Abstract
Purpose
Accurate diagnosis and optimal management of acute appendicitis, despite being the most common surgical emergency encountered in emergency departments, is often delayed in pediatric patients due to nonspecific symptoms and communication barriers, often leading to more complicated cases. The aim of this study is to investigate the diagnostic significance of common laboratory markers.
Methods
A total of 421 patients aged 15 and younger underwent surgical treatment for acute appendicitis. We conducted a retrospective analysis for white blood cell (WBC), C-reactive protein (CRP) and bilirubin. All patients were classified into simple or complicated appendicitis groups based on postoperative histology.
Results
The mean age of the patients in the complicated appendicitis group was younger than that in the simple group (P = 0.005). WBC, CRP and bilirubin levels were significantly higher in the complicated appendicitis group (P < 0.001, <0.001, 0.002). The relative risk for complicated appendicitis was calculated using age, WBC, CRP and bilirubin. Elevated CRP levels were associated with the highest risk for complicated appendicitis (hazard ratio [HR], 2.53; 95% confidence interval [CI], 1.38 to 4.65) followed by WBC (HR, 2.42; 95% CI, 1.07 to 5.46) and bilirubin (HR, 2.04; 95% CI, 1.09 to 3.82). The most sensitive markers for diagnosing complicated appendicitis were WBC (95.2%) and CRP (86.3%). Bilirubin levels showed the highest specificity at 74.8%.
Conclusion
The risk of complicated appendicitis was significantly higher in patients younger than 10 years old. Preoperative WBC, CRP and bilirubin have clinical value in diagnosing complicated appendicitis with a HR of 2.0 to 2.5. Our results suggest that the utilization of WBC, CRP, and bilirubin can assist in the diagnosis of complicated appendicitis in pediatric patients, allowing prompt diagnosis and optimal management.
Keywords: Appendicitis, Child, Leukocytes, C-reactive protein, Bilirubin
INTRODUCTION
Appendicitis remains the most common acute surgical condition of the abdomen and is also the most commonly misdiagnosed [1]. About one third of patients with appendicitis are younger than 18 years of age. Younger children typically present with complicated appendicitis due to their inability to provide accurate histories and typically low indexes of suspicion that lead to misdiagnosis [2].
Complicated appendicitis is closely related to wound infection, intraabdominal abscess formation, postoperative intestinal obstruction, prolonged ileus and rarely, enterocutaneous fistula. In females, it has been associated with fallopian tube dysfunction, leading to infertility [3]. Because of high morbidity of complicated appendicitis, careful diagnosis and prompt treatment is imperative.
The accuracy of diagnosing acute appendicitis has greatly improved with the introduction of computed tomography [4]. However, physicians should be cautious in the use of computed tomography (CT) for pediatric patients due to reports of long term adverse effects [5,6].
We conducted this study to investigate the diagnostic significance of common laboratory markers in children with complicated appendicitis.
METHODS
A total of 421 patients aged 15 or younger underwent surgical treatment for acute appendicitis from September 2003 to October 2011 at Wonju Christian Hospital. A retrospective analysis was completed by reviewing medical records.
Patient sex, age at surgery, and preoperative laboratory markers (white blood cell [WBC], C-reactive protein [CRP], bilirubin, aspartate aminotransferase [AST], and alanine aminotransferase [ALT]) were recorded. Hyperbilirubinemia was defined as total bilirubin >1.0 mg/dL. Normal values were defined as follows: WBC 4.4 to 10.0 × 103/µL, CRP < 0.5 mg/dL and AST, ALT <40 U/L.
All patients were classified into either simple or complicated appendicitis groups based on postoperative histology. Complicated appendicitis was defined as a gangrenous and/or perforated appendicitis. Many terms have been used to describe the varying stages of appendicitis, including acute appendicitis, suppurative appendicitis, gangrenous appendicitis, and perforated appendicitis. These distinctions are vague, and only the clinically relevant distinction of simple and complicated appendicitis should be used. We use the term 'complicated' appendicitis to describe both gangrenous and perforated appendicitis [7].
Statistical analysis
We conducted all analyses using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA). The mean values, SDs, ranges, and P-values were calculated for sex, age at operation, WBC, CRP, bilirubin levels, AST and ALT with Pearson's chi-square test. Sensitivity, specificity, positive predictive value and negative predictive value were calculated for WBC, CRP, bilirubin and age at operation. Hazard ratios (HRs) were calculated for WBC, CRP, bilirubin and age at operation through binary logistic regression after multivariate data analysis. A P-value ≤ 0.05 was used to indicate statistical significance.
RESULTS
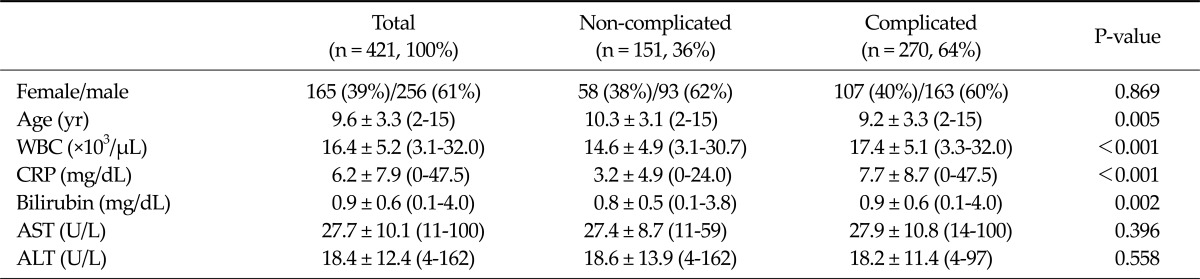
Of the 421 patients included in our study, there were 256 males (61%) and 165 females (39%). Of these, 270 patients (64%) were diagnosed with complicated appendicitis. There were no significant differences between sexes (P = 0.869).
The mean ages at operation were 10.3 years (SD, ±3.1; 2 to 15 years) and 9.2 years (SD, ±3.3; 2 to 15 years) for the simple and complicated groups, respectively. The ages of the patients in the complicated appendicitis group were significantly lower than in the simple group (P = 0.005).
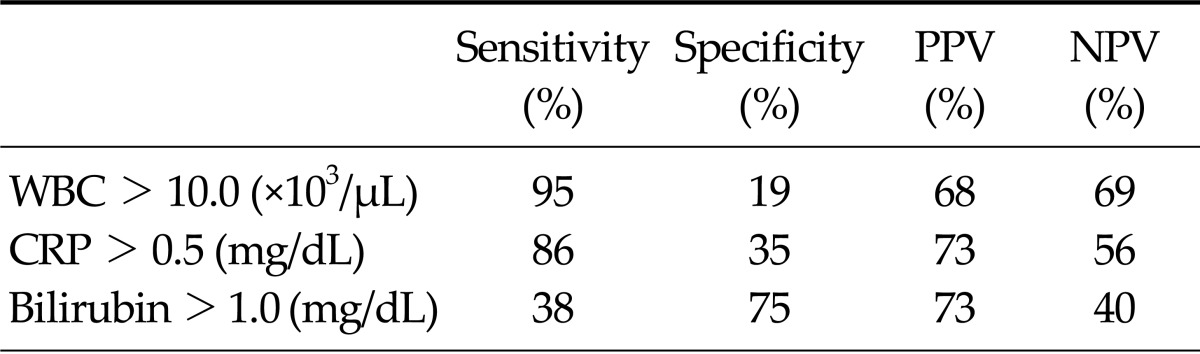
Mean bilirubin levels were 0.9 mg/dL (SD, ±0.6; 0.1 to 4.0 mg/dL). Bilirubin levels were 0.8 mg/dL (SD, ±0.5; 0.1 to 3.8 mg/dL) and 0.9 mg/dL (SD, ±0.6; 0.1 to 4.0 mg/dL), in the simple and complicated groups, respectively, with the complicated group exhibiting significantly higher levels (P = 0.002). Bilirubin showed the highest specificity in diagnosing complicated cases at 75% compared to WBC (19%) and CRP (35%).
Mean WBC was 16.4 × 103/µL (SD, ±5.2; 3.1 to 32.0 × 103/µL) for all patients. Mean WBCs in the simple and complicated groups were 14.6 × 103/µL (SD, ±4.9; 3.1 to 30.7 × 103/µL) and 17.4 × 103/µL (SD, ±5.1; 3.3 to 32.0 × 103/µL), respectively, with significantly higher levels in the complicated group (P < 0.001).
CRP levels were assessed preoperatively in 307 patients. The mean CRP was 6.2 mg/dL (SD, ±7.9; 0 to 47.5 mg/dL). For the simple and complicated groups, the mean CRPs were 3.2 mg/dL (SD, ±4.9; 0 to 24.0 mg/dL) and 7.7 mg/dL (SD, ±8.7; 0 to 47.5 mg/dL), respectively. CRP levels were significantly higher in the complicated group (P < 0.001). The sensitivity for CRP in the diagnosis of complicated appendicitis was 86%, while the specificity was 35% (Tables 1, 2).
Table 1.
Details of laboratory values, epidemiology of the two groups
Values are presented as mean ± standard deviation (range).
WBC, white blood cell; CRP, C-reactive protein; AST, aspartate aminotransferase; ALT, alanine aminotransferase.
Table 2.
Sensitivity, specificity, PPV, NPV for WBC, CRP, bilirubin
PPV, positive predictive value; NPV, negative predictive value; WBC, white blood cell; CRP, C-reactive protein.
No significant differences in AST or ALT levels were seen between the two groups (P = 0.653, 0.742).
No correlations between elevated bilirubin levels and AST or ALT levels was seen (P = 0.064, 0.111 by Pearson's correlation coefficient).
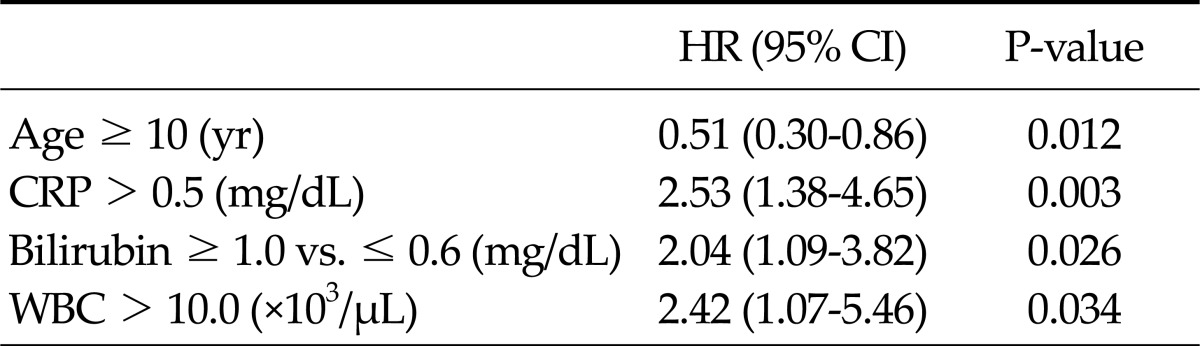
Binary multiple logistic regression analyses were conducted for age, WBC, CRP and bilirubin levels to assess the HR of these parameters. The risk of complicated appendicitis is decreased to almost half for children ten years and older (HR, 0.51; 95% CI, 0.30 to 0.86).
Patients with CRP levels higher than 0.5 mg/dL had a 2.53 times greater risk of complicated appendicitis than patients with CRP levels less than 0.5 mg/dL (HR, 2.53; 95% CI, 1.38 to 4.65). Patients with bilirubin levels greater than 1.0 mg/dL had a HR of 2.04 compared with those with bilirubin levels less than 0.6 mg/dL (HR, 2.04; 95% CI, 1.09 to 3.82). Patients with WBC greater than 10.0 × 103/µL had a HR of 2.42 compared with patients with WBC under 10.0 × 103/µL (HR, 2.42; 95% CI, 1.07 to 5.46) (Table 3).
Table 3.
Hazard ratio (HR) of age, CRP, bilirubin, WBC
CRP, C-reactive protein; WBC, white blood cell; CI, confidence interval.
DISCUSSION
Despite being the most common surgical emergency, acute appendicitis is often misdiagnosed, with negative appendectomy rates reported between 10 to 30% [1].
Morbidity following complicated appendicitis includes bacterial peritonitis, urinary disorders, small bowel obstruction and intra-abdominal abscesses, all of which are associated with poor postoperative outcomes. A careful history taking and thorough physical examination by a physician are essential in diagnosing appendicitis. Our results confirmed that the risk of complicated appendicitis was nearly two times greater in patients younger than 10 years old compared to patients 10 years and older. Evidently, there is a need for more objective and accurate measures for diagnosing appendicitis in children.
Even with recent advances in imaging, no single test can accurately diagnose perforation or gangrenous changes of the appendix. Common studies such as CT should also be used with caution in children because of the potential risks of radiation [5,6]. There have been several studies of the diagnostic value of separate laboratory markers such as WBC [8], CRP [9] and bilirubin [10], but without definite results. Our study is the first to evaluate different markers together in a single study.
Our results show that WBC and CRP are highly sensitive markers in the diagnosis of complicated appendicitis in children and bilirubin is a marker with high specificity. Patients with elevated WBC, CRP and bilirubin levels were found to have a 2.0 to 2.5 times increased risk of complicated appendicitis.
While WBC and CRP elevation are more common indicators of inflammation, there has been new attention paid to bilirubin, which is often overlooked in the diagnosis of acute appendicitis [10]. Many studies have been conducted on hyperbilirubinemia resulting from cholestasis commonly found in septic conditions [11,12]. Proinflammatory cytokines and nitric oxide inhibit hepatocellular bile formation. The impaired flow in the small and large bile ducts also contributes to cholestasis.
As stated in our introduction, younger children typically present with complicated appendicitis due to their inability to provide accurate histories and typically low indexes of suspicion that lead to misdiagnosis. This is consistent with our study findings. Children younger than 10 years old had two times higher risk for developing complicated appendicitis (Table 3). Objective markers and an adequate analysis of these markers is needed to create a normogram that will assist in the accurate diagnosis and treatment of this high risk group. There have been previous attempts at creating a diagnostic appendicitis scoring system based on certain clinical symptoms, signs and laboratory markers; however, there are few scoring systems that are currently applicable in children [13-15]. The majority of these scoring systems emphasize clinical variables (e.g., anorexia, nausea, pain migration) with laboratory markers given little or no weight [16]. In the younger pediatric population, there are limitations to analyzing clinical variables, lowering the validity of these scoring systems.
In conclusion, the results of our study confirmed that WBC, CRP and bilirubin levels have diagnostic significance in complicated appendicitis. Elevated WBC and CRP had the highest sensitivity and risk for complicated appendicitis, leading to a 2.5 times greater chance for complicated appendicitis. Bilirubin levels had the highest specificity for diagnosing complicated appendicitis, leading to a 2.0 times greater chance for complicated appendicitis in patients with elevated levels.
We expect further studies to validate the use of these markers in an appendicitis scoring system for children.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Pearl RH, Hale DA, Molloy M, Schutt DC, Jaques DP. Pediatric appendectomy. J Pediatr Surg. 1995;30:173–178. doi: 10.1016/0022-3468(95)90556-1. [DOI] [PubMed] [Google Scholar]
- 2.Jun GH, Jun BC, Lee HG, Bae JD, Kim NH, Ha DY, et al. Acute appendicitis in children under age of 5 years. J Korean Surg Soc. 2005;69:412–416. [Google Scholar]
- 3.Mueller BA, Daling JR, Moore DE, Weiss NS, Spadoni LR, Stadel BV, et al. Appendectomy and the risk of tubal infertility. N Engl J Med. 1986;315:1506–1508. doi: 10.1056/NEJM198612113152402. [DOI] [PubMed] [Google Scholar]
- 4.Pena BM, Taylor GA, Fishman SJ, Mandl KD. Effect of an imaging protocol on clinical outcomes among pediatric patients with appendicitis. Pediatrics. 2002;110:1088–1093. doi: 10.1542/peds.110.6.1088. [DOI] [PubMed] [Google Scholar]
- 5.Brenner DJ. Estimating cancer risks from pediatric CT: going from the qualitative to the quantitative. Pediatr Radiol. 2002;32:228–231. doi: 10.1007/s00247-002-0671-1. [DOI] [PubMed] [Google Scholar]
- 6.Doria AS, Moineddin R, Kellenberger CJ, Epelman M, Beyene J, Schuh S, et al. US or CT for diagnosis of appendicitis in children and adults? A meta-analysis. Radiology. 2006;241:83–94. doi: 10.1148/radiol.2411050913. [DOI] [PubMed] [Google Scholar]
- 7.Grosfeld JL, O'Neill JA, Fonkalsrud EW, Coran AG. Pediatric surgery. 6th ed. Philadelphia: Mosby/Elsevier; 2006. [Google Scholar]
- 8.Wang LT, Prentiss KA, Simon JZ, Doody DP, Ryan DP. The use of white blood cell count and left shift in the diagnosis of appendicitis in children. Pediatr Emerg Care. 2007;23:69–76. doi: 10.1097/PEC.0b013e31802d1716. [DOI] [PubMed] [Google Scholar]
- 9.Kaser SA, Fankhauser G, Willi N, Maurer CA. C-reactive protein is superior to bilirubin for anticipation of perforation in acute appendicitis. Scand J Gastroenterol. 2010;45:885–892. doi: 10.3109/00365521003728572. [DOI] [PubMed] [Google Scholar]
- 10.Sand M, Bechara FG, Holland-Letz T, Sand D, Mehnert G, Mann B. Diagnostic value of hyperbilirubinemia as a predictive factor for appendiceal perforation in acute appendicitis. Am J Surg. 2009;198:193–198. doi: 10.1016/j.amjsurg.2008.08.026. [DOI] [PubMed] [Google Scholar]
- 11.Chand N, Sanyal AJ. Sepsis-induced cholestasis. Hepatology. 2007;45:230–241. doi: 10.1002/hep.21480. [DOI] [PubMed] [Google Scholar]
- 12.Geier A, Fickert P, Trauner M. Mechanisms of disease: mechanisms and clinical implications of cholestasis in sepsis. Nat Clin Pract Gastroenterol Hepatol. 2006;3:574–585. doi: 10.1038/ncpgasthep0602. [DOI] [PubMed] [Google Scholar]
- 13.Samuel M. Pediatric appendicitis score. J Pediatr Surg. 2002;37:877–881. doi: 10.1053/jpsu.2002.32893. [DOI] [PubMed] [Google Scholar]
- 14.Bhatt M, Joseph L, Ducharme FM, Dougherty G, McGillivray D. Prospective validation of the pediatric appendicitis score in a Canadian pediatric emergency department. Acad Emerg Med. 2009;16:591–596. doi: 10.1111/j.1553-2712.2009.00445.x. [DOI] [PubMed] [Google Scholar]
- 15.Oh BY, Kim KH, Lee RA, Chung SS. Diagnostic efficacy of the alvarado score according to age in acute appendicitis. J Korean Surg Soc. 2010;78:100–105. [Google Scholar]
- 16.Lintula H, Pesonen E, Kokki H, Vanamo K, Eskelinen M. A diagnostic score for children with suspected appendicitis. Langenbecks Arch Surg. 2005;390:164–170. doi: 10.1007/s00423-005-0545-8. [DOI] [PubMed] [Google Scholar]