Abstract
Background
We sought to compare the epidemiologic features of Kawasaki disease (KD) in three Northern European countries and Japan.
Methods
Data were obtained from discharge databases for hospitals in Finland, Norway, and Sweden from 1999–2009 and from nationwide epidemiologic surveys in Japan from 1998–2008. Annual incidence for each country was calculated using regional census data.
Results
During the 11-year period, 1,390 KD patients were recorded in the registries of the three Northern European countries. Average annual incidence rates per 100,000 children less than 5 years were: Finland 11.4, Norway 5.4, and Sweden 7.4. Overall, 86.4% of Japanese KD patients were less than 5 years compared to only 67.8% in the four Northern European countries (p<0.001).
Conclusions
The incidence of KD in Northern Europe was constant over the study period and much lower than in Japan. There was a significant age difference between Northern European and Japanese KD patients that remains unexplained.
Keywords: coronary artery aneurysm, epidemiology, Kawasaki disease, vasculitis
INTRODUCTION
Despite thirty years of research, Kawasaki disease (KD) remains a mysterious illness of infants and children. Although an infectious trigger is suspected, the etiology remains unknown and diagnosis is based on fulfillment of clinical criteria in the setting of prolonged fever without other explanation. In the United States and Western Europe, there is no centralized reporting system that captures all diagnosed KD patients. In contrast, Northern European countries have effective centralized reporting systems for all hospitalized patients. This allows for a more reliable description of KD incidence and patient demographics.
Increasing numbers of KD patients are being reported from many regions of the world. In Japan, the country with the highest reported incidence, a steady increase in diagnosed cases is thought to represent a true increase in disease incidence because of long-standing, widespread physician awareness of the disease.[1] In contrast, it is debated whether the rising incidence reported from many Western countries is due to a true increase in number of cases or simply increased physician awareness.[2] Current incidence rates of KD have been recently updated for Denmark, but not for the other Northern European countries included in this report.[3] We sought to determine whether the incidence had changed in Finland, Norway, and Sweden, all countries that have stable national health systems and good epidemiologic surveillance of KD.
PATIENTS AND METHODS
The number of KD cases (ICD 9 code 446B or 446.98 or ICD 10 code M30.3) and demographic data were obtained from hospital discharge databases from 1999–2009 by investigators in Finland, Norway, and Sweden. Denominator data were obtained from each country’s national bureau of statistics. Data for Japan were obtained from the nationwide surveys with the last survey conducted in 2008. Incidence rates were compared using the chi square statistic.
RESULTS
During the 11-year period of this study, a total of 1,390 KD patients were recorded in the registries from the Northern European countries. Average incidence rates per 100,000 children less than 5 years during the period 1998–2009 were as follows: Finland 11.4, Norway 5.4, and Sweden 7.4 (Figure 1). During the period 1998–2008, the incidence rates for Japan rose from 111.7 to 218.6 per 100,000 children less than 5 years of age.[1]
Figure 1.
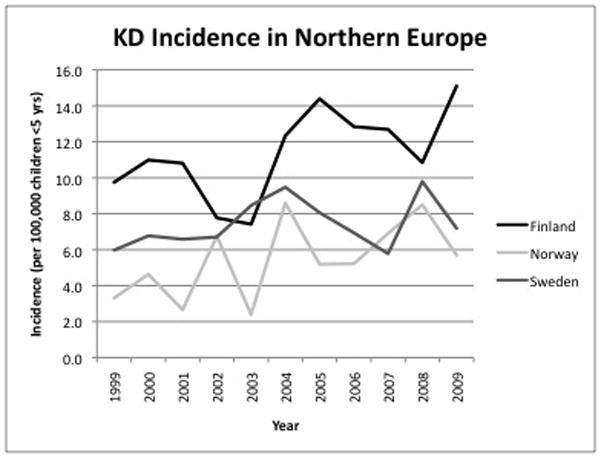
Annual incidence of Kawasaki disease in Northern European countries from 1999–2009 expressed as number of cases per 100,000 children less than 5 years of age.
Male patients comprised 68.8%, 61.2%, and 62.8% of the total KD population in Finland, Norway, and Sweden respectively. The distribution of the KD patients across age groups was similar for the three Northern European countries (Figure 2A). The percentage of patients less than 5 years was as follows: Finland 69.2%, Sweden 67.1%, and Norway 66.8%, with an overall percentage for the three countries of 67.8%. In contrast, of the 91,372 Japanese KD patients during this same period, 86.4% were less than 5 years (67.8% vs. 86.4%, P<0.001) (Figure 2B).
Figure 2.
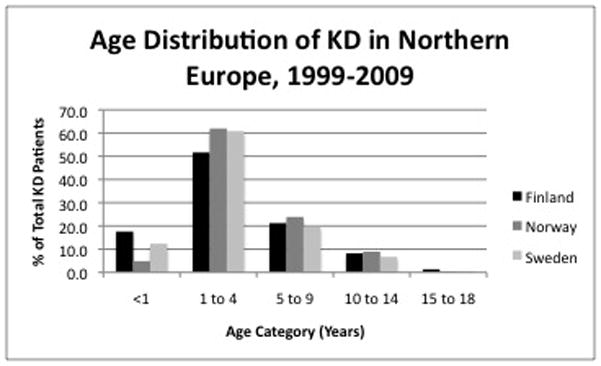
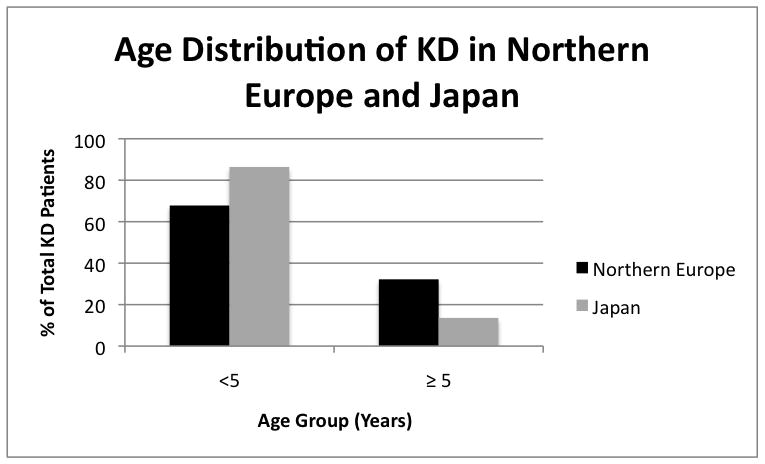
Age distribution of Kawasaki disease patients in Northern European countries (A) and compared to Japan (B).
DISCUSSION
The average annual incidence rates for KD in Northern European countries ranged from 5.4 to 11.4 patients per 100,000 children less than 5 years. Over the time period studied, incidence rates remained relatively constant and were similar to previous reports from these countries and to incidence rates reported for Denmark.[3] The Danish study reported increasing incidence in the 1980s and 1990s, followed by stabilization of rates from 2000–2004. No significant changes in incidence rates in the three Northern European countries were observed in the present study from 1999–2009. In contrast, incidence rates continued to rise over this time period in Japan where the latest incidence for KD is now approximately 218 per 100,000 children less than 5 years.[1].
Hypotheses to explain the very different incidence rates between Northern Europe and Japan include different exposure rates to the causative agent and differences in genetic susceptibility. One genetic difference between Northern European and Japanese populations has been clearly elucidated. The C-C chemokine receptor 5 (CCR5) Δ32 polymorphism prevents expression of CCR5 on the surface of cells and is protective against KD.[4] Japan, which has the highest incidence of KD, has the lowest prevalence of the CCR5Δ32 polymorphism. Conversely, Northern European countries, which have the lowest incidence of KD, have the highest prevalence of the CCR5Δ32 polymorphism.[4] While the prevalence of CCR5Δ32 may partially explain the lower incidence of KD in Northern European countries, it does not explain the older age at onset of these patients.
A significant difference in the age distribution of patients in Northern Europe was noted when compared to Japan. The difference in age distribution between Japan and the Northern European countries was consistent over time and unexplained. Understanding the difference in age distribution and incidence between these populations may shed light on the mechanisms that underlie this puzzling disease.
Acknowledgments
FUNDING
This work was supported in part by a grant from the National Institutes of Health, National Heart, Lung, and Blood Institute (K24 HL074864) to Jane C. Burns, M.D.
Footnotes
This work presented in part at the International Kawasaki Disease Symposia in Taipei, Taiwan in 2008 and in Kyoto, Japan in 2012.
COMPETING INTERESTS
None to declare.
References
- 1.Nakamura Y, Yashiro M, Uehara R, et al. Epidemiologic features of Kawasaki disease in Japan: results of the 2007–2008 nationwide survey. J Epidemiol. 2010;20(4):302–307. doi: 10.2188/jea.JE20090180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harnden A, Alves B, Sheikh A. Rising incidence of Kawasaki disease in England: analysis of hospital admission data. Bmj. 2002 Jun 15;324(7351):1424–1425. doi: 10.1136/bmj.324.7351.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fischer TK, Holman RC, Yorita KL, Belay ED, Melbye M, Koch A. Kawasaki syndrome in Denmark. Pediatr Infect Dis J. 2007 May;26(5):411–415. doi: 10.1097/01.inf.0000259964.47941.00. [DOI] [PubMed] [Google Scholar]
- 4.Burns JC, Shimizu C, Gonzalez E, et al. Genetic Variations in the Receptor-Ligand Pair CCR5 and CCL3L1 Are Important Determinants of Susceptibility to Kawasaki Disease. J Infect Dis. 2005 Jul 15;192(2):344–349. doi: 10.1086/430953. [DOI] [PMC free article] [PubMed] [Google Scholar]


