Abstract
Background:
One method used to disinfect a dental cast is immersion in a disinfecting solution. Repeated immersion of a cast in disinfectant may affect its physical properties.
Purpose:
The purpose of this study was to evaluate the changes in dimensional accuracy and hardness of the dental casts as a result of repeated disinfection in 0.525% sodium hypochlorite and 2% glutaraldehyde solutions.
Materials and Methods:
Sixty specimens were made of type III dental stone. Twenty specimens were immersed in slurry, a supernatant solution of calcium sulfate in distilled water (control casts), 20 specimens in 0.525% sodium hypochlorite, and 20 specimens in 2% glutaraldehyde solutions for 30 min and air dried for 24 h. This process was repeated for 7 times for testing. Linear dimensional change and hardness were determined according to American National Standards Institute/American Dental Association (ANSI/ADA) standards. The data were analyzed using two-way analysis of variance.
Results:
For specimens prepared with type III stones, treatment was by immersion in slurry (group I – control casts), and by immersion in 0.525% sodium hypochlorite (group II – test group 1) and in 2% glutaraldehyde solution (group III – test group 2). The specimens treated with sodium hypochlorite and glutaraldehyde showed more linear dimensional change compared to the specimens treated in slurry. However, the difference between test casts and control casts was significant. But the difference between the two test groups was not significant. Both the test groups showed decrease in hardness of the specimens compared to that specimens in control group. But the difference between two test groups was not significant in hardness. However,the values remained close to ANSI/ADA standards.
Conclusion:
The results demonstrated that repeated immersion of type III dental stone specimens in slurry with distilled water, 0.525% sodium hypochlorite and 2% glutaraldehyde, along with drying in air, caused a significant increase in linear dimension and a significant decrease in hardness.
KEY WORDS: Disinfectant, hardness, linear dimensional change, slurry
The oral environment harbors a large number of microorganisms in the saliva and blood that may contain infectious microbes. While the majority of these organisms pose no significant risk to dental professionals, a number of them cause infectious diseases that may be incurable, such as those caused by the hepatitis C virus and human immunodeficiency virus (HIV). The prevalence of these diseases and their potentially harmful effects mandate adherence to infection control procedures in the dental office and laboratory.[1]
A number of bacteria, fungi, and viruses present in the dental environment have been linked to debilitating and life-threatening diseases. Every effort, therefore, must be made to avoid cross-contamination of these microorganisms and to prevent the potential transfer of disease in the dental setting. The establishment and maintenance of comprehensive and effective infection control programs are a requirement for the dental office as well as the dental laboratory. These programs must be monitored regularly and examined to ensure that they are consistent with the standards of the time.[2]
Dental office personnel may not follow the recommended protocols for disinfecting impressions and other items that come in contact with a patient. Powell et al.[3] found that 67% of items sampled that were sent to laboratories showed the presence of numerous microorganisms, such as Enterobacter cloacae, Escherichia coli, and Klebsiella oxytoca, among others. The studies by Ralph L. Leung and Steven E. Schonfeld[4] have demonstrated that microorganisms are transferred from contaminated impressions to the surface of the cast and could be measured. American Dental Association (ADA) and the Centers for Disease Control and Prevention have suggested methods for the disinfection of dental casts, including immersion in or spraying with a disinfectant. It is important that these materials have no effect on dimensional accuracy. Other methods for decontamination of the casts include incorporating chemicals into gypsum at the time of mixing or using die stone containing disinfectant. However, these methods have been reported to affect mechanical properties such as setting time, compressive strength, and dimensional accuracy. Ivanovski et al.[5] found 2% glutaraldehyde to be the most effective disinfectant with the least adverse effects on the physical properties of a cast.
The ADA Council[2] revised its guidelines to incorporate immersion disinfections. The guidelines recommended chemical agents that are effective against virus, spores, and bacterial microorganisms. These agents include formaldehyde, chlorine compounds, glutaraldehyde, phenols, and iodophors. Immersion in sodium hypochlorite for 10 min at a concentration of 1:10 dilution (0.525%) is recommended for immersion disinfection.
It is important that disinfectant solutions should be not only effective as antimicrobial agents, but also should not degrade the physical properties of the gypsum casts. Studies have shown that sodium hypochlorite is an effective disinfectant against both bacteria and virus, including HIV and hepatitis B, requiring less than 30 min immersion. Another advantage of using sodium hypochlorite solution is its low cost. However, because of its poor stability over a period of time, the solution must be made fresh daily to ensure its efficacy.
The potential for cross contamination with stone casts is especially present in Prosthodontics because of multiple opportunities for the transfer of infectious agents from blood and saliva to the casts through impressions, record bases, occlusion rims, and trial dentures. According to Stern et al.,[6] it may be necessary to disinfect the definitive cast at least 7 times (60 min each) with either iodophor or phenol disinfectants from the time of fabrication through insertion of complete or removable partial prostheses.
The immersion of a completely set dental stone cast in water decreases the compressive and tensile strengths. The effect of the process of immersing a cast 7 times in sodium hypochlorite with slurry and drying for disinfection on its physical properties has not been studied and reported. The purpose of this study was to evaluate the dimensional stability and hardness of gypsum casts after repeated immersion disinfectants like sodium hypochlorite and glutaraldehyde.
Materials and Methods
Type III dental stone was subjected to repeated immersion in slurry and with two different disinfectant solutions, namely, 0.525% sodium hypochlorite and 2% glutaraldehyde.
Preparation of gypsum specimens
Three different test configurations were used. A master metal die was used to make a specimen which has a highly polished surface approximately 15 mm in diameter, on which were inscribed two parallel lines for the determination of dimensional stability. A collar was fabricated in metal for the test die to fit into. A space of 5 mm was provided between the test die and the collar for the elastomeric impression material. The impression was made with polyvinyl siloxane impression material.
Prior to fabricating each specimen, the surface of the master metal die was rinsed with distilled water and dried. Impression of test die was made in metal collar by placing polyvinyl siloxane material in the collar. Dental stone was mixed according to manufacturer's instructions. It was spatulated for 30 sec and added to the impression in small increments, placed on a mechanical vibrator to prevent formation of air bubbles. The cylindrical specimens were allowed to set for 1 h at ambient room temperature of 20°C ± 2°C. Similarly, 60 specimens were produced.
Disinfectant solution preparation
Three different solutions were tested for their effect on the dimensional accuracy and hardness of cylindrical test specimens:
Control solution 1: Slurry, a supernatant solution of calcium sulfate in distilled water
Test solution 1: Sodium hypochlorite (0.525%)
Test solution 2: Glutaraldehyde (2%).
Slurry was prepared by placing clean, completely set dental stone pieces in a plastic container of distilled water and allowing them to soak for 48 h. The resultant supernatant solution was stored at room temperature and was used for soaking the test cylindrical specimens.[7] The second solution was sodium hypochlorite diluted to 0.525% concentration with distilled water, which was made fresh daily to ensure efficacy. The third solution used was 2% glutaraldehyde. An immersion bath of 500 ml for disinfection of cylindrical specimens was established.
Twenty cylindrical specimens of type III dental stone were immersed in each of the three solutions:
Group I – (control) slurry,
Group II – 0.525% sodium hypochlorite, and
Group III – 2% glutaraldehyde.
Immersion was done for 30 min at room temperature. After immersion, all cylindrical specimens were removed from their respective baths and allowed to dry for 24 h at room temperature. The process of immersing and drying at room temperature conditions was repeated 7 times, and immersion bath solutions were replaced for each cycle. The sequence of 7 cycles was chosen as an average for the number of immersions in disinfectant solution necessary in the construction of complete and partial removable prostheses.[6] The accuracy of linear dimensions of stone cylindrical specimens was examined and evaluated according to the ADA specification No. 19.
Dimensional change of cylindrical specimens after immersion
After each immersion and drying cycles for 7 times for consecutive days, the distance between the parallel lines of each cast was measured under traveling microscope at angle illumination at ×10 magnification, and the mean of seven readings was taken as the final reading. The difference of the linear measurement of each corresponding cast before and after immersion and drying represented the dimensional change caused by the process of immersion in slurry, with sodium hypochlorite and glutaraldehyde solutions and drying.
Hardness
The Rockwell hardness testing machine, designed to measure hardness, has a stainless steel ball indenter with two-stage application. Stage one involves lowering a weight of 10 kg and stage two involves a weight of 60 kg. The gypsum specimens, after repeated immersion in disinfectant solution, were placed on the Rockwell platform and the head of the instrument was lowered until indenter just touched the surface of the specimen. The minor load was then applied. The dial gauge was set to zero reading. The secondary load was applied for a period of 1 min to give a hardness reading. Thus, a total of 60 readings were made for specimens in three groups.
Results
In the results, the mean measurement of the specimens measured and the standard deviation (SD) of measurements obtained after comparing the measurements of the specimens with the control groups and the mean hardness and SD of measurements obtained after comparing the measurements of the specimens with the control groups were illustrated and tabulated.
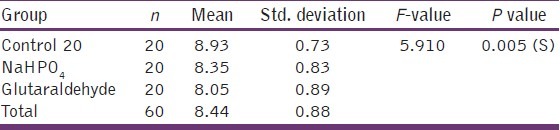
Table 1 represents the mean (in mm) of dimensional change and SD of the three groups. Table 2 represents the mean (in number) of hardness and SD of the three groups. Graph 1 represents the mean (in mm) of dimensional change and SD of the three groups. Graph 2 represents the mean (in number) of hardness and SD of the three groups.
Table 1.
Comparison of mean values of linear dimensional change among the three groups
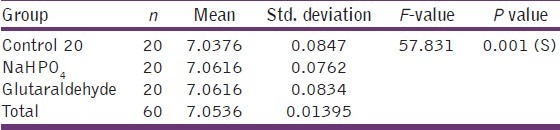
Table 2.
Comparison of mean values of hardness among the three groups
Graph 1.
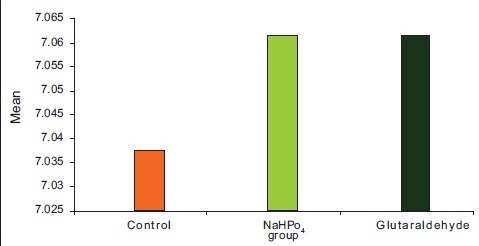
Comparison of mean values of linear dimensional change among the three groups
Graph 2.
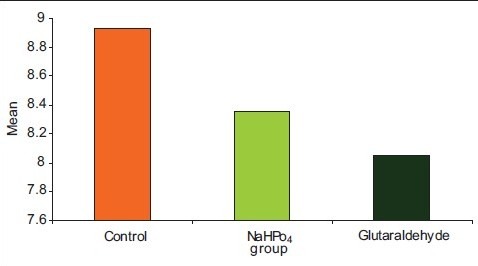
Comparison of mean values of hardness among the three groups
One-way analysis of variance (ANOVA) and SD showed significant increase in linear dimensional change in group II and group III compared to group I. But there was no significant difference between group II and group III. In case of hardness, there was significant decrease in group II and group III compared to group I. But there was no significant difference between group II and group III.
Discussion
In Prosthodontics, objects potentially contaminated with pathogenic microorganisms are transported between dental laboratory and dental clinic.[2] It has been claimed that to avoid cross contamination, specific disinfection measures should be followed. In the literature, the usual solution to this problem has been to chemically disinfect the impressions and casts and the efficacy of such disinfectants has been the subject of several studies.
The need for an infection control program is felt because a number of bacteria, fungi, and viruses present in the dental environment have been linked to debilitating and life-threatening diseases. Every effort, therefore, must be made to avoid cross contamination of these microorganisms and to prevent the potential transfer of disease in the dental setting. One common dental procedure that may cause cross contamination, especially between patients and dental laboratory personnel, is transfer of infectious agents from blood and saliva to the casts through impressions, record bases, occlusion rims, and trial dentures.
Some reports showed that certain microorganisms could be recovered from a gypsum cast when it is poured against a contaminated impression.[8] Several approaches to the sterilization and disinfection of either impressions or gypsum casts have been attempted, and most of them were microbiologically effective; however, some alterations in the physical properties of the materials were also detected.[9] An alternative method of using chemical disinfectant solutions as mixing-water substitutes was suggested. Others[10,11] used both gum arabic and calcium hydroxide additives to modify the hemihydrate powder before mixing with aqueous solutions of chemical disinfectants, and the results showed an improvement of strength and hardness of the resultant disinfected materials without affecting other surface properties.
Microwave radiation in dentistry has been widely accepted for sterilizing, polymerizing acrylic resins, removing wax from molds, shortening the dough stage of denture base acrylic resins, and for drying various kinds of gypsum products.[12] The study by Berg et al.[13] determined how effective is microwave oven irradiation than chemical disinfection.
According to Stern et al.,[6] casts should be disinfected at least 7 times (60 min each) with either iodophor or phenol disinfectants from the time of fabrication through insertion of complete or removable partial prostheses. The effect of the process of immersing a cast 7 times in sodium hypochlorite with slurry and drying for disinfection on its physical properties has not been studied and reported.
Polyvinyl siloxane impression material was used as it has excellent physical properties like unsurpassed accuracy. It can record fine details with best elastic recovery of all the available impression materials.[14] Because there is virtually no by-product formed in the polymerization reaction, there materials are dimensionally stable and can be poured at the convenience of the operator and also allow to make a second pour.
Dental gypsum products are the most widely used among other cast and die materials[15,16] because of ease of manipulation, reasonable properties (reproduction of details, hardness, compatibility with different impression materials, and acceptable compressive strength and accuracy),[17] and lower cost.[18]
Several studies found that glutaraldehyde and sodium hypochlorite disinfectants had least adverse effects on the physical properties of the casts. Ivanovski et al.[5] found 2% glutaraldehyde to be the most effective disinfectant with the least adverse effects on the physical properties of a cast. Breault et al.[19] reported that the addition of a 5.25% solution of sodium hypochlorite actually increases the compressive strength of gypsum and decreases the setting time, but leaves other physical properties unchanged. Immersion disinfection was used because reports describe using different chemical disinfectants for spray and immersion disinfection for both impressions and casts.
The casts were examined under low-angle light, at ×10 magnification, with stereo zoom microscope for the entirety of the parallel lines. The Rockwell hardness micro-indenter machine is designed to measure hardness.
In this study, gypsum specimens disinfected with sodium hypochlorite and glutaraldehyde showed more mean dimensional change (7.0616) compared to slurry (7.0376) [Table 1]. The findings of the present study could not be directly compared with previous studies because specimens were immersed only once for a period ranging from 10 to 60 min.[20] The findings of this study are in general agreement with previous studies.[6] There was no significant difference in dimensional change between gypsum products immersed in sodium hypochlorite and glutaraldehyde and change was due to interaction between the solution and dental stone.[21]
Gypsum specimens disinfected with sodium hypochlorite and glutaraldehyde showed less mean hardness (8.35 and 8.05, respectively) compared to slurry (8.93) [Table 2]. The findings of this study are in general agreement with those of a previous study by Syed Mohammed et al.[22] The decreased hardness in gypsum specimens immersed in disinfectant solutions may have been a result of a reaction between disinfectant and stone. The disinfectant did not visibly roughen the impression, but a film of disinfectant could be felt on the material even after thorough rinsing with water. This concentrated residual disinfectant may have reacted with gypsum to produce decreased hardness.[23]
Conclusions
An in vitro study was done to evaluate the changes in dimensional accuracy and hardness of the dental casts as a result of repeated disinfection in 0.525% sodium hypochlorite and 2% glutaraldehyde solutions.
The following conclusions were drawn from the present study:
Stone casts immersed in 0.525% sodium hypochlorite and 2% glutaraldehyde solutions showed significant linear dimensional change compared to stone casts in slurry.
Stone casts immersed in 0.525% sodium hypochlorite and 2% glutaraldehyde solutions showed no significant difference in dimensional accuracy.
Stone casts immersed in 0.525% sodium hypochlorite and 2% glutaraldehyde solutions showed significant reduction in hardness compared to stone casts in slurry.
Stone casts immersed in 0.525% sodium hypochlorite and 2% glutaraldehyde solutions showed no significant difference in hardness.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Twomey JO, Abdelaziz KM, Combe EC, Anderson DL. Calcium hypochlorite as a disinfecting additive for dental stone. J Prosthet Dent. 2003;90:282–8. doi: 10.1016/s0022-3913(03)00412-8. [DOI] [PubMed] [Google Scholar]
- 2.Patrick Naylor W. Infection control in fixed prosthodontics. Dent Clin N Am. 1992;36:809–31. [PubMed] [Google Scholar]
- 3.Lynn Powell G, Runnells RD, Saxon BA, Whisenant BK. The presence and identification of organisms transmitted to dental laboratories. J Prosthet Dent. 1990;64:235–7. doi: 10.1016/0022-3913(90)90185-f. [DOI] [PubMed] [Google Scholar]
- 4.Leung RL, Schonfeld SE. Gypsum casts as a potential source of microbial cross-combination. J Prosthet Dent. 1983;49:210–2. doi: 10.1016/0022-3913(83)90503-6. [DOI] [PubMed] [Google Scholar]
- 5.Ivanoski S, Savage NW, Brockhurst PJ, Bird PS. Disinfection of dental stone casts: Antimicrobial effects and physical property alterations. Dent Mater. 1995;11:19–23. doi: 10.1016/0109-5641(95)80004-2. [DOI] [PubMed] [Google Scholar]
- 6.Stern MA, Johnson GEL, Toolson HB. An evaluation of dental stones after repeated exposure to spray disinfectants. Part I: Abrasion and compressive strength. J Prosthet Dent. 1991;65:713–8. doi: 10.1016/0022-3913(91)90211-e. [DOI] [PubMed] [Google Scholar]
- 7.Morrow RM, Rudd KD, Rhoads JE, editors. Dental Laboratory procedures: Complete dentures. 2nd ed. Vol. 1. St. Louis: Mosby; 1986. p. 104. [Google Scholar]
- 8.Savage NW, Brockhurst PJ, Bird PS. Disinfection of dental stone casts: Antimicrobial effects and physical property alterations. Dent Mater. 1995;11:19–23. doi: 10.1016/0109-5641(95)80004-2. [DOI] [PubMed] [Google Scholar]
- 9.Holtan JR, Olin PS, Rudney JD. Dimensional stability of polyvinylsiloxane impression material following ethylene oxide and steam autoclave sterilization. J Prosthet Dent. 1991;65:519–25. doi: 10.1016/0022-3913(91)90292-5. [DOI] [PubMed] [Google Scholar]
- 10.Abdelaziz KM, Combe EC, Hodges JS. The effect of disinfectants on the properties of dental gypsum: 1.Mechanical properties. J Prosthodont. 2002;11:161–7. [PubMed] [Google Scholar]
- 11.Abdelaziz KM, Combe EC, Hodges JS. The effect of disinfectants on the properties of dental gypsum, part 2: Surface properties. J Prosthodont. 2002;11:234–40. doi: 10.1053/jpro.2002.129049. [DOI] [PubMed] [Google Scholar]
- 12.Tuncer N, Tufekcioglu HB, Calikkocaoglu S. Investigation on the compressive strength of several gypsum products dried by microwave oven with different programs. J Prosthet Dent. 1993;69:333–9. doi: 10.1016/0022-3913(93)90116-6. [DOI] [PubMed] [Google Scholar]
- 13.Berg E, Nielsen O, Skaug N. High-level microwave disinfection of dental gypsum casts. Int J Prosthodont. 2005;18:520–5. [PubMed] [Google Scholar]
- 14.Idris B, Houston F, Claffey N. Comparison of dimensional accuracy of one-and two-step techniques with the use of putty/wash addition silicone impression materials. J Prosthet Dent. 1995;74:535–41. doi: 10.1016/s0022-3913(05)80358-0. [DOI] [PubMed] [Google Scholar]
- 15.Anusavice KJ, editor. Phillips: Science of dental materials. 10th ed. St. Louis: Elsevier; 1996. p. 85. [Google Scholar]
- 16.Anusavice KJ, editor. Phillips: Science of dental materials. 11th ed. St. Louis: Elsevier; 1996. p. 85. [Google Scholar]
- 17.Craig RG, Powers JM, Wataha JC, editors. Dental materials: Properties and manipulation. 7th ed. St. Louis: Elsevier; 1999. p. 185. [Google Scholar]
- 18.Rosenstiel SF, Fujimoto J, Land M, editors. Contemporary fixed prosthodontics. 3rd ed. St. Louis: Elsevier; 2000. p. 431. [Google Scholar]
- 19.Breault LG. Die stone disinfection: Incorporation of sodium hypochlorite. J Prosthodont. 1998;7:13–6. doi: 10.1111/j.1532-849x.1998.tb00170.x. [DOI] [PubMed] [Google Scholar]
- 20.Bass RA, Plummer KD, Anderson EF. The effect of surface disinfectant on a dental cast. J Prosthet Dent. 1992;67:723–5. doi: 10.1016/0022-3913(92)90179-e. [DOI] [PubMed] [Google Scholar]
- 21.Abdullah MA. Surface detail, compressive strength, and dimensional accuracy of gypsum casts after repeated immersion in hypochlorite solution. J Prosthet Dent. 2006;95:462–8. doi: 10.1016/j.prosdent.2006.03.019. [DOI] [PubMed] [Google Scholar]
- 22.Hussain SM, Tredwin CJ, Nesbit M, Moles DR. The effect of disinfection on iireversible hydrocolloid and type III gypsum casts. J Prosthodont Restor Dent. 2006;11:52–4. [PubMed] [Google Scholar]
- 23.Vandewalie KS, Charlton DG, Schwartz RS, Reagan SE, Koeppen RG. Immersion disinfection of irreversible hydrocolloid impressions with sodium hypochlorite. Part II: Effect on gypsum. Int J Prosthodont. 1994;7:315–22. [PubMed] [Google Scholar]


