Abstract.
The objective of our study was to assess the efficacy of Graf ligamentoplasty in comparison with rigid fixation and fusion with the Hartshill horseshoe cage for similar severity of disc degeneration. Although studies have been done on the Graf ligamentoplasty procedure and the Hartshill horseshoe cage, their efficacy has never been compared in any study. This study was done to decide whether retaining mobility and stabilizing the spine is best or stiffening the lumbar segment by fusion is preferable. Between 1995 and 1997, a prospective randomized study was performed comparing Graf ligament stabilization and anterior lumbar interbody fusion. Twenty-eight patients had single-level Graf ligaments inserted and 27 patients had single-level anterior lumbar interbody fusion (ALIF) with a Hartshill horseshoe cage and tricortical iliac crest autograft. The two groups were similar in age, sex, symptoms, severity of the disc degeneration, and duration of follow-up. The chi-square test and t-test were used to evaluate the outcome. At a minimum follow-up of 2.1 years, we found that 93% of patients who had undergone Graf ligamentoplasty had a satisfactory outcome (rated "excellent" or "better") compared to 77.8% of patients who had been treated with ALIF with Hartshill horseshoe cage stabilization and fusion, when measured on the Oswestry Disability Index (P<0.05). Retaining mobility in the lumbar segments gives better results after stabilisation with Graf ligaments than rigid fixation and fusion with the Hartshill horseshoe cage in the short term. We will be watching this cohort of patients over the next few years.
Keywords. Lumbar interbody fusion, Graf ligament, Disc degeneration
Introduction
Graf ligamentoplasty
The soft system stabilization of Graf provides stabilization of the lumbar spinal segments without fusion [8]. Six- or seven-millimetre titanium pedicle screws are used bilaterally, and 8-mm braided polyester bands are looped over the posteriorly projecting screws. The bands are protected from adjacent bony prominences by cylindrical diabolos and are prevented from slipping off the pedicle screws by caps on the top of the screws. This construct constrains each motion segment in maximum extension (Fig. 1).
Fig. 1.

Radiograph showing Graf ligaments and pedicle screws
Abnormal rotatory movements and distraction at the facet joints associated with lumbar instability may be a cause of pain. The purpose of using a soft tissue stabilization system is to provide a firm but flexible posterior constraint to restore lumbar lordosis and stabilize the facet joints in extension [9]. Discogenic pain due to disc degeneration is thought to be a self-limiting phenomenon. Kirkaldy-Willis [16, 17] has described three stages of disc degeneration. The first stage is dysfunction. It is characterised by circumferential and radial tears in the disc annulus and localized synovitis and hypermobility of the facet joints. The second stage is instability. There is internal disruption of the disc, progressive disc resorption, degeneration of the facet joints with capsular laxity, subluxation, and joint erosion. The final stage is stabilization. This stage comprises osteophytosis and sometimes spinal stenosis. It is assumed that the Graf ligaments will stabilize the spine in stages 1 and 2 [12, 16, 17]. These ligaments will hold the spine in normal lordosis until there is normal adaptation to the loss of disc height (the stage of stabilization) [12, 16, 17].
The Hartshill horseshoe cage
Fusion for lumbar disc degeneration can be performed through an anterior or posterior approach. Posterior fusion is often supplemented with instrumentation. The success rates of anterior lumbar interbody fusion (ALIF) reported in the literature are quite variable. Penta and Fraser [23] reported a 68% patient satisfaction rate and 72.4% overall fusion rate at a minimum follow-up of 10 years. Tiusanen et al. [27] used posterior external fixators for stabilisation in ALIF. Solid fusion was obtained in 71% of patients, and 74% of patients were clinically very much improved at a minimum follow-up of 2 years (mean 5 years). Turner et al. [28] analysed 47 articles and found that on average 68% of patients had achieved a satisfactory outcome after lumbar fusion surgery (range 16–95%). Inoue and Watanabe [15] in 1982 reported on a large series of 350 patients who underwent anterior discectomy and interbody fusion for lumbar disc herniation. They achieved a 94.3% fusion rate, but the clinical results were good in 73% of patients.
Posterior fusion and instrumentation is a satisfactory method of treatment for low back pain. However, the outcome may be disappointing if the disc itself is the cause of pain. Flynn and Hoque [6], Stauffer and Coventry [26], and Newman and Grinstead [21] have reported complications of graft extrusion, compression and instability contributing to pseudarthrosis. The Hartshill horseshoe cage was designed to overcome these problems. To standardize our results to those recently reported in the literature [23, 27], we used validated objective scores and also assessed the sickness/disability benefit status and psychological distress of these patients.
The aim of our study was to evaluate the results of soft system stabilization in comparison with ALIF using Hartshill horseshoe cage for similar severity of disc degeneration.
Materials and methods
Forty-five patients treated for single-level disc degeneration by the senior author (N.R.B.), between April 1995 and June 1997, were included in the study. The patients were randomised to treatment with Graf ligamentoplasty (n=28) or ALIF supplemented with Hartshill horseshoe cage (n=27). Only patients who had discogenic back pain due to disc degeneration were included in the study; those who had disc prolapse or spinal stenosis due to disc degeneration were excluded.
Pre-operative diagnosis was made with magnetic resonance imaging (MRI) in all the patients and by provocative discography. The scans were graded from 1 to 4, using a modification of the classification proposed by Paajanen et al. [22] (Table 1 ). Discs appearing grey or black were classified as grade 1. Grade 2 was used to designate discs that were bulging or had annular tears. Grade 3 was used for discs that had end-plate changes, disc herniation, or less than 50% loss of disc height. Discs that had sequestered, or where there was frank intervetebral instability, or a listhesis of less than 25%, and there was greater than 50% loss of disc height but not total obliteration of the disc space were classified grade 4. Only patients with grade 3 or 4 on MRI scan were included in the study. Six patients with grade 1 and nine with grade 2 who had concordant pain on discogram were excluded from the study.
Table 1.
Classification of disc degeneration based on magnetic resonance imaging (MRI) scans (modified from Paajanen et al. [22])
| Grade | Characteristic |
|---|---|
| 1 | Bright signal intensity, provocative discography positive |
| 2 | Intermediate signal intensity |
| 3 | Low signal intensity + annular tears |
| 4 | Disc prolapse, loss of disc height, instability, and osteophytes |
The patients were assigned numbers after a decision was made to operate on them. A chit was drawn blindly from a box, with Graf ligament operation designated by "1" and Hartshill horseshoe fusion designated by "2". The draw was done a day before the operation, after which the patient was consented for the appropriate surgery. By picking up the chit from the box after shaking it well, we thought that the process was sufficiently random for there to be a 0.5 probability that the patient would have one of the two procedures.
Table 2 shows that the two groups were similar in age, sex, symptoms, grade of disc degeneration and duration of post-operative follow-up.
Table 2.
Demographic characteristics of the two groups
| Group A (Graf) | Group B (ALIF) | P-value | |
|---|---|---|---|
| Male | 17 | 12 | 0.3482 |
| Female | 11 | 15 | |
| Age: mean (range) | 44 (26–70) | 45 (25–67) | 0.9888 |
| Back pain, years: mean (range) | 7.3 (0.1–32) | 8.8 (2.1–32) | 0.9076 |
| Leg pain, years: mean (range) | 3.9 (0–20) | 7.3 (0–32) | 0.7210 |
| Disc disease grade 3a: no. of segments | 11 | 18 | 0.6645 |
| Disc disease grade 4a: no. of segments | 17 | 9 | 0.6471 |
| Mean follow-up | 2.5 (2.1–3.1) | 2.9 (2.1–4.4) | 0.9263 |
MRI grading
An independent assessor (S.M.) performed the entire review of the cases. The independent assessor was a specialist registrar, who reviewed the senior author's results. After the full assessment and analysis, the senior author read the results and supervised the interpretation of the outcome of this study.
Graf ligamentoplasty (group A)
Twenty-eight patients were randomised to Graf ligamentoplasty. The operation is performed through a midline posterior approach. Intra-operative radiographs were taken to confirm the level. The facet joint capsule was preserved whilst inserting the pedicle screws. Of the 28 patients reviewed, 17 were men and 11 were women, with a mean age of 44 years (range 26–70 years). The minimum follow-up period was 2.1 years after surgery (range 2.1–3.1 years; mean 2.5 years). The mean duration of pre-operative back pain and leg pain was 7.3 years and 3.9 years respectively. Eleven levels had grade 3 involvement and 17 levels had grade 4 involvement of their discs on the MRI scan. Eight of the levels had disc bulges, and one of these showed a high-intensity zone; ten levels had annular tears. The operative site involved the level L5-S1 in 13 cases, the L4-L5 level in 14 cases, and the L3-L4 level in 1 case.
Hartshill horseshoe cage (group B)
Twenty-seven patients were randomised to ALIF supplemented with the Hartshill horseshoe cage. The horseshoe shape of this titanium cage permits load bearing at the periphery of the endplates. The central space is empty to accommodate the bone graft. There are oblique holes in the implant for the screw fixation to the vertebral body (Fig. 2).
Fig. 2.

Hartshill horseshoe cage in the disc space with screws in the vertebral bodies stabilising the lumbar segment
The operation is performed through a direct anterior transperitoneal approach (Pfannenstiel) for L5-S1 and a standard anterolateral retroperitoneal approach for the other lumbar levels. Steinmann pins are inserted in the vertebral body and intra-operative radiographs are taken to confirm the level. The annulus is exposed and excised along with the nucleus pulposus right down to the posterior longitudinal ligament. The upper and lower endplates are cleared of all the cartilage up to the bleeding cancellous bone. A peripheral cortical rim is retained over the upper and lower surface of the adjacent vertebrae to seat the horseshoe cage. Tricortical iliac crest bone autograft was used for fusion along with small pieces of cancellous graft packed firmly in the horseshoe.
Of the 27 patients reviewed, 12 were men and 15 were women, with a mean age of 45 years (range 25–67 years). The minimum follow-up period was 2.1 years after surgery (range 2.1–4.4 years; mean 2.9 years). Eighteen patients had grade 3 involvement and nine patients had grade 4 involvement of their discs. Five patients had complete annular tears. The mean duration of pre-operative back pain and leg pain was 8.8 years and 7.3 years respectively. The fusion site involved the L5-S1 level in 13 cases, the L4-L5 level in 13 cases, and the L3-L4 level in 1 case.
Outcome assessment
Outcome was assessed according to a variety of measures of pain and function. Pre- and post-operative scores were available for all patients.
Oswestry Disability Questionnaire
Objective assessment was made by using the Oswestry Disability Questionnaire [5]. Patients were rated on the following parameters:
Excellent: improvement of at least 40 points and/or post-op score <20 on Oswestry Disability Index (ODI) and back to normal ODI function
Better: improvement of between 20 and 40 points, and/or score of between 20 and 40 on the ODI, and back to 50% of normal ODI function
Same: improvement of <20 points on the ODI and no functional recovery
Worse: post-op score worse than pre-op score on the ODI and poor ODI function after operation
Subjective rating of pain and function
Patients were asked to complete a ten-point visual analogue pain scale, with 0 indicating "no pain at all" and 10 indicating "maximum pain possible". A pain drawing was used for the patients to show the site of pain. They were asked to describe the characteristic of the pain, which was scored as: numbness 4, pin prick 3, burning 2, stabbing 1. Patients' pain and function were also evaluated using a "core set" of six questions as proposed by Deyo et al. [4]. This questionnaire covered the domains of pain symptoms, back-related function, generic well-being, disability (social role), and satisfaction with care (Fig. 3). The minimum score was 10 and the maximum 50. A post-operative score of ≤30 was considered to be a good overall outcome.
Fig. 3.
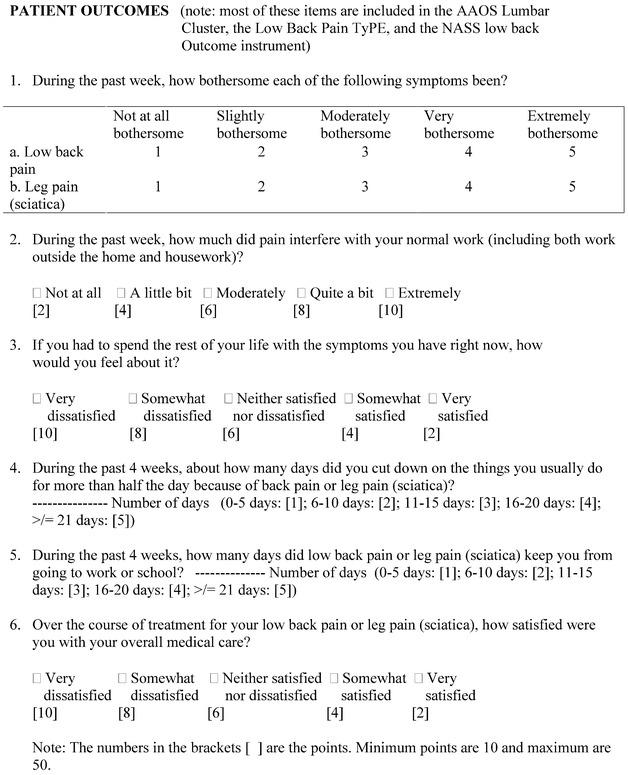
"Core set" of outcome measures for low back pain research [4] (note: most of these items are included in the AAOS Lumbar Cluster, the Low Back Pain TyPE, and the NASS Low Back Outcome instrument)
Psychological distress
A psychometric measure incorporating the Modified Somatic Perception Questionnaire (MSPQ) [20] and the Zung Depression Scale (ZDS) [29] was used to assess psychological distress at review. A combined score from 0 to 99 is calculated and distress is defined as a score of 29 or more for men and 33 or more for women.
Statistical analysis
The differences observed between the groups were analysed using the chi-square test and t-test.
Results
Clinical results
Graf ligamentoplasty
The pre-operative mean Oswestry Disability Score was 66 points (range 34–88 points) and the post-operative mean score was 25.3 (range 0–76 points). Twenty-six patients 93% improved significantly (rated as "excellent" or "better") when measured with the Oswestry Disability Questionnaire. The pain and function results derived from the pre-operative and post-operative Oswestry Disability Questionnaire are shown in Table 3 . The pre-operative "core set" mean score of 37.53 (range 18–50) improved significantly to a mean score of 20.25 (range 9–44). Twenty-two patients (78.6%) had improved significantly (score ≤30) as measured by the "core set" score. The improvements in the psychological distress, visual analogue pain scale, "core set" and pain drawing score were statistically significant (P<0.05).
Table 3.
Pre-operative and post-operative scores at last follow-up (ZDS+MSPQ Zung Depression Scale + Modified Somatic Perception Questionnaire, ALIF anterior lumbar interbody fusion)
| Group A (Graf) Mean (range) | Group B (ALIF) Mean (range) | |
|---|---|---|
| Pre-op. Oswestry | 66 (34–88) | 60.22 (34–86) |
| Post-op. Oswestry | 25.3 (0–76) | 33.3 (0–82) |
| Pre-op. functiona | 16.25 (0–30) | 16.48 (5–40) |
| Post-op. functiona | 56.43 (5–90) | 42.96 (5–75) |
| Pre-op. ZDS+MSPQ | 48.2 (18–75) | 46.03 (18–75) |
| Post-op. ZDS+MSPQ | 22 (0–71) | 31.07 (6–99) |
| Pre-op. pain drawing | 7.5 (1–15) | 8.55 (2–30) |
| Post-op. pain drawing | 4.5 (0–15) | 5.6 (0–36) |
| Pre-op. visual analogue | 8.4 (2–10) | 8.33 (4–10) |
| Post-op. visual analogue | 3.1 (0–10) | 4.04 (0–10) |
| Pre-op. "core set" | 37.53 (18–50) | 37.52 (20–50) |
| Post-op. "core set" | 20.25 (9–44) | 22.96 (8–50) |
a As measured by the Oswestry Disability Questionnaire
Hartshill horseshoe cage
The pre-operative mean Oswestry Disability Score was 60.2 points (range 34–86 points) and the post-operative mean score was 33.3 (range 0–82 points). Twenty-one patients (77.8%) improved significantly when measured with the Oswestry Disability Questionnaire. The pain and function results derived from the pre-operative and post-operative Oswestry Disability Questionnaire are shown in Table 3 . The pre-operative "core set" mean score of 37.52 (range 20–50) improved significantly to a mean score of 22.96 (range 8–50). Twenty-two patients (81.5%) had improved significantly (score ≤30) as measured by the "core set" score.
The improvements in the psychological distress, visual analogue pain scale, "core set" and pain drawing score were statistically significant (P<0.05).
Comparison of the outcome of the two procedures
Table 3 shows the scores of the two groups on a range of measurements. Table 4 shows the outcome of patients in each group according to their rating on the ODI. There was a statistically significant difference between the two groups, with the Graf ligamentoplasty patients doing better than patients who had fusion.
Table 4.
Comparison of the outcome of the two groups. The outcome of the Graf ligamentoplasty group was statistically significantly better than that of the ALIF with Hartshill horseshoe cage group (P=0.0477; chi-square test)
| Group A (Graf) | Group B (ALIF) | |
|---|---|---|
| Worse | 2 | 1 |
| Same | 0 | 5 |
| Better | 10 | 4 |
| Excellent | 16 | 17 |
Complications
In the Graf ligamentoplasty group (group A), one patient had superficial wound infection and one had chest infection. Both settled with oral antibiotics.
In the ALIF with Hartshill horseshoe cage group (group B), there was one misplaced horseshoe that caused radicular symptoms. The patient required a revision after a fortnight. In addition there was one patient with a urinary tract infection and another with iliac bone graft donor site persistent pain.
Fusion
Plain radiographs were available for review. At minimum follow-up of 2.1 years, the Hartshill horseshoe cage was well seated. The patients who did not improve or were worse after the operation underwent a technetium radioisotope bone scan and flexion-extension radiographs for evidence of pseudarthrosis. MRI and computed tomographic (CT) scans were used in the early part of the study to delineate fusion and graft status, but the signal artefacts obscured the fusion site. There was no abnormal mobility at the implant vertebral body interface and the bone scans were normal for the patients who had persistent post-operative symptoms. It is possible that a few of the bone grafts may not have fused in the patients who have shown clinical improvement. These patients did not have bone scan and flexion-extension radiographs, as they had shown clinical and statistically significant improvement. Therefore, the true fusion rate in our series is not known.
Discussion
Graf reported his initial results in 120 patients. According to his assessment, 80% were "positively satisfied" and 20% were "passable or mediocre". There was no objective assessment of the patients [8]. Grevitt et al. [10] reported on 50 consecutive patients with a minimum follow-up of 19 months, who had symptomatic degenerative disc disease. The pre-operative Oswestry score of 59% improved to 31%. Their clinical results were classified as "excellent" or "good" in 72% of patients, "fair" in 10%, "the same" in 16% and "worse" in 2%.
Graf recommended this procedure for instability associated with disc disease. Although we did not perform pre-operative stress radiographs to demonstrate overt instability, those patients who had grade 3 or 4 disc degeneration on MRI in our series probably had an element of instability [17].
Guigui and Chopin [11] evaluated the results of Graf ligamentoplasty in patients who underwent decompression after lumbar spinal stenosis. They studied 26 patients with a mean follow-up of 29 months. These patients had pre-operative and post-operative stress radiographs to measure the instability. The results were objectively scored. They found 27% of patients were unstable after the operation. They therefore concluded that soft system stabilization with neural decompression did not improve the results. In our study, we excluded patients who needed decompression, to decrease confounding variables. This was done to eliminate patients with radicular rather than discogenic problems. This made the two groups comparable in this aspect. Brechbuhler et al. [2] reported their results at a mean follow-up of 50 months. They recommended Graf ligamentoplasty for patients with no or only mild facet joint arthritis and minor disc degeneration. This was contrary to our findings. We found a 93% (Oswestry Index) improvement in our group of patients with moderate to severe disc degeneration, who had Graf ligaments.
There are many articles in the literature concerning anterior lumbar interbody fusion that estimate the results according to fusion rate and clinical success [1, 3, 13, 14, 15, 18, 21, 24, 25, 26, 28]. An improvement of 77.8% (Oswestry Index) for anterior lumbar interbody fusion supplemented with the Hartshill horseshoe cage is a better result than was achieved in several of the series reported in literature [1, 3, 15, 23, 25, 26, 27]. The clinical success rate in these studies was at best 74% subjective and 68% objective improvement. Harmon [13, 14] reported a 93% clinical success rate. However, his patients who underwent anterior fusion had acute disc prolapse. Our improved results are probably attributable to the immediate stabilisation achieved by the horseshoe cage. The cage also prevents the graft sinkage through the vertebral endplates, prevents graft extrusion, opens up the neural foramina and recreates the normal lordosis of the lumbar segment (Fig. 2).
The disadvantage of this cage is that, because it is made of titanium, it prevents radiographic assessment of fusion. Penta and Fraser [23] and Tiusanen et al. [27] have reported that pseudarthrosis did not affect their outcome. There were several patients who had pseudarthrosis but had clinical success in their series. This may suggest that fusion may not be as important as previously thought. It may be that, by regaining the disc height, the biomechanics of the facet joints and posterior ligaments is restored to near normal tension. A nonunion anteriorly will perhaps consist of firm fibrous union, probably 1 or 2 mm thick, which would allow very limited movement under a compressive load. Therefore, a nonunion anteriorly may still abolish disc space movement to a sufficient degree to relieve pain. This may explain the clinical success in the presence of pseudarthrosis. Penta and Fraser [23] also reported in their 10-year minimum follow-up that some of the patients who had pseudarthrosis at 2 years went on to a solid fusion later. This has also been observed by Leong et al. [19]. Therefore, with no clinical evidence of implant loosening in our series, one could hope for the pseudarthrosis rate to be lower with a long enough follow-up. The Hartshill horseshoe implant should fail eventually if there is pseudarthrosis, if the theory of a race between union and implant failure is true. However, we have not had a single failure so far. One can speculate that the horseshoe is subjected to compression forces and therefore may not fail as soon as the other implants that are fixed in tension. If that is the case then the implant may create a protected, conducive environment for a prolonged period for graft incorporation. Tiusanen et al. [27] and Stauffer and Coventry [26] have recommended anterior interbody fusion as a salvage procedure. Our results show that this procedure is a suitable primary procedure.
The patients who had Graf ligaments inserted did better than those who had ALIF with the cage, at a mean follow up of 30 months. Graf ligament keeps the lumbar segments mobile. Lumbar spine may not tolerate rigid fixation very well. This may be the reason that Graf ligaments have shown better outcome. Contrary to the recommendations of Brechbuhler et al. [2], we found that Graf ligaments were successful in alleviating the symptoms even in advanced stages of disc degeneration.
Our results have been somewhat better than those reported in other series [11, 12]. We were very cautious in the patient selection for our study. Patients with radicular pain were excluded. We used MRI and provocative discography in all our patients. Guigui and Chopin [11] had only three patients who underwent pre-operative MRI before Graf ligamentoplasty, and therefore the source of non-radicular pain was not known. This could perhaps be the reason of poor outcome in their series. In our study, patients with Graf ligamentoplasty did better than those reported by Hadlow et al. [12]. Their patients were not randomised into the two groups, but were given a choice of the operation. They also reported a higher incidence of depression with greater disability in the patients who received Graf stabilisation than those who received lumbar fusion. These could be confounding factors that could have led to a poor outcome in their series of patients who had Graf ligament stabilisation.
Gardner et al. [7] have reported that the prime indication for the Graf technique is mild to moderate degenerative disc disease that is highly symptomatic, with chronic back pain punctuated by acute and disabling episodes, which they called "the lumbar instability syndrome". They stated that Graf ligamentoplasty is generally not appropriate for advanced disc degeneration. Patients who had total loss of disc height and greater than 25% subluxation were excluded from the study. Perhaps we would define such degenerative changes as too advanced for soft tissue stabilisation. This was important, because we wanted to define the true role of Graf ligament stabilisation in low back surgery. We were somewhat surprised that some patients whose disc degeneration would perhaps be classified as "severe" by others [7] did well with stabilisation. There is perhaps a time when the instability becomes too advanced, and the collapse of the disc space so severe that the facet joints and the posterior spinal ligaments and muscles decompensate to such an extent that any soft system stabilisation would fail. We think that with the present investigation protocol, this stage is difficult to define. Perhaps we were lucky to have caught a few of those patients with severe disc degeneration who were not totally decompensated. The precise stage and extent of symptomatic disc degeneration that would not benefit from soft system stabilisation is yet to be defined. Perhaps future research could shed more light on this difficult problem. All our patients underwent MRI and provocative discography to produce a typical pattern of concordant pain. This group of patients was not severely depressed or disabled, nor did it have chronic behaviour pattern, which can often affect outcome in low back surgery.
Our results are short term, and it would be interesting to know whether this advantage is maintained at a mean follow-up of 5 years. With the caveat that the number of patients is small and the follow-up short, this study shows that stabilisation by Graf ligaments could have advantages over lumbar fusion. Therefore, it will be interesting to observe this cohort of patients in future.
Thus, one may recommend the Graf ligamentoplasty procedure over ALIF with Hartshill horseshoe cage for degenerative disc disease. It is a worthwhile procedure for disc degeneration in the short term.
References
- 1.Blumenthal SL (1988) The role of anterior lumbar fusion for internal disc disruption. Spine 13:566–569 [DOI] [PubMed]
- 2.Brechbuhler D, Markwalder TM, Braun M (1998) Surgical results after soft system stabilization of the lumbar spine in degenerative disc disease – long-term results. Acta Neurochir (Wien) 140:521–525 [DOI] [PubMed]
- 3.Calandruccio RA, Benton BF (1964) Anterior lumbar fusion. Clin Orthop 35:63–68 [PubMed]
- 4.Deyo RA, Battie M, Beurskens AJHM, et al (1998) Outcome measures for low back pain research. Spine 23:2003–2013 [DOI] [PubMed]
- 5.Fairbank JCT, Couper J, Davies JB, O'Brien JP (1980) The Oswestry low back pain disability questionnaire. Physiotherapy 66:271–273 [PubMed]
- 6.Flynn JC, Hoque MA (1979) Anterior fusion of the lumbar spine. J Bone Joint Surg Am 61:1143–1150 [PubMed]
- 7.Gardner A, Declerck G, Hardcastle P, Markwalder T-M, Moon M-S, Salanova C, Shim Y-S (2000) Letters to the editor. Spine 25:273–276 [DOI] [PubMed]
- 8.Graf H (1992) Lumbar instability. Surgical treatment without fusion. Rachis 412:123–137
- 9.Graf H (1990) Vertebral instability: stabilization without arthrodesis. Safir R Groups SEM (procedural manual)
- 10.Grevitt MP, Gardner AD, Spilsbury J, et al (1995) The Graf stabilization system: early results in 50 patients. Eur Spine J 4:169–175 [DOI] [PubMed]
- 11.Guigui P, Chopin D (1994) Assessment of the use of the Graf ligamentoplasty in the surgical treatment of lumbar spinal stenosis. Apropos of a series of 26 patients. Rev Chir Orthop Reparatrice Appar Mot 80:681–688 [PubMed]
- 12.Hadlow SV, Fagan AB, Hillier TM, Fraser RD (1998) The Graf ligamentoplasty procedure. Spine 23:1172–1179 [DOI] [PubMed]
- 13.Harmon PH (1960) Anterior extraperitoneal lumbar disc excision and vertebral body fusion. Clin Orthop 18:169–184
- 14.Harmon PH (1963) Anterior disc excision and fusion of the lumbar vertebral bodies. J Int Coll Surg 40:572–586 [PubMed]
- 15.Inoue S, Watanabe T (1984) Anterior discectomy and interbody fusion for lumbar disc herniation. Clin Orthop 183:22–31 [PubMed]
- 16.Kirkaldy-Willis WH (1983) Managing low back pain. Churchill Livingstone, New York
- 17.Kirkaldy-Willis WH, Hill RJ (1979) A more precise diagnosis for low back pain. Spine 4:102 [DOI] [PubMed]
- 18.Lane JD, Moore ES (1948) Transperitoneal approach to the intervertebral disc in the lumbar area. Ann Surg 127:537–551 [DOI] [PMC free article] [PubMed]
- 19.Leong JCY, Chuhn SY, Grange WJ, Fang D (1983) Long-term results of lumbar intervertebral disc prolapse. Spine 8:793–799 [DOI] [PubMed]
- 20.Main CJ (1983) The Multiple Somatic Perception Questionnaire (MSPQ). J Psychosom Res 27:503–514 [DOI] [PubMed]
- 21.Newman MH, Grinstead GL (1992) Anterior lumbar interbody fusion for internal disc disruption. Spine 17:831–833 [DOI] [PubMed]
- 22.Paajanen H, Erkintalo M, Kuusela T, Dahlstrom S, Kormano M (1983) Magnetic resonance study of disc degeneration in young low back pain patients. Spine 14:982–985 [DOI] [PubMed]
- 23.Penta M, Fraser RD (1997) Anterior lumbar interbody fusion. A minimum 10-year follow-up. Spine 22:2429–2434 [DOI] [PubMed]
- 24.Sacks S (1965) Anterior interbody fusion of the lumbar spine. J Bone Joint Surg Br 47:211–223 [PubMed]
- 25.Sorensen KH (1978) Anterior interbody lumbar spine fusion for incapacitating disc degeneration and spondylolisthesis. Acta Orthop Scand 49:269–277 [DOI] [PubMed]
- 26.Stauffer RN, Coventry MB (1972) Anterior interbody lumbar fusion: analysis of Mayo Clinic series. J Bone Joint Surg Am 54:756–768 [PubMed]
- 27.Tiusanen H, Seitsalo S, Osterman K, Soini J (1996) Anterior interbody lumbar fusion in severe low back pain. Clin Orthop 324:153–163 [DOI] [PubMed]
- 28.Turner JA, Ersek M, Herron L, et al (1992) Patient outcomes after lumbar spinal fusion. JAMA 268:907–911 [PubMed]
- 29.Zung WWK (1965) A self-rating depression scale. Arch Gen Psychiatry 12:63–70 [DOI] [PubMed]


