Abstract
Marijuana is known to have been used for medicinal and recreational purposes for thousands of years. Although marijuana has some diverse effects on cardiovascular system, there is insufficient knowledge concerning acute myocardial infarction (AMI) associated with marijuana and its underlying mechanism. We report the case of a 26 year-old young man suffering from ST-elevated AMI caused by marijuana abuse, which was successfully treating with percutaneous coronary intervention. It should be kept in mind that marijuana could be one of the most probable causes of AMI observed in apparently healthy young persons who use this drug.
Keywords: Cannabis, Myocardial infarction
Introduction
Marijiuna is the most widely used illicit drug in the United States and, marijiuana smoking is rapidly increasing in Europe and in some regions of Turkey.1),2) It is well known that marijiuana has several well-defined effects, such as irregularity of heart rate or blood pressure, vasospasm, vasodilation, and altered coronary flow to the heart and vascular system.2)
Although a few cases of myocardial infarction (MI) ascribing to marijuana use have been published,3-14) little is known about the association between the marijuana smoking and acute myocardial infarction (AMI). Herein, we describe the case of a 26-year-old young man suffering from ST-elevated AMI caused by an acute large thrombosis of the right coronary artery associated with marijuana abuse.
Case
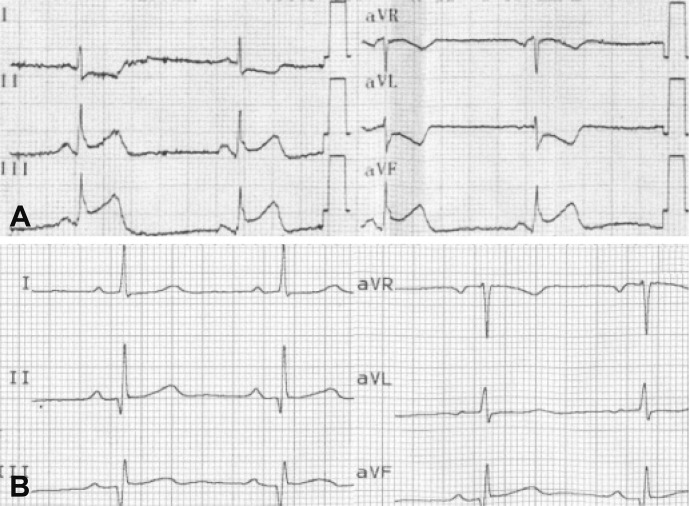
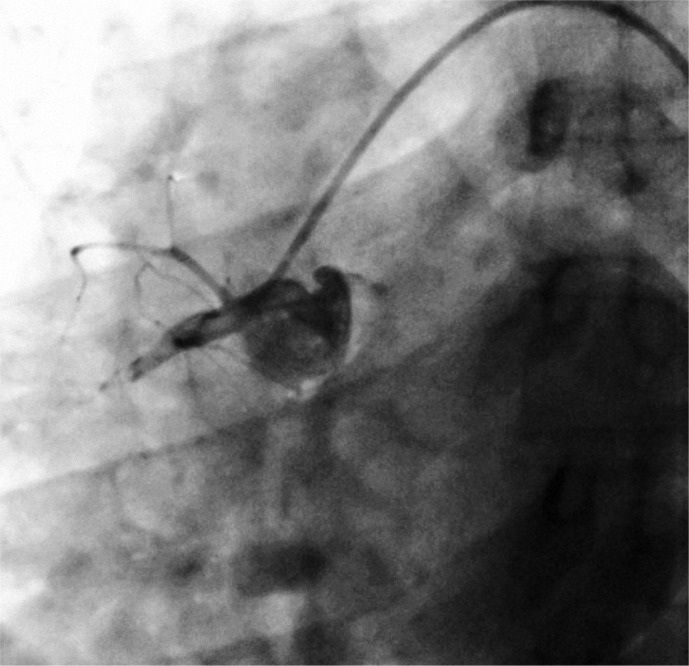
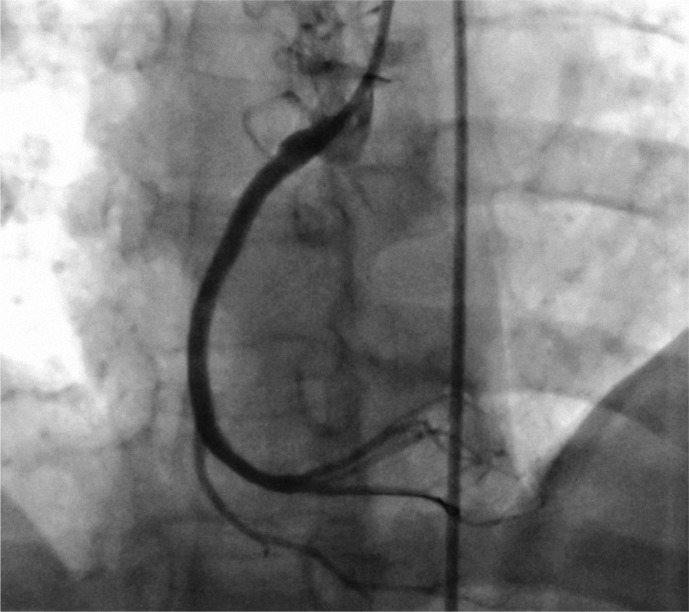
A 26-year-old man with no relevant risk factors for coronary artery disease, other than tobacco smoking, was admitted to our clinic because of retrosternal chest pain radiating to both arms for approximately 2 hours. On physical examination, he was distressed and sweaty, his blood pressure was 100/60 mm Hg. An electrocardiogram (ECG) showed sinus rhythm, heart rate of 55-60 bpm, and 2-3 mm ST-segment elevation formations on lead II, III and aVF derivations (Fig. 1A). The patient was not taking any medications. Later on, it was determined that patient had been smoking cannabis 2 times a week for the prior 8 years (last consumption 3 hours before onset of symptoms) and, in addition, smoked 10-15 tobacco cigarrettes per day over the same time period. In the emergency room, the patient was given aspirin first, followed by clopidogrel (a loading dose of 600 mg) and intravenous heparin (10000 IU). The patient was not given any thrombolytic therapy or the glycoprotein IIb/IIIa inhibitor before percutaneous coronary intervention (PCI). Thereafter, the patient was taken immediately to the coronary angiography laboratory for PCI. On coronary angiogram, it was observed that patient had minimal coronary irregularities, except for the total occlusion of proximal portion of the right coronary artery with a large thrombus burden (Fig. 2). A 0.014 inch intermediary guidewire was passed through the occlusion into the distal vessel, resulting in thrombolysis in myocardial infarction (TIMI)-0 flow. It was not possible to aspirate the large clot due to a lack of aspiration catheter at that moment. The large thrombotic burden and long coronary irregularities were seen after the culprit lesion was first predilated with 3.0×10 mm and 3.0×20 mm sized balloon catheters. We administered 200 microgram of nitroglycerin to the patient via the intracoronary route. Because of a large thrombus burden, a long irregularity of the right coronary artery and distal embolization, 3 differently sized stents were implanted, followed by intracoronary and intravenous infusion of the glycoprotein IIb/IIIa inhibitor, tirofiban, during PCI. Final angiography displayed no residual lesion with TIMI-III flow (Fig. 3). Patient's symptoms rebounded significantly after PCI. Then, ECG gradually showed the resolution of ST-segment elevation with Q-wave in the inferior leads (Fig. 1B). Creatine kinase (CK)-MB fraction of CK (CK-MB) and Troponin T values rose to 4461 IU/L (normal range: 22-200 IU/L), 386 U/L (normal range: <25 U/L) and 34 ng/mL (normal range: <0.04 ng/mL), respectively. Other hematological and biochemical tests revealed the following: Fibrinogen 2.1 g/L (normal range: 2.0-4.5 g/L), homocysteine 3.5 µmol/L (normal range: <12 µmol/L), total cholesterol 185 mg/dL (normal range: 125-200 mg/dL), triglyceride 94 mg/dL (normal range: 50-150 mg/dL), antithrombin III activity 107% (normal range: 70-125%), prothrombin time 11 second (normal range: 10-14 second), and activated partial thromboplastin time 29 second (normal range: 25-36 second). Factor V Leiden and prothrombin gene mutation tests were performed and found to be in the normal range. The patient was discharged without any complications after 4 days.
Fig. 1.
Electrocardiogram shows sinus rhythm and ST-segment elevation in the emergency room (A), and nearly complete resolution of ST-segment elevation with Q-wave in the inferior leads after percutaneous coronary intervention (B).
Fig. 2.
Left anterior oblique view of a large thrombotic occlusion of the proximal part of the right coronary artery.
Fig. 3.
Right anterior oblique cranial view of a thrombolysis in myocardial infarction-III flow after successfully treated with percutaneous coronary intervention of the thrombotic right coronary artery.
Discussion
Marijuana, which is drived from the plant Cannabis sativa, has been used for more than thousand years and for many different medicinal and recreational purposes.1),2) Although marijuana is known to contain at least 60 separate chemical products, the main biological effects of smoking marijuana result from delta-9-tetrahydrocannabinol (THC) and other cannabinoids (CBs). The effects of CBs are chiefly mediated by the activation of CB receptors. Two main subtypes of CB receptors have been determined and cloned (CB1 and CB2). While CB2 receptors are localized primarly to cells of the immune system, CB1 reseptors are found mainly in the central nervous system and, to a lesser extent, in certain peripheral tissues, such as the heart, adrenal gland, adipose tissue, liver, lung, and presynaptic nerve terminals.2)
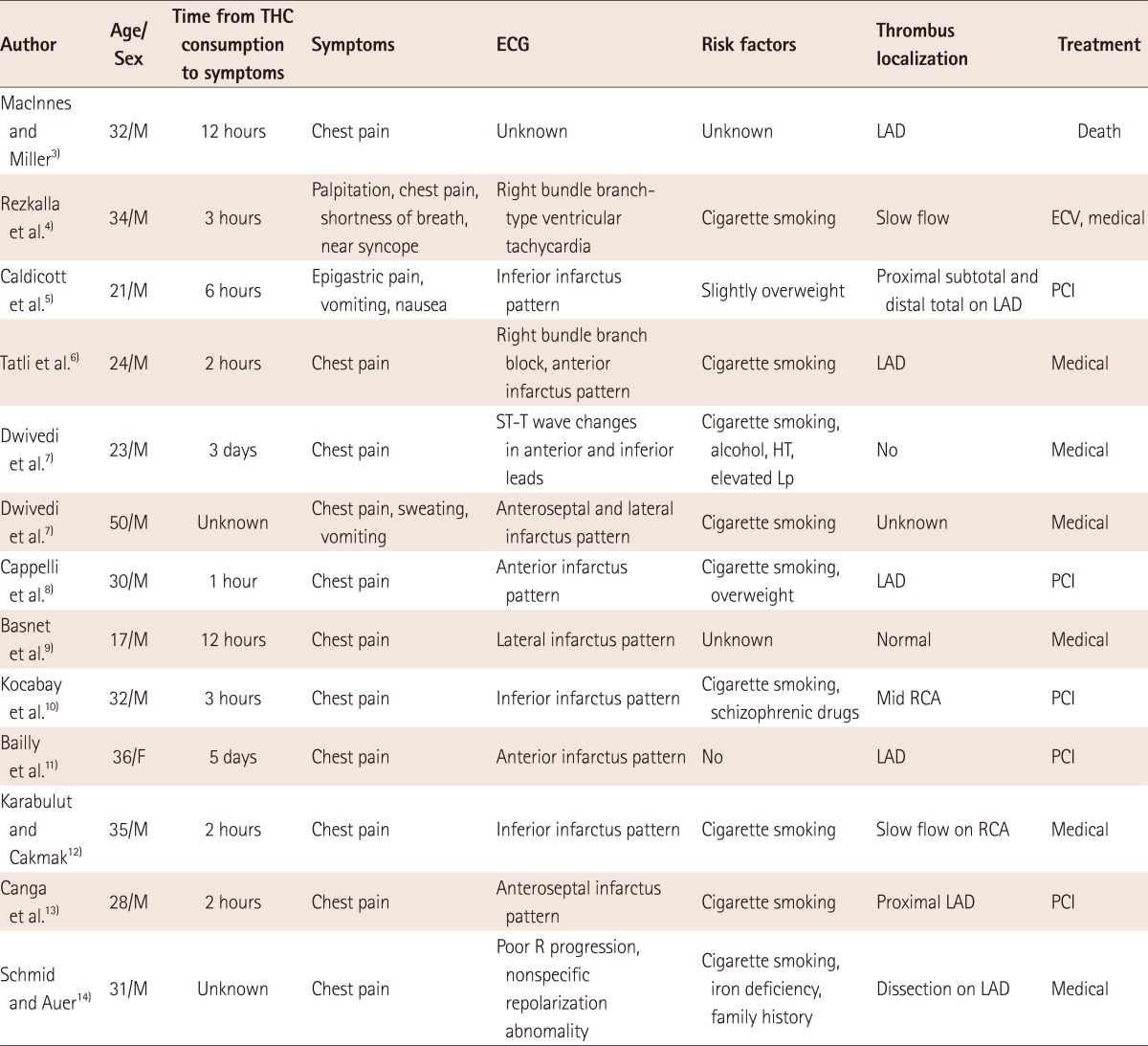
Cases of AMI, including other acute coronary syndromes, have rarely been reported as a consequence of marijuana use in the literature.3-14) We were able to determine that only 13 cases have been published with this specific entity through an inclusive search in PubMed. These case findings are displayed in Table 1. The mean age of patients was 30 years, with 92% being male. All patients presented with chest pain and MI, except for one patient case, which presented with palpitations, chest pain, near syncope, and ventricular tachycardia. The time from THC consumption to onset of symptoms ranged from 1 hour to 5 days. Although the underlying mechanism is not exactly known, some authors have speculated that the harmful effects of cannabis on the hemodynamic system may have precipitated the occurrence of MI in these cases. The cardiovascular effects of marijuana proceed primarily from a dose-dependent physiological effect on the autonomic nerve system. In acute doses, marijuana leads to a tachycardic effect of up to 160 beats per minute or higher, and a minor pressor-effect by increasing the sympathetic activity; chronic doses cause hypotension and bradycardia by increasing parasympathetic activity. A previously reported study has shown that marijuana smoking caused elevated carboxyhaemoglobin levels, resulting in reduced oxygen-carrying capacity, and a reduced exercise time of 48%, until angina is developed, whereas placebo reduced exercise time by 8.6%.15) A study by Mittleman et al.16) has also provided important evidence indicating that marijuana is a trigger of MI. In this study, it was reported that the risk of MI onset was elevated nearly 5 times over baseline in the hour after marijuana use, and the increased risk progressively decreased thereafter. Thus, the striking effects of marijuana may lead to deterioration of the balance between myocardial oxygen demand and supply, which easily prepares for an environment suitable for myocardial tissue ischemia.
Table 1.
Overview of published reports defining patients with acute coronary syndromes associated with marijuana smoking
M: male, F: female, ECV: electrical cardioversion, LAD: left anterior descending artery, RCA: right coronary artery, PCI: percutaneous coronary intervention, HT: hypertension, Lp: lipoprotein, ECG: electrocardiogram, THC: tetrahydrocannabinol
The effects of marijuana on coronary circulation in humans have not been well studied. Marijuana has various effects, such as vasoconstriction or vasodilation on different vascular beds and, may also cause coronary vasospasm or slow coronary flow (SCF) by its sympathetic or minimal pressor effects, especially in patients with atherosclerotic lesions present.2),4),9),12),15-17) Karabulut and Cakmak12) reported a case of inferior MI in a patient who had consumed marijuana regularly over a long period and whose coronary angiography demonstrated SCF. The authors concluded that marijuana consumption could be a major precipitating factor for SCF and MI. An additional study by Mukamal et al.17) suggested that marijuana may carry particular risk for susceptible persons with known cardiovascular disease. On the other hand, the culprit lesion in the vast majority of MIs usually develops at the site of a disrupted non-stenotic atherosclerotic plaque. Some authors have proposed a mechanism by which marijuana induced-spasm eventuates in endothelial denudation at the site of a stenotic or non-stenotic vulnerable atherosclerotic plaque in response to hemodynamic stressors. Hence, vasoactive and hemostatic factors released by platelets at this point may give rise to occlusive thrombus formation, culminating in AMI.3),16),17) A report by Maclnnes and Miller3) described a case of 32-year-old man with a ruptured coronary plaque leading to thrombus after marijuana use. In parallel with this logic, coronary vasospasm and endothelial damage at the position of sensitive plaque may be of great importance in the pathophysiology of AMI induced by marijuana abuse.
Another plausible explanation is that marijuana may have a direct effect on platelets or on the coagulation system. There is conflicting information on this topic. While some studies have demonstrated an inhibiting effect of large THC concentrations on agonist-induced platelet aggregation, others have reported elevated aggregation of platelets in the presence of THC.2) With regard to the effects of marijuana on the coagulation system, it has been reported that marijuana induced a minimal increase in factor VII activity, despite no clinically important changes in the coagulation system.2) Based on the availability of limited data, it is not clear as to whether marijuana alone induces direct thrombosis formation.
A subject of debate is whether marijuana-induced atrial fibrillation (AF) may result in coronary artery embolism, thus, leading to AMI. The majority of the aforementioned mechanisms are also acceptable in the underlying mechanisms of marijuana-induced AF. In recent years, it has been reported that few cases demonstrate an association between marijuna use and the development of AF.18) Such an association may play a crucial role in the clinical setting of patients with AMI caused by marijuana, even in short self-terminating episode of AF, in which AF may give rise to thromboembolic events, leading to coronary emboli. A formerly published case has demonstrated that AMI caused by coronary thromboembolism has taken place in patients with AF, even in the absence of the coronary artery disease or other risk factors.19) For this reason, it is reasonable to think that one of the most probable causes of AMI in a young individual, in particular related to large thrombosis, as in our case, may be due to marijuana-induced AF.
In conlusion, our report deals with the importance of awareness of the marijuana that may give rise to AMI, through the mechanisms discussed above, in apparently healthy young persons who occasionally or habitually use this drug.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Aktaş EÖ, Koçak A, Şenol E, et al. Evaluation of narcotic and stimulant drugs and abusers captured in Aegean region. Turkiye Klinikleri J Foren Med. 2006;3:13–24. [Google Scholar]
- 2.Mach F, Montecucco F, Steffens S. Cannabinoid receptors in acute and chronic complications of atherosclerosis. Br J Pharmacol. 2008;153:290–298. doi: 10.1038/sj.bjp.0707517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.MacInnes DC, Miller KM. Fatal coronary artery thrombosis associated with cannabis smoking. J R Coll Gen Pract. 1984;34:575–576. [PMC free article] [PubMed] [Google Scholar]
- 4.Rezkalla SH, Sharma P, Kloner RA. Coronary no-flow and ventricular tachycardia associated with habitual marijuana use. Ann Emerg Med. 2003;42:365–369. doi: 10.1016/s0196-0644(03)00426-8. [DOI] [PubMed] [Google Scholar]
- 5.Caldicott DG, Holmes J, Roberts-Thomson KC, Mahar L. Keep off the grass: marijuana use and acute cardiovascular events. Eur J Emerg Med. 2005;12:236–244. doi: 10.1097/00063110-200510000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Tatli E, Yilmaztepe M, Altun G, Altun A. Cannabis-induced coronary artery thrombosis and acute anterior myocardial infarction in a young man. Int J Cardiol. 2007;120:420–422. doi: 10.1016/j.ijcard.2006.08.012. [DOI] [PubMed] [Google Scholar]
- 7.Dwivedi S, Kumar V, Aggarwal A. Cannabis smoking and acute coronary syndrome: two illustrative cases. Int J Cardiol. 2008;128:e54–e57. doi: 10.1016/j.ijcard.2007.04.167. [DOI] [PubMed] [Google Scholar]
- 8.Cappelli F, Lazzeri C, Gensini GF, Valente S. Cannabis: a trigger for acute myocardial infarction? a case report. J Cardiovasc Med (Hagerstown) 2008;9:725–728. doi: 10.2459/JCM.0b013e3282f2cd0d. [DOI] [PubMed] [Google Scholar]
- 9.Basnet S, Mander G, Nicolas R. Coronary vasospasm in an adolescent resulting from marijuana use. Pediatr Cardiol. 2009;30:543–545. doi: 10.1007/s00246-009-9384-7. [DOI] [PubMed] [Google Scholar]
- 10.Kocabay G, Yildiz M, Duran NE, Ozkan M. Acute inferior myocardial infarction due to cannabis smoking in a young man. J Cardiovasc Med (Hagerstown) 2009;10:669–670. doi: 10.2459/JCM.0b013e32832bcfbe. [DOI] [PubMed] [Google Scholar]
- 11.Bailly C, Merceron O, Hammoudi N, Dorent R, Michel PL. Cannabis induced acute coronary syndrome in a young female. Int J Cardiol. 2010;143:e4–e6. doi: 10.1016/j.ijcard.2008.11.200. [DOI] [PubMed] [Google Scholar]
- 12.Karabulut A, Cakmak M. ST segment elevation myocardial infarction due to slow coronary flow occurring after cannabis consumption. Kardiol Pol. 2010;68:1266–1268. [PubMed] [Google Scholar]
- 13.Canga Y, Osmonov D, Karataş MB, Durmuş G, Ilhan E, Kırbaş V. Cannabis: a rare trigger of premature myocardial infarction. Anadolu Kardiyol Derg. 2011;11:272–274. doi: 10.5152/akd.2011.066. [DOI] [PubMed] [Google Scholar]
- 14.Schmid J, Auer J. Spontaneous coronary artery dissection in a young man - case report. J Cardiothorac Surg. 2011;6:22. doi: 10.1186/1749-8090-6-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aronow WS, Cassidy J. Effect of marihuana and placebo-marihuana smoking on angina pectoris. N Engl J Med. 1974;291:65–67. doi: 10.1056/NEJM197407112910203. [DOI] [PubMed] [Google Scholar]
- 16.Mittleman MA, Lewis RA, Maclure M, Sherwood JB, Muller JE. Triggering myocardial infarction by marijuana. Circulation. 2001;103:2805–2809. doi: 10.1161/01.cir.103.23.2805. [DOI] [PubMed] [Google Scholar]
- 17.Mukamal KJ, Maclure M, Muller JE, Mittleman MA. An exploratory prospective study of marijuana use and mortality following acute myocardial infarction. Am Heart J. 2008;155:465–470. doi: 10.1016/j.ahj.2007.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kosior DA, Filipiak KJ, Stolarz P, Opolski G. Paroxysmal atrial fibrillation following marijuana intoxication: a two-case report of possible association. Int J Cardiol. 2001;78:183–184. doi: 10.1016/s0167-5273(00)00459-9. [DOI] [PubMed] [Google Scholar]
- 19.Camaro C, Aengevaeren WR. Acute myocardial infarction due to coronary artery embolism in a patient with atrial fibrillation. Neth Heart J. 2009;17:297–299. doi: 10.1007/BF03086271. [DOI] [PMC free article] [PubMed] [Google Scholar]