Abstract
Background and Objectives
We investigated whether 1 hour reperfusion is enough to assess cardiodynamics and infarct size in both regional ischemia (RI) and global ischemia (GI) in isolated rat heart models.
Materials and Methods
Hearts were randomly assigned to one of the following groups (each n=14): 1) Sham hearts for 1 hour; 2) Sham hearts for 2 hours; 3) 30 minutes RI followed by 1 hour reperfusion; 4) 30 minutes of RI followed by 2 hours reperfusion; 5) 30 minutes GI followed by 1 hour reperfusion; and 6) 30 minutes GI followed by 2 hours reperfusion.
Results
There were no significant differences in infarct size between 1 hour and 2 hours reperfusion in both RI and GI. Left ventricular developed pressure was significantly decreased at both 1 hour and 2 hours reperfusion in groups of RI and GI compared to baseline (p<0.01). Rate-pressure product and +dP/dtmax also significantly decreased compared to baseline level at both 1 hour and 2 hours reperfusion in groups of RI and GI (p<0.05).
Conclusion
There was no significant difference in infarct size between 1 hour and 2 hours reperfusion in groups of RI and GI. Cardiodynamic variables measured at 1 hour and 2 hours reperfusion significantly decreased compared to baseline level. Our data suggests that reperfusion of 1 hour is sufficient to assess cardiodynamics in both regional and global ischemic isolated hearts model.
Keywords: Heart, Myocardial ischemia, Myocardial infarction, Myocardial reperfusion
Introduction
During the past several decades, the isolated perfused heart model with Langendorff apparatus has been widely and effectively used in rodents and rabbits in myocardial ischemia-reperfusion (I/R) injury research.1-3) In the myocardial I/R model, various duration sets of ischemia and reperfusion have been used according to researcher preference, species, ischemic models (regional or global), or end points.4-8) Approximately 30 minutes of index ischemia with 2 hours of reperfusion has been generally accepted for mechanical and morphometric measurements in isolated regional ischemic models using rat hearts.9-11)
Recently, an interesting and impressive amount of work on isolated heart I/R experiments has been reported. Ferrera et al.12) demonstrated that 1 hour reperfusion is enough for both cardiac function assessment and infarct size measurement in the isolated rat heart model. In their study, the infarct size measured at 1 hour and at 2 hours reperfusion after global normothermic ischemia was identical in both untreated control hearts and ischemic postconditioned hearts. This could make 1 hour reperfusion more accessible, effective, and save time compared to 2 hours reperfusion. However, clinically, regional myocardial ischemia is more important than global ischemia (GI). In addition, cardiac function progressively declines as reperfusion progresses in regional ischemic hearts, unlike the case with global ischemic hearts.
Therefore, the purpose of this study was to compare the cardiodynamics and infarct size between 1 hour and 2 hours of reperfusion in a regional ischemic model and to contrast these results with a global ischemic model.
Materials and Methods
The experimental procedures and protocols used in this study were reviewed and approved by our Institutional Animal Care and Use committee.
Making of ischemia and reperfusion
Male Sprague-Dawley rats (KOATECH Co., Cheongwon, Korea) weighing 300-350 gm received 100 mg/kg of pentobarbital sodium and 300 IU of heparin intraperitoneally. Hearts were isolated and perfused with normothermic modified Krebs-Henseleit (KH) buffer containing (in mM) 118.5 NaCl, 4.7 KCl, 1.2 MgSO4, 1.8 CaCl2, 24.8 NaHCO3, 1.2 KH2PO4, and 10 glucose, as described previously.13) Per-fusion was performed under a hydrostatic pressure of 100 cmH2O by adjusting the height of the reservoir. All hearts were allowed to stabilize at least 20 minutes and regional or GI was randomly induced.
All hearts were perfused within 30-40 seconds after excision. In the regional ischemic model, a snare was made with a PE50 tube at the major trunk of the left coronary artery or its prominent branches. Regional ischemia (RI), which was induced by pulling the snare, was confirmed by regional cyanosis and a substantial decrease in left ventricular developed pressure (LVDP). GI was induced by clamping the aorta. Reperfusion was started by releasing the ends of the suture in RI or by unclamping the aorta in GI.
Experimental protocols
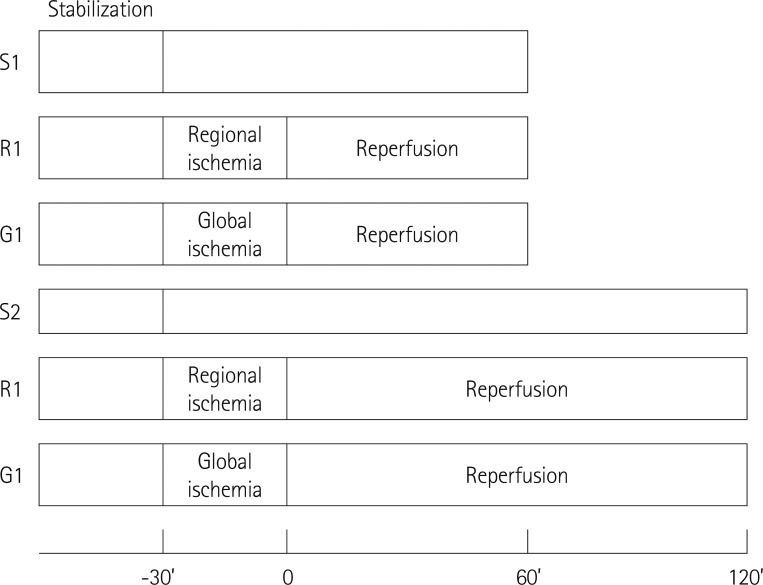
Hearts were randomly assigned to one of the following six groups: 1) S1, no ischemia and reperfusion Sham hearts for 1 hour; 2) S2, no ischemia and reperfusion Sham hearts for 2 hours; 3) R1: 30 minutes RI followed by 1 hour reperfusion; 4) R2, 30 minutes of RI followed by 2 hours reperfusion; 5) G1, 30 minutes GI followed by 1 hour reperfusion; and 6) G2, 30 minutes GI followed by 2 hours reperfusion (Fig. 1).
Fig. 1.
Experimental protocols. For measurement of infarct size and cardiodynamics, isolated rat hearts were exposed to 30 minutes ischemia followed by 2 hours reperfusion. Details for S1, S2, R1, R2, G1, and G2 are provided in the text.
Assessment of cardiac function
In isolated hearts, a fluid-filled balloon was inserted into the left ventricle and the balloon volume was adjusted to give a left ventricular end-diastolic pressure (LVEDP) of 5-10 mm Hg at the beginning of the experiment. The LVDP, which is regarded as a marker of contractility of the isolated rat heart, was calculated as the difference between left ventricular systolic pressure (LVSP) and LVEDP. Coronary flow (CF) was measured by timed collection of the perfusate dripping from the right heart into a graduated cylinder. Hemodynamic data, including heart rate (HR), LVSP, and LVEDP, were continuously recorded with BIOPAC system (BIOPAC Systems Inc., Goleta, CA, USA). The maximum of first derivative of left ventricular pressure (+dP/dtmax) was analyzed using analytic software (BSL v3.7.3). To compare the cardiodynamics between 1 hour and 2 hours, the CF, HR, LVDP, rate-pressure product (RPP), and +dP/dtmax measured at 1 hour and 2 hours after reperfusion were compared among the groups of S2, R2, and G2.
Determination of area at risk and infarct size
After 1 hour or 2 hours of reperfusion, the area at risk (AR) and area of necrosis (AN) were measured by fluorescent polymer microspheres (2-9 µm in diameter, Duke Scientific Corp., Palo Alto, CA, USA) and 2,3,5-triphenyltetrazolium chloride (TTC, Sigma-Aldrich Chemical., St. Louis, MO, USA) staining as described previously.14) The coronary artery was re-occluded and fluorescent polymer microspheres were infused. The hearts were weighed, frozen, and cut into 2-mm slices. The slices were incubated in 1% TTC in sodium phosphate buffer 37℃ for 20 minutes. The slices were immersed in 10% formalin and then examined under UV light. The AR and AN zone were quantified with Image Tool (UTHSCSA Image Tool, version 3.0, University of Texas, Health Science Center, San Antonio, TX, USA) and were converted into volumes by multiplying the areas. The volume of AN was expressed as a percentage of the AR volume or LV volume. All measurements were performed in a blinded fashion.
Statistical analysis
Data are presented as mean±SEM. Data analysis was performed with a personal computer statistical software package {Statistical Package for the Social Sciences (SPSS) for Windows, Release 18.0; SPSS Inc., Chicago, IL, USA}. Data were analyzed using t-test, and one-way and repeated measured analysis of variance. Differences were considered to be statistically significant when p were <0.05. To compare the differences in infarct size and cardiodynamics at the two different time points (1 hour and 2 hours), we performed sample size calculation using the GPower program. Assuming alpha level set at p=0.05, power (1-β) set to 0.8, and expecting to see effect size of at least 0.5, then the necessary the sample size in each group would be 14.
Results
There was no ventricular fibrillation (VF) in the Sham hearts while VF occurred after reperfusion in 28 ischemia-induced hearts (7 in R1, 6 in G1, 6 in R2, and 7 in G2) with no significant difference in the occurrence of VF among ischemia-induced groups.
Infarct size results
The body weight, heart weight, and LV volume were equivalent among groups (Table 1). The average AR/LV in R1 group and R2 group was 62.9% and 66.9% (p>0.05), respectively, which indicates that the two regional ischemic groups were subjected to equivalent degrees of RI. There were no significant differences in AN/LV between S1 (0.2±0.1%) and S2 (0.8±0.3%); R1 (14.4±2.3%) and R2 (16.5±2.4%); and G1 (23.7±5.4%) and G2 (39.6±6.2%), respectively (p>0.05). And there was no significant difference in AN/AR between R1 (22.8±4.3%) and R2 (26.9±3.7%); and G1 (23.7±5.5%) and G2 (39.6±6.2%) (p>0.05) (Fig. 2).
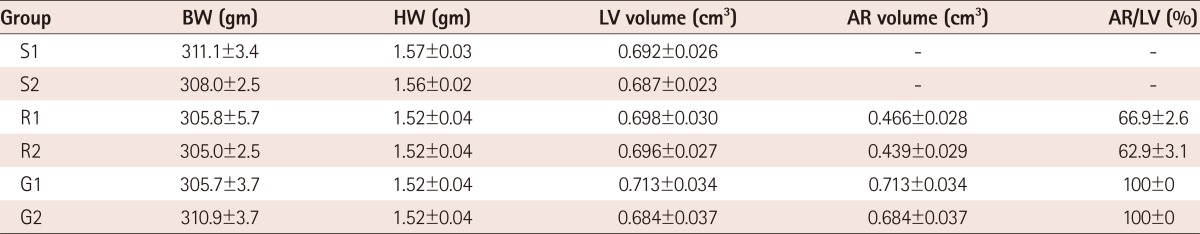
Table 1.
Morphometric data (n=14 for all groups)
Values are mean±SEM. Details for S1, S2, R1, R2, G1, and G2 are provided in the text. BW: body weight, HW: heart weight, LV: left ventricle, AR: area at risk
Fig. 2.
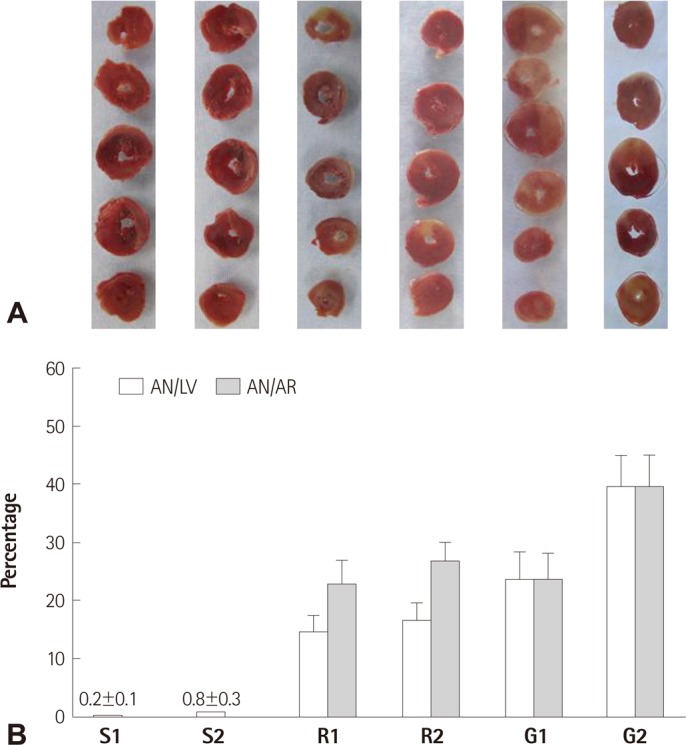
Morphometric changes after myocardial ischemia and reperfusion in isolated rat heart. A: representative sequential left ventricle slices each group showing area of necrosis (pale area) with triphenyltetrazolium chloride staining. B: percent of infarct area over area at risk. Values are mean±SEM. Details for S1, S2, R1, R2, G1, and G2 are provided in the text. There were no significant differences in AN/LV and AN/AR between S1 and S2, R1 and R2, and G1 and G2, respectively. AR: area at risk, AN: area of necrosis, LV: left ventricle, SEM: standard error of mean.
Functional recovery
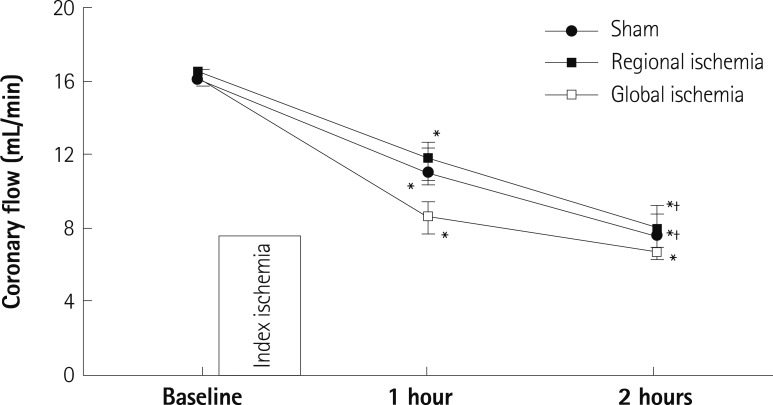
There were no significant differences in baseline CF, HR, LVDP, RPP, and +dP/dtmax among groups (Table 2). CF steadily declined after reperfusion in all groups and there were significant differences in CF at 1 hours and at 2 hours compared to baseline levels in all groups (p<0.01). In Sham and RI groups, the CF at 2 hours significantly decreased compared to 1 hour reperfusion (p<0.01) (Fig. 3).
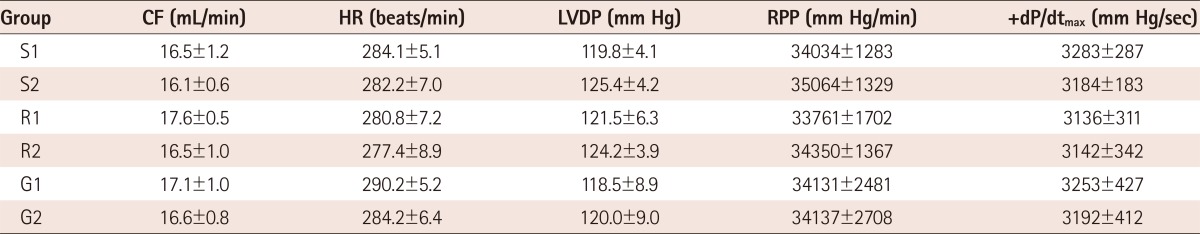
Table 2.
Baseline coronary flow and cardiodyanmics (n=14 for all groups)
Values are mean±SEM. There were no significant differences among groups. Details for S1, S2, R1, R2, G1, and G2 are provided in the text. CF: coronary flow, HR: heart rate, LVDP: left ventricular developed pressure, RPP: rate-pressure product, +dP/dtmax: maximum positive left ventricular pressure derivative
Fig. 3.
Changes in coronary flow in isolated rat hearts. 1 hour and 2 hours means 1 hour and 2 hours after reperfusion, respectively. *p<0.05 vs. baseline, †p<0.05 vs. 1 hour after reperfusion.
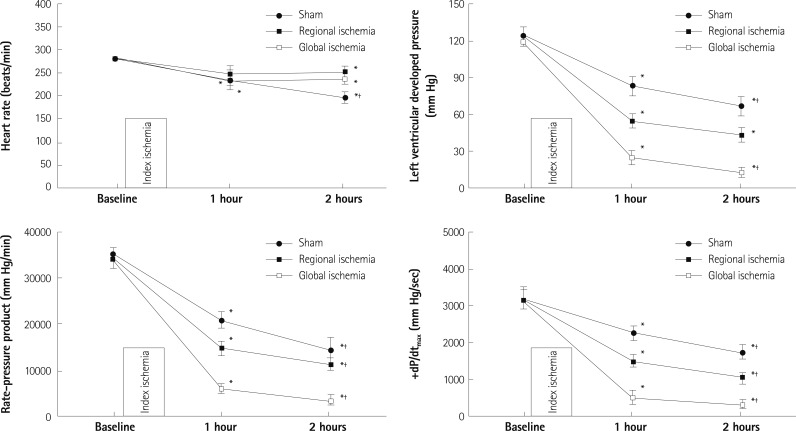
The HR steadily decreased after reperfusion. In the RI group, HR was significantly decreased at 2 hours (p<0.05) but not at 1 hour compared to baseline level. However, HR significantly decreased at both 1 hour and 2 hours compared to baseline level in the GI group (p<0.05) (Fig. 4). LVDP significantly decreased at 1 hour and 2 hours compared to baseline levels in all groups (p<0.001). There were significant differences in RPP at 1 hour and at 2 hours compared to baseline levels in all groups (p<0.001). In addition, there were significant differences in +dP/dtmax at 1 hour and at 2 hours compared to baseline levels in all groups (p<0.001).
Fig. 4.
Changes in cardiodynamics in isolated rat hearts. 1 hour and 2 hours means 1 hour and 2 hours after reperfusion, respectively. *p<0.05 vs. baseline, †p<0.05 vs. 1 hour after reperfusion.
Discussion
In 1895, the Langendorff apparatus was first designed by the German physiologist Oscar Langendorff for experiments on the isolated perfused mammalian heart which continued to beat and pump for several hours while being provided with oxygen and nutrients via a perfusate. This system, which is best suited for use with small animal hearts, allows studies on electrophysiology, myocardial metabolism and performance, infarct size, and pharmacological responses.
Infarct measurement, recovery of cardiac function, or myocardial enzyme release have been considered endpoints for anti-infarct measurement. The measurement of infarct size is an attractive surrogate and a reliable endpoint for early assessment of myocardial I/R injury, even though absolute infarct size results have varied among reports. Indeed, the averaged AN/AR in untreated isolated control hearts has been reported by some authors as high as 60% with TTC staining.15),16) However, about 30% of the AN/AR has been reported in untreated control hearts by other authors and our reports.13),17) Risk area and infarct size measurement may account for this discrepancy. In the present study, there were no significant differences in infarct size between 1 hour and 2 hours reperfusion in both regional and GI, even though myocardial infarction measured at 1 hour reperfusion trended toward smaller infarct size in isolated rat hearts. This suggests that 1 hour of reperfusion is enough when infarct size measurement is an endpoint in both regional and global I/R injury-induced isolated rat hearts. The recent report by Ferrera et al.12) also supports the usefulness of infarct measurement at 1 hour reperfusion in their global ischemic model.
Coronary flow and cardiodynamics, including LVDP, RPP, and dP/dtmax, were significantly decreased at both 1 hour and 2 hours reperfusion compared to baseline level in our regional and global ischemic hearts, except HR at 1 hour in regional ischemic heart. Our results differ from those of Ferrera et al.12) who reported no significant difference between 1 hour and 2 hours reperfusion in RPP recovery. They used 6 hearts for each group. However, we relied upon power analysis to determine that a sample size of 14 hearts in each group were necessary to detect important differences. The difference in sample size may underlie the different results and our result suggests that cardiodynamic variables differ at 1 hour and 2 hours.
Meanwhile, tissue salvage by an anti-infarct intervention leads to an improvement in cardiac function. Cardiodynamics, including LVDL and +dP/dtmax, along with infarct measurement are considered an improvement marker of post-ischemic LV function of isolated rat hearts.18-20) However, Gelpi et al.21) demonstrated that post-ischemic LVDP may be an unreliable marker of tissue salvage for preconditioning studies. Reduction in infarct size is not always associated with an improvement in functional recovery due to the continued stunning or the possibility that the salvaged tissue is not yet normal.7) Meanwhile, cardiac function progressively declined in isolated perfused hearts with time, even in those not subjected to I/R injury such as our Sham hearts. In addition, the LVDP and +dP/dtmax in isolated untreated control heart subjected to I/R model significantly declined after reperfusion compared to baseline level.22) In addition, in the Langendorff system, a fluid-filled, balloon-tipped catheter is usually used to measure intraventricular pressure. It is important to keep the balloon volume to a minimum and keep LVEDP low because of the isovolemic balloon system. Generally, researchers prefer to make their own balloons. Therefore, differences in balloon size would also affect intraventricular pressure.
Reperfusion time as well as the severity of ischemia may also affect AR/AN. In the present study, there were no significant differences in AR/LV among groups, suggesting that ischemia severity did not differ among groups. We did not measure levels of cardiac enzymes such as lactate dehydrogenase or creatine kinase as indicators of myocardial necrosis. Because there is evidence that lactate dehydrogenase and creatine kinase levels peak at first 1 hour of reperfusion rather than at 2 hours of reperfusion,12) future studies should compare cardiac enzyme levels in our models.
In conclusion, there is no significant difference in infarct size between 1 hour and 2 hours reperfusion in regional and global ischemic model. One hour reperfusion is effective to study myocardial ischemia and reperfusion injury in both regional and global ischemic isolated rat heart models.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Sako EY, Kingsley-Hickman PB, From AH, Ugurbil K, Foker JE. Substrate effects in the post-ischemic myocardium. J Surg Res. 1988;44:430–435. doi: 10.1016/0022-4804(88)90186-2. [DOI] [PubMed] [Google Scholar]
- 2.Stark G, Huber U, Hofer E, Tritthart HA. Continuous ECG measurements of intracardiac activity from the surface of Langendorff-perfused guinea pig hearts. Basic Res Cardiol. 1987;82:437–444. doi: 10.1007/BF01907091. [DOI] [PubMed] [Google Scholar]
- 3.Tanguay M, Blaise G, Dumont L, Beique G, Hollmann C. Beneficial effects of volatile anesthetics on decrease in coronary flow and myocardial contractility induced by oxygen-derived free radicals in isolated rabbit hearts. J Cardiovasc Pharmacol. 1991;18:863–870. doi: 10.1097/00005344-199112000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Batchu SN, Law E, Brocks DR, Falck JR, Seubert JM. Epoxyeicosatrienoic acid prevents postischemic electrocardiogram abnormalities in an isolated heart model. J Mol Cell Cardiol. 2009;46:67–74. doi: 10.1016/j.yjmcc.2008.09.711. [DOI] [PubMed] [Google Scholar]
- 5.Dickson EW, Hogrefe CP, Ludwig PS, Ackermann LW, Stoll LL, Denning GM. Exercise enhances myocardial ischemic tolerance via an opioid receptor-dependent mechanism. Am J Physiol Heart Circ Physiol. 2008;294:H402–H408. doi: 10.1152/ajpheart.00280.2007. [DOI] [PubMed] [Google Scholar]
- 6.Garcia SC, Pomblum V, Gams E, Langenbach MR, Schipke JD. Independency of myocardial stunning of endothelial stunning? Basic Res Cardiol. 2007;102:359–367. doi: 10.1007/s00395-007-0657-0. [DOI] [PubMed] [Google Scholar]
- 7.Lochner A, Genade S, Moolman JA. Ischemic preconditioning: infarct size is a more reliable endpoint than functional recovery. Basic Res Cardiol. 2003;98:337–346. doi: 10.1007/s00395-003-0427-6. [DOI] [PubMed] [Google Scholar]
- 8.Ofir M, Arad M, Porat E, et al. Increased glycogen stores due to gamma-AMPK overexpression protects against ischemia and reperfusion damage. Biochem Pharmacol. 2008;75:1482–1491. doi: 10.1016/j.bcp.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 9.Gross GJ, Baker JE, Hsu A, Wu HE, Falck JR, Nithipatikom K. Evidence for a role of opioids in epoxyeicosatrienoic acid-induced cardioprotection in rat hearts. Am J Physiol Heart Circ Physiol. 2010;298:H2201–H2207. doi: 10.1152/ajpheart.00815.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lamberts RR, Onderwater G, Hamdani N, et al. Reactive oxygen species-induced stimulation of 5'AMP-activated protein kinase mediates sevoflurane-induced cardioprotection. Circulation. 2009;120(11 Suppl):S10–S15. doi: 10.1161/CIRCULATIONAHA.108.828426. [DOI] [PubMed] [Google Scholar]
- 11.Xi J, McIntosh R, Shen X, et al. Adenosine A2A and A2B receptors work in concert to induce a strong protection against reperfusion injury in rat hearts. J Mol Cell Cardiol. 2009;47:684–690. doi: 10.1016/j.yjmcc.2009.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ferrera R, Benhabbouche S, Bopassa JC, Li B, Ovize M. One hour reperfusion is enough to assess function and infarct size with TTC staining in Langendorff rat model. Cardiovasc Drugs Ther. 2009;23:327–331. doi: 10.1007/s10557-009-6176-5. [DOI] [PubMed] [Google Scholar]
- 13.Jang Y, Xi J, Wang H, Mueller RA, Norfleet EA, Xu Z. Postconditioning prevents reperfusion injury by activating delta-opioid receptors. Anesthesiology. 2008;108:243–250. doi: 10.1097/01.anes.0000299437.93898.4a. [DOI] [PubMed] [Google Scholar]
- 14.Song DK, Jang Y, Kim JH, Chun KJ, Lee D, Xu Z. Polyphenol (-)-epigallocatechin gallate during ischemia limits infarct size via mitochondrial K(ATP) channel activation in isolated rat hearts. J Korean Med Sci. 2010;25:380–386. doi: 10.3346/jkms.2010.25.3.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bouwman RA, Vreden MJ, Hamdani N, et al. Effect of bupivacaine on sevoflurane-induced preconditioning in isolated rat hearts. Eur J Pharmacol. 2010;647:132–138. doi: 10.1016/j.ejphar.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 16.Taliyan R, Singh M, Sharma PL, Yadav HN, Sidhu KS. Possible involvement of α1-adrenergic receptor and K(ATP) channels in cardioprotective effect of remote aortic preconditioning in isolated rat heart. J Cardiovasc Dis Res. 2010;1:145–151. doi: 10.4103/0975-3583.70917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee DS, Steinbaugh GE, Quarrie R, et al. Ischemic postconditioning does not provide cardioprotection from long-term ischemic injury in isolated male or female rat hearts. J Surg Res. 2010;164:175–181. doi: 10.1016/j.jss.2010.08.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kolettis TM, Kontaras K, Spartinos I, et al. Dose-dependent effects of sildenafil on post-ischaemic left ventricular function in the rat isolated heart. J Pharm Pharmacol. 2010;62:346–351. doi: 10.1211/jpp.62.03.0009. [DOI] [PubMed] [Google Scholar]
- 19.Maslov LN, Lasukova OV, Krylatov AV, et al. Role of cannabinoid receptors in the regulation of cardiac contractility during ischemia/reperfusion. Bull Exp Biol Med. 2006;142:557–561. doi: 10.1007/s10517-006-0417-4. [DOI] [PubMed] [Google Scholar]
- 20.Rohlicek CV, Viau S, Trieu P, Hébert TE. Effects of neonatal hypoxia in the rat on inotropic stimulation of the adult heart. Cardiovasc Res. 2005;65:861–868. doi: 10.1016/j.cardiores.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 21.Gelpi RJ, Morales C, Cohen MV, Downey JM. Xanthine oxidase contributes to preconditioning's preservation of left ventricular developed pressure in isolated rat heart: developed pressure may not be an appropriate end-point for studies of preconditioning. Basic Res Cardiol. 2002;97:40–46. doi: 10.1007/s395-002-8386-0. [DOI] [PubMed] [Google Scholar]
- 22.Chen HT, Yang CX, Li H, et al. Cardioprotection of sevoflurane postconditioning by activating extracellular signal-regulated kinase 1/2 in isolated rat hearts. Acta Pharmacol Sin. 2008;29:931–941. doi: 10.1111/j.1745-7254.2008.00824.x. [DOI] [PubMed] [Google Scholar]