Abstract
Objectives
To determine whether cognitive behavioral social skills training (CBSST) is an effective psychosocial intervention to improve functioning in older consumers with schizophrenia, and whether defeatist performance attitudes are associated with change in functioning in CBSST.
Design
An 18-month, single-blind, randomized controlled trial.
Setting
Outpatient clinic at a university-affiliated Veterans Affairs hospital.
Participants
Veteran and non-veteran consumers with schizophrenia or schizoaffective disorder (N=79) age 45–78.
Interventions
CBSST was a 36-session, weekly group therapy that combined cognitive behavior therapy with social skills training and problem solving training to improve functioning. The comparison intervention, goal-focused supportive contact (GFSC), was supportive group therapy focused on achieving functioning goals.
Measurements
Blind raters assessed functioning (primary outcome: Independent Living Skills Survey) CBSST skill mastery, positive and negative symptoms, depression, anxiety, defeatist attitudes, self-esteem, and life satisfaction.
Results
Functioning trajectories over time were significantly more positive in CBSST than in GFSC, especially for participants with more severe defeatist performance attitudes. Greater improvement in defeatist attitudes was also associated with better functioning in CBSST, but not GFSC. Both treatments showed comparable significant improvements in amotivation, depression, anxiety, positive self-esteem and life satisfaction.
Conclusions
CBSST is an effective treatment to improve functioning in older consumers with schizophrenia, and both CBSST and other supportive goal-focused interventions can reduce symptom distress, increase motivation and self esteem, and improve life satisfaction. Participants with more severe defeatist performance attitudes may benefit most from cognitive behavioral interventions that target functioning.
The number of older consumers with schizophrenia, like the number of older persons in the general population, is growing rapidly. By 2020, 41% of the United States population will be over age 45(1). This will mean a dramatic increase in demand for treatments targeting the unique needs of older consumers with schizophrenia. Aging in schizophrenia is typically associated with improvement in positive symptoms and reduced hospitalization, but impairments in functioning persist (1). Medications that reduce positive symptoms do not improve daily life functioning. It has become a national research priority to identify treatments to improve community role functioning and quality of life in people with severe mental illnesses (2). Evidence-based psychosocial interventions that improve functioning have been identified and recommended in best practice guidelines, but these practices are rarely available to most people with schizophrenia, especially older consumers (3). There has been very little research on psychosocial interventions for older consumers with schizophrenia (4–8).
Cognitive behavioral therapy (CBT) and social skills training (SST) are effective interventions to improve functioning in schizophrenia. A meta-analysis of 35 CBT clinical trials (9) recently showed that, although the vast majority of studies focused on positive symptoms as the primary treatment target, CBT also had beneficial impact on functioning. Fifteen of the studies reviewed included functioning measures and the average effect size for improvement in functioning (d=0.38) and negative symptoms (d=0.44) was comparable to that for positive symptoms (d=0.37). Numerous studies of consumers with schizophrenia have also shown that SST improves functioning (10, 11). A meta-analysis of 22 SST trials (11) found a large effect size for proximal content-mastery outcomes (d=1.20), moderate effect sizes for intermediate outcomes, including performance-based measures of social and daily living skills (d=0.52), community functioning (d=0.52), and negative symptoms (d=0.40), and small effect sizes for more distal outcomes, like other symptoms (d=0.15) and relapse (d=0.23).
Given the established efficacy of CBT and SST in schizophrenia trials, we developed a group therapy intervention that combined these two treatments called, Cognitive Behavioral Social Skills Training (CBSST) (12, 13). By adding CBT to SST, thoughts that interfere with skill performance in the real world (e.g., low self-efficacy, defeatist performance attitudes) can be addressed in therapy. CBSST was specifically designed to help older people with schizophrenia attain personalized functioning goals. In a prior clinical trial (6, 14), we randomized 76 people with schizophrenia or schizoaffective disorder (M age = 54) to treatment as usual (TAU) or CBSST. Participants in CBSST showed significantly greater CBSST skill mastery on (d=.61) and functioning (d=.50) relative to participants in TAU, and these improvements were maintained at one-year follow-up (14). This trial showed that CBSST was more effective than TAU, but did not control for nonspecific therapist contact. We, therefore, conducted the present trial comparing CBSST with an active psychosocial control condition, goal-focused supportive contact (GFSC). GFSC was an enhanced supportive contact intervention focused on helping consumers set and work toward functioning goals in a support group that provided the same amount of therapist and group contact as CBSST.
To strengthen the efficacy of interventions like CBSST and identify consumers most likely to benefit from such interventions, it is important to identify potential moderators and mechanisms of change. Several researchers (15–18) recently found that defeatist performance attitudes (e.g., “Why bother, I always fail,” “It’s not worth the effort”) are associated with poor functioning and negative symptoms in schizophrenia. Rector et al. (18) proposed that defeatist attitudes about the personal costs of applying energy toward goal-directed tasks can lead to passivity and avoidance of activities that require effort, as a defense against anticipated failure and negative evaluations by others. The premise that defeatist beliefs can influence real world functioning behavior is a key component of the cognitive model that guides CBT, and CBT interventions are uniquely designed to challenge and change defeatist attitudes that may contribute to poor functioning in schizophrenia. Consumers with more severe defeatist beliefs, therefore, may be more likely to benefit from CBT that target functioning, and reduction in severity of defeatist attitudes may mediate improvements in functioning in CBT.
The present study was a randomized controlled trial comparing CBSST with GFSC in middle-aged and older consumers with schizophrenia or schizoaffective disorder. The aims of the study were to determine whether: (1) CBSST is effective compared to an active psychosocial intervention that controls for therapist contact and incorporates recovery-oriented goal-setting interventions; (2) defeatist attitudes at the beginning of treatment moderate treatment outcomes; and (3) reduction in defeatist attitudes during treatment mediate treatment outcome. The primary hypothesis was that self-reported everyday functioning would be significantly greater in CBSST relative to GFSC. We also hypothesized that people with greater severity of defeatist attitudes would show better functioning outcomes in CBSST than in GFSC, and that reduction in severity of defeatist attitudes during CBSST would mediate improvements in functioning.
Methods
Design
All study procedures were approved by the institutional review board of the University of California, San Diego. After informed consent and baseline assessments, participants were randomly assigned by an independent statistician to one of two treatment conditions: CBSST or GFSC. Participants were then treated for 9 months and followed longitudinally for 9 months after treatment, with baseline, 4.5-month (mid-treatment), 9-month (end-of-treatment), 13.5-month (mid-follow-up) and 18-month follow-up assessments. Assessors were blind to treatment allocation. Participants received compensation for completing assessment visits, but not for attending treatment sessions. Transportation was offered to participants for all group therapy and assessment visits, because transportation is often a challenge for older adults with schizophrenia.
Participants
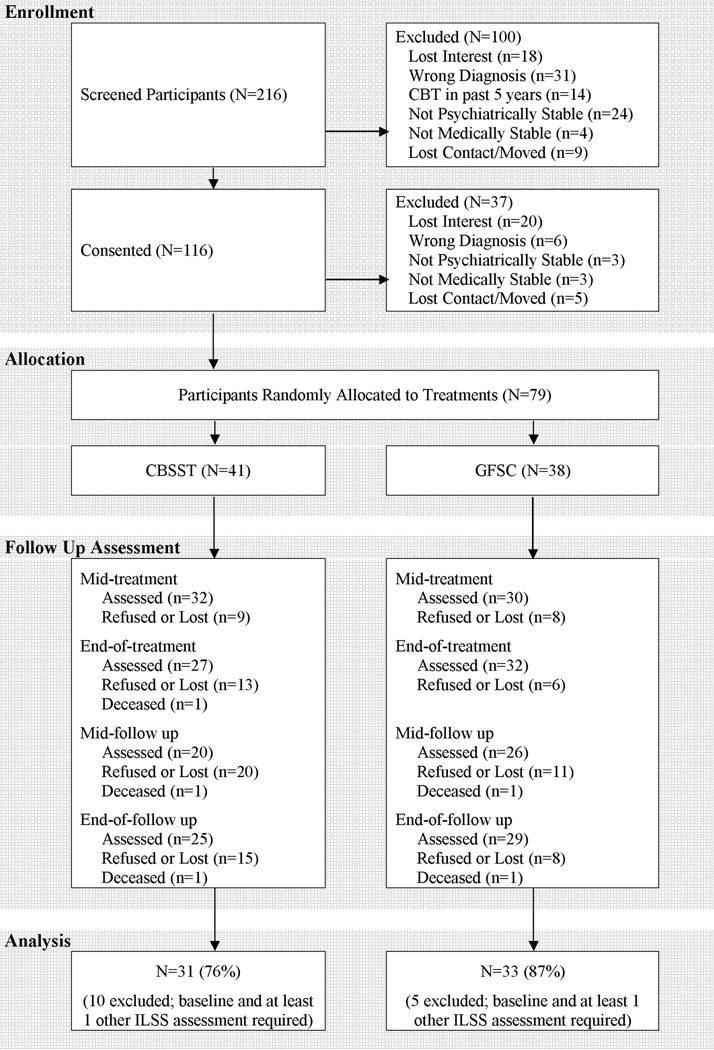
Community-dwelling veteran (N=27) and non-veteran (N=52) consumers with schizophrenia or schizoaffective disorder (N=79) over age 45 were enrolled, but 15 participants without valid assessments on the primary outcome measure (Independent Living Skills Survey) at baseline and at least one post-baseline assessment were excluded (final sample N=64; see Figure 1). Participants were recruited from outpatient residential and treatment settings in the Veterans Affairs an Diego Healthcare System, University of California, San Diego Medical Center Outpatient Psychiatry Services, and the San Diego County Mental Health System from 2005–2008. All participants met diagnostic criteria for schizophrenia or schizoaffective disorder based on the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (SCID–I) (19) and available medical record review. Diagnoses of schizophrenia included 41 paranoid, 18 undifferentiated, 2 disorganized, 3 residual, and 15 schizoaffective disorder. Exclusion criteria consisted of prior exposure to CBT during the previous five years, level of care required at baseline that would interfere outpatient therapy groups (e.g., hospitalization for medical, psychiatric, or substance abuse problems), or disabling medical problems that would interfere with therapy or testing. At baseline, 55 consumers reported at least one first generation antipsychotic medication, 29 at least one second generation antipsychotic, 15 both types of antipsychotics, and 4 reported no antipsychotic medications. Forty-two consumers also reported antidepressant medications, and 20 reported mood-stabilizers.
Figure 1.
Flow of older consumers with schizophrenia or schizoaffective disorder through an 18-month randomized controlled trial comparing cognitive behavioral social skills training (CBSST) with a goal focused supportive contact (GFSC) control treatment.
Interventions
Cognitive Behavioral Social Skills Training (CBSST)
CBSST integrates CBT and SST techniques to target the different factors that contribute to poor functioning (6,12,13,20). CBSST is a group therapy intervention delivered in three, six-session modules that are intended to be completed twice, for a total of 36 weekly sessions (9 months). The three modules are Thought Challenging, Social Skills Training, and Problem-Solving Training. Each group therapy session was two hours, with a lunch or snack break mid-way. Cognitive therapy was combined with role-play practice of communication skills and problem-solving training. The CBSST treatment manual included a participant workbook that describes the skills and includes homework assignment forms. Each group session was facilitated by two doctoral-level or masters-level therapists with at least two years of CBT experience. The same therapists delivered CBSST and GFSC. Two of us (E.G., J.R.M.) provided training and weekly supervision, including review of session videotapes.
In the Thought Challenging Module, cognitive therapy was the exclusive focus, but thought challenging was also used throughout the other two modules. The cognitive interventions were not strongly formulation or schema based, rather cognitive therapy components were focused on the practice of simplified thought challenging skills and behavioral experiment activities. Thought challenging skills were used to address symptoms and challenge defeatist beliefs that interfere with functioning behaviors, including expectancies (“It won’t be fun”), self-efficacy beliefs (“I always fail”), and ageist beliefs (e.g., “I’m too old to change”), as well as anomalous beliefs (“Spirits will harm me”). Group members were introduced to the general concepts of CBT, including the relationship between thoughts, actions and feelings (generic cognitive model), automatic thoughts, thought challenging through behavioral experiments and examining evidence for beliefs, and mistakes in thinking. The primary thought challenging skill trained was the 3C’s: Catch It, Check It, Change It (“It” is an unhelpful thought).
The primary goal of the Social Skills Training module was to improve communication skills through behavioral role plays. Important role-plays included age-relevant situations (e.g., talking to a doctor about obtaining eyeglasses), interacting with roommates, friends and family, making new friends, and effectively interacting with case managers, doctors, and other service providers and support persons.
Basic problem-solving skills were trained in the Problem-Solving Module using the acronym, SCALE – Specify the problem, Consider all possible solutions, Assess the best solution, Lay out a plan, and Execute and Evaluate the outcome. The focus was on developing specific and feasible plans to solve real-world problems, including scheduling pleasant activities, improving living situations, finances, using public transportation, finding a volunteer or paid job, enrolling in classes, and getting glasses or a hearing aid.
The primary targets of the intervention were different in each module, but defeatist attitudes and other thoughts that could be obstacles to goal achievement were targeted in each module. In the thought challenging module, defeatist attitudes were the primary target, but delusional beliefs and beliefs about voices were targeted only if they interfered with functional goal achievement (e.g., voices saying not to go out). In the social skills training module, effective communication and assertiveness skills were the primary target, but defeatist attitudes were addressed in the context of social role plays (e.g., expectations for success in communications). In the problem-solving module, making plans to take steps toward functional goal achievement was the primary target, but defeatist attitudes were addressed in the context of executing plans (e.g., low self efficacy beliefs).
Goal-Focused Supportive Contact (GFSC)
This active psychosocial control condition provided the same frequency (weekly) and amount (36 2-hr. sessions) of therapist and other group member contact as CBSST. The GFSC intervention was enhanced supportive contact that included a primary focus, like CBSST, on setting and achieving functioning goals (e.g., living, learning, working and socializing). Sessions were semi-structured and consisted of check-in about symptoms and potential crisis management, followed by a flexible discussion about setting and working toward functioning goals. Sessions typically included components of psychoeducation, empathy, and non-directive reinforcement of health, coping, and symptom management behaviors, that grew out of group discussions, with minimal therapist guidance.
Outcome Measures
Functioning (primary outcome)
Self-reported functioning was assessed using the Independent Living Skills Survey (ILSS) (21). The ILSS is a 51-item, self-report measure which was administered in an interview format to assess ten domains of functioning (e.g., hygiene, cooking, cleaning, health maintenance, money management, socialization, leisure activities, work, school). According to standard scoring procedures, items were scored 0 (not performed), 1 (performed) or “Not Able to Demonstrate” (e.g., for food preparation items when meals were provided by assisted living staff), and the average of available items was computed for each domain (domain scores were not computed if more than half the items were missing or scored “Not Able to Demonstrate”). The average of available domain scores was used in all analyses (range = 0–1; minimum of seven domains required).
Defeatist Attitudes (mediator/moderator)
The Defeatist Performance Attitude Scale (DPAS) is a 15-item self-report subscale derived from factor analysis of the commonly-used Dysfunctional Attitude Scale (22–24). The DPAS indexes endorsement of defeatist attitudes about one’s ability to perform goal-directed tasks (e.g., “If you cannot do something well, there is little point in doing it at all”, “If I fail at my work, then I am a failure as a person,” “People will probably think less of me if I make mistakes and fail”). Items are rated on a 1–7 Likert scale and higher total scores (range = 15–105) indicate more severe defeatist performance attitudes.
Secondary Outcomes
The Comprehensive Module Test (CMT) was used to assess CBSST skills acquisition. The CMT was originally developed for use with SST modules (25) to assess factual knowledge about skills and the application of skills in vignettes, and was adapted for this study to assess mastery of the specific content trained in CBSST (CMT total range = 0–33). The Positive and Negative Syndrome Scale (PANSS) (26), Scale for the Assessment of Negative Symptoms (SANS) (27), Beck Depression Inventory – 2nd Edition (BDI-II) (28), and Beck Anxiety Inventory (BAI) (29) were administered to assess clinical symptoms. Based on factor analytic studies of the SANS (30–32), two negative symptom factors were derived: Diminished Expression, defined as the average of Affective Flattening and Alogia global ratings (items 8, 13); and Diminished Motivation, defined as the average of Avolition-Apathy and Anhedonia-Asociality global ratings (items 17, 22). The Self-Esteem Rating Scale-Short Form (SERS) 33) is a 20-item self-report scale. The Positive and Negative Self-Esteem subscale scores were included in the analyses. Finally, overall life satisfaction was assessed using the Life Satisfaction Index (LSI) (34), which measures components of well-being on several dimensions (e.g., zest vs. apathy, self-concept, optimism) in later life.
Reliability
Assessors received training using videotape and practice interviews and did not complete assessments until achieving at least .80 inter-rater reliability. Inter-rater reliability (interclass correlation) was .88 for PANSS total, .87 for PANSS positive, and .83 for SANS total.
Blind Ratings
Raters were blind to treatment group membership. To assess the blind, raters guessed which treatment arm participants were in before completing assessments using a 7-point scale (1=Definitely GFSC; 2=Most Likely GFSC; 3=Maybe GFSC; 4=Neutral/Unsure Either Way; 5=Maybe CBSST; 6=Most Likely CBSST; 7=Definitely CBSST). Only 6 end of treatment assessments and 8 6-month follow-up assessments were rated “most likely” or “definitely” CBSST or GFSC, and 6 of these 14 group membership guesses were wrong. Raters were, therefore, either unsure about group membership or their guesses were at chance, suggesting the blinding of raters was successful.
Statistical Analyses
Growth curve models using mixed-effects regression modeling (HLM v6.06) to predict each outcome variable were estimated using time (in months centered at baseline) as a level-1 predictor and group (coded CBSST = 0.5; GFSC = −0.5) as a level-2 predictor of both the slope and intercept parameters. To examine whether defeatist attitudes moderated outcome for functioning (ILSS) and negative symptoms (SANS factors), baseline DPAS (centered at the median value) and the interaction between baseline DPAS and treatment group were included as predictors of the slope and intercept in the models predicting ILSS and SANS factors. In addition, to control for associations between negative symptoms, defeatist attitudes and functioning (15–18), baseline SANS total (sum of factor scores) was also included as a covariate in the ILSS model. The model for ILSS initially showed a significant group effect (parameter estimate = −0.05, t(70)= −2.45, p=.017), indicating the treatment groups differed significantly on the primary outcome variable at baseline. We, therefore, also included baseline ILSS as a covariate in the final ILSS model, which required that only participants with baseline and at least one other ILSS assessment were included. Finally, to examine whether change in defeatist attitudes (DPAS) during treatment mediated change in functioning (ILSS) and negative symptom (SANS factors) outcomes, linear regressions were computed using change in DPAS from baseline to end of treatment and baseline scores on the outcome measure as predictors of ILSS and SANS factor score at 18-month assessments.
Results
Sample
The flow of participants through the 18-month protocol is shown in Figure 1. After dropout and exclusion of participants for missing data, 81% of randomized participants were included in analyses. The groups did not differ significantly in dropout rates at any assessment point. The average age of the final sample at baseline was 55.0 (SD=6.6; range =46–78). The majority of the participants were Caucasian (66%), male (55%), unmarried (95%), with a high school education (M years of education =12.5; SD=2.0), and living in assisted community housing (69%). The treatment groups did not differ significantly on any of these demographic variables. The sample had, on average, only moderate symptom severity (PANSS total M= 64.7, SD=19.1).
Treatment Adherence and Fidelity
On average, participants in CBSST attended 83% of the 36 group therapy sessions offered and participants in the GFSC attended 82%. The mean number of sessions attended did not differ significantly between the two treatment groups (CBSST M= 30.3, SD= 12.3 range =3 to 45; GFSC: M=29.6, SD=13.2 range =0 to 44; t(62)=0.23, p =.816).
All therapy sessions were videotaped and the Cognitive Therapy Rating Scale for Psychosis (CTS-Psy; Haddock et al., 2001) was used to rate fidelity from 24 randomly-selected sessions (stratified by treatment group and CBSST module). Therapists were blind to which sessions would be rated. Fidelity ratings were completed by expert raters from the Psychopathology Research Unit directed by Dr. Aaron T. Beck at the University of Pennsylvania, Philadelphia. The CTS-Psy total was significantly greater in CBSST (M=37.8, S.D.=8.1) relative to GFSC (M=17.6, S.D.=3.1), t(22)=6.39, p<.001. The total CTS-Psy for CBSST, but not for GFSC, was above the recommended cutoff for competent CBT for psychosis (>=30; Haddock et al., 2001). In particular, the total CTS-Psy rating for subscales measuring specific CBT components was significantly greater for CBSST than for GFSC (sum of Agenda, Feedback, Guided Discovery, Focus on Key Cognitions, Choices of Intervention, and Homework subscales: CBSST M=22.7, S.D.=6.4; GFSC M=3.1, S.D.=4.5; t(22)=7.34, p < .001), but the treatment groups did not differ significantly in nonspecific therapist characteristics (sum of Interpersonal Effectiveness, Understanding, and Collaboration subscales: CBSST M=15.1, S.D.=3.2; GFSC M=14.4, S.D.=4.5; t(22)=0.43, p=.671). Therefore, the two treatments, which were delivered by the same therapists, had comparable nonspecific supportive components, but specific CBSST components did not slip into the GFSC condition.
Outcome
Descriptive statistics for each outcome are shown in Table 1 and results from mixed-effects regression modeling are presented in Tables 2 and 3. Significant group by time interactions were found for ILSS (primary functioning outcome; Table 1) and CMT (Table 2), indicating significantly greater increase in functioning and skills acquisition for CBSST than for GFSC. In addition, the effect of time, but not the group by time interaction, was significant for SANS Diminished Motivation, BAI, BDI-II, LSI, and SERS Positive, indicating significant improvements in negative symptoms, anxiety, depression, life satisfaction and positive self esteem in both treatments, but improvements in CBSST were not significantly greater than improvements in GFSC for these secondary outcomes.
Table 1.
Descriptive statistics for all outcome measures at each assessment point for each treatment group
| Baseline | Mid-Treatment (4.5 mos.) | End of Treatment (9 mos.) | Mid-Follow Up (13.5 mos.) | Follow Up (9 mos.) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | M (SD) | N | M (SD) | N | M (SD) | N | M (SD) | N | M (SD) | ||
| ILSS | CBSST | 31 | 0.66 (0.09) | 29 | 0.68 (0.10) | 26 | 0.69 (0.07) | 18 | 0.68 (0.07) | 25 | 0.71 (0.07) |
| GFSC | 33 | 0.70 (0.11) | 30 | 0.71 (0.10) | 32 | 0.71 (0.11) | 26 | 0.72 (0.12) | 29 | 0.68 (0.13) | |
| CMT | CBSST | 31 | 6.2 (3.6) | 30 | 8.6 (5.6) | 26 | 12.0 (7.1) | 19 | 10.5 (4.8) | 24 | 11.2 (7.2) |
| GFSC | 33 | 4.8 (3.3) | 30 | 6.2 (5.1) | 32 | 5.5 (4.1) | 26 | 6.3 (4.3) | 28 | 5.8 (3.8) | |
| PANSS Positive |
CBSST | 31 | 18.3 (8.1) | 29 | 17.4 (6.4) | 26 | 15.5 (5.8) | 19 | 15.8 (6.8) | 25 | 15.7 (5.5) |
| GFSC | 33 | 17.8 (6.3) | 30 | 16.6 (5.7) | 32 | 16.1 (5.3) | 26 | 18.0 (6.7) | 29 | 18.5 (8.1) | |
| SANS Diminished Expression |
CBSST | 31 | 1.63 (1.37) | 29 | 1.72 (1.13) | 26 | 1.21 (1.12) | 19 | 1.71 (1.00) | 25 | 1.62 (1.06) |
| GFSC | 33 | 1.79 (1.09) | 30 | 1.48 (0.87) | 32 | 1.38 (1.04) | 26 | 1.62 (1.31) | 29 | 1.83 (1.30) | |
| SANS Diminished Motivation |
CBSST | 31 | 2.02 (1.17) | 29 | 2.09 (1.35) | 26 | 1.90 (1.30) | 19 | 1.53 (1.03) | 25 | 1.72 (1.02) |
| GFSC | 33 | 2.46 (1.15) | 30 | 2.15 (1.18) | 32 | 1.83 (1.31) | 26 | 1.92 (1.43) | 29 | 1.93 (1.44) | |
| BAI | CBSST | 31 | 16.4 (12.7) | 30 | 14.2 (12.3) | 26 | 15.7 (14.2) | 19 | 12.3 (12.2) | 25 | 11.5 (10.1) |
| GFSC | 33 | 14.5 (12.1) | 30 | 12.4 (12.1) | 32 | 10.6 (10.1) | 26 | 10.5 (11.4) | 29 | 10.4 (11.0) | |
| BDI-II | CBSST | 31 | 16.3 (9.8) | 30 | 17.2 (12.3) | 26 | 15.0 (12.6) | 19 | 9.1 (7.9) | 25 | 14.4 (10.2) |
| GFSC | 33 | 16.4 (13.5) | 30 | 13.8 (11.2) | 32 | 14.3 (14.0) | 26 | 12.9 (12.7) | 29 | 11.1 (11.2) | |
| LSI | CBSST | 31 | 9.7 (3.7) | 30 | 9.7 (3.9) | 26 | 10.8 (4.1) | 19 | 10.5 (4.4) | 23 | 12.1 (4.2) |
| GFSC | 33 | 9.2 (4.3) | 30 | 9.4 (4.2) | 32 | 10.2 (4.4) | 26 | 10.3 (3.8) | 28 | 10.4 (3.7) | |
| DPAS | CBSST | 31 | 53.3 (14.1) | 29 | 53.1 (14.8) | 26 | 50.8 (13.5) | 19 | 48.2 (13.5) | 25 | 53.2 (18.9) |
| GFSC | 33 | 47.3 (19.2) | 30 | 49.0 (20.2) | 32 | 47.3 (19.6) | 26 | 49.9 (20.9) | 29 | 45.3 (17.9) | |
| SERS Positive |
CBSST | 30 | 47.2 (11.6) | 30 | 45.3 (11.4) | 26 | 50.0 (11.0) | 19 | 51.1 (9.5) | 24 | 52.5 (9.8) |
| GFSC | 32 | 42.8 (14.4) | 30 | 45.8 (13.5) | 32 | 42.5 (14.6) | 26 | 46.5 (16.9) | 28 | 47.4 (15.5) | |
| SERS Negative |
CBSST | 30 | 32.3 (10.9) | 30 | 30.8 (10.4) | 26 | 31.8 (11.6) | 19 | 27.7 (10.2) | 24 | 31.4 (10.0) |
| GFSC | 32 | 31.3 (13.0) | 30 | 29.6 (14.5) | 32 | 29.4 (13.9) | 26 | 26.9 (12.7) | 28 | 29.5 (13.0) | |
Notes: CBSST=Cognitive Behavioral Social Skills Training; GFSC=Goal Focused Supportive Contact; ILSS=Independent Living Skills Survey; CMT=Comprehensive Modules Test; PANSS=Positive and Negative Syndrome Scale; BAI; Beck Anxiety Inventory; BDI-II=Beck Depression Inventory-II; LSI=Life Satisfaction Index; DPAS=Defeatist Performance Attitude Scale; SERS=Self-Esteem Rating Scale.
Table 2.
Results of mixed-effects regression modeling examining defeatist attitudes as a moderator of functioning and negative symptom outcomes
| Outcome Measure | Predictor Variables | Parameter Estimate |
t | p |
|---|---|---|---|---|
| ILSS 10-Domain Averagea | Intercept | 0.6985 | 86.24 | <.001 |
| Baseline ILSS | 0.5670 | 5.49 | <.001 | |
| Group | −0.0175 | −0.91 | .365 | |
| Baseline DPAS | −0.0004 | −0.62 | .535 | |
| Group × Baseline DPAS | 0.0001 | 0.13 | .896 | |
| Time | −0.0006 | −0.80 | .429 | |
| Baseline ILSS × Time | −0.0020 | −0.29 | .772 | |
| Group × Time | 0.0038 | 2.38 | .021 | |
| Baseline DPAS × Time | −0.0001 | −1.59 | .118 | |
| Group × DPAS × Time | 0.0001 | 1.72 | .090 | |
| SANS Diminished Expression | Intercept | 1.6110 | 12.61 | <.001 |
| Group | −0.0489 | −0.19 | .849 | |
| Baseline DPAS | 0.0141 | 1.77 | .082 | |
| Group × Baseline DPAS | −0.0135 | −0.84 | .403 | |
| Time | −0.0008 | −0.07 | .946 | |
| Group × Time | −0.0104 | −0.46 | .650 | |
| Baseline DPAS × Time | −0.0005 | −0.73 | .468 | |
| Group × DPAS × Time | 0.0007 | 0.52 | .603 | |
| SANS Diminished Motivation | Intercept | 2.2206 | 15.49 | <.001 |
| Group | −0.2978 | −1.04 | .304 | |
| Baseline DPAS | 0.0123 | 1.12 | .268 | |
| Group × Baseline DPAS | −0.0193 | −0.88 | .383 | |
| Time | −0.0259 | −2.97 | .005 | |
| Group × Time | 0.0070 | 0.40 | .688 | |
| Baseline DPAS × Time | 0.0002 | 0.36 | .719 | |
| Group × DPAS × Time | 0.0008 | 0.81 | .423 |
Notes:
Baseline ILSS measurement used as a covariate. ILSS=Independent Living Skills Survey; DPAS=Defeatist Performance Attitude Scale; SANS=Scale for Assessment of Negative Symptoms. Time in months was centered at baseline and group was coded: CBSST = 0.5 and GFSC = −0.5.
Table 3.
Results of mixed-effects regression modeling for secondary outcomes
| Outcome Measure | Variables | Parameter Estimate |
t | p |
|---|---|---|---|---|
| CMTa | Intercept | 6.14 | 13.72 | <.001 |
| Group | 1.91 | 2.13 | .037 | |
| Time | 0.17 | 5.24 | <.001 | |
| Group × Time | 0.23 | 3.44 | .001 | |
| PANSS Positive | Intercept | 17.44 | 22.49 | <.001 |
| Group | 0.93 | 0.60 | .549 | |
| Time | −0.03 | −0.81 | .423 | |
| Group × Time | −0.14 | −1.74 | .086 | |
| BAI | Intercept | 14.91 | 10.66 | <.001 |
| Group | 2.39 | 0.86 | .396 | |
| Time | −0.19 | −2.84 | .007 | |
| Group × Time | 0.03 | 0.21 | .832 | |
| BDI-II | Intercept | 16.25 | 11.95 | <.001 |
| Group | 0.80 | 0.30 | .768 | |
| Time | −0.16 | −2.64 | .011 | |
| Group × Time | 0.09 | 0.70 | .488 | |
| LSI | Intercept | 9.40 | 19.70 | <.001 |
| Group | 0.39 | 0.41 | .683 | |
| Time | 0.08 | 3.83 | <.001 | |
| Group × Time | −0.01 | −0.13 | .896 | |
| DPAS | Intercept | 50.63 | 26.01 | <.001 |
| Group | 5.35 | 1.38 | .174 | |
| Time | −0.07 | −0.63 | .531 | |
| Group × Time | −0.14 | −0.60 | .554 | |
| SERS Positive | Intercept | 44.80 | 31.51 | <.001 |
| Group | 2.87 | 1.01 | .317 | |
| Time | 0.23 | 3.54 | .001 | |
| Group × Time | 0.07 | 0.52 | .603 | |
| SERS Negative | Intercept | 31.13 | 21.44 | <.001 |
| Group | 1.27 | 0.44 | .663 | |
| Time | −0.08 | −1.20 | .236 | |
| Group × Time | 0.09 | 0.71 | .482 |
Notes:
The Group × Time interaction for CMT was also significant with baseline CMT as a covariate: Parameter estimate=0.16, t=2.12, p=.038. CMT=Comprehensive Modules Test; PANSS=Positive and Negative Syndrome Scale; BAI; Beck Anxiety Inventory; BDI-II=Beck Depression Inventory-II; LSI=Life Satisfaction Index; DPAS=Defeatist Performance Attitude Scale; SERS=Self-Esteem Rating Scale.
Time in months was centered at baseline and group was coded: CBSST = 0.5 and GFSC = −0.5.
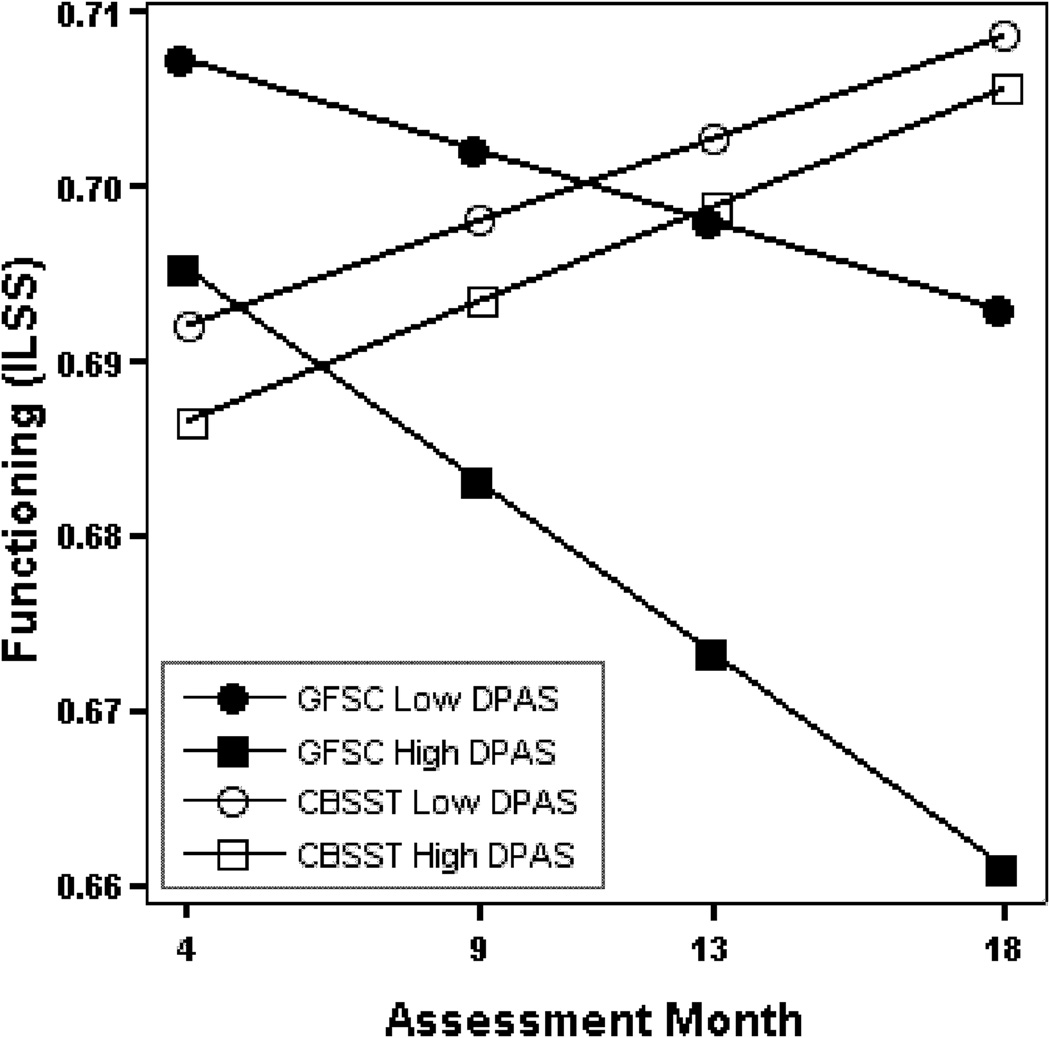
Defeatist Attitude Moderation and Mediation
With regard to moderation, Table 2 shows that the three-way interaction between treatment group, baseline defeatist attitude severity (DPAS) and time was not significant for the ILSS (p=.090) or the two SANS factors (Diminished Expression, p=.603; Diminished Motivation p=.423). Figure 1 shows the model-derived ILSS score trajectories for hypothetical participants in each treatment group with high (58) and low (42) baseline DPAS scores (higher scores indicate greater severity of defeatist performance attitudes). The figure shows a negative effect of more severe defeatist attitudes on functioning in the GFSC group, but this negative impact appeared to be mitigated by CBSST treatment. The benefit of CBSST relative to GFSC appeared to be greatest for participants with more severe defeatist attitudes, especially at 18-month follow up.
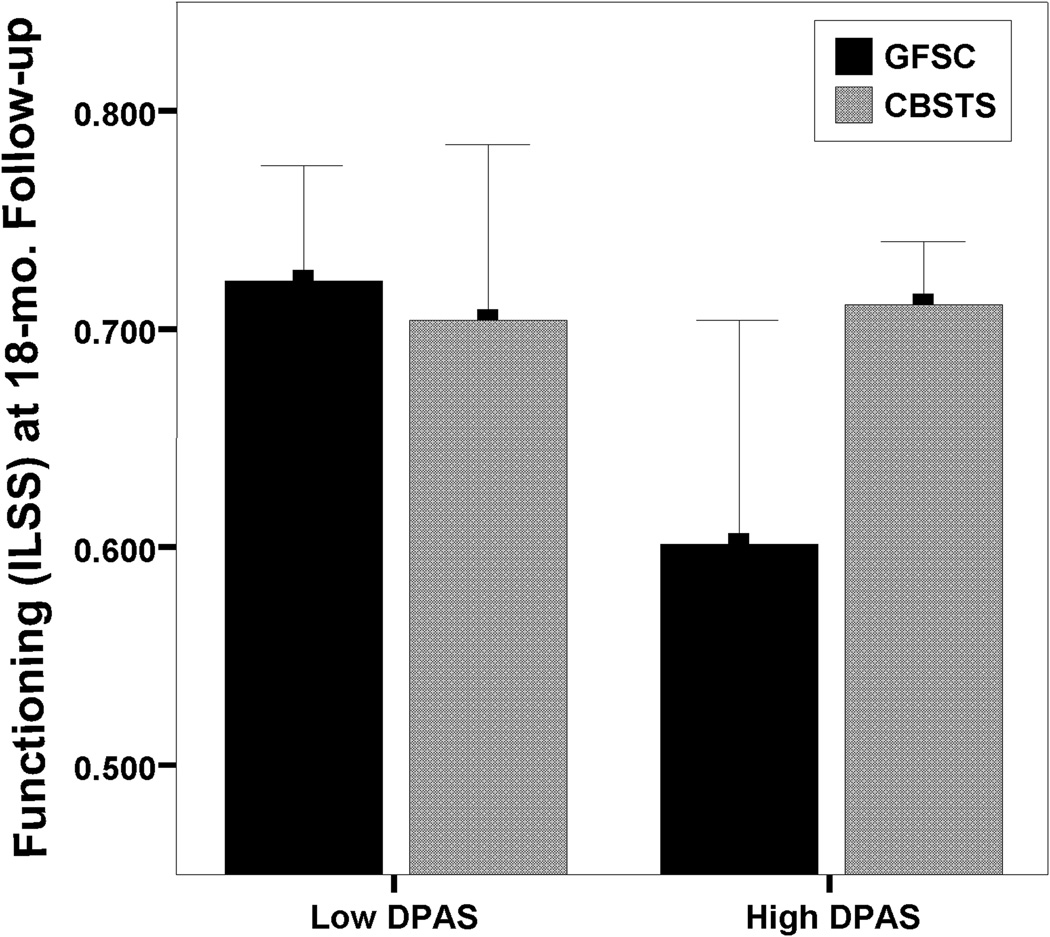
This observation was confirmed by splitting the sample at the median DPAS score into high (>50) and low (<=50) DPAS subgroups, and testing whether the treatment group effect on functioning (ILSS) was greater for high relative to low DPAS subgroups at 18-month follow up (see Figure 3). A 2 treatment groups × 2 DPAS subgroups analysis of variance showed a significant treatment group by DPAS subgroup interaction, F(1,53)=4.61, p=.037, and a large, significant treatment group effect was found for participants with high DPAS scores, t(26)=2.84, p=.009, d=1.11, but the treatment group effect was not significant for participants with low DPAS scores, t(24)=0.41, p=.683, d=0.18.
Figure 3.
Mean Independent Living Skills Survey (ILSS) scores at 18-month follow up for participants in cognitive behavioral social skills training (CBSST) and goal focused supportive contact (GFSC) divided into subgroups of high and low severity of defeatist performance attitudes (DPAS) based on splitting the sample at the median DPAS score (50). Error bars indicate 95% confidence intervals.
With regard to mediation, change in DPAS over the course of treatment was a significant predictor of ILSS at 18-month follow up for participants in CBSST, standardized β=−.38, t(20)=2.10, p=.049, but not for participants in GFSC, standardized β=.05, t(25)=0.32, p=.753. This suggests that reduction in severity of defeatist attitudes during treatment was associated with better functioning nine months post-treatment, but only for participants receiving CBSST. In the regressions for SANS factors, no significant DPAS change effects were found for either treatment group.
Discussion
The results indicated that CBSST is an effective psychosocial intervention to improve functioning in older consumers with schizophrenia. Functioning trajectories over time were significantly more positive in CBSST than in GFSC. These findings replicated the results of our prior trial (6, 14) and showed that the benefits of CBSST cannot be attributed to nonspecific therapist factors, alone. Self-reported everyday functioning improved to a greater extent in CBSST than in GFSC, suggesting specific CBT and SST interventions were more potent interventions than goal-setting and supportive contact.
The results also provided some evidence that defeatist performance beliefs are associated with change in functioning in treatment. Reduction in severity of defeatist attitudes during treatment was significantly correlated with improvement in functioning at 18-month follow up in CBSST, but not in supportive contact. This finding provides some evidence for mediation, but severity of defeatist attitudes did not change significantly in treatment (Table 3), which is required by contemporary mediation criteria (e.g., (36)). The finding of a large treatment group difference in participants with more severe defeatist attitudes (d=1.11), but only minimal treatment benefit in participants with less severe defeatist attitudes (d=0.18), also provides some support for moderation, but the three-way interaction between defeatist attitudes, treatment group and time in the mixed-model analysis was not significant. The possibility that functioning outcomes in CBT are mediated or moderated by defeatist beliefs will therefore require further study, but the findings of this study are recent research (15–18) suggesting that cognitive therapy interventions targeting defeatist beliefs may be beneficial to consumers with schizophrenia. Future studies should also examine other possible mediators, like social competence. CBT was combined with SST in CBSST, because both interventions can be used to target everyday functioning in complementary ways. CBT can modify inaccurate, defeatist beliefs, while SST can improve social competence. It is possible that improved social competence could be a mediator for a subgroup with more severe social skills deficits, but less severe defeatist beliefs.
It is notable that both treatments showed comparable significant improvements in amotivation, depression, anxiety, positive self-esteem and life satisfaction. This suggests that an active psychosocial intervention that includes at least supportive contact and systematic recovery-oriented goal setting, which requires minimal therapist training, can be beneficial to older consumers with schizophrenia for reducing symptom distress, and increasing motivation, self esteem and overall subjective life satisfaction. Other researchers have pointed out the benefits of supportive contact interventions to consumers with schizophrenia (37). In our prior study (6,14) comparing CBSST with treatment as usual (TAU), participants in TAU did not show meaningful improvement in symptom domains and showed a decline in functioning over time, so the improvements found in the present study for GFSC are greater than would be expected in standard care. However, functioning improved to a greater extent in CBSST than in GFSC, suggesting CBT and SST interventions may be more potent interventions to improve functioning, especially for individuals with more severe defeatist attitudes and social skills deficits.
Treatments personalized to the individual needs and recovery goals of consumers may be more effective. If replicated, the moderation effects found in this study may suggest that CBT interventions, like CBSST, that target functioning should be recommended for consumers with more severe defeatist attitudes. Supportive goal-setting interventions may be less costly, because they require less advanced therapists and less therapist training, so it may be more cost effective to offer consumers with less severe defeatist attitudes supportive goal setting, rather than CBT or CBSST, especially given the other benefits of GFSC identified in this study. We are currently conducting a cost analysis of CBSST treatment delivery to help inform cost effective treatment planning.
It is important to note that the sample was not geriatric, but the sample was older than samples in the vast majority of schizophrenia research, which typically has been restricted to patients below age 50. Given the shorter average life span of patients with schizophrenia, "old age" may also have different cutoffs in this group of individuals. Cohort differences (e.g., physical comorbidity, illicit substance use, hospitalization rates, etc.) lead to greater similarity between middle-aged and elderly, rather than younger, consumers with schizophrenia (38). The study also had several limitations, including the failure of the randomization to match the treatment groups on the primary outcome measure (ILSS) at baseline, but we attempted to control for this by using baseline ILSS as a covariate. Finally, participant dropout varied across assessments and was high at some time points, but the multilevel modeling analyses do not require complete data and 81% of randomized participants were included in the primary analyses.
Figure 2.
Functioning (Independent Living Skills Survey; ILSS) trajectories across assessment points from mid-treatment to 18-month follow up for hypothetical participants in cognitive behavioral social skills training (CBSST) and goal focused supportive contact (GFSC) with baseline DPAS scores set to high (58) and low (42) values (higher scores indicate greater severity of defeatist performance beliefs). Trajectories were estimated from mixed-effects regression modeling with covariates set to their median values (see Table 2).
Acknowledgements
We thank the participants who volunteered for this study. This material is based upon work supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Rehabilitation Research and Development Service, and the National Institute of Mental Health (NIMH RO1MH071410 to Dr. Granholm), and the UCSD Advanced Center for Innovations in Services and Interventions Research (ACISIR: NIMH P30MH66248 to Dr. Dilip Jeste).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Trial Registry: ClinicalTrials.Gov #NCT00237796 (http://clinicaltrials.gov/show/NCT00237796)
References
- 1.Jeste DV, Twamley EW, Eyler Zorrilla LT, et al. Aging and outcome in schizophrenia. Acta Psychiatr Scand. 2003;107:336–343. doi: 10.1034/j.1600-0447.2003.01434.x. [DOI] [PubMed] [Google Scholar]
- 2.Insel TR. Translating scientific opportunity into public health impact: a strategic plan for research on mental illness. Arch Gen Psychiatry. 2009;66:128–133. doi: 10.1001/archgenpsychiatry.2008.540. [DOI] [PubMed] [Google Scholar]
- 3.Kreyenbuhl J, Buchanan RW, Dickerson FB, et al. The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2009. Schizophr Bull. 2010;36:94–103. doi: 10.1093/schbul/sbp130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bartels SJ, Forester B, Mueser KT, et al. Enhanced skills training and health care management for older persons with severe mental illness. Community Ment Health J. 2004;40:75–90. doi: 10.1023/b:comh.0000015219.29172.64. [DOI] [PubMed] [Google Scholar]
- 5.Bartels SJ, Pratt SI. Psychosocial rehabilitation and quality of life for older adults with serious mental illness: recent findings and future research directions. Curr Opin Psychiatry. 2009;22:381–385. doi: 10.1097/YCO.0b013e32832c9234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Granholm E, McQuaid JR, McClure FS, et al. A randomized, controlled trial of cognitive behavioral social skills training for middle-aged and older outpatients with chronic schizophrenia. Am J Psychiatry. 2005;162:520–529. doi: 10.1176/appi.ajp.162.3.520. [DOI] [PubMed] [Google Scholar]
- 7.Pratt SI, Mueser KT, Driscoll M, et al. Medication nonadherence in older people with serious mental illness: prevalence and correlates. Psychiatr Rehabil J. 2006;29:299–310. doi: 10.2975/29.2006.299.310. [DOI] [PubMed] [Google Scholar]
- 8.Patterson TL, Mausbach BT, McKibbin C, et al. Functional adaptation skills training (FAST): a randomized trial of a psychosocial intervention for middle-aged and older patients with chronic psychotic disorders. Schizophr Res. 2006;86:291–299. doi: 10.1016/j.schres.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 9.Wykes T, Steel C, Everitt B, et al. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor. Schizophr Bull. 2008;34:523–537. doi: 10.1093/schbul/sbm114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benton MK, Schroeder HE. Social skills training with schizophrenics: a meta-analytic evaluation. J Consult Clin Psychol. 1990;58:741–747. doi: 10.1037//0022-006x.58.6.741. [DOI] [PubMed] [Google Scholar]
- 11.Kurtz MM, Mueser KT. A meta-analysis of controlled research on social skills training for schizophrenia. J Consult Clin Psychol. 2008;76:491–504. doi: 10.1037/0022-006X.76.3.491. [DOI] [PubMed] [Google Scholar]
- 12.Granholm E, McQuaid JR, Auslander L, McClure FS. Group cognitive-behavioral social skills training for older outpatients with chronic schizophrenia. J Cog Psychother Int Quart. 2004;18:265–279. [Google Scholar]
- 13.McQuaid JR, Granholm E, McClure FS, et al. Development of an integrated cognitive-behavioral and social skills training intervention for older patients with schizophrenia. J Psychother Pract Res. 2000;9:149–156. [PMC free article] [PubMed] [Google Scholar]
- 14.Granholm E, McQuaid JR, McClure FS, et al. Randomized controlled trial of cognitive behavioral social skills training for older people with schizophrenia: 12-month follow-up. J Clin Psychiatry. 2007;68:730–737. doi: 10.4088/jcp.v68n0510. [DOI] [PubMed] [Google Scholar]
- 15.Avery R, Startup M, Calabria K. The role of effort, cognitive expectancy appraisals and coping style in the maintenance of the negative symptoms of schizophrenia. Psychiatry Res. 2009;167:36–46. doi: 10.1016/j.psychres.2008.04.016. [DOI] [PubMed] [Google Scholar]
- 16.Grant PM, Beck AT. Defeatist beliefs as a mediator of cognitive impairment, negative symptoms, and functioning in schizophrenia. Schizophr Bull. 2009;35:798–806. doi: 10.1093/schbul/sbn008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Horan WP, Rassovsky Y, Kern RS, et al. Further support for the role of dysfunctional attitudes in models of real-world functioning in schizophrenia. J Psychiatr Res. 2010;44:499–505. doi: 10.1016/j.jpsychires.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rector NA, Beck AT, Stolar N. The negative symptoms of schizophrenia: a cognitive perspective. Can J Psychiatry. 2005;50:247–257. doi: 10.1177/070674370505000503. [DOI] [PubMed] [Google Scholar]
- 19.First MB, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version (SCID-CV) Washington, D.C.: American Psychiatric Press, Inc.; 1996. [Google Scholar]
- 20.Granholm E, McQuaid JR, McClure FS, et al. A randomized controlled pilot study of cognitive behavioral social skills training for older patients with schizophrenia. Schizophr Res. 2002;53:167–169. doi: 10.1016/s0920-9964(00)00186-9. [DOI] [PubMed] [Google Scholar]
- 21.Wallace CJ, Liberman RP, Tauber R, et al. The independent living skills survey: a comprehensive measure of the community functioning of severely and persistently mentally ill individuals. Schizophr Bull. 2000;26:631–658. doi: 10.1093/oxfordjournals.schbul.a033483. [DOI] [PubMed] [Google Scholar]
- 22.Cane DB, Olinger LJ, Gotlib IH, et al. Factor structure of the dysfunctional attitude scale in a student population. Journal of Clinical Psychology. 1986;42:307–309. [Google Scholar]
- 23.Weissman AN, Beck AT. Development and validation of the Dysfunctional Attitude Scale: A preliminary investigation. Paper presented at the Annual Meeting of the American Educational Research Association; Toronto, CA. 1978. [Google Scholar]
- 24.Weissman AN. Assessing depressogenic attitudes: A validation study. Paper presented at the 51st annual meeting of the Eastern Psychological Association; Hartford, CT. 1980. [Google Scholar]
- 25.Liberman RP. Psychosocial treatments for schizophrenia. Psychiatry. 1994;57:104–114. doi: 10.1080/00332747.1994.11024674. [DOI] [PubMed] [Google Scholar]
- 26.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 27.Andreasen NC. Negative symptoms in schizophrenia. Definition and reliability. Arch Gen Psychiatry. 1982;39:784–788. doi: 10.1001/archpsyc.1982.04290070020005. [DOI] [PubMed] [Google Scholar]
- 28.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- 29.Beck AT, Steer RA. Beck Anxiety Inventory manual. San Antonio, TX: The Psychological Corporation; 1990. [Google Scholar]
- 30.Blanchard JJ, Cohen AS. The structure of negative symptoms within schizophrenia: implications for assessment. Schizophr Bull. 2006;32:238–245. doi: 10.1093/schbul/sbj013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peralta V, Cuesta MJ. Dimensional structure of psychotic symptoms: an item-level analysis of SAPS and SANS symptoms in psychotic disorders. Schizophr Res. 1999;38:13–26. doi: 10.1016/s0920-9964(99)00003-1. [DOI] [PubMed] [Google Scholar]
- 32.Sayers SL, Curran PJ, Mueser KT. Factor Structure and Construct Validity of the Scale for the Assessment of Negative Symptoms. Psychological Assessment. 1996;8:269–280. [Google Scholar]
- 33.Lecomte T, Corbiere M, Laisne F. Investigating self-esteem in individuals with schizophrenia: relevance of the Self-Esteem Rating Scale-Short Form. Psychiatry Res. 2006;143:99–108. doi: 10.1016/j.psychres.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 34.Wallace KA, Wheeler AJ. Reliability Generalization of the Life Satisfaction Index. Educational and Psychological Measurement. 2002;62:674–684. [Google Scholar]
- 35.Haddock G, Devane S, Bradshaw T, et al. An investigation into the psychometric properties of the Cognitive Therapy Scale for Psychosis (CTS-Psy) Behavl & Cognitive Psychother. 2001:221–233. [Google Scholar]
- 36.Kraemer HC, Wilson GT, Fairburn CG, et al. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 37.Penn DL, Mueser KT, Tarrier N, et al. Supportive therapy for schizophrenia: possible mechanisms and implications for adjunctive psychosocial treatments. Schizophr Bull. 2004;30:101–112. doi: 10.1093/oxfordjournals.schbul.a007055. [DOI] [PubMed] [Google Scholar]
- 38.Jeste DV, Alexopoulos GS, Bartels SJ, et al. Consensus statement on the upcoming crisis in geriatric mental health: research agenda for the next 2 decades. Arch Gen Psychiatry. 1999;56:848–853. doi: 10.1001/archpsyc.56.9.848. [DOI] [PubMed] [Google Scholar]