Abstract
Objective
Various procedures have been introduced for anterior interbody fusion in degenerative cervical disc disease including plate systems with autologous iliac bone, carbon cages, and cylindrical cages. However, except for plate systems, the long-term results of other methods have not been established. In the present study, we evaluated radiologic findings for cylindrical cervical cages over long-term follow up periods.
Methods
During 4 year period, radiologic findings of 138 patients who underwent anterior cervical fusion with cylindrical cage were evaluated at 6, 12, 24, and 36 postoperative months using plain radiographs. We investigated subsidence, osteophyte formation (anterior and posterior margin), cage direction change, kyphotic angle, and bone fusion on each radiograph.
Results
Among the 138 patients, a minimum of 36 month follow-up was achieved in 99 patients (mean follow-up : 38.61 months) with 115 levels. Mean disc height was 7.32 mm for preoperative evaluations, 9.00 for immediate postoperative evaluations, and 4.87 more than 36 months after surgery. Osteophytes were observed in 107 levels (93%) of the anterior portion and 48 levels (41%) of the posterior margin. The mean kyphotic angle was 9.87° in 35 levels showing cage directional change. There were several significant findings : 1) related subsidence [T-score (p=0.039) and anterior osteophyte (p=0.009)], 2) accompanying posterior osteophyte and outcome (p=0.05).
Conclusion
Cage subsidence and osteophyte formation were radiologically observed in most cases. Low T-scores may have led to subsidence and kyphosis during bone fusion although severe neurologic aggravation was not found, and therefore cylindrical cages should be used in selected cases.
Keywords: Cylindrical cage, Kyphosis, Osteophyte, Radiologic, Subsidence
INTRODUCTION
Anterior cervical discectomy and fusion (ACDF) is widely recommended and is the gold standard of treatment in degenerative cervical disease9,12,36). In addition, autografts of iliac crest bone for ACDF are associated with higher fusion rates than allografts due to superior osteoconductive and osteoinductive properties2,13). However, complications related to autologous iliac bone graft include severe donor site pain, increased operative time, and wound infection2). Recently, to overcome these disadvantages, surgical techniques using cages have been recommended1,3,23). Among these devices, the cylindrical titanium cages had been used, sometimes, with the advantages such as easy maneuverability and short operating time23). However, recently, the use of plating system is using to overcome the kyphosis and to restrict micro-motion. Here, we present the radiological and clinical outcomes of patients who underwent cylindrical cage procedures after long-term follow-up of at least 36 months.
MATERIALS AND METHODS
Patient selection
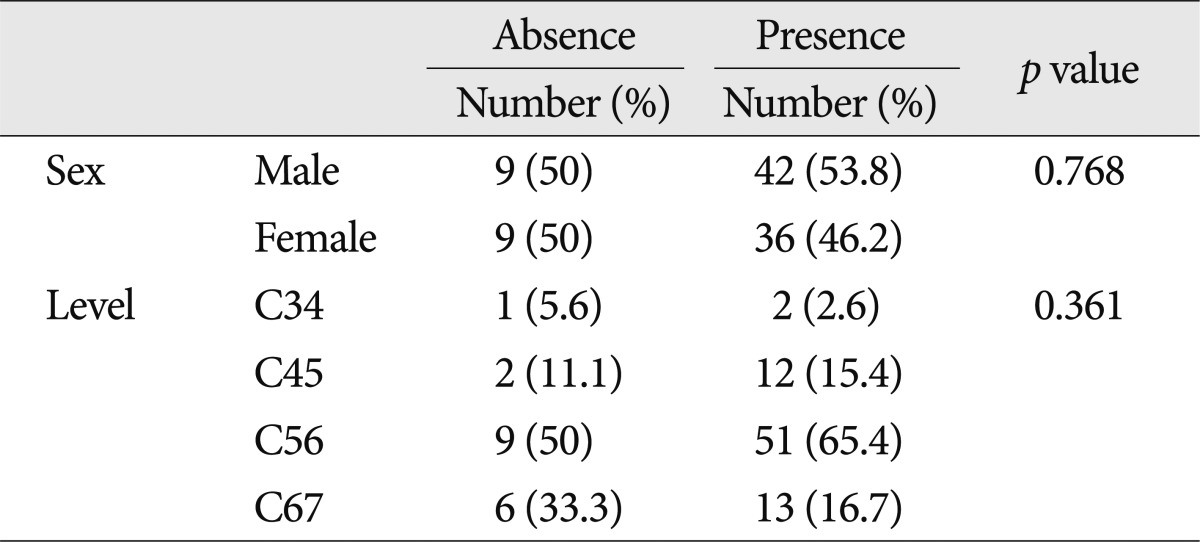
From 2003 to 2006, anterior interbody fusion with a cylindrical cage (AMSLU™ cage, Eurosurgical, Amsterdam, The Netherlands) was performed in 138 patients (Fig. 1). Among these patients, a total of 99 were followed-up for more than 36 months and were retrospectively enrolled in the present study through reviews of medical charts, operative notes, and radiologic images.
Fig. 1.
The cylindrical titanium cage (AMSLU™ cage, Eurosurgical, Amsterdam, The Netherlands) used in the present study.
Radiologic assessment
Plain radiographs including anterior-posterior views and lateral views including neutral, flexion, and extension were obtained during the preoperative period, immediately after surgery, 6 months, 12 months, 24 months, and at least 36 months after surgery.
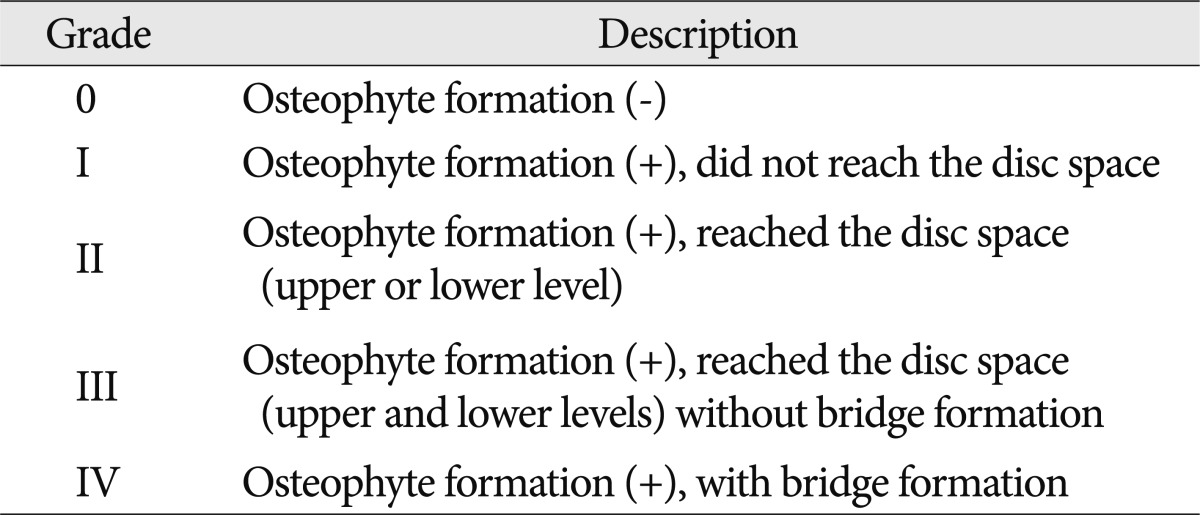
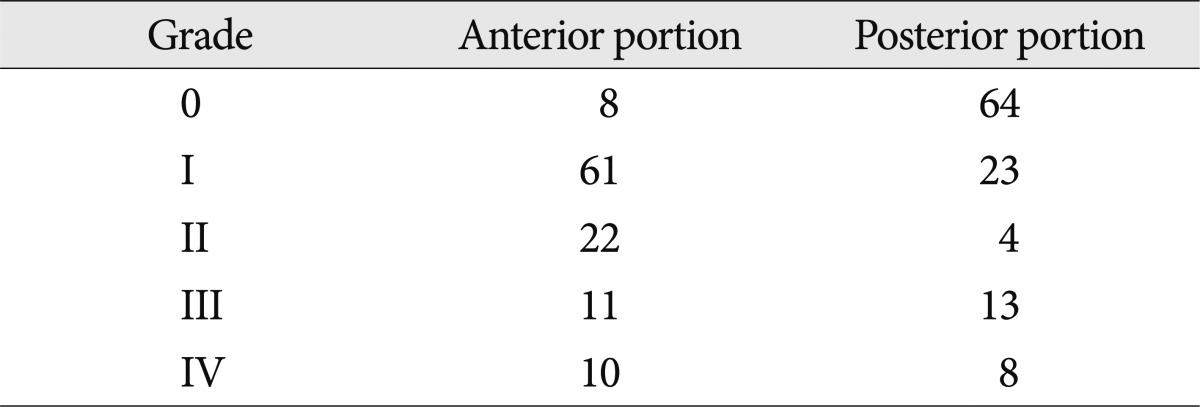
At each follow-up, we evaluated radiographs for bony fusion, subsidence, kyphotic angle from cage direction change, osteophyte formation of anterior and posterior portion, and surgical complications. For the evaluation of cage subsidence, intervertebral disc height was measured by dividing of the sum of the three points including the anterior, posterior, and midpoint interbody distance by 323). Subsidence was defined as any settlement in disc height of at least 3 mm on lateral radiographs. We defined bony fusion as occurring when segmental motion was not noted in dynamic radiographs and there was no radiolucency around the cage14). The kyphotic angle was measured between the superior line of the upper body and inferior line of the lower body of the vertebra only in the operative level when 12 months postoperative day, compared with immediate postoperative lateral views. The degree of osteophyte formation was evaluated using the classification scheme shown in Table 1. Whole series radiographs were used to determine surgical complications related to cage placement.
Table 1.
Osteophyte formation grades
Surgical technique
All surgical procedures were performed by a single surgeon using a standardized technique. Using a microscope, the anterior osteophyte was removed in order to approach the disc space, after which cervical dissection was performed by the traditional Smith-Robinson procedure. Next, causative lesions such as disc fragments or hard discs were removed as completely as possible to preserve the endplates with curettage. And then, the intervertebral disc space was reamed away with the decision of the cage height according to reamer size at the same time. The cylindrical cage packed with reamed bone and anterior osteophytic bone was inserted by turning an implant inserter clockwise and applying light pressure.
Clinical assessment
For assessments of clinical outcomes, visual analogue scale (VAS) scores were taken at the same radiologic follow-up times. Final clinical outcomes were assessed according to Odom's criteria35).
Statistical analysis
Spearman's correlation coefficient and phi correlation test were used to evaluate the relevance among age, sex, T-score, VAS score, and clinical outcome related to subsidence and location of osteophyte formation. The Mann-Whitney U test was used to identify relationships with subsidence of age, VAS score and T-score, while the chi-square test was used to analysis subsidence related factors including sex and levels. p-values less than 0.05 according to analyses using SPSS (Version 13.0 : SPSS Inc., Chicago, IL, USA) were considered statistically significant.
RESULTS
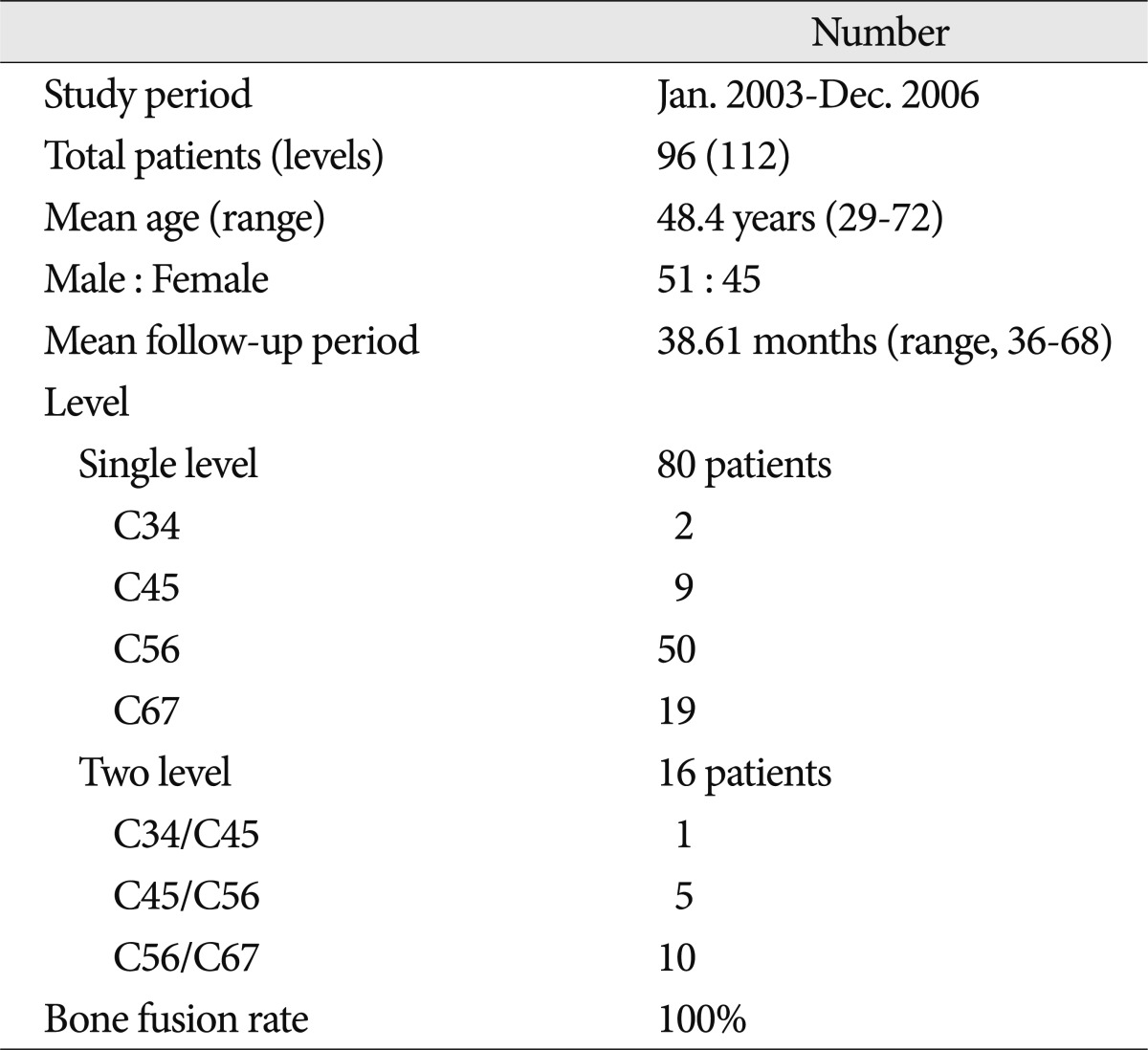
Patient demographics (Table 2)
Table 2.
Demographics of patients enrolled in the study
Among the 138 patients enrolled in the study, 38 patients with 47 levels were lost to follow-up. In addition, 4 cases were excluded due to early stage infection after receiving autologous iliac bone grafts using the anterior plate and screw system after infection control. Thus, a total of 96 patients (112 levels) were enrolled in the present study. The males were 51 patients and females were 45. The mean age of enrolled patients was 48.4±9.09 years (range, 29-72 years). The longest follow-up period was 68 months with a mean follow-up of 38.6±4.06 months. The levels of anterior interbody fusion surgery were C3-4 in 3 levels, C4-5 in 15, C5-6 in 65, and C6-7 in 29. Two-level surgery was performed on the C45/C45 levels in one patient, C45/C56 in 5 patients, and C56/C67 in 10 patients. Bone fusion was confirmed in all enrolled cases (100%) via dynamic lateral views at 12-month follow-up visits.
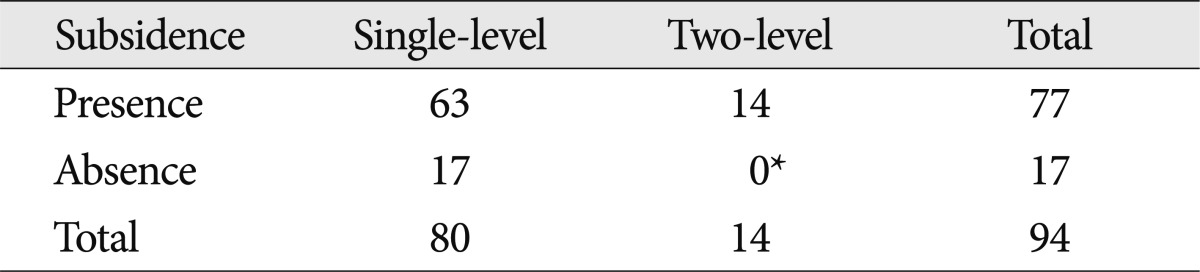
Subsidence (Table 3)
Table 3.
Comparisons of subsidence rate between single-level and two-level groups*
*Subsidence in one of the two levels in two cases
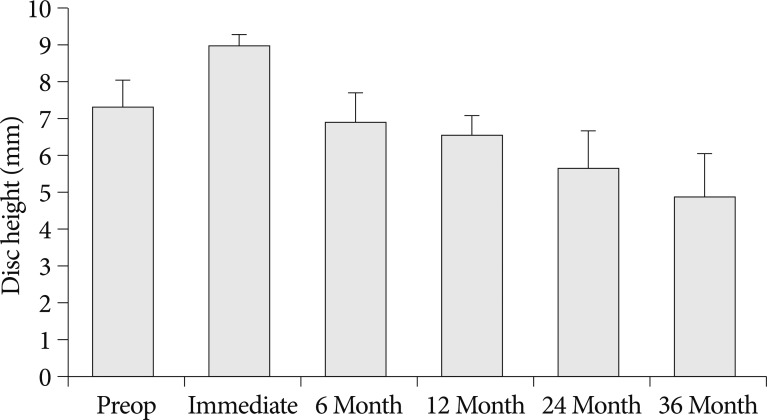
The mean disc heights were as follows : 7.32±0.73 mm in preoperative evaluations, 9.00±0.31 in immediate postoperative evaluations, 6.94±0.79 at 6 months, 6.54±0.57 at 12 months, 5.67±1.02 at 24 months, and 4.87±1.16 after more than 36 months after surgery (Fig. 2). The rates of subsidence were determined in 79 patients (82%) with 93 levels (83%). Of the 16 patients who had two-level fusion, subsidence of all levels was observed in 14 (88%) : the two remaining patients had subsidence at only one of the two levels (upper level in one patient and lower level in the other patient).
Fig. 2.
Graph presented the change pattern of subsidence according to the follow-up period. Subsidence progressed as time passed.
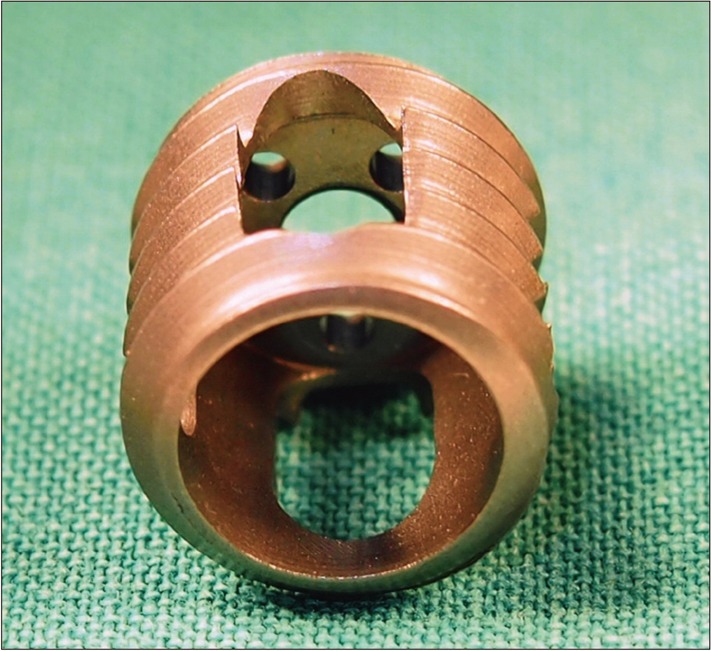
Osteophyte formation (Table 4)
Table 4.
Osteophyte formation after anterior cervical discectomy and fusion using cylindrical cage
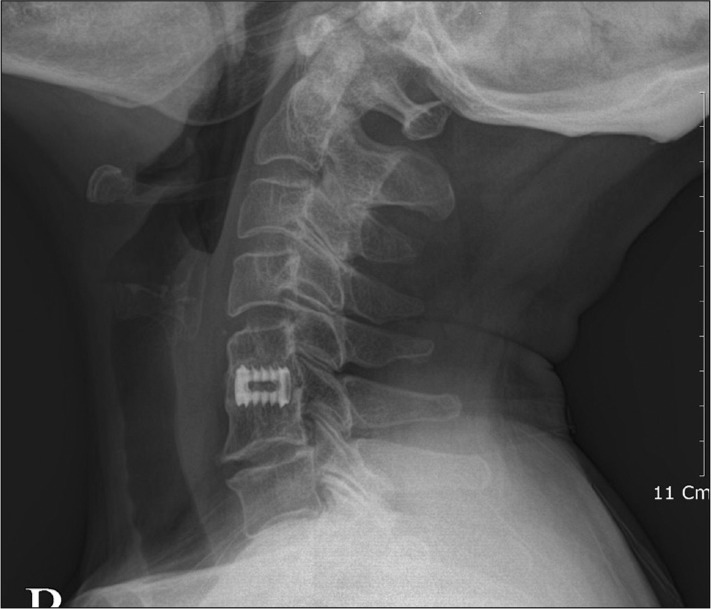
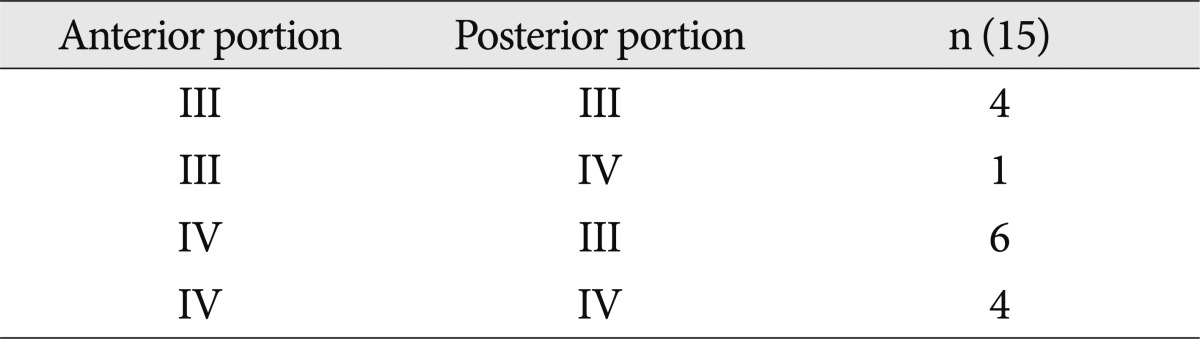
Formation of osteophytes (at least grade I) was observed in 104 levels (93%) of the anterior margin and 48 levels (43%) of the posterior margin. Additionally, grade III or worse osteophytes of the anterior and posterior portions were observed in 21 of the levels (19%). Among them, lateral X-rays simultaneously revealed grade IV osteophytes at the anterior and posterior margins (Fig. 3). Other conditions associated with osteophyte formation were as follows : grade IV of the anterior portion and grade III of the posterior portion in 6 cases, grade III and grade IV in 1 case, and grade III and III in 4 cases (Table 5).
Fig. 3.
Grade IV osteophyte at the anterior and posterior margin in lateral X-ray.
Table 5.
Simultaneous formation of osteophytes of grade III or higher on the anterior and posterior portions
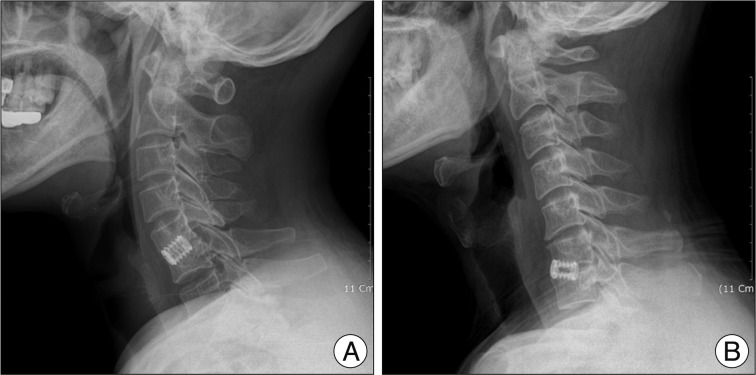
Kyphotic changes (Fig. 4)
Fig. 4.
Kyphosis related cage direction change. The cage migrated upward causing cervical kyphosis (A). Cervical kyphosis caused by downward cage migration (B).
The mean angle of kyphosis was 3.27°±8.51. Most common case did not show significant kyphotic changes except cases with cage directional changes. Among them, changes in cage direction causing cervical kyphosis were found in 35 levels. In these groups, the mean degree of kyphosis was 9.87±4.37° with a range of 2.75° to 17°. There was upward migration in 21 levels and downward migration in 14 levels.
Cage related complications
There were no significant complications associated with cylindrical cage placement, such as cage migration to the spinal cord or anterior displacement during follow-up radiographs.
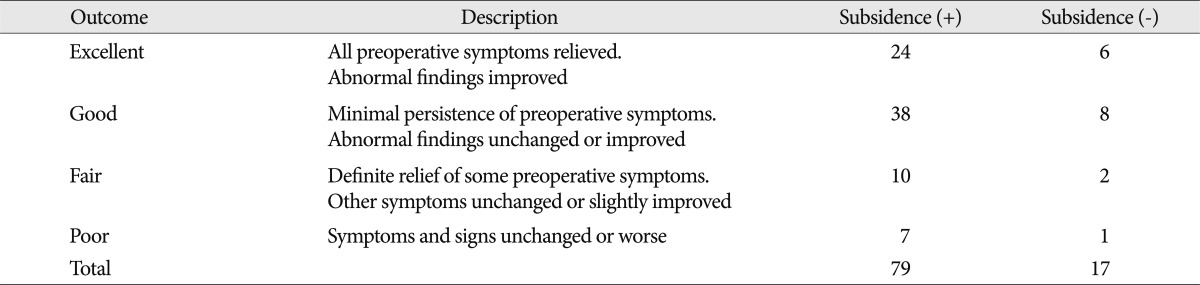
Clinical outcomes
Final outcomes were evaluated by Odom's criteria35). Clinical outcomes of 'more than good' were noted for 62 patients (78%) for whom subsidence had occurred and 14 (82%) for whom subsidence had not occurred (Table 6). Statistical analyses of the enrolled patients showed that anterior osteophyte formation was not influenced by clinical VAS score : however, there was a solid correlation between posterior osteophyte formation and poor VAS score after 12 months.
Table 6.
Comparisons of clinical outcomes between the subsidence group and non-subsidence group* according to Odom's criteria
*Two patients with subsidence on one of the two levels were included in the subsidence group
Statistical result among the various factors
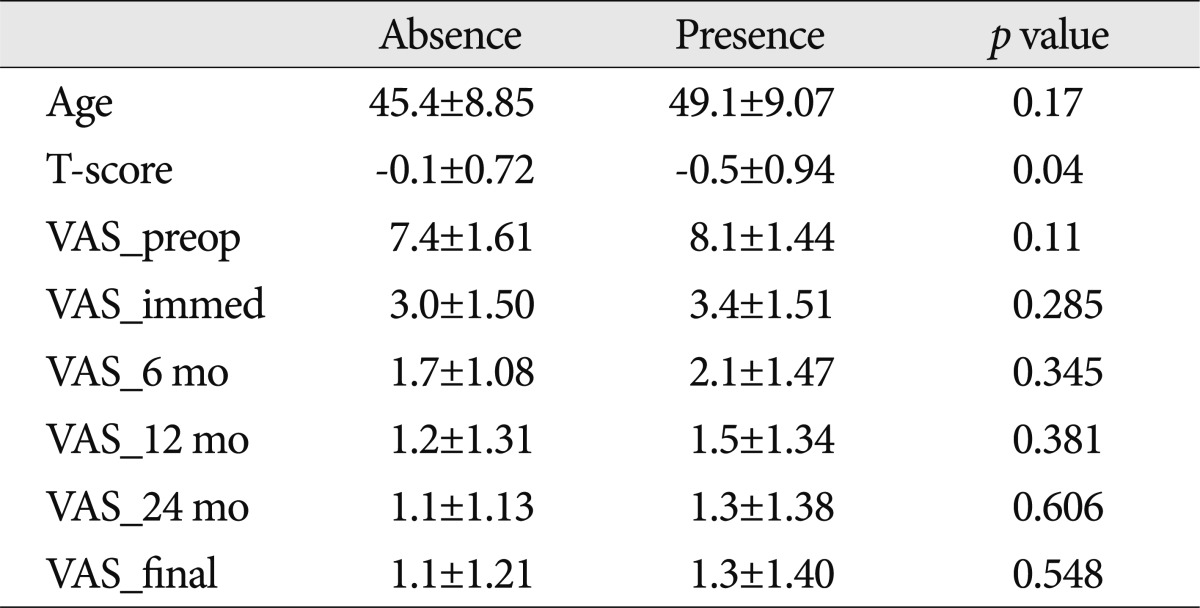
Although T-scores were statistically significant with respect to subsidence (p=0.039), they were not correlated with osteophyte formation (p=0.089 in the anterior portion and 0.051 in the posterior portion) according to analysis by level (Table 7). Likewise, T-scores were not correlated with subsidence and osteophyte formation in one level surgeries (Table 8). Significant relationships between posterior osteophyte formation and VAS score were observed in patients with one level surgery (p<0.05), but not in two level treated patients (p>0.05) (Table 8, 9). When subsidence related factors were evaluated, only T-scores were associated with subsidence (p=0.04), while VAS scores were not (p>0.05) (Table 10). In addition, there were no relationships between subsidence and other factors such as sex and surgery level (p>0.05) (Table 11).
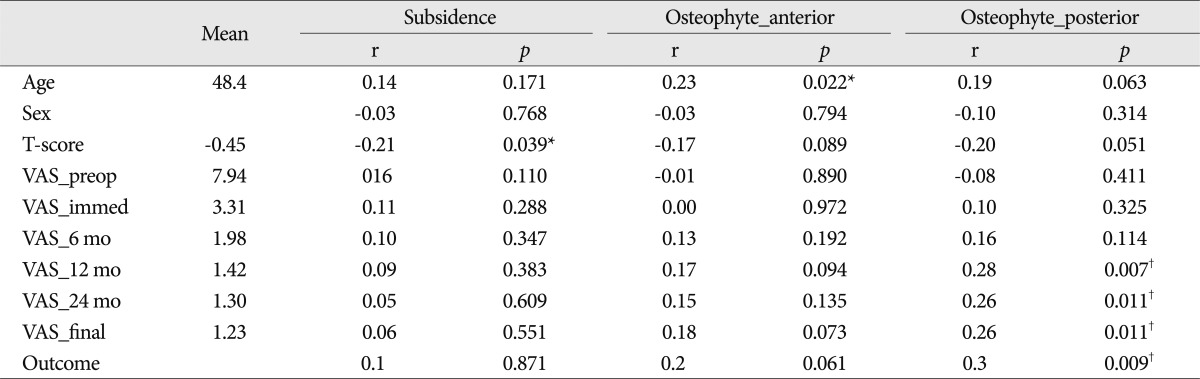
Table 7.
Statistical analysis by Spearman's coefficient correlation and phi correlation in all enrolled patients*
*VAS : visual analogue scale. †Statistical significance (p<0.05)
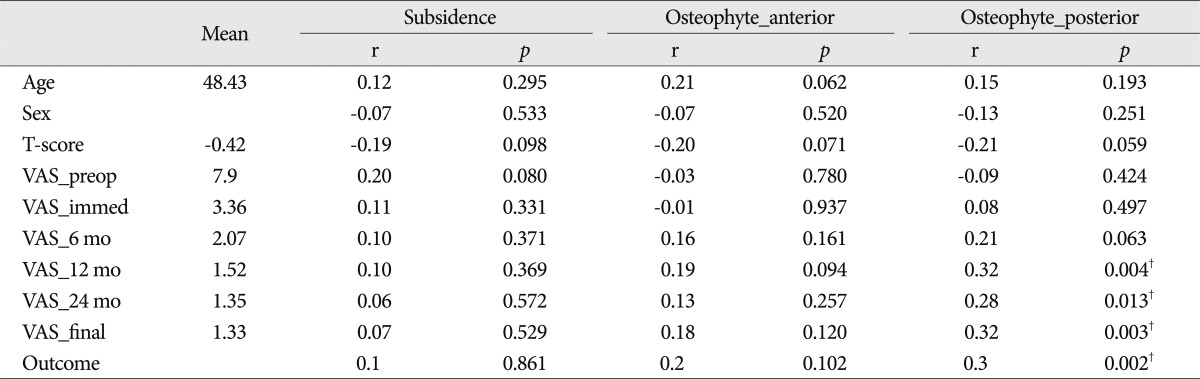
Table 8.
Statistical analysis by Spearman's coefficient correlation and phi correlation in patients with one level surgery*
*VAS : visual analogue scale. †Statistical significance (p<0.05)
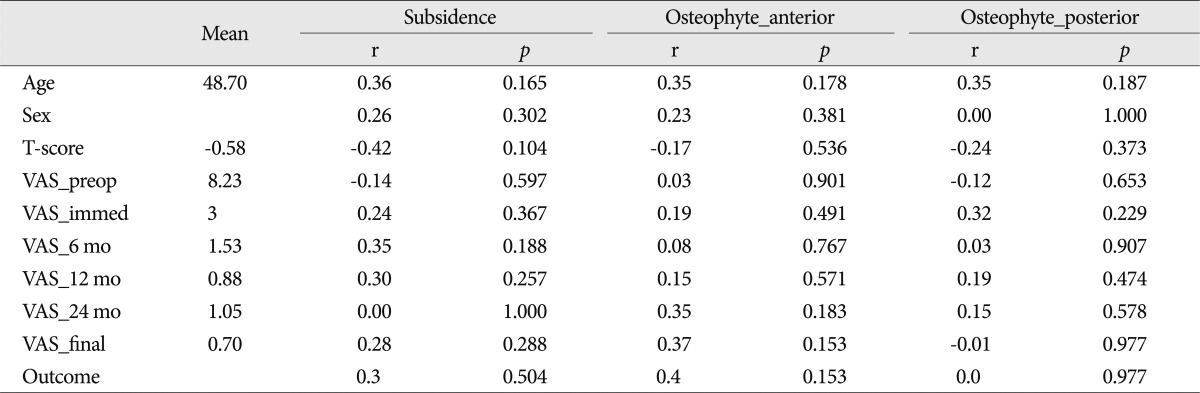
Table 9.
Statistical analysis by Spearman's coefficient correlation and phi correlation in patients with two level surgery*
*VAS : visual analogue scale
Table 10.
Statistical analysis of subsidence related factors*
*Statistical analysis by Mann-Whitney U test, visual analogue scale (VAS)
Table 11.
Statistical analysis of subsidence related sex and level*
*Statistical analysis by chi-square test, visual analogue scale (VAS)
DISCUSSION
Traditional ACDF using autografts without plates, as recommended by Robinson and Smith38) has several limitations such as graft collapse, graft expulsion, pseudoarthrosis, and donor site morbidities that include bleeding, infection, persistent pain, fractures of the iliac bone, and poor esthetic results2,7,17,30-32,39). Although plate systems and allografts reduce such problems, this method is still associated with complications including screw pull-out, breakage of the plate system, and lower bone fusion rate in allograft materials6,27,32,41). Furthermore, the quality of autologous iliac bone is not always good in elderly patients40). Use of interbody cage addresses these problems associated with autologous iliac bone grafts, because there is no need to harvest autografts or to utilize allografts.
The cylindrical metal cage has many benefits including short incision, short operating time, low complication rate associated with bone graft, easy maneuverability of instrument and high rate of bone fusion23). However, the use of cylindrical cage is relatively decreasing, because it has some complications, which failed to preserve disc height, prevent kyphosis, and preserve a natural intervertebral alignment26). Therefore, in the present study, authors investigated the some complication rate and clinical correlation among them.
According to previous studies, the subsidence rates of cylindrical cervical cages are between 4% and 22%19,21,39). Tureyen demonstrated that the mean narrowing rate was 35.6±9% in 43 patients, and asserted that subsidence is inevitable42). In contrast, Hida et al.20) found that subsidence was observed in only 14 of 146 patients over a long follow-up period, probably due to the preservation of intervertebral cortical bone, anterior cage location, and usage of properly sized cages when using cylindrical, threaded cage. However, in the present study we observed a higher rate of subsidence (93 of 112 levels) compared to previous reports. Although this rate reflects the definition of subsidence used in our study, which is relatively large (3 mm) when considering cervical disc height, the 82% subsidence rate reported in this study is nevertheless much higher than those of previous reports. Interestingly, according to a preliminary report, the subsidence rate is 2% at 6 months and 22% at 12 months23). Although several cases were lost during long-term follow-up, the subsidence had progressed in approximately 60% cases after 2 years. Despite identifying bone unions between 6 and 12 months, in our opinion, this observation may reflect bony growth around the cage into the empty disc space through the cage pores. A previous study demonstrated that cylindrical cages have disadvantages with respect to subsidence rate, but are superior with respect to fusion rate4,26,42,43). To prevent subsidence, interbody cages should meet several qualifications including large contact surfaces and preservation of endplates. Because cylindrical cages should be drilled into the disc space, partial destruction of the endplate is inevitable, which improves bony ingrowth20,43). Bone mineral density (BMD) is another factor influencing subsidence43). Moreover, subsidence risk with respect to BMD is higher for cylindrical cages than for other types of cages43). In the present study, subsidence was strongly correlated with T-scores when evaluated in all enrolled whole patients, but not in individual one level and two level patients. This may be due to the small sample used for the present study.
Osteophyte formation is a degenerative process in the spine. Benneker et al.5) showed that several radiological findings, including disc height loss, osteophyte formation, and intradiscal calcification, are correlated with morphological grades in degenerative lumbar spine disease. Further, several studies have demonstrated that the process of osteophyte formation begins with the degeneration of intervertebral discs10,15,33). As intervertebral disc degeneration progresses, processes such as such as dehydration of the nucleus pulposus and disintegration of annulus fibrosus lead to compressive stiffness and disc fiber strains11,25,29). Additionally, external pressure and stress induces a remodeling process that causes osteophyte formation10,15,28,33). Osteophyte formation following ACDF at the fusion level has not been frequently reported, but may occur at the adjacent level via degenerative changes caused by fusion surgery29,37). In our opinion osteophyte formation may follow ACDF using a cage because the remodeling process may be promoted by removal of preoperative osteophytes in order to approach the disc space, although formation of osteophyte is not always correlated with removal of anterior spur. As conventional ACDF is performed using anterior plates, there is no space for formation of osteophytes though ACDF using a cage, as cages limit anterior bony growth. In addition, because micro-motion may remain after neck motion, there are more external pressure and stress on the bony structures after fusion surgery using a cage than after ACDF using a plate system. So, better stability of plate system may restrict the formation of osteophyte. Finally, the identified osteophytes may be not true osteophytes, but rather external overgrowths of bone during the progression of subsidence and bone union. Thus, if osteophytes are defined only as anterior projections of bony formations from the anterior border, the rates of osteophyte formation may be underestimated in our data.
The lordotic curvature of the normal cervical spine may vary from 20° to 35° for C2 to C7, according to the measurement method used8,16,19,22,34). A previous report by Grob et al.18) found that abnormal sagittal curvature of the cervical spine is related to neck pain. Kyphotic misalignment following ACDF has also been accepted as a factor promoting degenerative processes in adjacent levels24). Therefore, kyphotic curvature must not be increased during bony fusion. According to our data, however, the mean kyphotic change in 35 cases was about 9°. When considering that most of the kyphosis was detected in patients with subsidence, the kyphotic changes might have been due to directional changes (either upward or downward) that developed during cage settlement and subsidence. In other words, because the cylindrical cages were located in the disc space following partial destruction of the endplate, the cages may have migrated during the process of bone fusion.
There were no cases of severe neurologic symptoms associated with radiological abnormalities including subsidence, osteophyte formation at the anterior portion, or kyphotic curvature. The patients with radiological abnormalities did not have severely aggravated VAS scores, and their neurologic symptoms including myelopathy, radiculopathy, and dysphasia were similar to those obtained after the postoperative period in the above cases. However, VAS scores and final clinical outcomes were decreased by posterior osteophyte formation. Therefore, neurosurgeons should keep in mind the possibility of spinal cord compression by posterior osteophyte formation. In addition, it is important to note that there were no cases neurological deterioration associated with two level surgery, regardless of osteophyte location. This result may have been due to the smaller number of patients who underwent two level surgery than one level surgery. Alternatively, two level cervical fusion with cylindrical devices was associated with less formation of posterior osteophytes, possibly due to the relatively restricted cervical motion that resulted compared with one level fusion.
There are several limitations in the present study. First, because we address only the long-term follow-up of cylindrical cage treatment, acute stage complications such as infections, reoperation due to cage migration or malposition were not examined in this study. Second, it is possible that we overestimated osteophyte formation.
CONCLUSION
The present study describes the long term (at least 36 months) follow-up results of cylindrical cage treatment according to radiologic characteristics including subsidence, osteophyte formation, and kyphosis in a large study sample. Cage subsidence and osteophyte formation were present in almost all of the cases in our sample, which is inconsistent with the findings of previous reports. Surgeons should explain the possibility that neurologic outcomes may be aggravated by posterior osteophyte formation in late stages to patients during preoperative preparation. Cylindrical cages are relatively safe when used in patients with normal BMD, with a possibility of subsidence and kyphosis during bone fusion in patients with low T-scores, although there are low risks of severe neurologic aggravation.
Acknowledgements
This work was supported by the research fund of Hanyang University (HY-2010-C). Institutional Review Board approval was provided by Hanyang University Medical Center (HYUH-IRB-2011-R-35).
References
- 1.al-Hami S. Cervical monosegmental interbody fusion using titanium implants in degenerative, intervertebral disc disease. Minim Invasive Neurosurg. 1999;42:10–17. doi: 10.1055/s-2008-1053361. [DOI] [PubMed] [Google Scholar]
- 2.Arrington ED, Smith WJ, Chambers HG, Bucknell AL, Davino NA. Complications of iliac crest bone graft harvesting. Clin Orthop Relat Res. 1996:300–309. doi: 10.1097/00003086-199608000-00037. [DOI] [PubMed] [Google Scholar]
- 3.Auguste KI, Chin C, Acosta FL, Ames CP. Expandable cylindrical cages in the cervical spine : a review of 22 cases. J Neurosurg Spine. 2006;4:285–291. doi: 10.3171/spi.2006.4.4.285. [DOI] [PubMed] [Google Scholar]
- 4.Bartels RH, Donk RD, Feuth T. Subsidence of stand-alone cervical carbon fiber cages. Neurosurgery. 2006;58:502–508. doi: 10.1227/01.NEU.0000197258.30821.50. discussion 502-508. [DOI] [PubMed] [Google Scholar]
- 5.Benneker LM, Heini PF, Anderson SE, Alini M, Ito K. Correlation of radiographic and MRI parameters to morphological and biochemical assessment of intervertebral disc degeneration. Eur Spine J. 2005;14:27–35. doi: 10.1007/s00586-004-0759-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bishop RC, Moore KA, Hadley MN. Anterior cervical interbody fusion using autogeneic and allogeneic bone graft substrate : a prospective comparative analysis. J Neurosurg. 1996;85:206–210. doi: 10.3171/jns.1996.85.2.0206. [DOI] [PubMed] [Google Scholar]
- 7.Bohlman HH, Eismont FJ. Surgical techniques of anterior decompression and fusion for spinal cord injuries. Clin Orthop Relat Res. 1981:57–67. [PubMed] [Google Scholar]
- 8.Bovim G, Schrader H, Sand T. Neck pain in the general population. Spine (Phila Pa 1976) 1994;19:1307–1309. doi: 10.1097/00007632-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Brodke DS, Zdeblick TA. Modified Smith-Robinson procedure for anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 1992;17:S427–S430. doi: 10.1097/00007632-199210001-00014. [DOI] [PubMed] [Google Scholar]
- 10.Brown TD, Pedersen DR, Gray ML, Brand RA, Rubin CT. Toward an identification of mechanical parameters initiating periosteal remodeling : a combined experimental and analytic approach. J Biomech. 1990;23:893–905. doi: 10.1016/0021-9290(90)90354-6. [DOI] [PubMed] [Google Scholar]
- 11.Buckwalter JA. Aging and degeneration of the human intervertebral disc. Spine (Phila Pa 1976) 1995;20:1307–1314. doi: 10.1097/00007632-199506000-00022. [DOI] [PubMed] [Google Scholar]
- 12.Emery SE, Bolesta MJ, Banks MA, Jones PK. Robinson anterior cervical fusion comparison of the standard and modified techniques. Spine (Phila Pa 1976) 1994;19:660–663. [PubMed] [Google Scholar]
- 13.Fernyhough JC, White JI, LaRocca H. Fusion rates in multilevel cervical spondylosis comparing allograft fibula with autograft fibula in 126 patients. Spine (Phila Pa 1976) 1991;16:S561–S564. doi: 10.1097/00007632-199110001-00022. [DOI] [PubMed] [Google Scholar]
- 14.Fountas KN, Kapsalaki EZ, Smith BE, Nikolakakos LG, Richardson CH, Smisson HF, et al. Interobservational variation in determining fusion rates in anterior cervical discectomy and fusion procedures. Eur Spine J. 2007;16:39–45. doi: 10.1007/s00586-006-0116-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goel VK, Ramirez SA, Kong W, Gilbertson LG. Cancellous bone Young's modulus variation within the vertebral body of a ligamentous lumbar spine--application of bone adaptive remodeling concepts. J Biomech Eng. 1995;117:266–271. doi: 10.1115/1.2794180. [DOI] [PubMed] [Google Scholar]
- 16.Gore DR, Sepic SB, Gardner GM. Roentgenographic findings of the cervical spine in asymptomatic people. Spine (Phila Pa 1976) 1986;11:521–524. doi: 10.1097/00007632-198607000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Graham JJ. Complications of cervical spine surgery. A five-year report on a survey of the membership of the Cervical Spine Research Society by the Morbidity and Mortality Committee. Spine (Phila Pa 1976) 1989;14:1046–1050. [PubMed] [Google Scholar]
- 18.Grob D, Frauenfelder H, Mannion AF. The association between cervical spine curvature and neck pain. Eur Spine J. 2007;16:669–678. doi: 10.1007/s00586-006-0254-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hald HJ, Danz B, Schwab R, Burmeister K, Bähren W. [Radiographically demonstrable spinal changes in asymptomatic young men] Rofo. 1995;163:4–8. doi: 10.1055/s-2007-1015936. [DOI] [PubMed] [Google Scholar]
- 20.Hida K, Iwasaki Y, Yano S, Akino M, Seki T. Long-term follow-up results in patients with cervical disk disease treated by cervical anterior fusion using titanium cage implants. Neurol Med Chir (Tokyo) 2008;48:440–446. doi: 10.2176/nmc.48.440. discussion 446. [DOI] [PubMed] [Google Scholar]
- 21.Hwang SL, Hwang YF, Lieu AS, Lin CL, Kuo TH, Su YF, et al. Outcome analyses of interbody titanium cage fusion used in the anterior discectomy for cervical degenerative disc disease. J Spinal Disord Tech. 2005;18:326–331. doi: 10.1097/01.bsd.0000164198.30725.2d. [DOI] [PubMed] [Google Scholar]
- 22.Juhl JH, Miller SM, Roberts GW. Roentgenographic variations in the normal cervical spine. Radiology. 1962;78:591–597. [Google Scholar]
- 23.Joung YI, Oh SH, Ko Y, Yi HJ, Lee SK. Subsidence of cylindrical cage (AMSLUtrade mark Cage) : postoperative 1 year follow-up of the cervical anterior interbody fusion. J Korean Neurosurg Soc. 2007;42:367–370. doi: 10.3340/jkns.2007.42.5.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Katsuura A, Hukuda S, Saruhashi Y, Mori K. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J. 2001;10:320–324. doi: 10.1007/s005860000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim YE, Goel VK, Weinstein JN, Lim TH. Effect of disc degeneration at one level on the adjacent level in axial mode. Spine (Phila Pa 1976) 1991;16:331–335. doi: 10.1097/00007632-199103000-00013. [DOI] [PubMed] [Google Scholar]
- 26.Kolstad F, Nygaard ØP, Andresen H, Leivseth G. Anterior cervical arthrodesis using a "stand alone" cylindrical titanium cage : prospective analysis of radiographic parameters. Spine (Phila Pa 1976) 2010;35:1545–1550. doi: 10.1097/BRS.0b013e3181d259c1. [DOI] [PubMed] [Google Scholar]
- 27.Kumaresan S, Yoganandan N, Pintar FA. Finite element analysis of anterior cervical spine interbody fusion. Biomed Mater Eng. 1997;7:221–230. [PubMed] [Google Scholar]
- 28.Kumaresan S, Yoganandan N, Pintar FA, Maiman DJ, Goel VK. Contribution of disc degeneration to osteophyte formation in the cervical spine : a biomechanical investigation. J Orthop Res. 2001;19:977–984. doi: 10.1016/S0736-0266(01)00010-9. [DOI] [PubMed] [Google Scholar]
- 29.Lopez-Espina CG, Amirouche F, Havalad V. Multilevel cervical fusion and its effect on disc degeneration and osteophyte formation. Spine (Phila Pa 1976) 2006;31:972–978. doi: 10.1097/01.brs.0000215205.66437.c3. [DOI] [PubMed] [Google Scholar]
- 30.López-Oliva Muñoz F, García de las Heras B, Concejero López V, Asenjo Siguero JJ. Comparison of three techniques of anterior fusion in single-level cervical disc herniation. Eur Spine J. 1998;7:512–516. doi: 10.1007/s005860050117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Majd ME, Vadhva M, Holt RT. Anterior cervical reconstruction using titanium cages with anterior plating. Spine (Phila Pa 1976) 1999;24:1604–1610. doi: 10.1097/00007632-199908010-00016. [DOI] [PubMed] [Google Scholar]
- 32.Matge G. Anterior interbody fusion with the BAK-cage in cervical spondylosis. Acta Neurochir (Wien) 1998;140:1–8. doi: 10.1007/s007010050049. [DOI] [PubMed] [Google Scholar]
- 33.Nathan H. Osteophytes of the vertebral column. Ananatomical study of their development according to age, race and sex with considerations as to their etiology and significance. J Bone Joint Surg. 1962;44:243–268. [Google Scholar]
- 34.Nojiri K, Matsumoto M, Chiba K, Maruiwa H, Nakamura M, Nishizawa T, et al. Relationship between alignment of upper and lower cervical spine in asymptomatic individuals. J Neurosurg. 2003;99:80–83. doi: 10.3171/spi.2003.99.1.0080. [DOI] [PubMed] [Google Scholar]
- 35.Odom GL, Finney W, Woodhall B. Cervical disk lesions. J Am Med Assoc. 1958;166:23–28. doi: 10.1001/jama.1958.02990010025006. [DOI] [PubMed] [Google Scholar]
- 36.Orr RD, Zdeblick TA. Cervical spondylotic myelopathy. Approaches to surgical treatment. Clin Orthop Relat Res. 1999:58–66. [PubMed] [Google Scholar]
- 37.Robertson JT, Papadopoulos SM, Traynelis VC. Assessment of adjacent-segment disease in patients treated with cervical fusion or arthroplasty : a prospective 2-year study. J Neurosurg Spine. 2005;3:417–423. doi: 10.3171/spi.2005.3.6.0417. [DOI] [PubMed] [Google Scholar]
- 38.Robinson RA, Smith GW. Anterior cervical disc removal and interbody fusion for cervical disc syndrome. Bull Johns Hopkins Hosp. 1955;96:223–224. [Google Scholar]
- 39.Sawin PD, Traynelis VC, Menezes AH. A comparative analysis of fusion rates and donor-site morbidity for autogeneic rib and iliac crest bone grafts in posterior cervical fusions. J Neurosurg. 1998;88:255–265. doi: 10.3171/jns.1998.88.2.0255. [DOI] [PubMed] [Google Scholar]
- 40.Senter HJ, Kortyna R, Kemp WR. Anterior cervical discectomy with hydroxylapatite fusion. Neurosurgery. 1989;25:39–42. doi: 10.1097/00006123-198907000-00007. discussion 42-43. [DOI] [PubMed] [Google Scholar]
- 41.Thomé C, Krauss JK, Zevgaridis D. A prospective clinical comparison of rectangular titanium cages and iliac crest autografts in anterior cervical discectomy and fusion. Neurosurg Rev. 2004;27:34–41. doi: 10.1007/s10143-003-0297-2. [DOI] [PubMed] [Google Scholar]
- 42.Türeyen K. Disc height loss after anterior cervical microdiscectomy with titanium intervertebral cage fusion. Acta Neurochir (Wien) 2003;145:565–569. doi: 10.1007/s00701-003-0050-1. discussion 569-570. [DOI] [PubMed] [Google Scholar]
- 43.Wilke HJ, Kettler A, Goetz C, Claes L. Subsidence resulting from simulated postoperative neck movements : an in vitro investigation with a new cervical fusion cage. Spine (Phila Pa 1976) 2000;25:2762–2770. doi: 10.1097/00007632-200011010-00008. [DOI] [PubMed] [Google Scholar]