Abstract
Contrast-enhanced ultrasound is one of method for evaluating renal perfusion. The purpose of this project was to assess perfusion patterns and dynamics in normal micropig kidney using ultrasonographic contrast media. Eight young healthy micropigs were included in this study. Micropigs were anesthetized with propofol and received an intravenous bolus of microbubble contrast media through an ear vein. Time/mean pixel value (MPV) curves were generated for selected regions in the right renal cortex and medulla. The parenchyma was enhanced in two phases. The cortex was first enhanced followed by a more gradual enhancement of the medulla. A significant difference in perfusion was detected between the cortex and medulla. Following the bolus injection, the average upslope was 0.68 ± 0.27 MPV/sec, downslope was -0.27 ± 0.13 MPV/sec, baseline was 73.9 ± 16.5 MPV, peak was 84.6 ± 17.2 MPV, and time-to-peak (from injection) was 17.5 ± 6.6 sec for the cortex. For the medulla, the average upslope was 0.50 ± 0.24 MPV/sec, downslope was -0.12 ± 0.06 MPV/sec, baseline was 52.7 ± 7.0 MPV, peak was 65.2 ± 9.3 MPV, and time-to-peak (from injection) was 27.5 ± 5.0 sec. These data can be used as normal reference values for studying young micropigs.
Keywords: contrast ultrasound, kidney, micropig, perfusion
Introduction
Contrast-enhanced ultrasonography is an imaging modality that takes advantage of microbubble technology. For contrast-enhanced ultrasound, gas microbubbles are injected intravenously. The microbubble contrast agent, encapsulated by a shell of sulfur hexafluoride, can be detected in the circulation for several minutes. Tissue parenchymal microcirculation is visualized as echoes returning from contrast-enhanced blood [2,19]. Contrast-enhanced ultrasound can be potentially used to assess tissue perfusion using gas-filled microbubbles as a tracer. Because the microbubbles remain entirely within the intravascular space and have a rheology similar to that of red blood cells [6,7], we hypothesized that their renal tissue kinetics could be used to quantify the flow of renal arterial blood and nutrients.
Contrast-enhanced ultrasound has been used to evaluate renal conditions in humans. Renal parenchymal lesions in patients with acute pyelonephritis and renal transplant patients can be detected with this technique [8]. In a recent study performed in pigs, glomerular capillary hemorrhage was observed with contrast-enhanced ultrasonography [11]. Additionally, this method was used to depict global changes in renal blood flow in pigs [3]. It is possible to evaluate renal function using contrast-enhanced renal sonography with a moderate association between enhancement values and creatinine indices [9]. This technique also has been used to study the liver and pancreas in healthy dogs, cats, and human patients [12,13,17]. Administration of contrast ultrasound agent has been proven to be safe and noninvasive for dogs [18]. The purpose of the present study was to evaluate the normal perfusion pattern of kidney in healthy anesthetized micropigs using contrast-enhanced ultrasonography. The data obtained could serve as a reference when evaluating renal diseases that affect kidney perfusion.
Materials and Methods
Animal preparation
The studies were performed with eight healthy mixed-breed, PWG micropigs (3~4 months old, body weight, 11~13 kg), which were purchased from Medi Kinetics (Korea). All animals were raised under microbiologically controlled conditions. Pig pallet dry food and water were provided ad libitum. This research strictly followed regulations set forth in the Guide for the Care and Use of Laboratory Animals of Seoul National University, Korea.
Methods
All micropigs underwent a physical examination and a basic blood analysis (measuring serum creatinine, blood urea nitrogen, and electrolyte levels) was performed. The kidneys were then evaluated with B-mode ultrasonography. No evidence of focal or diffuse abnormalities was found. The micropigs were anesthetized with a mixture of tiletamine and zolazepam (Zoletil; Virbac, France) at a dosage of 8 mg/kg; anesthesia was maintained with propofol (Provive; Claris, India) delivered by intravenous injection at a constant rate of 0.5 mg/kg/min.
For contrast-enhanced harmonic imaging, a 5~12 MHz broadband linear probe and harmonic imaging system (Sonoace 9900; Medison, Korea) were used. The sagittal plane of the right kidney was imaged. The right kidney was selected for analysis because this kidney provided a better acoustic window in the micropigs. Before imaging, the hair was clipped and acoustic gel was applied for acoustic coupling. The transducer was carefully held by hand and maintained in the location of the kidney at approximately the same depth. Adjustable parameters such as depth, gain, and focal zones were optimized during preliminary studies and used for all imaging procedures. A real-time gray scale contrast enhanced ultrasound was performed by a single investigator with 2 years of experience in ultrasonography.
All micropigs received a bolus of microbubble contrast medium encapsulated by a shell of sulphur hexafluoride (SonoVue, 0.06 mL; Bracco SpA, Italy) delivered intravenously through an ear vein. The contrast medium was administrated via a three-way stopcock; this was followed by rapid delivery of a 5-mL bolus of saline. At the beginning of injection, images were captured for approximately 5 min at a rate of one frame per 5 sec for the first 120 sec and then at a rate of one frame per 30 sec.
Images were stored as BMP files and then transferred to a personal computer for analysis with NIH Image software (ver. 1.43; National Institutes of Health, USA). A region of interest (ROI) was drawn as large as possible, typically containing 200~500 pixels without including any adjacent tissue such as mesentery or interlobar arteries. Standardized time intensity curves depicting the signal intensity plotted against time were created based on selected ROIs in the renal cortex and medulla. The mean pixel values (MPVs) for each ROI in each image frame were then calculated.
The functional perfusion parameters were chosen according to previously described definitions [15,18]. Time-to-peak intensity (in seconds) is the time when intensity peaks. Peak intensity (MPV) is the maximal signal intensity, and average baseline (MPV) was also determined. Average upslope and downslope (MPV/sec) along with the standard deviations were calculated using Excel software (Microsoft, USA).
Statistical analysis
Statistical analyses were performed with Prism (ver. 5.04; GraphPad Software, USA). Upslope and downslope data were tested for linearity by assessing significance (p < 0.05) to validate the use of linear regression analysis. A paired t-test with a two-tailed p was used to compare the perfusion parameters such as the upslope, downslope, baseline intensity, peak intensity, and time-to-peak between the renal cortex and medulla. p-values < 0.05 were considered to be statistically significant.
Results
In general, it was easy to perform the contrast harmonic imaging examinations. Contrast enhancement of the normal renal parenchyma showed two phases in every micropig. After injecting the contrast medium, the cortex was initially enhanced followed by a more gradual enhancement of the medulla. The cortex had uniformly fast enhancement, and concentration of the enhancement was more intense in the renal cortex than the medulla (Figs. 1 and 2). A significant difference in perfusion was detected between renal cortex and medulla.
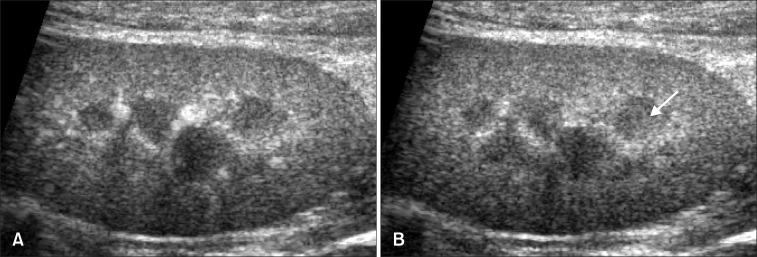
Fig. 1.
(A) Representative longitudinal plane images of the renal cortex captured at the time of peak intensity using contrast-enhanced ultrasonography. Maximum contrast enhancement of the renal cortex occurred at 17.5 ± 6.6 sec. (B) The renal medulla was also enhanced (arrow) and had a uniformly hyperechoic appearance.
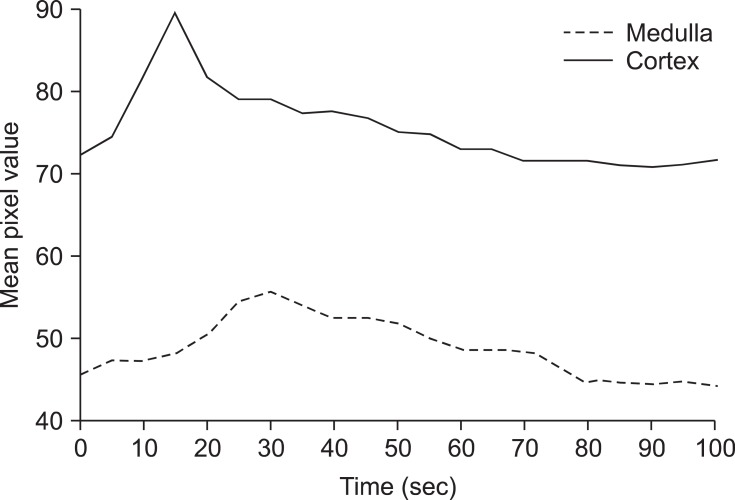
Fig. 2.
Representative time-mean pixel value (MPV) curves obtained by contrast-enhanced ultrasonography in the renal cortex and medulla of a healthy micropig. The upper curve represents enhancement of the cortex and the lower curve shows enhancement of the medulla.
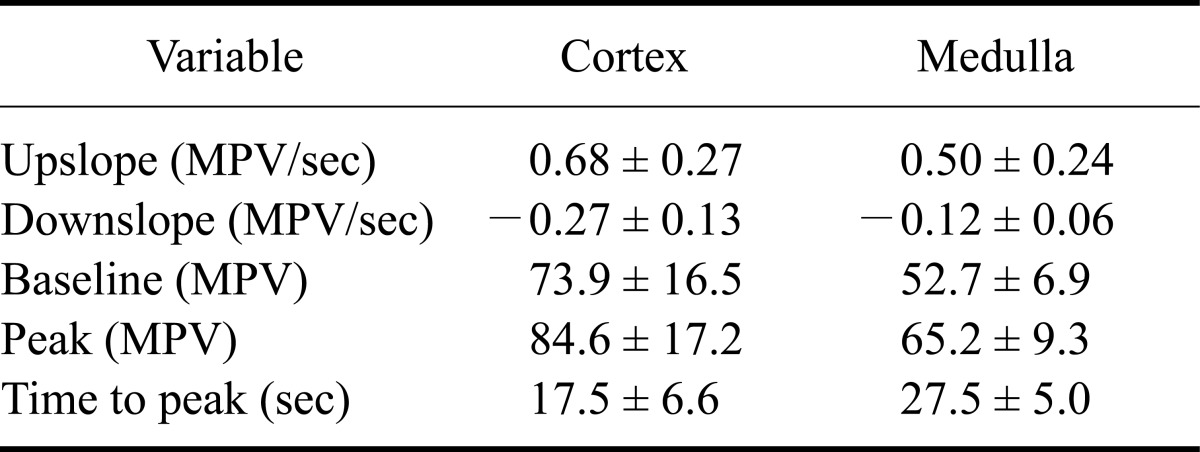
The average baseline intensity was 73.9 ± 16.5 MPV in the renal cortex and 52.7 ± 6.9 MPV in the renal medulla. The mean upslope was 0.68 ± 0.27 MPV/sec in the renal cortex and 0.50 ± 0.24 MPV/sec in the renal medulla. The average peak intensity in the renal cortex was 84.6 ± 17.2 MPV and 65.2 ± 9.3 MPV in the renal medulla. The mean time-to-peak in the renal cortex was 17.5 ± 6.6 sec and 27.5 ± 5.0 sec in the renal medulla. In the renal cortex, the average downslope was -0.27 ± 0.13 MPV/sec and -0.12 ± 0.06 MPV/sec in the medulla. The baseline, upslope, downslope, peak intensity, and time-to-peak values were all significantly different (p < 0.05) when comparing the renal cortex and medulla (Table 1).
Table 1.
Renal perfusion parameters in healthy micropigs using contrast-enhanced ultrasonography
All data are expressed as the mean ± SD. MPV: mean pixel value.
Discussion
The first ultrasound contrast agents mainly contained air microbubbles. Their persistence following injection is brief, and most bubbles are destroyed during the first passage through the lungs [16]. SonoVue, a stabilized aqueous suspension of sulphur hexafluoride microbubbles encapsulated in a phospholipid shell, is a second-generation ultrasound contrast medium. This agent is less fragile than first-generation compounds and its time of enhancement is longer [1].
Interlobular arteries branch off from arcuate arteries and radiate throughout through the cortex, ending in networks of capillaries in regions just inside the capsule. Interlobular arteries also branch off to afferent arterioles that carry blood to the glomeruli. Throughout most of the cortex, efferent arterioles subdivide into a second set of capillaries that supply blood to renal tubules and Henle's loop. Efferent glomerular arterioles in the juxtaglomerular glomeruli divide into vessels that supply the contiguous tubules and vessels which enter the bases of the renal medulla. Normally, blood circulating in the cortex is more abundant than that in the medulla [4,5,14].
Significant differences between perfusion patterns in the renal cortex and medulla can be explained by the dual renal capillary system. In kidneys, blood is supplied to the renal cortex before the medulla. We found that enhancement in the renal cortex was early, homogeneous, and intense. This was followed by gradual heterogeneous enhancement of the medulla and represented the delayed peak. The renal medulla seemed to have sparse enhancement first seen at the periphery followed by gradual enhancement of the inner portions according to the direction of blood flow.
The dual capillary bed system accounts for the difference between cortex and medulla perfusion patterns. The fast early cortex inflow is a reflection of blood flow into the glomeruli. The delayed peak may represent tubular perfusion into the second capillary bed concurrent with a more gradual inflow to the medulla. The overall decreased intensity of the medulla compared to the cortex at peak medulla intensity may be due to overall increased vascular space in the cortex, cortical bubble destruction, or venous drainage from the cortex tubules directly into the interlobular veins [18].
Many factors may influence the MPV within the renal cortex and medulla. First of all, we found a statistically significant difference in the peak intensity of the ROIs both for depth and size. The mean peak intensity decreased with increasing ROI depth and increasing ROI size [10]. Microbubble destruction can be affected by gain, mechanical index, and frequency. As these factors increase, the MPV decreases due to destruction of the contrast medium. Although these factors influence the MPV, they do not change with time and so time-to-peak, upslope, and downslope are rarely affected. However, mechanical factors such as saline flushing rate, three-way stopcock utilization, and volume of the saline flush can vary over time. These factors should be consistent for all studies. In the present investigation, normal renal perfusion values were determined for the micropig. However, these values should only be applied for studies using the same protocol and ultrasound settings because they are likely to differ with other protocols and machine settings.
In conclusion, we determined that contrast-enhanced ultrasonography could be used to evaluate renal perfusion in the kidney of micropigs. This technique is minimally invasive and useful for assessing renal perfusion in a clinical setting. Data from our study can be used as normal reference values and may be applied to the evaluation of young micropigs with renal disease.
Acknowledgments
This study was supported by a grant (2007 0401034006) from the Biogreen 21 program, Rural Development Administration, Korea.
References
- 1.Ascenti G, Zimbaro G, Mazziotti S, Chimenz R, Fede C, Visalli C, Scribano E. Harmonic US imaging of vesicoureteric reflux in children: usefulness of a second generation US contrast agent. Pediatr Radiol. 2004;34:481–487. doi: 10.1007/s00247-004-1190-z. [DOI] [PubMed] [Google Scholar]
- 2.Bouakaz A, de Jong N. WFUMB Safety symposium on echo-contrast agents: nature and types of ultrasound contrast agents. Ultrasound Med Biol. 2007;33:187–196. doi: 10.1016/j.ultrasmedbio.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 3.Claudon M, Barnewolt CE, Taylor GA, Dunning PS, Gobet R, Badawy AB. Renal blood flow in pigs: changes depicted with contrast-enhanced harmonic US imaging during acute urinary obstruction. Radiology. 1999;212:725–731. doi: 10.1148/radiology.212.3.r99se14725. [DOI] [PubMed] [Google Scholar]
- 4.Evans HE, Christensen GC. The urogenital system. In: Evans HE, editor. Miller's Anatomy of the Dog. 3rd ed. Philadelphia: WB Saunders; 1993. pp. 494–503. [Google Scholar]
- 5.Hollenberg N. The physiology of the renal circulation. In: Black D, Jones NF, editors. Renal Disease. 4th ed. Oxford: Blackwell; 1979. pp. 30–63. [Google Scholar]
- 6.Jayaweera AR, Edwards N, Glasheen WP, Villanueva FS, Abbott RD, Kaul S. In vivo myocardial kinetics of air-filled albumin microbubbles during myocardial contrast echocardiography. Comparison with radiolabeled red blood cells. Circ Res. 1994;74:1157–1165. doi: 10.1161/01.res.74.6.1157. [DOI] [PubMed] [Google Scholar]
- 7.Keller MW, Segal SS, Kaul S, Duling B. The behavior of sonicated albumin microbubbles within the microcirculation: a basis for their use during myocardial contrast echocardiography. Circ Res. 1989;65:458–467. doi: 10.1161/01.res.65.2.458. [DOI] [PubMed] [Google Scholar]
- 8.Kim B, Lim HK, Choi MH, Woo JY, Ryu J, Kim S, Peck KR. Detection of parenchymal abnormalities in acute pyelonephritis by pulse inversion harmonic imaging with or without microbubble ultrasonographic contrast agent. Correlation with computed tomography. J Ultrasound Med. 2001;20:5–14. doi: 10.7863/jum.2001.20.1.5. [DOI] [PubMed] [Google Scholar]
- 9.Kinns J, Aronson L, Hauptman J, Seiler G. Contrast-enhanced ultrasound of the feline kidney. Vet Radiol Ultrasound. 2010;51:168–172. doi: 10.1111/j.1740-8261.2009.01646.x. [DOI] [PubMed] [Google Scholar]
- 10.Leinonen MR, Raekallio MR, Vainio OM, Ruohoniemi MO, O'Brien RT. The effect of the sample size and location on contrast ultrasound measurement of perfusion parameters. Vet Radiol Ultrasound. 2011;52:82–87. [PubMed] [Google Scholar]
- 11.Miller DL, Dou C, Wiggins RC. Contrast-enhanced diagnostic ultrasound causes renal tissue damage in a porcine model. J Ultrasound Med. 2010;29:1391–1401. doi: 10.7863/jum.2010.29.10.1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nyman HT, Kristensen AT, Kjelgaard-Hansen M, McEvoy FJ. Contrast-enhanced ultrasonography in normal canine liver. Evaluation of imaging and safety parameters. Vet Radiol Ultrasound. 2005;46:243–250. doi: 10.1111/j.1740-8261.2005.00034.x. [DOI] [PubMed] [Google Scholar]
- 13.O'Brien RT, Iani M, Matheson J, Delaney F, Young K. Contrast harmonic ultrasound of spontaneous liver nodules in 32 dogs. Vet Radiol Ultrasound. 2004;45:547–553. doi: 10.1111/j.1740-8261.2004.04094.x. [DOI] [PubMed] [Google Scholar]
- 14.Pallone TL, Zhang Z, Rhinehart K. Physiology of the renal medullary microcirculation. Am J Physiol Renal Physiol. 2003;284:F253–F266. doi: 10.1152/ajprenal.00304.2002. [DOI] [PubMed] [Google Scholar]
- 15.Pietra M, Brini E, Fracassi F, Diana A, Cipone M. Use of the galactose-based contrast agent SHU 508A (Levovist) in renal ultrasonography of the dog. Vet Res Commun. 2005;29(Suppl 2):305–307. doi: 10.1007/s11259-005-0068-3. [DOI] [PubMed] [Google Scholar]
- 16.Quaia E. Microbubble ultrasound contrast agents: an update. Eur Radiol. 2007;17:1995–2008. doi: 10.1007/s00330-007-0623-0. [DOI] [PubMed] [Google Scholar]
- 17.Rademacher N, Ohlerth S, Scharf G, Laluhova D, Sieber-Ruckstuhl N, Alt M, Roos M, Grest P, Kaser-Hotz B. Contrast-enhanced power and color Doppler ultrasonography of the pancreas in healthy and diseased cats. J Vet Intern Med. 2008;22:1310–1316. doi: 10.1111/j.1939-1676.2008.0187.x. [DOI] [PubMed] [Google Scholar]
- 18.Waller KR, O'Brien RT, Zagzebski JA. Quantitative contrast ultrasound analysis of renal perfusion in normal dogs. Vet Radiol Ultrasound. 2007;48:373–377. doi: 10.1111/j.1740-8261.2007.00259.x. [DOI] [PubMed] [Google Scholar]
- 19.Wei K, Le E, Bin JP, Coggins M, Thorpe J, Kaul S. Quantification of renal blood flow with contrast-enhanced ultrasound. J Am Coll Cardiol. 2001;37:1135–1140. doi: 10.1016/s0735-1097(00)01210-9. [DOI] [PubMed] [Google Scholar]