17) | 4 (9) | 1 (2) | 0.04 |
| Thought problems, n (%) | 7 (15) | 3 (7) | 3 (7) | 0.12 |
| Attention problems, n (%) | 10 (22) | 7 (16) | 4 (10) | 0.13 |
| Rule breaking behavior, n (%) | 4 (9) | 4 (9) | 2 (5) | 0.56 |
| Aggressive behavior, n (%) | 7 (15) | 3 (7) | 2 (5) | 0.12 |
| Internalizing problems, n (%) | 10 (22) | 9 (20) | 7 (17) | 0.32 |
| Externalizing problems, n (%) | 11 (24) | 6 (13) | 4 (10) | 0.13 |
| Total problems, n (%) | 12 (26) | 7 (16) | 5 (12) | 0.10 |
| Competency subscales | ||||
| Activities, n (%) | 8 (17) | 4 (9) | 8 (20) | 0.55 |
| Social, n (%) | 10 (22) | 6 (13) | 9 (22) | 0.82 |
| School, n (%) | 9 (20) | 10 (22) | 9 (22) | 0.66 |
| Total competencies, n (%) | 13 (18) | 9 (20) | 11 (27) | 0.99 |
| DSM subscales | ||||
| Affective problems, n (%) | 7 (15) | 3 (7) | 1 (2) | 0.02 |
| Anxiety problems, n (%) | 6 (13) | 5 (11) | 3 (7) | 0.28 |
| Somatic problems, n (%) | 9 (20) | 7 (15) | 5 (12) | 0.26 |
| ADHD problems, n (%) | 9 (20) | 6 (14) | 2 (5) | 0.08 |
| Oppositional defiance, n (%) | 8 (17) | 4 (9) | 3 (7) | 0.06 |
| Conduct problems, n (%) | 7 (15) | 4 (9) | 3 (7) | 0.36 |
Mantel-Haenszel chi square P value
School records and teacher narrative results for the children over three years are shown in Table VII. Similar to the parent-reported behavioral assessments, there were no significant changes in rates of academic difficulty. The school records showed that approximately 50% of the students had an IEP, 504 plan, or other individualized program for education, which is similar to the rate reported by parents through interview. Teachers noted that 24% of students had any academic weakness or area of concern on the report card narratives. Although not statistically significant, the percentage of children whose teachers expressed concerns about attention span and working independently trended toward an increase, with 24% of students having a weakness or area of concern in any executive function in the third year.
Table VII.
Rates of school-related performance problems or concerns in children with unilateral hearing loss, as documented in school records and teacher narrative reports.
| Year 1 n = 46 | Year 2 n = 46 | Year 3 n = 41 | P value* | |
|---|---|---|---|---|
| IEP/504 plan | 0.76 | |||
| IEP | 13 (30) | 15 (34) | 13 (32) | |
| 504 only | 5 (11) | 3 (7) | 4 (10) | |
| Diagnostic evaluation | 2 (5) | 0 | 2 (5) | |
| Homebound instruction | 1 (2) | 0 | 0 | |
| Individualized Service plan | 0 | 1 (2) | 1 (2) | |
| Weakness/Area of concern | ||||
| Reading | 13 (29) | 6 (14) | 8 (20) | 0.29 |
| Math | 6 (13) | 6 (14) | 5 (12) | 0.89 |
| Writing | 6 (13) | 4 (9) | 6 (15) | 0.83 |
| Spelling | 2 (4) | 0 | 0 | 0.09 |
| Any academics | 14 (30) | 9 (20) | 10 (24) | 0.49 |
| Behavior | 3 (7) | 10 (23) | 7 (18) | 0.15 |
| Social skills | 2 (4) | 8 (18) | 3 (8) | 0.59 |
| Fine motor skills | 1 (2) | 7 (16) | 4 (10) | 0.20 |
| Executive functions | ||||
| Attention | 4 (9) | 7 (16) | 9 (22) | 0.08 |
| Understand directions | 6 (13) | 4 (9) | 3 (8) | 0.37 |
| Organization skills | 1 (2) | 6 (14) | 4 (10) | 0.18 |
| Working slowly | 2 (4) | 3 (7) | 3 (8) | 0.56 |
| Completing assignments | 1 (2) | 1 (2) | 2 (5) | 0.47 |
| Working independently | 1 (2) | 3 (7) | 4 (10) | 0.13 |
| Any executive function | 8 (17) | 12 (26) | 10 (24) | 0.42 |
| Speech-language therapy | 9 (20) | 13 (30) | 9 (22) | 0.76 |
| Social work/counseling | 2 (5) | 6 (14) | 3 (8) | 0.58 |
| Occupational therapy | 4 (9) | 2 (5) | 1 (2) | 0.19 |
| Reading program | 3 (7) | 2 (5) | 4 (10) | 0.57 |
| Additional academic instruction | 3 (7) | 7 (16) | 6 (15) | 0.23 |
Mantel-Haenstzel chi square P value
Among the 13–15 children whose IEP documents were available for review each year, reasons for the individualized plan included hearing, language, speech, and health impairment; fine motor skills weakness; and specific learning disability. The services to be provided via the IEP varied considerably depending on the child’s needs, and included speech therapy, occupational therapy, special education classes, tutoring, and hearing accommodations. In year 1, hearing impairment was noted to be the reason for IEP in five children out of 13 (38%); this was similar for year 2 (six of 15 children, or 40%), and for year 3 (seven of 13 children, or 54%). Other reasons for an IEP were noted for 10 of 13 (77%) in year 1, 8 of 15 (53%) in year 2, and 7 of 13 (54%) in year 3. Some children had multiple reasons for an IEP. The IEP teams often did not include an audiologist, teacher for the deaf/hard of hearing, or itinerant teacher for the hearing impaired; only one, six, and five children had such hearing professionals on their IEP teams during years 1, 2, and 3, respectively. Six children used an FM system in year 1, eight in year 2, and nine in year 3 of the study. Two children used a hearing aid in year 1, four in year 2, and one in year 3.
DISCUSSION
The children with UHL in this study began with low average scores in oral language skills, but improved significantly over time. These increases over time may be interpreted in at least one of three ways. The first possible interpretation is that of “catch-up,” where children with UHL improved their oral language skills at a quicker rate than their age-matched peers. Because age-adjusted standardized scores were used to measure cognitive and language skills, mean scores normally would be expected to stay about the same, with means of 100 and SD of 15, from year to year. However, statistical norms are created using cross-sectional data in large groups of participants, and do not necessarily reflect the longitudinal developmental changes within individual children. The second possible interpretation is that the increase of scores represent statistical regression to the mean in children who began with low scores, especially in oral language, due to variability in test taking.26 The third possible explanation for the improvement in scores is the phenomenon of practice effects, which refers to gains in scores on tests when a person is retested on the same or very similar instruments.27 This practice effect improvement has been reported to be 3 to 11 points at 3-to-6 month intervals for the Wechsler Adult Intelligence Scale (WAIS), with similar gains documented for other cognitive tests for children and adolescents.28, 29 Because children with NH were not included in this longitudinal study as controls, the possibility that practice effects contribute to the present results cannot be ruled out.
The improvement in verbal IQ scores among those who received IEPs suggests that when children with UHL are identified to have educationally-significant problems through the schools, the intervention associated with the IEP may be sufficient to increase language scores. In addition, the cognitive level of the child may modify the increase in language skills, as demonstrated in Figure 1. Indeed, the characteristics of the children with the largest increases of language and verbal IQ scores demonstrate that those with greater cognitive resources may compensate for their UHL and overcome the initial delays in language. As Table V demonstrates, the increase of OE scores appears to be robust, with a predicted increase of nearly 15 points over a six-year period.
However, increases in language scores do not appear to be sufficient to improve academic performance, with half of the cohort still receiving IEPs at the last follow-up, and no decrease in the rate of behavioral problems reported by teachers. In addition, achievement scores showed no increase over time. The rate of IEPs in this cohort is about quadruple the national rate (12.3%) as of 2007,30 and the majority of these children received IEPs for reasons other than their hearing impairment. Theoretically, 100% of children with UHL should receive IEPs to provide accommodations for hearing disability; having only one functional eye or hand is not challenged as being a disability. However, the persistently high rate of IEPs for non-hearing reasons suggests that educational problems do not resolve easily, and a lack of hearing professionals on IEP teams might explain why schools seem to ignore UHL as a contributing factor to school performance.
Another important caveat to the improved language scores is the persistence of parent-and teacher-identified problems in school. Parents reported clinically important problems with School, social, and Activities Competencies in ≥ 20% of the cohort during the final year of data collection. Parents also noted that ≥ 10% of children had clinically important problems with attention, internalizing and externalizing problems on the Syndrome scales. Similarly, teachers expressed concern about attention in 22%, organizational skills in 10%, and working independently in 10% during the final year. Almost one-quarter of students had persistent weaknesses with any academic area. Although these reports are subjective and not easily quantifiable, the overall and academic development of these children with UHL appears delayed compared with their peers with NH.
A major limitation of this study is that a control group was not followed longitudinally. Without controls, whether the improvements in standardized verbal IQ, full IQ, and OE and OC scores are unique to children with UHL or common to typically-developing children regardless of hearing status cannot be confirmed. Because standardization of scores implicitly requires age-based comparison of outcomes, we had assumed that assessment of standard scores in our cohort would allow indirect comparison with other typically-developing children. However, since standardization of scores is done with cross-sectional studies rather than longitudinal, the expected change in longitudinal scores in NH children, taking practice effects into account, is not known. Yet the baseline (year 1) standardized scores of the children in the present study were similar to those of children with UHL in a previous case-control study,13 so at least the initial assessment scores appear comparable.
Another limitation is that the participants were followed for only three years, until a mean age of 9.7 years. Because they were not followed into adolescence, it is not known whether these children will achieve the same level of language proficiency at a delayed time point. Since oral language skills have been linked to reading proficiency and literacy in deaf children, a delay in oral language skills can impede a child’s ability to use reading as a tool to learn and acquire new knowledge.31, 32 A delay in achieving expected levels of language skill in adolescence would be preferable to never achieving proficiency or having disordered language skills. Yet it is still unclear whether increased language proficiency, albeit at a delayed time point, would produce comparable improvements in educational outcome. At the final assessment of this study, teachers and schools did not note appreciable decreases in academic problems.
A majority of this cohort had severe-to-profound UHL, thus the results may not be generalizable to children with mild-to-moderate hearing loss. Because some children received heterogeneous duration and quality of amplification through the use of hearing aids or FM systems, it is uncertain whether the improvement in scores could be partially attributable to aural rehabilitation. However, in one small study, children with mild-to-moderate UHL reported marked qualitative benefits from using digital hearing aids in school.33 While improvements in school performance were not documented in that study, the duration of follow-up (3 months) was likely too short to measure any difference. A controlled study of amplification in children with UHL will be necessary to demonstrate clear benefit to language and educational performance outcomes.
The public health and health policy significance of these findings are tied to the inconsistent determination that UHL is a “significant hearing loss” in the U.S. and across the globe. In the United Kingdom, permanent hearing loss in children is defined as bilateral hearing loss ≥ 40 dB.34, 35 In the U.S., eligibility for services under Part B and Part C of the Individuals with Disabilities Education Improvement Act (IDEA) of 2004 is determined by each state, and children with UHL often do not qualify. Thus, children with UHL are not automatically eligible for Early Intervention through the First Steps or Birth to Three programs (Part C of IDEA), or preschool or school IEPs (Part B of IDEA), as are children with bilateral hearing loss.36, 37 Even though hearing impairment was included among the reasons for an IEP, other educationally important diagnoses were common in this cohort, and many children did not receive hearing assistance through the provision of an FM system at school.
Although children with UHL usually do not display obvious deficits in language and communication, the problems they face have been documented repeatedly. Some have even speculated that their “invisibility” and the lack of acknowledgement by educators, physicians and others that UHL can impair hearing has resulted in poorer school performance than in children with bilateral moderate hearing loss who receive special services.38, 39 Using functional MRI and functional connectivity MRI scans, investigators have demonstrated neuroanatomical differences between children with UHL and NH controls.40, 41 These differences involved not only auditory regions, but also attention and executive control regions, and may explain why a seemingly minor decrease in hearing would lead to increased language and educational problems.
While many children with UHL in this study displayed speech-language delays and educational performance problems that led to speech therapy and IEPs, clearly not all children with UHL have such issues. Instead, many compensate very well, and to them UHL may merely be a nuisance when trying to communicate in noisy backgrounds. Differentiating children who require help to achieve expected speech and school performance from those who need no such help would be an important investigational next step. Identifying and developing interventions that ameliorate or eliminate these problems would be another area of future research. These interventions may include early intervention in infants or toddlers, amplification, auditory rehabilitation, and perhaps cognitive training.
CONCLUSIONS
Children with UHL in this study demonstrated improvement in standardized oral language scores and verbal IQ over time. This improvement may be attributable to “catch-up,” regression to the mean, or practice effects, so the clinical significance is uncertain. Predictors of increased scores included receipt of IEPs and higher baseline cognitive levels. These increases in language and verbal IQ scores were not accompanied by improvements in achievement test scores or school performance, however. Notably, 27% scored at or below the third percentile on CBCL total competency scale, and teachers reported weaknesses or concerns with academic or executive function skills in about one-quarter. They suggest persistent delays in overall and academic development in children with UHL compared to children with NH. Further studies in older children and adolescents are needed to determine whether the effects of UHL extend into pursuit of higher education and occupations.
Acknowledgments
Funding: This study was supported by NIH grants K23 DC006638 and UL1RR024992.
Abbreviations used
- UHL
unilateral hearing loss
- NH
normal hearing
- HL
hearing level
- PTA
pure tone average
- FPL
federal poverty level
- OWLS
Oral and Written Language Scales
- LC
Listening Comprehension
- OE
Oral Expression
- OC
Oral Composite
- IQ
intelligence quotient
- WRS
word recognition scores
Footnotes
Conflict of Interest: None
Presentation: This work will be presented at The Triological Society 115th Annual Meeting, San Diego, California, USA, April 20, 2012. It is a co-recipient of the Mosher Award for Triological Thesis.
Level of Evidence: 1b, Individual prospective cohort study
References
- 1.Oyler RF, Oyler AL, Matkin ND. Warning: a unilateral hearing loss may be detrimental to a child’s academic career. Hear J. 1987;40(9):18–22. [Google Scholar]
- 2.Barsky-Firkser L, Sun S. Universal newborn hearing screenings: a three-year experience. Pediatrics. 1997;99(6):E4. doi: 10.1542/peds.99.6.e4. [DOI] [PubMed] [Google Scholar]
- 3.Finitzo T, Albright K, O’Neal J. The newborn with hearing loss: detection in the nursery. Pediatrics. 1998;102(6):1452–60. doi: 10.1542/peds.102.6.1452. [DOI] [PubMed] [Google Scholar]
- 4.Mehra S, Eavey RD, Keamy DG., Jr The epidemiology of hearing impairment in the United States: newborns, children, and adolescents. Otolaryngol Head Neck Surg. 2009;140(4):461–72. doi: 10.1016/j.otohns.2008.12.022. [DOI] [PubMed] [Google Scholar]
- 5.Shargorodsky J, Curhan SG, Curhan GC, Eavey R. Change in Prevalence of Hearing Loss in US Adolescents. JAMA. 2010;304(7):772–8. doi: 10.1001/jama.2010.1124. [DOI] [PubMed] [Google Scholar]
- 6.Bess FH, Tharpe AM. Unilateral hearing impairment in children. Pediatrics. 1984;74(2):206–16. [PubMed] [Google Scholar]
- 7.Keller WD, Bundy RS. Effects of unilateral hearing loss upon educational achievement. Child Care Health Dev. 1980;6(2):93–100. doi: 10.1111/j.1365-2214.1980.tb00801.x. [DOI] [PubMed] [Google Scholar]
- 8.Oyler RF, Oyler AL, Matkin ND. Unilateral hearing loss: demographics and educational impact. Language, Speech and Hearing Services in Schools. 1988 Apr;19:201–10. [Google Scholar]
- 9.Lieu JE. Speech-language and educational consequences of unilateral hearing loss in children. Arch Otolaryngol Head Neck Surg. 2004;130(5):524–30. doi: 10.1001/archotol.130.5.524. [DOI] [PubMed] [Google Scholar]
- 10.Bess FH. The unilaterally hearing-impaired child: a final comment. Ear Hear. 1986;7(1):52–4. doi: 10.1097/00003446-198602000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Borg E, Edquist G, Reinholdson AC, Risberg A, McAllister B. Speech and language development in a population of Swedish hearing-impaired pre-school children, a cross-sectional study. Int J Pediatr Otorhinolaryngol. 2007;71(7):1061–77. doi: 10.1016/j.ijporl.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 12.Klee TM, Davis-Dansky E. A comparison of unilaterally hearing-impaired children and normal-hearing children on a battery of standardized language tests. Ear Hear. 1986;7(1):27–37. doi: 10.1097/00003446-198602000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Lieu JE, Tye-Murray N, Karzon RK, Piccirillo JF. Unilateral hearing loss is associated with worse speech-language scores in children. Pediatrics. 2010;125(6):e1348–e1355. doi: 10.1542/peds.2009-2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peckham CS, Sheridan MD. Follow-up at 11 years of 46 children with severe unilateral hearing loss at 7 years. Child Care Health Dev. 1976;2(2):107–11. doi: 10.1111/j.1365-2214.1976.tb00865.x. [DOI] [PubMed] [Google Scholar]
- 15.Woodcock K, Pole JD. Educational attainment, labour force status and injury: a comparison of Canadians with and without deafness and hearing loss. Int J Rehabil Res. 2008;31(4):297–304. doi: 10.1097/MRR.0b013e3282fb7d4d. [DOI] [PubMed] [Google Scholar]
- 16.Teasdale TW, Sorensen MH. Hearing loss in relation to educational attainment and cognitive abilities: a population study. Int J Audiol. 2007;46(4):172–5. doi: 10.1080/14992020601089484. [DOI] [PubMed] [Google Scholar]
- 17.Dalton DS, Cruickshanks KJ, Klein BE, Klein R, Wiley TL, Nondahl DM. The impact of hearing loss on quality of life in older adults. Gerontologist. 2003 Oct;43(5):661–8. doi: 10.1093/geront/43.5.661. [DOI] [PubMed] [Google Scholar]
- 18.Tambs K. Moderate effects of hearing loss on mental health and subjective well-being: results from the Nord-Trondelag Hearing Loss Study. Psychosom Med. 2004;66(5):776–82. doi: 10.1097/01.psy.0000133328.03596.fb. [DOI] [PubMed] [Google Scholar]
- 19.Giolas TG, Wark DJ. Communication problems associated with unilateral hearing loss. J Speech Hear Disord. 1967;32(4):336–43. doi: 10.1044/jshd.3204.336. [DOI] [PubMed] [Google Scholar]
- 20.Newman CW, Jacobson GP, Hug GA, Sandridge SA. Perceived hearing handicap of patients with unilateral or mild hearing loss. Ann Otol Rhinol Laryngol. 1997;106(3):210–4. doi: 10.1177/000348949710600305. [DOI] [PubMed] [Google Scholar]
- 21.Federal Register. Annual update of the HHS poverty guidelines. Federal Register. 2005 Feb 18;70(33):8373–5. [Google Scholar]
- 22.Wechsler D. [Accessed 5-15-2009];Wechsler Abbreviated Scale of Intelligence™ (WASI™) Available at URL: http://www.pearsonassessments.com/HAIWEB/Cultures/en-us/Productdetail.htm?Pid=015-8981-502.
- 23.Wechsler D. [Accessed 6-23-2011];Wechsler Individual Achievement Test. (2). (WIAT-II). Available at URL: http://www.pearsonassessments.com/HAIWEB/Cultures/en-us/Productdetail.htm?Pid=015-8983-505.
- 24.Carrow-Woolfolk E. Oral and written language scales (OWLS): Listening Comprehension and Oral Expression Manual. Minneapolis, MN: NCS Pearson Inc; 1995. [Google Scholar]
- 25.Achenbach TM. Child behavior checklist, ASEBA. Manual. 2003 Jan 10; [Google Scholar]
- 26.Bland JM, Altman DG. Statistics Notes: Some examples of regression towards the mean. BMJ. 1994;309(6957):780. doi: 10.1136/bmj.309.6957.780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaufman AS. Practice effects. In: Sternberg RJ, editor. Encyclopedia of human intelligence. New York: Macmillan Publishing Company; 1994. pp. 828–33. [Google Scholar]
- 28.Slade PD, Townes BD, Rosenbaum G, et al. The serial use of child neurocognitive tests: development versus practice effects. Psychol Assess. 2008;20(4):361–9. doi: 10.1037/a0012950. [DOI] [PubMed] [Google Scholar]


