Abstract
Aim
This study aims to examine the prevalence of alcohol and/or other drugs (AOD) in a large sample of fatally injured drivers.
Design
Using data from the Fatality Analysis Reporting System for 2005–2009, the authors examined the prevalence of AOD detected in fatally injured drivers in the United States.
Setting
Fatal motor vehicle crashes occurring on public roads.
Participants
Drivers who died within one hour of the crash in 14 states that performed toxicological testing on more than 80% of these drivers.
Measurements
Prevalence of AOD and multivariable-adjusted prevalence ratios (aPR).
Findings
Of the 20,150 fatally injured drivers studied, 57.3% tested positive for AOD, including 19.9% being positive for two or more substances. Alcohol was the most commonly detected substance, present in 40.2% of the fatally injured drivers, followed by cannabinols (10.5%), stimulants (9.0%), narcotics (5.7%), and depressants (4.0%). Multivariable analysis revealed that AOD was significantly more prevalent among drivers who died in single-vehicle crashes [aPR 1.69, 95% confidence interval (CI): 1.62–1.76], or nighttime crashes (aPR 1.43, 95% CI: 1.39–1.47), or who had a driving-while-intoxicated conviction within the past three years (aPR 1.41, 95% CI: 1.35–1.47), and less prevalent among drivers who were 65 years or older (aPR 0.45, 95% CI: 0.42–0.49), Asian (aPR 0.47, 95% CI 0.41–0.53), or female (aPR 0.88, 95% CI: 0.85–0.91), or who were operating a motor carrier (aPR 0.41, 95% CI 0.34–0.48).
Conclusions
More than half of fatally injured drivers in the United States had been using AOD and approximately 20% had been using polydrugs. The prevalence of AOD use varies significantly with driver and crash characteristics.
Keywords: Accidents -Traffic, Alcohol Consumption, Drug Users, Cannabinoids, Motor Vehicles, Prescription Drugs, Safety
INTRODUCTION
Public concern about drugged driving has heightened in recent years, fueled in part by high profile crashes [1, 2], rising consumption of prescription drugs, and increased morbidity and mortality related to prescription drug abuse [3-11]. In the United States, from 1991 to 2007, opiate prescriptions rose from approximately 40 million to around 180 million [6]. National estimates of emergency department visits involving illicit drugs, alcohol, and pharmaceuticals show an almost two-fold increase between 2004 and 2009 [12]. The 2009 National Survey on Drug Use and Health estimates that 10.5 million persons 12 or more years of age drove under the influence of illicit drugs in the prior year [12]. The Office of National Drug Control Policy, along with the Department of Transportation and the National Institute on Drug Abuse, has identified driving under the influence of drugs as a priority area for drug control research and interventions [13-16].
Polydrug use by drivers, i.e., the use of two or more drugs concurrently, is of particular concern as the interaction effects of different drug combinations may be significantly greater than the effects of using individual drugs alone [17-21]. Compared with the use of alcohol or cannabis alone, the combined effect of these substances poses excess risk of impairments in driving performance and crash involvement [18, 22]. Studies have revealed that the effect of cannabis on impairment in driving performance is greater in combination with amphetamines, benzodiazepines, and opiates than for these other drugs alone [19, 22, 23]. Similar findings have been reported for benzodiazepines used in combination with opiates [22].
Epidemiologic data on polydrug use in drivers are sparse. Results from roadside surveys indicate that about 2% of drivers in the United States and 1% of drivers in Europe are positive for two or more drugs [24, 25]. Toxicological testing data for drivers injured in motor vehicle crashes suggest that up to 25% tested positive for multiple drugs, with alcohol, cannabis, and opiates being the most frequently detected substances [26, 27]. Studies of drivers arrested for suspected impaired driving in Scotland and Finland suggest an increasing trend in polydrug use [28, 29]. A recent cross-sectional survey of fatally injured drivers in four European countries found that the prevalence of polydrug use varied from 6.4% in Portugal to 15.2% in Norway [30]. Previous studies documenting the prevalence of polydrug use in injured drivers in the United States were limited to small sample sizes from single institutions. In the present study, we aim to examine the prevalence of alcohol and/or other drugs (AOD) and specific drug combinations in a large sample of fatally injured drivers by capitalizing on recently available comprehensive toxicological testing data in 14 states.
METHODS
Data source
Data for this study came from the Fatality Analysis Reporting System (FARS). Compiled by the National Highway Traffic Safety Administration, FARS is a census of fatal traffic crashes occurring within the United States and includes all crashes involving a motor vehicle traveling on a public road and resulting in a fatality within 30 days of the crash [31]. This data system contains detailed data on the circumstances, vehicles, and people involved in the crash. Data are abstracted from police reports, state administrative files, and medical records by trained analysts using standard forms and protocols. Data are monitored using specified quality control procedures [32]. Data elements include driver characteristics, such as, sex, race, ethnicity, drug and alcohol test results. Crash circumstances including vehicle type, day, time, and year of crash are also recorded. Although FARS started recording testing results for non-alcohol drugs since 1991, drug testing was performed on only about 30% of fatally injured drivers nationwide. Drug testing on fatally injured drivers, however, has become routine in an increasing number of states in recent years [10].
Study sample
The study sample consisted of 22,649 drivers who died within one hour of the crash between January 1, 2005 and December 31, 2009 in states that performed toxicological testing on more than 80% of their fatally injured drivers (California, Connecticut, Illinois, Kentucky, Maryland, Montana, New Hampshire, New Jersey, North Dakota, Ohio, Pennsylvania, Vermont, Washington, and West Virginia). Despite higher than 80% testing rates, data from North Carolina and New Mexico were excluded from the study sample because test results recorded in FARS for these two states were deemed unreliable [32, 33]. Of the 22,649 drivers in the study sample, 2,499 (11.0%) were excluded from the analysis due to the lack of drug testing data. Drivers who survived more than one hour after the crash (n=9,160) or with missing time of death information (n=225) were excluded from this study because of concerns about the accuracy and reliability of drug testing data for these drivers.
Statistical analysis
To assess selection bias resulting from incomplete drug testing, drivers with and without toxicological results were examined by driver characteristics (age, sex, race, ethnicity, driver type, driving while intoxicated (DWI) conviction in the past 3 years, crash within the past 3 years, and blood alcohol concentration (BAC)), and crash circumstances (number of vehicles involved, day of crash, time of day, and year), as well as time until death and the location of death. Race was grouped as White, Black, Asian (Chinese, Japanese, Hawaiian, Filipino, Asian Indian, Other Indian, Korean, Samoan, Vietnamese, Guamanian, Other Asian, and Pacific Islander), Native American, Other (multiple races and all other races), and Unknown. Ethnicity was categorized as Hispanic, Non-Hispanic and Unknown. Driver types were categorized as motor carrier, defined as a driver of a motor vehicle with a gross vehicle weight of 26,000 pounds or greater, versus any other type of road vehicle [34]. BAC was measured in grams per deciliter. The number of vehicles involved in the crash was categorized into whether one or two or more vehicles were involved. Day of crash was categorized into whether the crash occurred on a weekday (Monday to Thursday) or a weekend (Friday to Sunday). Time of crash was grouped as day (crashes occurring between 7:00 am and 6:59 pm) and night (crashes occurring between 7:00 pm and 6:59 am) [30]. Chi-square tests with an alpha level of 0.05 were used to determine whether drivers with and without drug test results differed by driver characteristics and crash circumstances.
The prevalence of drug involvement in fatally injured drivers was tabulated by drug class. Using robust-variance Poisson regression, multivariable-adjusted prevalence ratios (aPR) and 95% confidence intervals (CI) were estimated separately for single-drug use, polydrug use, and any drug use [35]. Variables that were statistically significant in bivariable analyses, along with driver demographic characteristics, were included in each multivariable model. Data analyses were performed using Statistical Analysis Software, version 9.2 (SAS Institute, Inc., Cary North Carolina) and Stata/SE, version 11.2 (StataCorp LP, College Station, Texas).
Drug testing assessments
Drug tests were performed using chromatography and radioimmunoassay techniques based on blood and/or urine specimens [27, 36]. Up to four drugs, including alcohol, were recorded for each driver. When multiple drugs were reported, non-alcohol drugs were logged in the FARS data in the following priority order: narcotics, depressants, stimulants, marijuana and other licit drugs [27]. Drugs were categorized according to the FARS coding manual [37] and grouped into the following categories: alcohol, cannabinol, stimulant, narcotic, depressant (exclusive of alcohol), hallucinogen, phencyclidine (PCP), anabolic steroid, inhalant, and “other” drugs. Due to small numbers, the hallucinogen, PCP, anabolic steroid, and inhalant categories were combined. “Other” drugs include drugs not classified as the above categories in the FARS coding manual [37]. These are generally other legal drugs (such as beta-blockers, anti-epileptics, antihistamines or antidepressants) that may or may not impair driving ability [27]. Drugs administered after the crash were not included [10]. Polydrug use was operationally defined as testing positive for two or more substances, with alcohol being treated as a drug. If a driver tested positive for a drug and its metabolite, the driver was only categorized as being positive for the parent drug. For example, if a driver tested positive for methamphetamine and amphetamines, the driver was categorized as testing positive for methamphetamine only.
Drug testing protocols might vary from state to state [38, 39]. Some states tested for fewer drugs than others [40]. The testing methods and specimens might not be exactly the same across the states. The possible bias resulting from different specimens, however, was unlikely to pose a serious threat to the validity of this study given that 94% of the study sample had at least one test based on a blood specimen.
RESULTS
Representativeness of the study sample
Overall, 89% of drivers in the study sample were tested for AOD. Drivers for whom laboratory drug testing results were available and drivers who were excluded from the analysis due to the lack of drug testing data were similar with regard to sex, driver type, the number of vehicles involved in the crash, crash in the past 3 years, day of crash, time until driver death, and location of driver death (Table 1). Notable exceptions to the comparability between the two groups were that drivers who were tested were more likely to be 25–34 years of age and white, have a known ethnicity, be alcohol-positive (i.e., BAC ≥ 0.01 g/dL), and be involved in night-time crashes. Drivers who were fatally injured in 2005 were more likely to have incomplete drug testing data than in subsequent years (Table 1). Of the 20,150 drivers included in the analysis, 94% had at least one drug test result based on a blood specimen.
Table 1.
Characteristics of Fatally Injured Drivers who Died within One Hour of the Crash by Toxicological Testing Status, Selected States, United States, 2005–2009
| Toxicological testing complete (n=20,150) |
Toxicological testing incomplete (n=2,499) |
|||
|---|---|---|---|---|
|
|
||||
| Characteristic | No. of Drivers |
% | No. of Drivers |
% |
| Age (in years)a,b | ||||
| <16 | 60 | 0.3 | 26 | 1.0 |
| 16-20 | 2327 | 11.6 | 257 | 10.3 |
| 21-24 | 2590 | 12.9 | 279 | 11.2 |
| 25-34 | 4217 | 20.9 | 446 | 17.9 |
| 35-44 | 3554 | 17.6 | 395 | 15.8 |
| 45-54 | 3273 | 16.2 | 389 | 15.6 |
| 55-64 | 2138 | 10.6 | 318 | 12.7 |
| ≥ 65 | 1985 | 9.9 | 388 | 15.5 |
| Sexa,b | ||||
| Female | 4418 | 21.9 | 615 | 24.6 |
| Male | 15731 | 78.1 | 1884 | 75.4 |
| Racea,c | ||||
| White | 14819 | 73.5 | 1748 | 69.9 |
| Black | 1410 | 7.0 | 114 | 4.6 |
| Asian | 497 | 2.5 | 435 | 1.8 |
| Native American | 209 | 1.0 | 95 | 1.5 |
| Other | 128 | 0.6 | 17 | 0.7 |
| Unknown | 3087 | 15.3 | 538 | 21.5 |
| Ethnicitya,c | ||||
| Hispanic | 2313 | 11.5 | 203 | 8.1 |
| Non-Hispanic | 14432 | 71.6 | 1723 | 68.9 |
| Unknown | 3405 | 16.9 | 573 | 22.9 |
| Driver Type | ||||
| Motor carrier | 398 | 2.0 | 53 | 2.1 |
| Non-motor carrier | 19752 | 98.0 | 2446 | 97.9 |
| Number of Vehicles Involved | ||||
| 1 | 15122 | 75.0 | 1884 | 75.4 |
| ≥ 2 | 5028 | 25.0 | 615 | 24.6 |
| DWI conviction within the Prior 3 years b | ||||
| No | 18885 | 95.6 | 2333 | 95.6 |
| Yes | 876 | 4.4 | 107 | 4.4 |
| Crash within the Prior 3 yearsa,b | ||||
| No | 15450 | 83.6 | 1951 | 85.5 |
| Yes | 3041 | 16.4 | 332 | 14.5 |
| Blood Alcohol Concentration (in g/dL)a,b,c | ||||
| 0.00 | 11977 | 59.7 | 571 | 51.1 |
| 0.01-0.07 | 1079 | 5.4 | 61 | 5.5 |
| ≥ 0.08 | 7015 | 35.0 | 485 | 43.4 |
| Day of Crash | ||||
| Friday-Sunday | 10126 | 50.3 | 1252 | 50.1 |
| Monday-Thursday | 10024 | 49.7 | 1247 | 49.9 |
| Time of Crasha,b | ||||
| Day (7:00 am and 6:59 pm) | 9755 | 49.2 | 1346 | 54.6 |
| Night (7:00 pm and 6:59 am) | 10091 | 50.8 | 1117 | 45.4 |
| Year of Crasha,c | ||||
| 2005 | 4133 | 20.5 | 735 | 29.4 |
| 2006 | 4368 | 21.7 | 553 | 22.1 |
| 2007 | 4337 | 21.5 | 416 | 16.6 |
| 2008 | 3960 | 19.7 | 366 | 14.6 |
| 2009 | 3352 | 16.6 | 429 | 17.2 |
| Time until Driver Death c | ||||
| Instantly | 9968 | 49.5 | 1200 | 48.0 |
| 1-59 minutes | 10182 | 50.5 | 1299 | 52.0 |
| Death Location b | ||||
| At scene | 16180 | 80.3 | 2007 | 80.3 |
| En route | 163 | 0.8 | 20 | 0.8 |
| Other | 3801 | 18.9 | 472 | 18.9 |
Group with complete drug assessments differs significantly from group with incomplete assessment, two-sided P<0.05.
Totals vary due to missing data.
Due to rounding some percentage totals may not add to 100.
Note: The overall testing rate for this group of drivers is 89%.
Prevalence of drug use
Of the 20,150 drivers who were tested for drugs, 11,550 (57.3%, 95% CI: 56.6– 58.0%) were positive for at least one drug, including 7,549 (37.5%) positive for one drug and 4,001 (19.9%, 95% CI: 19.3–20.4%) positive for two or more drugs (Table 2). Alcohol was the most commonly detected drug, present alone or in combination with one or more other drugs in 40.2% (95% CI 39.5–40.8) of the tested drivers. Non-alcohol drugs were detected in 31.8% of drivers (95% CI: 31.1–32.4). Cannabinols (10.5%, 95% CI: 10.0–10.9) were the most frequently detected non-alcohol drug, followed by stimulants (9.0%, 95% CI: 8.6–9.4), narcotics (5.7%, 95% CI: 5.4–6.0), and depressants (4.0%, 95% CI: 3.7–4.2) (Table 2). The specific drug combinations commonly detected were alcohol with cannabinols, cocaine, or methamphetamine, accounting for 32.4% of all polydrug use. For drivers testing positive for three drugs, the most frequently detected drug classes were alcohol, cannabinols and stimulants, with cocaine being the most commonly detected stimulant (Table 2).
Table 2.
Prevalence and 95% Confidence Intervals (CI) of Alcohol and Other Drugs in Fatally Injured Drivers who Died within One Hour of the Crash by Drug Category and Sex, Selected States, United States, 2005–2009
| Drug category | Overall, % (n=20,150) (95% CI) |
Males, % (n=15,731) (95% CI) |
Females, % (n=4,418) (95% CI) |
|---|---|---|---|
| Single Drug | 37.5 (36.8–38.1) | 39.7 (38.9–40.4) | 29.6 (28.2–31.0) |
| Alcohol | 25.6 (25.0–26.2) | 28.3 (27.6–29. 0) | 16.0 (14.9–17.1) |
| Non-alcohol druga | 11.9 (11.5–12.4) | 11.4 (10.9–11.9) | 13.7 (12.7–14.7) |
| Cannabinol | 3.0 (2.8–3.3) | 3.3 (3.0–3.6) | 2.1 (1.7–2.5) |
| Stimulant | 2.3 (2.1–2.6) | 2.3 (2.1–2.6) | 2.4 (2.0–2.9) |
| Narcotic | 1.0 (0.8–1.1) | 0.8 (0.7–1.0) | 1.5 (1.2–1.9) |
| Depressant | 0.7 (0.6–0.8) | 0.5 (0.4–0.7) | 1.1 (0.8–1.5) |
| Hallucinogen– phencyclidine–anabolic steroid–inhalant |
0.1 (0.0–0.2) | 0.2 (0.1–0.2) | 0.1 (0.0–0.2) |
| Other | 4.7 (4.4–5.0) | 4.3 (3.9–4.6) | 6.5 (5.7–7.2) |
| Two drugs a | 14.4 (13.9–14.8) | 14.9 (14.4–15.5) | 12.3 (11.4–13.3) |
| Alcohol and cannabinol | 4.0 (3.8–4.3) | 4.5 (4.2–4.8) | 2.4 (1.9–2.9) |
| Alcohol and stimulant | 2.6 (2.4–2.8) | 2.7 (2.5–3.0) | 2.1 (1.7–2.5) |
| Alcohol and other drug | 2.8 (2.6–3.0) | 2.6 (2.4–2.9) | 2.0 (1.6–2.4) |
| All other two-drug combinations |
5.2 (4.9–5.5) |
5.1 (4.7–5.4) | 5.9 (5.2-6.6) |
| Three drugs a | 4.9 (4.6–5.2) | 4.8 (4.5–5.2) | 5.1 (4.5–5.8) |
| Alcohol, cannabinol, and stimulant |
0.8 (0.7–0.9) | 0.9 (0.8–1.1) | 0.3 (0.2–0.5) |
| Alcohol, stimulant, and other drug |
0.6 (0.5–0.7) | 0.6 (5.3–7.9) | 0.4 (0.2–0.6) |
| Alcohol, cannabinol, and other drug |
0.4 (0.3–0.5) | 0.4 (0.3–0.6) | 0.4 (0.2–0.6) |
| All other three-drug combinations |
3.1 (2.9-3.3) | 2.8 (2.6–3.1) | 4.1 (3.5–4.7) |
| Four drugs | 0.6 (0.5–0.7) | 0.7 (0.5–0.8) | 0.4 (0.2–0.6) |
| One or more drugs a | 57.3 (56.6–58.0) | 60.1 (59.3–60.8) | 47.5 (46.0–49.0) |
| Two or more drugs | 19.9 (19.3–20.4) | 20.4 (19.8–21.1) | 17.8 (16.7–19.0) |
Subcategory percentages may not add to category percentages due to rounding.
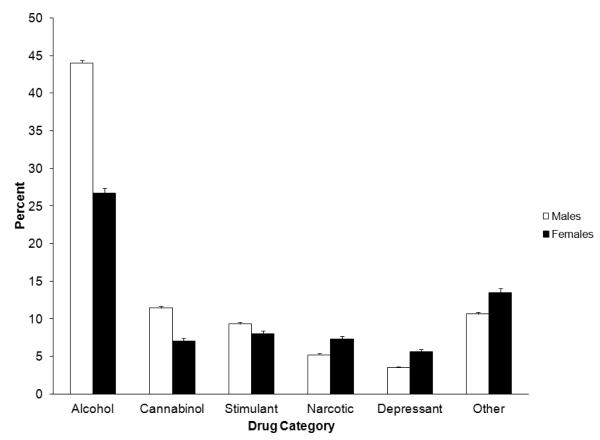
Male drivers had significantly higher prevalence rates of single-drug use and two-drug use than female drivers (Table 2). Overall, 60.1% of male drivers and 47.5% of female drivers tested positive for at least one drug (Table 2). The overall prevalence of non-alcohol drugs was similar between male (31.8%, 95% CI: 31.1–32.6%) and female drivers (31.5%, 95% CI: 30.2–32.9%). The prevalence of specific drugs, however, differed significantly between sexes, with men being more likely to use alcohol, cannabinols, and stimulants and women being more likely to use narcotics, depressants, and other drugs (Figure 1).
Figure 1.
Prevalence and Standard Error of Alcohol and Other Drugs in Fatally Injured Drivers who Died within One Hour of the Crash by Drug Category and Sex, Selected States, United States, 2005–2009
Native American drivers had the highest prevalence of drug use (83.7%, including 37.8% of single-drug use and 45.9% of polydrug use). Non-Hispanic drivers, non-motor carrier drivers, drivers involved in crashes in the prior 3 years, drivers involved in single-vehicle crashes, and drivers with a DWI within the prior 3 years were more likely to test positive for a single-drug and for polydrugs (Table 3).
Table 3.
Prevalence and 95% Confidence Intervals (CI) of Single-Drug Use and Polydrug Use by Driver and Crash Characteristics for Fatally Injured Drivers who Died within One Hour of the Crash, Selected States, United States, 2005–2009
| Characteristic | No. of Driversa |
Positive for One Drugb |
Positive for Two or More Drugsb |
Positive in Total |
|---|---|---|---|---|
|
| ||||
| % (95% CI) | % (95% CI) | % (95% CI) | ||
| Age (in years) | ||||
| <25 | 4977 | 37.5 (36.2–38.9) | 20.1 (19.0–21.2) | 57.6 (56.3–59.0) |
| 25-34 | 4217 | 44.0 (42.5–45.5) | 24.1 (22.9–25.5) | 68.2 (66.7–69.6) |
| 35-44 | 3554 | 41.6 (36.2–38.9) | 22.7 (21.3–24.2) | 64.3 (62.7–65.9) |
| 45-54 | 3273 | 37.2 (35.5–38.9) | 22.3 (20.9–23.8) | 59.5 (57.8–61.2) |
| 55-64 | 2138 | 31.0 (29.1–33.0) | 14.7 (13.3–16.3) | 45.7 (43.6–47.9) |
| ≥ 65 | 1985 | 23.2 (21.3–25.1) | 6.5 (5.5–7.7) | 29.7 (27.7–31.8) |
| Sex | ||||
| Female | 4418 | 29.6 (28.3–31.0) | 17.9 (16.7–19.0) | 47.5 (46.0–49.0) |
| Male | 15,731 | 39.7 (38.9–40.4) | 20.4 (19.8–21.1) | 60.1 (59.3–60.8) |
| Race | ||||
| White | 14,819 | 37.4 (36.6–38.1) | 20.9 (20.2–21.5) | 58.2 (57.4–59.0) |
| Black | 1410 | 39.5 (36.9–42.1) | 18.0 (16.0–20.1) | 57.5 (54.9–60.1) |
| Asian | 497 | 25.3 (21.6–29.4) | 7.2 (5.1–9.9) | 32.6 (28.5–36.9) |
| Native American | 209 | 37.8 (31.2–44.7) | 45.9 (39.0–52.9) | 83.7 (78.0–88.5) |
| Other | 128 | 39.8 (31.3–48.9) | 13.3 (7.9–20.4) | 53.1 (44.1–62.0) |
| Unknown | 3087 | 38.9 (37.2–40.7) | 16.4 (15.1–17.8) | 55.3 (53.6–57.1) |
| Ethnicity | ||||
| Hispanic | 2313 | 40.5 (38.4–42.5) | 17.3 (15.7–18.9) | 57.7 (55.7–59.7) |
| Non-Hispanic | 14,432 | 36.6 (35.8–37.4) | 21.1 (20.4–21.8) | 57.7 (56.8–58.5) |
| Unknown | 3405 | 39.2 (37.6–41.0) | 16.4 (15.1–17.6) | 55.6 (53.9–57.3) |
| Driver Type | ||||
| Motor carrier | 398 | 20.4 (16.5–24.6) | 6.5 (4.3–9.4) | 26.9 (22.6–31.5) |
| Non-motor carrier |
19,752 | 37.8 (37.1–38.5) | 20.1 (19.6–20.7) | 57.9 (57.2–58.6) |
| Number of Vehicles Involved | ||||
| 1 | 15,122 | 41.1 (40.3–41.9) | 22.8 (22.1–23.5) | 63.9 (63.1–64.7) |
| ≥ 2 | 5028 | 26.5 (25.3–27.7) | 11.1 (10.2–12.0) | 37.5 (36.2–38.9) |
| DWI conviction within the Prior 3 years | ||||
| No | 18,885 | 36.7 (36.0–37.4) | 19.0 (18.4–19.6) | 55.7 (55.0–56.4) |
| Yes | 876 | 51.9 (48.6–55.3) | 38.4 (35.1–41.7) | 90.3 (88.1–92.2) |
| Crash within the Prior 3 years | ||||
| No | 15,450 | 36.7 (36.0–37.5) | 17.3 (16.7–17.9) | 54.1 (53.2–54.9) |
| Yes | 3041 | 38.3 (36.6–40.1) | 22.3 (20.8–23.8) | 60.6 (58.8–62.3) |
| Blood Alcohol Concentration (in g/dL) | ||||
| 0.00 | 11,977 | 19.8 (19.1–20.5) | 8.7 (8.2–9.2) | 28.5 (27.7–29.3) |
| 0.01-0.07 | 1079 | 59.0 (56.0–62.0) | 41.0 (38.0–44.0) | 100 |
| ≥ 0.08 | 7015 | 64.3 (63.2–65.5) | 35.7 (34.5–36.8) | 100 |
| Day of Crash | ||||
| Friday-Sunday | 10,126 | 41.7 (40.7–42.6) | 20.6 (19.9–21.4) | 62.3 (61.4–63.3) |
| Monday-Thursday | 10,024 | 33.2 (32.3–34.2) | 19.1 (18.3–19.8) | 52.3 (51.3–53.3) |
| Time of Crash | ||||
| Day (7:00 am and 6:59 pm) |
9755 | 28.2 (27.3–29.1) | 14.8 (14.1–15.5) | 43.0 (42.0–44.0) |
| Night (7:00 pm and 6:59 am) |
10,091 | 46.0 (45.1–47.0) | 24.4 (23.6–25.3) | 70.4 (69.5–71.3) |
| Year of Crash | ||||
| 2005 | 4133 | 36.8 (35.4–38.3) | 19.8 (18.6–21.0) | 56.6 (55.1–58.1) |
| 2006 | 4368 | 37.3 (35.9–38.8) | 18.7 (17.6–19.9) | 56.0 (54.6–57.5) |
| 2007 | 4337 | 38.1 (36.7–39.6) | 19.2 (18.1–20.4) | 57.3 (55.9–58.8) |
| 2008 | 3960 | 37.6 (36.1–39.1) | 20.1 (18.9–21.4) | 57.7 (56.1–59.2) |
| 2009 | 3352 | 37.4 (35.8–39.1) | 22.0 (20.6–23.4) | 59.4 (57.7–61.1) |
| Survival Time After Crash Death | ||||
| Instantly | 9968 | 37.9 (37.0–38.9) | 20.2 (19.4–21.0) | 58.1 (57.2–59.1) |
| 1-59 minutes | 10,182 | 37.0 (36.1–38.0) | 19.5 (18.7–20.3) | 56.5 (55.6–57.5) |
| Death Location | ||||
| At scene | 16,180 | 37.9 (37.1–38.6) | 20.7 (20.0–21.3) | 58.5 (57.8–59.3) |
| En route | 163 | 35.6 (28.3–43.4) | 16.0 (10.7–22.5) | 51.5 (43.6–59.4) |
| Other | 3801 | 35.8 (34.3–37.4) | 16.6 (15.5–17.8) | 52.4 (50.8–54.0) |
Totals vary due to missing data.
Alcohol is treated as a drug.
Multivariable modeling revealed that drug use was significantly more prevalent among drivers who died in single-vehicle crashes (aPR 1.69, 95% CI: 1.62–1.76), or nighttime crashes (aPR 1.43, 95% CI: 1.39–1.47), or who had a driving-while-intoxicated conviction within the past three years (aPR 1.41, 95% CI: 1.35–1.47), and less prevalent among drivers or who were 65 years or older (aPR 0.45, 95% CI: 0.42– 0.49), Asian (aPR 0.47, 95% CI 0.41–0.53), or female (aPR 0.88, 95% CI: 0.85–0.91), or who were operating a motor carrier (aPR 0.41, 95% CI 0.34–0.48) (Table 4). Results from multivariable models for single-drug use and polydrug use were generally consistent (Table 4).
Table 4.
Estimated Adjusted Prevalence Ratio (aPR) and 95% Confidence Intervals (CI) of Single and Polydrug Use by Driver and Crash Characteristics for Fatally Injured Drivers who Died Within One Hour of the Crash, Selected States, United States, 2005–2009
| Characteristic | Positive for One Druga |
Positive for Two or More Drugsa |
Positive in Total |
|---|---|---|---|
|
| |||
| aPR (95% CI) | aPR (95% CI) | aPR (95% CI) | |
| Age (in years) | |||
| <25 | 0.78 (0.75–0.81) | 0.69 (0.64–0.73) | 0.80 (0.77–0.83) |
| 25-34 | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| 35-44 | 1.00 (0.97–1.04) | 1.02 (0.96–1.08) | 1.01 (0.98–1.05) |
| 45-54 | 0.93 ( 0.89–0.97) | 0.98 (0.91–1.04) | 0.99 (0.95–1.03) |
| 55-64 | 0.71(0.67–0.76) | 0.62 (0.56–0.68) | 0.75 (0.71–0.79) |
| ≥ 65 | 0.51 (0.47–0.55) | 0.27 (0.24–0.32) | 0.45 (0.42–0.49) |
| Sex | |||
| Female | 0.79 (0.76–0.82) | 0.84 (0.79–0.89) | 0.88 (0.85–0.91) |
| Male | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| Race | |||
| White | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| Black | 0.91 (0.87–0.96) | 0.78 (0.71–0.86) | 0.86 (0.82–0.91) |
| Asian | 0.56 (0.49–0.64) | 0.25 (0.18–0.35) | 0.47 (0.41–0.53) |
| Native American | 1.30 (1.16–1.46) | 1.53 (1.31–1.78) | 1.33 (1.20–1.48) |
| Other | 0.86 (0.72–1.04) | 0.64 (0.43–0.93) | 0.80 (0.67–0.96) |
| Unknown | 0.89 (0.80–0.98) | 0.73 (0.62–0.87) | 0.83 (0.75–0.92) |
| Ethnicity | |||
| Hispanic | 0.90 (0.86–0.94) | 0.73 (0.67–0.79) | 0.83 (0.80–0.87) |
| Non-Hispanic | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| Unknown | 1.02 (0.94–1.13) | 0.99 (0.84–1.17) | 0.99 (0.90–1.08) |
| Driver Type | |||
| Motor carrier | 0.40 (0.34–0.48) | 0.24 (0.18–0.33) | 0.41 (0.34–0.48) |
| Non-motor carrier | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| Number of Vehicles Involved | |||
| 1 | 1.68 (1.61–1.75) | 2.36 (2.19–2.54) | 1.69 (1.62–1.76) |
| ≥ 2 | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| DWI conviction within the prior 3 years | |||
| No | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| Yes | 1.44 (1.38–1.49) | 1.81 (1.70–1.93) | 1.41 (1.35–1.47) |
| Crash within the prior 3 years | |||
| No | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| Yes | 1.04 (1.00–1.07) | 1.20 (1.13–1.27) | 1.11 (1.08–1.15) |
| Day of Crash | |||
| Friday-Sunday | 1.15 (1.12–1.18) | 1.13 (1.08–1.18) | 1.07 (1.04–1.09) |
| Monday-Thursday | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| Time of Crash | |||
| Day (7:00 am and 6:59 pm) |
1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| Night (7:00 pm and 6:59 am) |
1.67 (1.62–1.73) | 1.76 (1.67–1.85) | 1.43 (1.39–1.47) |
| Year of Crash | |||
| 2005 | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| 2006 | 1.00 (0.96–1.05) | 1.02 (0.95–1.09) | 1.01 (0.97–1.05) |
| 2007 | 1.01 (0.97–1.05) | 1.00 (0.93–1.07) | 0.99 (0.96–1.03) |
| 2008 | 1.02 (0.97–1.06) | 1.04 (0.97–1.12) | 1.03 (0.99–1.07) |
| 2009 | 1.06 (1.01–1.11) | 1.19 (1.10–1.28) | 1.12 (1.07–1.17) |
| Death Location | |||
| At scene | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| En route | 1.01 (0.88–1.17) | 1.06 (0.85–1.13) | 1.06 (0.93–1.20) |
| Other | 0.91 (0.89–0.94) | 0.87 (0.83–0.92) | 0.93 (0.90–0.95) |
Alcohol is treated as a drug.
DISCUSSION
Results of this study indicate that more than half (57%) of fatally injured drivers in the United States had been using at least one drug and 20% had been using two or more drugs. The prevalence of single-drug use and polydrug use reported in this study is generally consistent with previous reports from the United States and Canada [26, 27, 41]. The large sample size of this study made it possible to examine the specific drugs involved in polydrug use and the driver characteristics associated with drug use. Despite the decline of alcohol-related motor vehicle crashes in recent years [42, 43], alcohol remains the most commonly detected drug, present in 40% of fatally injured drivers dying within one hour of the crash. In two- and three-drug combinations, alcohol was most frequently detected in the presence of marijuana and stimulants, with cocaine and methamphetamine being the most commonly used stimulant drugs.
The prevalence of single-drug use and polydrug use varies significantly with driver characteristics. In addition to several demographic variables known to be associated with drug use, such as sex, age, race, and ethnicity, this study adds more evidence for DWI history as a valid marker of subsequent use of alcohol and other drugs and for the effectiveness of mandatory drug testing programs in improving driving safety. With adjustment for demographic characteristics, drivers with a DWI history in the past three years are 44% more likely than drivers without a DWI history to test positive for single-drug use, and 81% more likely to test positive for two or more drugs. Furthermore, motor carrier drivers, who are subject to mandatory alcohol and drug testing programs, were substantially less likely than other drivers to test positive for alcohol and other drugs. Similar findings have been reported in previous research [33, 44, 45], suggesting that mandatory alcohol and drug education, testing, and vehicle interlocks should be part of the punitive consequences of DWI and driving under the influence [46].
Debate exists over how best to classify medications and drugs in relation to driving safety, as it can be difficult to determine whether a substance is used as prescribed, or as intended [47]. Detection of drugs may indicate the use of illegal drugs, prescription drugs, or over-the-counter drugs, but does not necessarily imply that a drug was misused. In this study, the “other” drug category may include substances not considered to impair driving performance, but “other” drug use nevertheless is significant because the implications of ingesting multiple substances, illicit, prescription, or over-the-counter are not fully understood [19, 20, 48-49]. Therefore, understanding what drugs may be included in the “other” drug category is important. A study of crash fatalities in the United Kingdom shows that a range of prescription and over-the-counter medications are classified as “other”, including anti-convulsants, anti-histamines, anti-inflammatories, anti-psychotics, cardiac drugs and diabetic drugs [50]. Drugs of abuse captured as “other” drugs in the UK study [50], i.e., gamma hydroxybutyric acid, benzylpiperazine, and ketamine, are categorized by the FARS coding manual and the present study as depressants, “other” drugs, and hallucinogens, respectively.
Although this study provides compelling evidence about the prevalence and correlates of AOD in driver fatalities, it is subject to several limitations. First, the study sample is limited to fatally injured drivers who died within one hour of the crash in states where toxicological testing is performed on a routine basis. Although the inclusion and exclusion criteria for selecting the study subjects help enhance the internal validity of the study, they may reduce the generalizability of the findings across different driver population groups and geographic regions. The prevalence of AOD detected in non-fatally injured drivers [51] and in roadside surveys [24] is generally much lower than reported in this study, implying that use of alcohol and other drugs is associated with increased injury severity and heightened crash risk [52, 53].
Second, this study examined drug use, which may or may not correspond to acute impairment. There is no uniformly accepted definition of impairment by different drugs [46, 54]. Variations in individual tolerance, pharmacological characteristics of different drugs, and dose make it difficult to identify drug impairment [1, 38, 55]. Discerning drug impairment from drug involvement is not possible from these data as the amount of drug present was not available in the FARS data, and because the physiological effects differ by drug and the effects of drugs are more varied and less well defined than, for example, alcohol [38, 39]. Legal definitions of drug impairment differ from state to state. As of 2008, impairment related to drugs was defined in 15 states as operating a motor vehicle with any detectable level of an illicit drug or its metabolites [3]. Other states have characterized impairment as substance use that reduces a driver’s ability to operate a vehicle safely by diminishing motor skills and reaction time and altering perception [3, 56]. Moreover, drug detection could represent the presence of a drug metabolite from past use [54]. A person can test positive for a non-alcohol drug (e.g., marijuana) several weeks after use. Therefore, a positive test result identified drug use, but does not necessarily indicate that the user was impaired by the drug at the time of the test.
Finally, it was not possible to discern if polydrug use reflected concurrent or simultaneous ingestion of drugs. Simultaneous polydrug use has been shown to confer greater morbidity and negative health consequences [57, 58].
The complexity involved with studying drug impairment has led researchers to put forth a number of recommendations to more effectively examine drugged driving, including training of coroners, pathologists, and toxicologists to ensure complete laboratory analyses (preferably using whole blood) for a standardized list of drugs [25, 30, 59]. The guidelines will likely facilitate research by clarifying what drugs are categorized in the other drug classification and helping to identify interaction effects of different drug combinations on driving safety [25, 30, 59, 60].
The results of this study indicate that use of AOD is pervasive among fatally injured drivers in the United States. Alcohol is the most frequently used drug both alone and in combination with other drugs. In view of the magnitude of AOD in fatally injured drivers, expanding routine drug testing of drivers involved in motor vehicle crashes is warranted. For non-fatally injured drivers, an initial screening of oral fluid may help decide whether to obtain a blood or urine sample [61]. Screening oral fluid would allow a wider group of drivers to be studied and may serve as a deterrent against driving under the influence of alcohol and other drugs.
ACKNOWLEDGEMENTS
This work was supported by grants R21DA029670 from the National Institute on Drug Abuse and AA009963 from the National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health. The authors wish to thank Ms. Barbara Lang for her editorial and administrative assistance.
This research was supported by grants DA029670 from the National Institute on Drug Abuse and AA009963 from the National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health. The authors have no connection with the tobacco, alcohol, pharmaceutical or gaming industries. No constraints on publishing exist.
Footnotes
DECLARATION OF INTEREST The authors have no conflicts of interest to declare.
References
- 1.Goodnough A, Zezima K. Drivers on prescription drugs are hard to convict. The New York Times. 2010 Jul 25;:A1. [Google Scholar]
- 2.Baker A, Foderaro LW. Tests Show Driver was Drunk in Parkway Crash That Killed 8. The New York Times. 2009 Aug 4;:A1. [Google Scholar]
- 3.National Institute on Drug Abuse . Drugged driving. National Institute on Drug Abuse, National Institutes of Health, US Department of Health & Human Services; Bethesda, MD: [Accessed November 10, 2011]. 2010. Available at: http://www.nida.nih.gov/infofacts/driving.html. Archived at: http://www.webcitation.org/63692Otpq. [Google Scholar]
- 4.Walsh JM, DuPont RL. The Drugged Driving Epidemic. The Washington Post. 2007 Jun 17; [Google Scholar]
- 5.McCarthy ML. Prescription drug abuse up sharply in the USA. Lancet. 2007;369(9572):1505–6. doi: 10.1016/S0140-6736(07)60690-4. [DOI] [PubMed] [Google Scholar]
- 6.Volkow ND. [Accessed November 10, 2011];Scientific Research on Prescription Drug Abuse. Statement Before the Subcommittee on Crime and Drugs of the Senate Judiciary Committee. 2008 Mar 12; 110th Congress, 2nd Session. Available from: http://www.hhs.gov/asl/testify/2008/03/t20080312a.html. Archived at: http://www.webcitation.org/6369HiIe6.
- 7.Cai R, Crane E, Poneleit K, Paulozzi L. Emergency department visits involving nonmedical use of selected prescription drugs in the United States, 2004–2008. J Pain Palliat Care Pharmacother. 2010;24(3):293–7. doi: 10.3109/15360288.2010.503730. [DOI] [PubMed] [Google Scholar]
- 8.Substance Abuse and Mental Health Services Administration. Drug Abuse Warning Network 2009: Selected Tables of National Estimates of Drug-Related Emergency Department Visits. Center for Behavioral Health Statistics and Quality; Rockville, MD: 2010. [Google Scholar]
- 9.Paulozzi LJ. [Accessed November 10, 2011];Trends in Unintentional Drug Overdose Deaths. Statement Before the Subcommittee on Crime and Drugs of the Senate Judiciary Committee. 2008 March 12; 110th Congress, 2nd Session. (Testimony of Leonard J. Paulozzi, MD, Medical Epidemiologist, Division of Unintentional Injury Prevention of the National Center for Injury Prevention and Control). Available from: http://www.hhs.gov/asl/testify/2008/03/t20080312b.html. Archived at: http://www.webcitation.org/6369SLNC6.
- 10.National Highway Traffic Safety Administration . Drug Involvement in Fatally Injured Drivers. In: National Center for Statistics and Analysis, editor. Traffic Safety Facts. National Center for Statistics and Analysis, National Highway Traffic Safety Administration; Washington, DC: 2010. (Report No. DOT HS 811 415) [Google Scholar]
- 11.LeRoy A, Morse M. l. Multiple Medications and Vehicle Crashes: Analysis of Databases. National Highway Traffic Safety Administration; Washington, DC: 2009. (Report No. DOT HS 810 858) [Google Scholar]
- 12.Results from the 2009 National Survey on Drug Use and Health: Volume I. Summary of National Findings. Department of Health and Human Services; Rockville, MD: [Accessed November 10, 2011]. 2010. Substance Abuse and Mental Health Services Administration. Available from: http://oas.samhsa.gov/NSDUH/2k9NSDUH/2k9Results.htm#1.1. Site prohibits archiving. [Google Scholar]
- 13.Dupont RL, Voas RB, Walsh JM, Shea C, Talpins SK, Neil MM. The need for drugged driving per se laws: a commentary. Traffic Inj Prev. 2012;13(1):31–42. doi: 10.1080/15389588.2011.632658. [DOI] [PubMed] [Google Scholar]
- 14.Office of National Drug Control Policy (ONDCP) 2011 National Drug Control Strategy. The White House Administration Office of National Drug Control Policy; Washington (DC): [Accessed January 27, 2012]. 2011a. Available from: http://www.whitehouse.gov/ondcp/2011-national-drug-control-strategy. Archived at: http://www.webcitation.org/65ljtkfhY. [Google Scholar]
- 15.Office of National Drug Control Policy (ONDCP) Drugged Driving. The White House Administration Office of National Drug Control Policy; Washington (DC): [Accessed January 27, 2012]. 2011b. Available from: http://www.whitehouse.gov/ondcp/drugged-driving. Archived at: http://www.webcitation.org/65ljnp5fz. [Google Scholar]
- 16.Kerlikowske RD, Sabet K. Commentary on Voas et al. (2011): drug-free roadways - can we get there from here? Steps to reducing drugged driving in the United States. Addiction. 2011;106(7):1228–9. doi: 10.1111/j.1360-0443.2011.03470.x. [DOI] [PubMed] [Google Scholar]
- 17.Stramer GA, Bird KD. Investigating drug-ethanol interactions. Br J clin Pharmac. 1984;18:27S–35S. doi: 10.1111/j.1365-2125.1984.tb02580.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Highway Traffic Safety Administration Marijuana and alcohol combined severely impede driver performance. Ann Emerg Med. 2000;35:398–9. [PubMed] [Google Scholar]
- 19.Gjerde H, Kinn G. Impairment of Drivers due to Cannabis in Combination with Other Drugs. Forensic Science International. 1991;50:57–60. doi: 10.1016/0379-0738(91)90133-4. [DOI] [PubMed] [Google Scholar]
- 20.Weathermon R, Crabb D. Alcohol and Medication Interactions. Alcohol Research & Health. 1999;23(1):40–54. [PMC free article] [PubMed] [Google Scholar]
- 21.Movig KL, Mathijssen M, Nagel P, van Egmond T, de Gier JJ, Leufkens HG, et al. Pyschoactive substance use and the risk of motor vehicle accidents. Accident Analysis and Prevention. 2004;36:631–6. doi: 10.1016/S0001-4575(03)00084-8. [DOI] [PubMed] [Google Scholar]
- 22.Drummer O. Epidemiology and traffic safety: culpability studies. In: Verster J, Pandi-Perumal SR, Ramaekers JG, de Gier JJ, editors. Drugs, Driving and Traffic Safety. Verlag; Basel, Switzerland: 2009. [Google Scholar]
- 23.Leung SY. Benzodiazepines, opioids and driving: An overview of the experimental research. Drug and Alcohol Review. 2011;30:281–6. doi: 10.1111/j.1465-3362.2011.00311.x. [DOI] [PubMed] [Google Scholar]
- 24.Lacey JH, Kelley-Baker T, Furr-Holden D, Voas RB, Romano E, Ramirez A, et al. 2007 National roadside survey of alcohol and drug use by drivers: drug results. National Highway Traffic Safety Administration; Washington, DC: 2009. (Report No. DOT HS 811 249) [Google Scholar]
- 25. [Accessed May 16, 2012];Prevalence of Alcohol and Other Psychoactive Substances in Drivers in General Traffic. Part I: General Results. Driving under the Influence of Drugs, Alcohol, and Medicines. 6th Framework Program Deliverable 2.2.3. Available from: http://www.druid-project.eu/cln_031/nn_107534/sid_B21CAD080C96E7B112DEA0E3C2B077AA/nsc_true/Druid/EN/deliverales-list/deliverables-list-node.html?__nnn=true. Archived at: http://www.webcitation.org/65lkh0El7.
- 26.Walsh JM, Flegel R, Atkins R, Cangianelli LA, Cooper C, Welsh C, et al. Drugs and alcohol use among drivers admitted to a Level-1 trauma center. Accident Analysis and Prevention. 2005;37:894–901. doi: 10.1016/j.aap.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 27.Kaplan J, Kraner J, Paulozzi L. Alcohol and other drug use among victims of motor-vehicle crashes–West Virginia, 2004–2005. MMWR Morb Mortal Wkly Rep. 2006;55(48):1293–6. [PubMed] [Google Scholar]
- 28.Officer J. Trends in drug use of Scottish drivers arrested under Section 4 of the Road Traffic Act -A 10 year review. Science and Justice. 2009;49:237–41. doi: 10.1016/j.scijus.2009.09.016. [DOI] [PubMed] [Google Scholar]
- 29.Karjalainen K, Lintonen T, Impinen AO, Lillsunde PM, Ostamo AI. Poly-drug findings in drugged driving cases during 1977-2007. Journal of Substance Use. 2010;15(2):143–56. [Google Scholar]
- 30. [Accessed February 21, 2012];Driving under the Influence of Drugs, Alcohol, and Medicines. 6th Framework Program Deliverable 2.2.5. Prevalence of alcohol and other psychoactive substances in injured and killed drivers. Available from: http://www.druid-project.eu/cln_031/nn_107534/sid_B21CAD080C96E7B112DEA0E3C2B077AA/nsc_true/Druid/EN/deliverales-list/deliverables-list-node.html?__nnn=true. Archived at: http://www.webcitation.org/65lkh0El7.
- 31.National Highway Traffic Safety Administration . FARS Analytic Reference Guide, 1975 to 2009. National Highway Traffic Safety Administration; Washington, DC: [Accessed November 10 2011]. 2010. Available from: http://www-nrd.nhtsa.dot.gov/Pubs/811352.pdf. Archived at: http://www.webcitation.org/636A2RE7c. [Google Scholar]
- 32.Substance Abuse and Mental Health Services Administration . National Survey on Drug Abuse and Health Report. State Estimates of Drunk and Drugged Driving. Substance Abuse and Mental Health Services Administration; Rockville, MD: [Accessed November 10, 2011]. 2010. Available from: http://www.oas.samhsa.gov/2k10/205/DruggedDriving.htm. Site prohibits archiving. [Google Scholar]
- 33.Shepard M. Experts concerned about ‘drug driving’. Albuquerque journal. 2006 Jan 7;:A1. [Google Scholar]
- 34.Brady JE, Baker SP, DiMaggio C, McCarthy ML, Rebok GW, Li G. Effectiveness of mandatory alcohol testing programs in reducing alcohol-related fatal crashes involving motor carriers. Am J Epidemiol. 2009;170:775–82. doi: 10.1093/aje/kwp202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162:199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 36.Li L, Zhang X, Levine B, Li G, Zielke HR, Fowler DR. Trends and pattern of drug abuse deaths in Maryland teenagers. J Forensic Sci. 2011;56(4):1029–33. doi: 10.1111/j.1556-4029.2011.01743.x. [DOI] [PubMed] [Google Scholar]
- 37.National Highway Traffic Safety Administration . FARSHELF. FARS Coding and Validation Manual 2008. National Highway Traffic Safety Administration; Washington, DC: 2008. [Google Scholar]
- 38.Walsh JM, de Gier JJ, Christopherson AS, Verstraete AG. Drugs and driving. Traffic Inj Prev. 2004;5(3):241–53. doi: 10.1080/15389580490465292. [DOI] [PubMed] [Google Scholar]
- 39.The Walsh Group . The feasibility of per se drugged driving legislation: consensus report. The Walsh Group; Bethesda, MD: 2002. p. 15pp. [Google Scholar]
- 40.Smink BE, Ruiter B, Lusthof KJ, Zweipfenning PG. Driving under the influence of alcohol and/or drugs in the Netherlands 1995-1998 in view of the German and Belgian legislation. Forensic Science International. 2001;120:195–203. doi: 10.1016/s0379-0738(00)00476-x. [DOI] [PubMed] [Google Scholar]
- 41.Brault M, Dussault J, Bouchard J, Lemire AM. The contribution of alcohol and other drugs among fatally injured drivers in Quebec: Final results. In: Olivier J, Williams P, Clayton A, editors. Proceedings of the 17th International Conference on Alcohol, Drugs and Traffic Safety; Glasgow, UK. International Council on Alcohol, Drugs and Traffic Safety; 2004. [Google Scholar]
- 42.National Highway Traffic Safety Administration . Alcohol-Impaired Driving. In: National Center for Statistics and Analysis, editor. Traffic Safety Facts. National Center for Statistics and Analysis, National Highway Traffic Safety Administration; Washington, DC: 2009. (Report No. DOT HS 811 155) [Google Scholar]
- 43.National Highway Traffic Safety Administration . Alcohol-Impaired Driving. In: National Center for Statistics and Analysis, editor. Traffic Safety Facts. National Center for Statistics and Analysis, National Highway Traffic Safety Administration; Washington, DC: [Accessed November 10, 2011]. 2010. (Report No. DOT HS 811 385). Available from: http://www-nrd.nhtsa.dot.gov/Pubs/811385.pdf. Archived at: http://www.webcitation.org/636ASVwW7. [Google Scholar]
- 44.Hingson R, Zha W. Changes In and Predictors of Driving after Drug Use and Involvement in Traffic Crashes because of Drugs, 1992–2005. In: Verster J, Pandi-Perumal SR, Ramaekers JG, de Gier JJ, editors. Drugs, Driving and Traffic Safety. Verlag; Basal, Switzerland: 2009. [Google Scholar]
- 45.Impinen A, Rahkonen O, Karjalainen K, Lintonen T, Lillsunde P, Ostamo A. Substance use as a predictor of driving under the influence (DUI) rearrests: A 15-year retrospective study. Traffic Injury Prevention. 2009;10(3):220–6. doi: 10.1080/15389580902822725. [DOI] [PubMed] [Google Scholar]
- 46.Voas R, DuPont R, Talpins S, Shea CL. Towards a national model for managing impaired driving offenders. Addiction. 2011;106:1221–7. doi: 10.1111/j.1360-0443.2010.03339.x. [DOI] [PubMed] [Google Scholar]
- 47.Alvarez FJ, del Rio MC. Medicinal Drugs and driving: From research to clinical practice. Trends in Pharmacological Science. 2002;23(9):441–3. doi: 10.1016/s0165-6147(02)02083-7. [DOI] [PubMed] [Google Scholar]
- 48.McGwin G, Sims RV, Pulley L, Roseman JM. Relations among chronic medical conditions, medications and automobile crashes in the elderly: A population-based case-control study. Am J Epidemiol. 2000;152(5):424–31. doi: 10.1093/aje/152.5.424. [DOI] [PubMed] [Google Scholar]
- 49.Engeland A, Skurtveit S, Morland J. Risk of road traffic accidents associated with the prescription of drugs: a registry-based cohort study. Ann Epidemiol. 2007;17(8):597–602. doi: 10.1016/j.annepidem.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 50.Elliot S, Woolacott H, Braithwaite R. The prevalence of drugs and alcohol found in traffic fatalities: A comparative study of victims. Science and Justice. 2009;49:19–23. doi: 10.1016/j.scijus.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 51.Longo MC, Hunter CE, Lokan RJ, White JM, White MA. The prevalence of alcohol, cannabinoids, benzodiazepines and stimulants amongst injured drivers and their role in driver culpability - Part I: the prevalence of drug use in drivers, and characteristics of the drug-positive group. Accident Analysis and Prevention. 2000;32(5):613–22. doi: 10.1016/s0001-4575(99)00111-6. [DOI] [PubMed] [Google Scholar]
- 52.Li G, Keyl PM, Smith GS, Baker SP. Alcohol and injury severity: reappraisal of the continuing controversy. J Trauma. 1997;42(3):562–9. doi: 10.1097/00005373-199703000-00032. [DOI] [PubMed] [Google Scholar]
- 53.Li MC, Brady JE, DiMaggio CJ, Lusardi AR, Tzong KY, Li G. Marijuana Use and Motor Vehicle Crashes: A Meta-analysis. Epidemiol Rev. 2012;34(1):65–72. doi: 10.1093/epirev/mxr017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ramaekers JG. Pitfalls in estimating drug-related crash risk. Trends Pharmacol Sci. 2003;24(3):114–5. doi: 10.1016/S0165-6147(03)00030-0. [DOI] [PubMed] [Google Scholar]
- 55.Alvarez FJ, Del Rio MC. Response to Ramaekers: Pitfalls in estimating drug-related crash risk. Trends Pharmacol Sci. 2003;24(3):115. doi: 10.1016/S0165-6147(03)00030-0. [DOI] [PubMed] [Google Scholar]
- 56.Kelly E, Darke S, Ross J. A review of drug use and driving: epidemiology, impairment, risk factors and risk perceptions. Drug Alcohol Rev. 2004;23(3):319–44. doi: 10.1080/09595230412331289482. [DOI] [PubMed] [Google Scholar]
- 57.Collins R, Ellickson P, Bell R. Simultaneous Polydrug Use among Teens: Prevalence and Predictors. Journal of Substance Abuse. 1999;10(3):233–53. doi: 10.1016/s0899-3289(99)00007-3. [DOI] [PubMed] [Google Scholar]
- 58.McCabe SE, Cranford JA, Morales M, Young A. Simultaneous and Concurrent Polydrug Use of Alcohol and Prescription Drugs: Prevalence, Correlates and Consequences. Journal of Studies on Alcohol. 2006;67:529–37. doi: 10.15288/jsa.2006.67.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Walsh JM, Verstraete AG, Huestis MA, Morland J. Guidelines for research on drugged driving. Addiction. 2008;103(8):1258–68. doi: 10.1111/j.1360-0443.2008.02277.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Busko M. [Accessed September 6, 2011];Drugged driving research guidelines will make study comparisons easier [electronic article] Medscape Medical News. 2008 Available at: http://www.medscape.com/viewarticle/579572. Archived at: http://www.webcitation.org/636BG1rM9.
- 61.Gjerde H, Mordal J, Christophersen AS, Bramness JG, Morland J. Comparison of drug concentrations in blood and oral fluid collected with the intercept sampling device. J Anal Toxicol. 2010;34(4):204–9. doi: 10.1093/jat/34.4.204. [DOI] [PubMed] [Google Scholar]