Abstract
Objectives
Consumption of red and processed meat (RPM) is a leading contributor to greenhouse gas (GHG) emissions, and high intakes of these foods increase the risks of several leading chronic diseases. The aim of this study was to use newly derived estimates of habitual meat intakes in UK adults to assess potential co-benefits to health and the environment from reduced RPM consumption.
Design
Modelling study using dietary intake data from the National Diet and Nutrition Survey of British Adults.
Setting
British general population.
Methods
Respondents were divided into fifths by energy-adjusted RPM intakes, with vegetarians constituting a sixth stratum. GHG emitted in supplying the diets of each stratum was estimated using data from life-cycle analyses. A feasible counterfactual UK population was specified, in which the proportion of vegetarians measured in the survey population doubled, and the remainder adopted the dietary pattern of the lowest fifth of RPM consumers.
Outcome measures
Reductions in risks of coronary heart disease, diabetes and colorectal cancer, and GHG emissions, under the counterfactual.
Results
Habitual RPM intakes were 2.5 times higher in the top compared with the bottom fifth of consumers. Under the counterfactual, statistically significant reductions in population aggregate risks ranged from 3.2% (95% CI 1.9 to 4.7) for diabetes in women to 12.2% (6.4 to 18.0) for colorectal cancer in men, with those moving from the highest to lowest consumption levels gaining about twice these averages. The expected reduction in GHG emissions was 0.45 tonnes CO2 equivalent/person/year, about 3% of the current total, giving a reduction across the UK population of 27.8 million tonnes/year.
Conclusions
Reduced consumption of RPM would bring multiple benefits to health and environment.
Article summary
Article focus
Consumption of RPM is a leading contributor to GHG emissions.
High intakes of RPMs increase the risks of several leading chronic diseases.
This research identifies a low RPM dietary pattern that is already followed by a substantial fraction of the UK population and estimates health and environmental benefits that would result from its general adoption.
Key messages
Habitual RPM intakes are 2.5 times higher in the top compared with the bottom fifth of the UK consumers.
Sustained dietary intakes at a counterfactual reduced level in the UK population would materially reduce incidence of coronary heart disease, diabetes mellitus and colorectal cancer, by 3%–12%.
The predicted reduction in UK food- and drink-associated GHG emissions would equate to almost 28 million tonnes of CO2 equivalent/year across the population.
Strengths and limitations of this study
This research uses a food-based approach, taking intake-risk associations from meta-analyses rather than assuming the mechanisms by which the foods influence disease risk.
The dietary data were collected a decade ago; however, the headline results from a more recent national dietary survey reveal that intakes of all meat categories were broadly similar, although slightly higher in 2008/2009 than in 2000/2001.
Introduction
Climate change is ‘the biggest global health threat of the 21st century’,1 and appropriately chosen mitigation policies could ‘bring significant immediate co-benefits for population health and well-being’.2
Food and drink account for around one third of total greenhouse gas (GHG) emissions attributable to the UK consumers (when contributions from land-use change for agriculture are included). Around half of these emissions are ‘embedded’ in imports.3 Livestock products are particularly GHG intensive, with the Food and Agriculture Organisation attributing 18% of total global GHG emissions to these (when contributions from land use and land-use change are included).4 Although emissions can be reduced by changing production methods, savings achieved will not be sufficient to offset the effects of rising global demand, and radical departures from ‘business as usual’ trajectories will be needed to prevent global GHG emissions from livestock production rising unsustainably.5 6 Even when food imports to the UK are ignored, failure to reduce domestic agricultural emissions will risk making the government's 2050 target for an 80% reduction in total UK-based GHG emissions ‘unattainable’.7 Considering only the final food products, the UK is approximately 50% to 90% self-sufficient in livestock production (see web appendix). However, total GHG emissions arising from the full life-cycles of livestock food products are much bigger because of the overseas emissions associated with the large quantity of cereals and soy imported to feed animals raised in the UK.
Recent large meta-analyses8–10 have found significant increases in risk of coronary heart disease (CHD), type 2 diabetes and colorectal cancer with increased intake of processed meat (risk increases of 42%, 19% and 18%, respectively, per 50 g increase per day). A significant increase in colorectal cancer risk has also been shown with increased intake of red meat (17%/100 g increase per day).
Here, we estimate the co-benefits to health and climate change mitigation if, in the UK, high consumers of red and processed meat (RPM) were to adopt the dietary patterns of current low consumers. We estimate the reductions in GHG emissions using published life-cycle analyses of different foods and predict health benefits using published associations of RPM intakes with incidence of CHD, diabetes mellitus and colorectal cancer from recent meta-analyses. Together, these diseases accounted for almost 12% of the total disease burden in the UK in 2004.11
Methods
Dietary measurements
Meat intakes have been estimated from the 2000/2001 British National Diet and Nutrition Survey (NDNS), which collected 7 days of weighed dietary records from a sample of 1724 respondents aged 19–64 years.12 As previous reports from this source had not separately identified the meat content of composite meat-containing dishes, we derived new estimates by systematically recoding the original records.13 Meats were classified as (unprocessed) red, processed or white, and all foods were allocated to one of 45 food categories, designed to be relatively homogeneous in both their nutritional characteristics and the GHG emissions arising from their supply (table 1, which also includes the operational definitions of red, white and processed meat).
Table 1.
Greenhouse gas emissions, expressed as CO2 equivalents/kg food produced for consumption in the UK*
| Food category | GHG emissions (kg CO2-e/kg) | Inclusions/notes | Source | |
| Unprocessed meat | ||||
| 1 | Beef | 30.00 | DEFRA14 | |
| 2 | Lamb | 50.00 | DEFRA14 | |
| 3 | Pork | 10.00 | DEFRA14 | |
| 4 | Other red meat† | 30.00 | Venison, goat | Mean beef/pork/lamb |
| 5 | White meat‡ | 4.00 | Chicken, turkey, game birds | DEFRA14 |
| 6 | Other birds | 5.32 | Duck, goose | DEFRA14 |
| Processed meat§ | ||||
| 7 | Processed beef | 30.00 | = Beef | |
| 8 | Processed pork | 10.00 | Sausage meat, bacon, ham | = Pork |
| 9 | Processed white meat | 4.00 | = White meat | |
| Fish | ||||
| 10 | Fresh fish/shellfish | 2.60 | Wallen et al 15 | |
| 11 | Frozen fish | 6.50 | Wallen et al 15 | |
| Dairy/eggs | ||||
| 12 | Milk | 1.30 | Yoghurt, cream, custard | DEFRA14 |
| 13 | Cheese | 9.80 | Wallen et al 15 | |
| 14 | Ice cream | 0.64 | Wallen et al 15 | |
| 15 | Egg | 3.00 | DEFRA14 | |
| Starchy staples | ||||
| 16 | Bread | 0.73 | DEFRA14 | |
| 17 | Breakfast cereal | 1.00 | Wallen et al 15 | |
| 18 | Pasta | 0.81 | Wallen et al 15 | |
| 19 | Rice | 1.68 | Wallen et al 15 | |
| 20 | Unprocessed potato | 0.16 | DEFRA14 | |
| 21 | Frozen potato | 0.57 | Wallen et al 15 | |
| 22 | Other potato products | 2.37 | Wallen et al 15 | |
| 23 | Flour/other grains | 1.00 | Wallen et al 15 | |
| Fruit and vegetables | ||||
| 24 | Vegetables (1) | 0.50 | Roots, onions, brassicas | Wallen et al 15 |
| 25 | Vegetables (2) | 3.30 | All other, including salad | Wallen et al 15 |
| 26 | Pulses | 0.64 | Dried/tinned | Wallen et al 15 |
| 27 | Tomatog | 2.00 | Including tinned | DEFRA14 |
| 28 | Fruit | 0.40 | All | Wallen et al 15 |
| Fats | ||||
| 29 | Butter | 0.98 | Wallen et al 15 | |
| 30 | Margarine | 2.12 | Wallen et al 15 | |
| 31 | Cooking oil | 3.53 | Wallen et al 15 | |
| Other | ||||
| 32 | Crispbread/biscuits | 2.65 | Wallen et al 15 | |
| 33 | Buns/cakes | 0.91 | Wallen et al 15 | |
| 34 | Chocolate/sweets | 1.80 | Wallen et al 15 | |
| 35 | Sugar/honey/treacle | 4.18 | Wallen et al 15 | |
| 36 | Jam/marmalade | 0.81 | Including chutneys | Wallen et al 15 |
| Beverages | ||||
| 37 | Soft beverages | 0.56 | Wallen et al 15 | |
| 38 | Mineral water | 0.56 | = Soft beverages | |
| 39 | Alcoholic beverages | 0.56 | = Soft beverages | |
| 40 | Fruit juice/syrup | 0.99 | Including cordials | Wallen et al 15 |
| 41 | Coffee | 33.00 | DEFRA14 | |
| 42 | Tea | 4.10 | Including herbal tea | DEFRA14 |
| 43 | Cocoa | 210.00 | Including hot chocolate | DEFRA14 |
| 44 | Tap water | 0.00 | Including that in foods | No data |
| 45 | Miscellaneous | 1.85 | All other | Mean of all |
Further details in web appendix: assumptions and methods used in the derivation of greenhouse gas emissions from food produced for the UK consumers.
Emission estimates are preferentially based on life-cycle analyses. Where emissions vary by production system within and beyond the UK, values are averages weighted on contributions to the UK food supply.
The following definitions were used, consistent those used in the meta-analyses of intake-risk associations: †Red meat as beef, veal, pork, lamb, mutton and goat, either fresh, minced (including hamburgers) or frozen, but unprocessed other than by cooking with heat. Although processed meats were primarily red meats, the term ‘red meat’ has been used in this report to refer to ‘unprocessed red meat’, unless otherwise specified.‡White meat as meat from poultry, fresh, minced or frozen, but unprocessed other than by cooking with heat.§Processed meat as meat preserved by smoking, curing, salting or addition of nitrates, nitrites or other preservatives. Under this definition, processed meats were primarily red, but included white meats, and included ham, bacon, pastrami, salami, sausages and processed deli or luncheon meats.
Intakes of each type of meat were adjusted for total energy intake (in grams/megajoule). The NDNS sample was then split by sex and stratified on the basis of average daily intakes of RPM. Self-declared vegetarians (2.3% of men, 6.2% of women) were allocated to their own stratum.16 Remaining respondents were then ranked by average daily RPM intake and divided into fifths (F1 being lowest consumers, F5 highest). Mean RPM intakes for each of the resulting six sex-specific strata were standardised to the sex-specific mean energy intake in the total sample.
Among non-vegetarians, marked within-person variability existed in daily intakes of RPM over the 7-day recording period. As a consequence, the differences between strata created on the basis of just 7 days of observation were substantially greater than the differences that would have resulted had it been possible to create strata using information on each individual's usual (long-term average) intake. A method for correcting this inflation of between-stratum differences has been described elsewhere.13 In brief, sex-specific ratios of between- and within-person variances for energy-adjusted RPM intakes (in grams/megajoule) were used to derive sex-specific correction factors according to the following equation:
These correction factors (0.622 in men and 0.542 in women) were used to ‘shrink’ the differences between each stratum's initial estimated mean and the sex-specific grand mean in order to estimate expected mean usual intakes for each stratum—as though they had been created on the basis of usual intakes rather than on intakes observed over just 7 days. For self-reported vegetarians, recorded intakes of RPM (which were not all null) were taken as the best estimates of usual intakes.
Mean energy-standardised intakes of all the 45 food categories were then calculated for each stratum. Stratum F1 was taken to exemplify a ‘climate-friendly’ low RPM dietary pattern. Key food and nutrient intakes plus health, behavioural and socio-demographic variables across these strata are described elsewhere.13
Assignment of GHG emissions to food categories
Emissions (shown in table 1) are expressed as kilograms of CO2 equivalent (CO2-e) GHG resulting from all steps involved in making a given weight of food available for human consumption. Published values determined by life-cycle analyses were identified and used to estimate average emissions for each of the 45 food categories.14 15 Because emissions vary with system and country of production, weighted averages were calculated for meats according to proportions imported or produced in the UK under various systems. In the absence of data, processed meats were ascribed the values of equivalent unprocessed meats. Values for similar foods were interpolated where data were lacking. For the residual ‘miscellaneous’ category, the mean of all non-meat non-beverage categories was applied (further details in web appendix).
Specification of a counterfactual diet
A ‘feasible alternative’17 counterfactual distribution of diets was specified as one in which the proportions of vegetarians in each sex doubled and the remainder of the population adopted the average dietary pattern of F1. All else was assumed to remain equal. Calculations were based on data for persons aged 19–64 years. Estimates for Britain in 2000/2001 were assumed to be generalisable to the UK over the following decade to the present day.
Changes in meat-related disease risks with the counterfactual intakes
Risk relationships for RPM intakes and CHD, diabetes mellitus and colorectal cancer were taken from published meta-analyses, presented in table 2.8–10 The log of the RRs was assumed to be linearly related to absolute intakes across the full range of exposures in the data set, including the low (but not null) RPM intakes reported by self-declared vegetarians. Stratum-specific RRs were used to estimate proportional changes in aggregated population risks. These ‘potential impact fractions’ (PIF) were estimated separately for each sex, using the following equation18:
where p refers to the proportion of the population in a given stratum, i identifies the stratum and 1 and 2 identify the current and counterfactual intakes, respectively. An overall PIF for each disease was calculated as the simple average of the values for men and women. Effects of reduced intakes of RPM on colorectal cancer risk were assumed to be independent so that, for a given disease, the combined effect of both changes was estimated as: ((1−PIF1) × (1−PIF2)). This proportional change was then applied to the WHO estimates for disease burdens in the UK for 2004 to give a population aggregate risk reduction for the UK.11 Proportional risk reductions were also estimated for the hypothetical scenario of reducing RPM from the mean level for F5 to a sustained intake at the mean for F1.
Table 2.
Relative risks (RRs) of incident coronary heart disease, diabetes mellitus and colorectal cancer for differences of 100 g/day usual intakes of red and 50 g/day of usual intakes of processed meat from two meta-analyses
| Exposure | Disease | RR (95% CI) | Meta-analysis | Comments |
| Red meat* (RR per 100 g/day) | Coronary heart disease | 1.00 (0.81 to 1.23) | Micha et al 10 | Based on four estimates, most controlled for total energy intake. No between-study heterogeneity or publication bias was evident. The range of exposures across all included studies (means in lowest/highest categories) was 15.7–118.6 g/day. |
| Diabetes mellitus | 1.16 (0.92 to 1.46) | Micha et al 10 | Based on five estimates, most controlled for total energy intake. No between-study heterogeneity or publication bias was evident. The range of exposures across all included studies (means in lowest/highest categories) was 15.7–118.6 g/day. | |
| Colorectal cancer | 1.17 (1.05 to 1.31) | WCRF/AICR9 | Based on eight cohort studies, most controlled for total energy intake. There was no evidence of heterogeneity was present, and a random-effects model was used. There were insufficient studies to check for publication bias. Intakes per category spanned the range 1 to >200 g/day. | |
| Processed meat† (RR per 50 g/day) | Coronary heart disease | 1.42 (1.07 to 1.89) | Micha et al 10 | Based on six estimates, most controlled for total energy intake. Between-study heterogeneity and publication bias were evident; sensitivity analysis did not significantly change the outcome, and a random-effects model was used. The range of exposures across all included studies (means in lowest/highest categories) was 2.9–40.7 g/day. |
| Diabetes mellitus | 1.19 (1.11 to 1.27) | Micha et al 10 | Based on six estimates, most controlled for total dietary energy. Some heterogeneity was evident, but publication bias was not; sensitivity analysis did not significantly change the outcome, and a random-effects model was used. The range of exposures across all studies (means in lowest/highest categories) was 2.9–40.7 g/day. | |
| Colorectal cancer | 1.18 (1.10 to 1.28) | WCRF/AICR9 | Based on nine cohort studies, most controlled for total energy intake. Low heterogeneity was present, and a random-effects model was used. Publication bias was not evident. Intakes per category spanned the range 1 to>100 g/day. |
Red meat as beef, veal, pork, lamb, mutton and goat, either fresh, minced (including hamburgers) or frozen, but unprocessed other than by cooking with heat. Although processed meats were primarily red meats, the term ‘red meat’ has been used in this report to refer to ‘unprocessed red meat’, unless otherwise specified.
Processed meat as meat preserved by smoking, curing, salting or addition of nitrates, nitrites or other preservatives. Under this definition, processed meats were primarily red, but included white meats, and included ham, bacon, pastrami, salami, sausages and processed deli or luncheon meats.
Estimation of GHG emissions
Diet-attributable GHG emissions were estimated for each stratum by multiplying mean intakes of each of the 45 food categories by their average emission value (table 1) and summing resulting values. Estimated habitual intakes were used for RPMs; however, as the proportional changes to other food categories (after adjustment of meat intakes from measured to estimated habitual) were negligible (<3%), values derived from reported intakes were used for these. Resulting dietary emissions estimates were energy adjusted using the mean energy intake in the stratum and standardised to the mean sex-specific energy intake in the overall sample.
Diet-attributable GHG emissions under the counterfactual were calculated for each sex as weighted means of strata V and F1 (proportions in V doubling and F1 intake applied to all non-vegetarians). The overall value was calculated as the simple average of means for each sex. The difference between counterfactual and current emissions values gave the expected average reduction in emissions from the specified changes in measured dietary intakes at 19–64 years. These were then adjusted for average energy requirements in the total population relative to the study sample (which was restricted to ages 19–64 years). This adjustment factor was estimated at 0.93.19 Finally, the change in emissions based on measured intakes was rescaled to the level of the food supply supporting the measured intakes. This was based on the FAO Food Balance Sheet estimates, which give total meat available for consumption in Britain as 219 g/person/day compared with the measured intakes of 104 g/person/day. This ratio for meats was used as an estimate for inflation of total dietary GHG emissions, although it is accepted that wastage varies between food groups. No attempt was made to model the effects of reducing waste.
Results
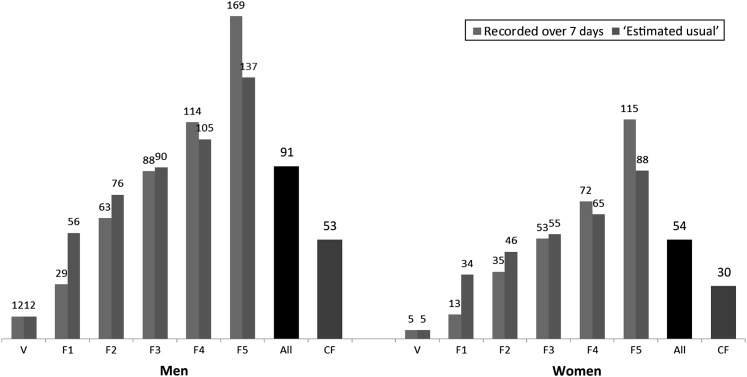
RPM intakes show marked heterogeneity across the British population, with habitual intakes around 2.5 times higher in the top (F5) than in the bottom (F1) fifth of non-vegetarians. Under our counterfactual, 4.7% of men and 12.3% of women were vegetarian and the remainder adopted the sex-specific dietary pattern of F1. Average RPM intakes were reduced from 91 to 53 g/day in men and from 54 to 30 g/day in women (42% and 44% reductions, respectively), as shown in figure 1.
Figure 1.
Reported and estimated habitual intakes of red and processed meat across strata based on energy-adjusted red and processed meat intake (mean and 95% CI). Intakes in mean g/day following energy adjustment and standardisation to sex-specific mean total reported energy intake. Overall factual and counterfactual (CF) mean intakes are also shown. V, vegetarian; F1–5, fifths of energy-adjusted red and processed meat intake (F1=lowest intake).
Changes in disease risks
Assuming epidemiologically observed risk associations are causal and independent, statistically significant risk reductions for the three diseases of interest would range from 3.2% to 12.2% under the counterfactual scenario (see table 3). Benefits would be greatest in those with the highest current intakes (F5; see table 4).
Table 3.
Predicted reductions (%) in population risks of coronary heart disease, diabetes and colorectal cancer from sustained exposure at counterfactual intakes of red and processed meat and both (assuming independence of effects)
| Red meat | Processed meat | Red and processed meat | |
| % Risk change (95% UI*) | % Risk change (95% UI*) | % Risk change (95% UI*) | |
| Coronary heart disease | |||
| Men | 0.0† (−10.4 to 11.0) | −9.7 (−1.8 to −18.1) | −9.7† (3.6 to −22.0) |
| Women | 0.0† (6.4 to −6.2) | −6.4 (−1.2 to −11.9) | −6.4† (1.8 to −14.3) |
| Diabetes mellitus | |||
| Men | −7.5† (4.2 to −18.6) | −4.9 (−2.8 to −7.3) | −12.0† (4.5 to −22.7) |
| Women | −4.5† (2.5 to −11.5) | −3.2 (−1.9 to −4.7) | −7.5 (−0.5 to −14.5) |
| Colorectal cancer | |||
| Men | −7.9 (−2.4 to −13.5) | −4.6 (−2.4 to −7.2) | −12.2 (−6.4 to −18.0) |
| Women | −4.8 (−1.4 to −8.3) | −3.0 (−1.6 to −4.7) | −7.7 (−4.0 to −11.3) |
Uncertainty intervals estimated by Monte Carlo simulation, using @Risk software (Palisade).
Non-significant.
Table 4.
Predicted reductions (%) in risks of coronary heart disease, diabetes and colorectal cancer for persons with usual intakes at the mean levels for F5 had they had sustained exposure at usual intakes for F1 of red and processed meat and both (assuming independence of effects)
| Red meat | Processed meat | Red plus processed meat | |
| % Risk change (95% UI*) | % Risk change (95% UI*) | % Risk change (95% UI*) | |
| Coronary heart disease | |||
| Men | 0.0† (25.7 to −20.4) | −20.6 (−4.2 to −35.1) | −20.6† (1.3 to −37.0) |
| Women | 0.0† (17.6 to −14.7) | −11.0 (−2.2 to −20.0) | −11.1† (7.7 to −26.7) |
| Diabetes mellitus | |||
| Men | −14.9† (9.2 to −33.8) | −10.5 (−6.4 to −15.7) | −24.1† (1.6 to −41.7) |
| Women | −10.8† (6.6 to −25.6) | −5.7 (−3.3 to −8.4) | −15.9† (0.9 to −30.0) |
| Colorectal cancer | |||
| Men | −15.7 (−4.9 to −25.6) | −10.3 (−5.5 to −15.5) | −24.4 (−13.6 to −34.1) |
| Women | −11.4 (−3.4 to −19.0) | −6.4 (−2.8 to −8.4) | −16.2 (−8.4 to −23.7) |
Uncertainty intervals estimated by Monte Carlo simulation, using @Risk software (Palisade).
Non-significant.
Changes in GHG emissions
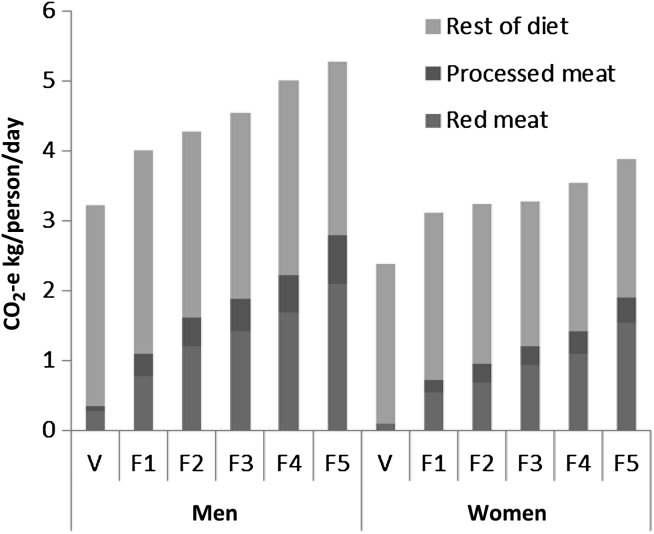
Total daily GHG emissions attributable to measured dietary intakes were estimated at 4.58 kg CO2-e in men and 3.34 kg CO2-e in women (unweighted mean 3.96 kg CO2-e). The sex difference disappeared when emissions were expressed per megajoule of dietary energy (0.47 kg CO2-e/MJ in men, 0.49 kg CO2-e/MJ in women). Red meat intake accounted for 31% of dietary CO2-e emissions in men and 27% in women, with processed meat accounting for an additional 10% and 8% in men and women, respectively.
CO2-e emissions attributable to diet are shown for each stratum in figure 2. Emissions for men increased by one third from F1 to F5 and for women by one quarter. Emissions attributable to dietary constituents other than RPM were relatively constant across strata.
Figure 2.
Diet-related standardised energy-adjusted CO2-e emissions according to dietary component across sex-specific categories of energy-adjusted red and processed meat intake (based on estimated habitual intake of red and processed meats). V, vegetarian; F1–5, fifths of energy-adjusted red and processed meat intake (F1=lowest intake)
Diet-related emissions, calculated on the basis of intakes, were reduced by 0.47 kg CO2-e/person/day (or 12%) to 3.96 kg CO2-e/person/day in men and 3.02 kg CO2-e/person/day in women. Scaling this estimate up to the food supplies supporting these intakes increases the expected reduction to 1.23 kg CO2-e/person/day or 0.45 tonnes/person/year. For the 2009 UK population of 61 792 000, this amounts to a total GHG reduction of 27.8 million tonnes/year.
Discussion
We have identified a low RPM dietary pattern that is already followed by a substantial fraction of the UK population and estimated the health and environmental benefits that would result from its general adoption. Although the dietary intake data used here were collected a decade ago, the headline results from a more recent NDNS (fieldwork carried out 2008/2009) reveal that intakes of all meat categories were broadly similar, although slightly higher than in 2000/2001.20 This indicates that our estimates remain relevant and may even be conservative and highlights the need for action to prevent further increases in intake in the UK population.
We estimate that sustained dietary intakes at our counterfactual levels would materially reduce incidence of CHD, diabetes mellitus and colorectal cancer. Our method for calculating changes in population aggregate risks could not allow for confounding on the outcome.21 Our point estimates for these reductions have associated uncertainties, which we have estimated using Monte Carlo simulation, although the RR estimates may still be more uncertain than we have assumed. Our estimates have been based on meta-analyses of a limited number of reports of the association between intakes of different types of meat and the chronic diseases of interest and are therefore highly dependent on these results. A more recent meta-analysis indicates that our results may be conservative for diabetes.22 This research, including over 440 000 individuals, found a similar but statistically significant increase in risk of type 2 diabetes with unprocessed red meat intake (RR 1.19 (95% CI 1.04 to 1.37) per 100 g unprocessed red meat per day) but a far stronger association with processed meat than that used here (RR 1.51 (95% CI 1.25 to 1.83) per 50 g processed meat per day). A recent update of the WCRF/AICR meta-analysis does not change the RR estimates given in that report and used in our analyses.23
Using meta-analyses of the association between intakes of different types of meat and the risks of vascular disease and diabetes, we have avoided simply regarding meat as a vehicle for dietary fats and assuming all associated risks to be mediated via effects on blood lipids.24 This food-based approach to assessing the health effects of meat is supported by the failure of epidemiological studies to confirm expected associations between intakes of unprocessed red meat and risk of CHD, by the differing patterns of epidemiological association with unprocessed and processed red meat and by the evidence that RPM intakes are associated with other vascular risk factors, notably blood pressure.25 26 While we have only considered a limited range of diseases here, the incidence of stroke and a wider range of cancers could also be expected to decline.27
Using 2004 Global Burden of Disease estimates for the UK,11 the reduction in health losses under the counterfactual would be 50 960 disability-adjusted life-years (DALYs) per year for ischaemic heart disease, 5421 DALYs per year for diabetes and 13 761 DALYs per year for colorectal cancer. If effects on these diseases were independent of each other, total reduction in DALYs would be 70 142/year, equivalent to almost 1% of health losses from all causes in the UK in 2004. These calculations are based on the assumptions that effects on incidence-based disease burdens are proportional to effects on incidence and that the results based on the diets of 19–64 year-olds are applicable to the over-65 population, where the majority of the disease burden lies.
The predicted reduction in GHG emissions would equate to a total saving in UK food- and drink-associated emissions of 27.8 million tonnes CO2-e/year across the 2009 UK population. To put this into context, the UK GHG ‘footprint’ has been estimated (using production-based accounts) at 10.16 tonnes CO2-e/person/year.28 29 Total emissions attributable to the UK consumers will exceed this by perhaps 30%–40% due to large net imports of embedded GHG.30 This implies that consumption-based emissions are over 14 tonnes CO2-e/person/year. Emissions reductions under the counterfactual therefore represent a saving of over 3% of this figure, a worthwhile amount given that climate change mitigation is going to require contributions from diverse sources.
Recent work for the UK Committee on Climate Change (CCC) has modelled the reductions in GHG emissions both in the UK and in overseas resulting from three specified dietary change scenarios.7 31 Under a scenario in which UK intake of livestock products was reduced by 50% (with a two-third reduction in all meat and the deficit replaced with plant-based foods), the reduction in GHG emissions was estimated to be 15.0 million tonnes CO2-e/year. In a second scenario, beef and sheep meat were replaced with pig and poultry, with no overall reduction in total meat intake, resulting in a reduction in GHG emissions of 6.3 million tonnes CO2-e/year. The dietary changes in the CCC scenarios were more extreme than the counterfactual dietary pattern taken here, with either a greater total reduction in meat or total elimination of beef and sheep meat. However, the GHG reductions estimated in this work were greater due to inflation to account for wasted food. While we made no attempt to model the impact of a reduction in waste, this demonstrates the great potential to make GHG savings even without major dietary changes through reducing waste. This approach, however, would not bring co-benefits to health.
We found that around one quarter of the UK population had habitual intakes of RPM below 55 g/day and 27 g/day for men and women, respectively, representing around two thirds (62%) and one half (51%) of their sex-specific means. Examination of the rest of the diet revealed that some, but far from all, of this reduction was offset by increased white meat intake, and remaining dietary substitution for RPM came from a wide variety of other sources.10 We have not considered beneficial effects from compensatory increases in other dietary components, especially fruit and vegetables and dietary fibre. Other assessments of the health effects of broadly similar dietary changes have found these beneficial effects to be of even greater magnitude than the reductions in harms.24 Recent estimation of the health effects of the CCC dietary scenarios has found that the greatest health gains were achieved when meat was replaced by fruits and vegetables.32 The influence of increases in these foods was far greater than health benefits attributable to reductions in salt consumption or changes in the fatty acid profile of the diets. When considering both the health and environmental effects of reducing RPM consumption therefore substitute foods are important, and clear advice should be given regarding these in order that benefits are maximised.
Intakes of RPM are socially patterned, especially in women. Forty-five per cent of low (F1) but only 29% of high (F5) RPM strata for women were in social class I or II and 41% versus 19% had formal education beyond A level.12 Although mainly outside the scope of this paper, it may also be noted that inequalities in health outcomes are produced by inequalities in health determinants, so a downward convergence of RPM intakes would be expected to yield a third benefit: a reduction in health inequalities. This is illustrated by the large potential risk reductions available to high consumers were they to converge down to the intakes of the low consumers.
Climate change mitigation is a far-future benefit that may not directly affect those who must make lifestyle changes now. It is therefore unlikely to be a strong motivator for change. In contrast, health benefits provide near-term rewards to individuals for climate-friendly changes and may thus ‘nudge’ humanity towards a sustainable future. Dietary recommendations should no longer be based on direct health effects alone. While the UK government has acknowledged the environmental impact of livestock production and is taking action with the industry to improve efficiency,33 changes in production will be insufficient alone to meet challenging emission reduction targets. Joint producer and consumer responsibility is needed, supported by the use of both production- and consumption-based GHG accounts. Averting dangerous climate change will require multiple changes at all levels of society, and the potential contribution of reduced RPM consumption should be addressed.
Supplementary Material
Footnotes
To cite: Aston LM, Smith JN, Powles JW. Impact of a reduced red and processed meat dietary pattern on disease risks and greenhouse gas emissions in the UK: a modelling study. BMJ Open 2012;2:e001072. doi:10.1136/bmjopen-2012-001072
Contributors: All authors contributed to conception and design of the study. Data analysis and interpretation were performed by LMA and JP. All authors contributed to manuscript preparation and have approved the submitted manuscript.
Funding: Work contributing to this manuscript was carried out as part of the University of Cambridge MPhil in Public Health degree (LMA and JNS, supervised by JWP); degrees were funded by the NHS East of England Multi-Professional Deanery.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: This research used the publicly available NDNS data set. GHG emissions were estimated from various published sources and are listed in the web appendix.
References
- 1. Costello A, Abbas M, Allen A, et al. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet 2009;373:1693–733 [DOI] [PubMed] [Google Scholar]
- 2. Garnett T. Cooking Up a Storm: Food, Greenhouse Gas Emissions and Our Changing Climate. Guildford: Food Climate Research Network, 2008 [Google Scholar]
- 3. Audsley E, Brander M, Chatterton J, et al. How Low Can We Go? An Assessment of Greenhouse Gas Emissions from the UK Food System and the Scope for Reduction by 2050. Godalming: WWF-UK, 2010 [Google Scholar]
- 4. Food and Agriculture Organisation Livestock's Long Shadow: Environmental Issues and Options. Rome: FAO, 2006 [Google Scholar]
- 5. McMichael AJ, Powles JW, Butler CD, et al. Energy and health 5-Food, livestock production, energy, climate change, and health. Lancet 2007;370:1253–63 [DOI] [PubMed] [Google Scholar]
- 6. Erb KH, Haberl H, Krausmann K, et al. Eating the Planet: Feeding and Fuelling the World Sustainably, Fairly and Humanely—A Scoping Study. Commissioned by Compassion in World Farming and Friends of the Earth UK. Vienna: Institute of Social Ecology, 2009 [Google Scholar]
- 7. Committee on Climate Change The Fourth Carbon Budget: Reducing Emissions through the 2020s. London: Committee on Climate Change, 2010. http://www.theccc.org.uk/reports/fourth-carbon-budget (accessed 28 Jun 2011). [Google Scholar]
- 8. WCRF/AICR Food, Nutrition, Physical Activity and the Prevention of Cancer: a Global Perspective. Washington DC: AICR, 2007 [Google Scholar]
- 9. Norat T, Chan D, Lau R, et al. The Associations Between Food, Nutrition and Physical Activity and the Risk of Colorectal Cancer: WCRF/AICR Systematic Literature Review Continuous Update Project Report. Imperial College London: WCRF/AICR, 2010 [Google Scholar]
- 10. Micha R, Wallace S, Mozaffarian D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: a systematic review and meta-analysis. Circulation 2010;121:2271–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. WHO Global Health Observatory Data Repository Death and DALY estimates for 2004 by cause for WHO member states. Geneva: WHO, 2009. http://apps.who.int/ghodata/?vid=10011 (accessed 20 Sep 2011). [Google Scholar]
- 12. Office for National Statistics National Diet and Nutrition Survey: Adults Aged 19 to 64 years, 2000-2001 [computer file] SN: 5140. Colchester, Essex: UK Data Archive [distributor], 2005 [Google Scholar]
- 13. Aston LM, Smith JN, Powles JW. Meat intake in Britain in relation to other dietary components and to demographic and risk factor variables: analyses based on the National Diet and Nutrition Survey of 2000/2001. J Hum Nutr Diet. In press. [DOI] [PubMed] [Google Scholar]
- 14. Department for Environment Food and Rural Affairs Scenario Building to Test and Inform the Development of a BSI Method for Assessing GHG Emissions from Food. Research Project Final Report FO0404. London: DEFRA, 2009 [Google Scholar]
- 15. Wallen A, Brandt N, Wennersten R. Does the Swedish consumer's choice of food influence greenhouse gas emissions? Environ Sci Policy 2004;7:525–35 [Google Scholar]
- 16. Henderson L, Gregory J, Swann G. The National Diet and Nutrition Survey: adults aged 19 to 64 years. Volume 1: Types and quantities of foods consumed. Norwich: HMSO, 2002 [Google Scholar]
- 17. Murray CJL, Lopez AD. On the comparable quantification of health risks: lessons from the Global Burden of Disease study. Epidemiology 1999;10:594–605 [PubMed] [Google Scholar]
- 18. Ezzati M, Lopez AD, Rodgers A, et al. Selected major risk factors and global and regional burden of disease. Lancet 2002;360:1347–60 [DOI] [PubMed] [Google Scholar]
- 19. Schofield WN. Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr 1985;39(S1):5–41 [PubMed] [Google Scholar]
- 20. Food Standards Agency Tables – NDNS Headline results from Year 1 of the Rolling Programme (2008/9). FSA, 2010. http://www.food.gov.uk/science/dietarysurveys/ndnsdocuments/ndns0809year1 (accessed 15 Jul 2010). [Google Scholar]
- 21. Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health 1998;88:15–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pan A, Sun Q, Bernstein AM, et al. Red meat consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updates meta-analysis. Am J Clin Nutr 2011;94:1088–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chan DS, Lau R, Aune D, et al. Red and processed meat and colorectal cancer incidence: meta-analysis of prospective studies. PLoS One 2011;6:e20456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Scarborough P, Noaham KE, Clarke D, et al. Modelling the impact of a healthy diet on cardiovascular disease and cancer mortality. J Epidemiol Community Health 2012;66:420–6 [DOI] [PubMed] [Google Scholar]
- 25. Miura K, Greenland P, Stamler J, et al. Relation of vegetable, fruit, and meat intake to 7-year blood pressure change in middle-aged men: the Chicago Western Electric Study. Am J Epidemiol 2004;159:572–80 [DOI] [PubMed] [Google Scholar]
- 26. Steffen LM, Kroenke CH, Yu X, et al. Associations of plant food, dairy product, and meat intakes with 15-y incidence of elevated blood pressure in young black and white adults: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Clin Nutr 2005;82:1169–77 [DOI] [PubMed] [Google Scholar]
- 27. Friel S, Dangour AD, Garnett T, et al. Public health benefits of strategies to reduce greenhouse-gas emissions: food and agriculture. Lancet 2009;374:2016–25 [DOI] [PubMed] [Google Scholar]
- 28. Department for Environment Food and Rural Affairs The Environment in Your Pocket. Norwich: The Stationery Office, 2009 [Google Scholar]
- 29. Office for National Statistics Population Estimates. 2010. http://www.ons.gov/ons/rel/npp/national-population-projections/2010-based-projections/index.html [Google Scholar]
- 30. Davis S, Caldeira K. Consumption-based accounting of CO2 emissions. Proc Natl Acad Sci U S A 2010;107:5687–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Audsley E, Angus A, Chatterton JC, et al. Food, land and greenhouse gases: The effect of changes in UK food consumption on land requirements and greenhouse gas emissions. Report for the Committee on Climate Change. Cranfield: Cranfield University, 2010 [Google Scholar]
- 32. Scarborough P, Allender S, Clarke D, et al. Modelling the health impact of environmentally sustainable dietary scenarios in the UK. Eur J Clin Nutr 2012;66:710–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. EBLEX Change in the Air: The English Beef and Sheep Production Roadmap. Kenilworth: EBLEX, 2009 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.