Abstract
Pyogenic granuloma is tumor-like proliferation to a nonspecific infection. Clinically, pyogenic granuloma presents as sessile or pedunculated exophytic mass with a smooth or lobulated surface which has a tendency to bleed easily. These lesions tend to occur slightly more in females, frequently involving the gingiva of the maxillary region. Histologically, these lesions show an excessive proliferation of vascular type of connective tissue to a nonspecific infection. The most common treatment is surgical excision with eradication of local irritants. This case report describes a pyogenic granuloma on the labial mucosa in a 33-year-old male, discussing the clinical features and histopathologic features that distinguish this lesion from other similar oral mucosa lesions.
KEY WORDS: Lobular capillary hemangioma, pregnancy tumor, pyogenic granuloma
Pyogenic granuloma is one of the most common benign tumors like proliferations affecting the oral cavity.[1] Several authors consider pyogenic granuloma as an inflammatory hyperplasia that ulcerates. Ulceration can occur mostly because of trauma during mastication, following which the lesion becomes contaminated by the oral flora and liquids; as a result, an acute inflammatory response occurs.[2]
Pyogenic granuloma is a misnomer as the lesion is not associated with pus formation and histologically the lesion is composed of granulation tissue. Clinically, the lesion showed necrotic white material which resembled pus, thus impelled clinicians to refer to these lesions as pyogenic granuloma. Several authors preferred to term this entity as lobular capillary hemangioma based on the histological appearance.
Pyogenic granulomas typically occur on the mucosal surfaces, particularly the mouth and the skin.[3,4] These lesions may be seen at any age and tend to occur more commonly in females than in males.[1] Pyogenic granulomas are commonly seen on the gingiva, particularly the anterior segment,[2] where they are presumably caused by calculus or foreign material within the gingival crevice. Hormonal changes of puberty and pregnancy may modify the gingival reparative response to injury, producing what was once called a “pregnancy tumor.” Under these circumstances, multiple gingival lesions or generalized gingival hyperplasia may be seen. The lesions usually appear in the second and third trimesters of pregnancy, most of which resolve soon after delivery.[5]
Pyogenic granulomas are uncommonly seen elsewhere in the mouth, but may appear in areas of frequent trauma, such as the upper[6] and lower lip, buccal mucosa, tongue,[1] and alveolar mucosa in edentulous regions.[2] Pyogenic granulomas occurring on the skin commonly involve the hands, forearms, and face, and may occur at any age, but are most often seen in children and are thought to be caused by minor trauma.[2]
Clinically, pyogenic granulomas begin as small, red papules that rapidly increase in size ranging from a few millimeters to several centimeters. However, they rarely extend to more than 4 cm in diameter. Few cases have even caused displacement of teeth resulting in malcclusion.[7] These lesions can also present as asymptomatic, pedunculated, raspberry-like nodules, which on passage of time become ulcerated due to secondary trauma. Initially, the lesions may be covered by yellow, fibrous membrane or by epithelium of variable thickness. The lesions are delicate and minor trauma may cause considerable bleeding. Pyogenic granulomas may have an initial period of rapid growth, followed by stabilization and occasionally regression.
Radiographic investigations of pyogenic granuloma do not exhibit any distinct diagnostic feature as the lesion arises from the soft tissue, but can aid in ruling out any other lesions clinically mimicking pyogenic granuloma. Review of literature shows rare cases of pyogenic granuloma, which have been reported to cause bone loss but no resorption of the root of the teeth in the affected region.[8,9]
Histologically, pyogenic granulomas are exophytic masses usually covered by fibropurulent membrane. Surface of these lesions at times may be covered by an atrophic to proliferating keratinized epithelium.[7] The lesions show a connective tissue with distinct lobular arrangement with central larger vessels and aggregates of well-formed capillaries seen in the periphery. Clusters of polymorphonuclear leukocytes are present in some areas of the granulation tissue, especially areas adjacent to the necrotic or ulcerated surface. Neutrophils are present in the superficial zone of ulcerated pyogenic granulomas.[2] Necrosis may be seen in association with surface ulceration. The stroma of younger lesions is edematous with active fibroblasts, but advanced lesions undergo considerable fibrosis with few and mature fibroblasts. Immunohistochemistry shows that pyogenic granulomas express typical endothelial markers such as CD31.[3]
Clinically, the differential diagnosis includes lesions with similar appearance such as peripheral giant cell granuloma, peripheral odontogenic or ossifying fibroma, vascular lesions such as hemangioma, and rarely metastatic carcinomas.
Due to its high cellularity and frequent mitotic activity, pyogenic granuloma may rarely suggest the possibility of angiosarcoma, as pyogenic granulomas are circumscribed and display a lobular growth pattern, features inconsistent with angiosarcoma. Other differentials including Kaposi sarcoma can be ruled out as deeper zones show formation of slit-like vascular spaces lined with hyperchromatic spindled cells exhibiting varying degrees of infiltration. Similar histopathology of vascular proliferations can be seen in any neoplasm and it is important that doubtful areas need to be sampled to rule out any other tumors.[3]
Case Report
A 33-year-old male patient reported with chief complaint of a growth on the lower lip since 15 days. The growth was initially small when the patient had first noticed it, but had grown rapidly to attain the present size.
Clinical examination revealed a well-defined, solitary, pedunculated mass on the lower labial mucosa, facing the incisal margins of lower anteriors. The growth was irregular in shape and measured around 3×2 cm. The surface of the growth was pale white with areas of erythema. On palpation, the growth was firm in consistency, non-tender, and showed minimal bleeding [Figure 1].
Figure 1.

Solitary, pedunculated mass around 3×2 cms seen on the lower labial mucosa
Hard tissue examination revealed generalized attrition which was marked in the lower anteriors. Also observed was crowding of lower anteriors causing lingual displacement of 32 and 42. Generalized hard and soft deposits along with stains were also seen particularly in relation to the lower anteriors, indicating a poor oral hygiene.
Based on the history and clinical examination, a provisional diagnosis of pyogenic granuloma was made and the growth was excised under local anesthesia. Histopathologic examination revealed a granulation tissue with proliferation of endothelial cells forming budding capillaries which contained erythrocytes, observed toward the center of the tissue. Surface of the growth was devoid of epithelium and was covered by a fibropurulent membrane. The connective tissue comprised delicate collagenous fibers with infiltration of acute and chronic inflammatory cells, chiefly neutrophils and lymphocytes. These findings were consistent with a histopathologic diagnosis of pyogenic granuloma [Figures 2 and 3].
Figure 2.
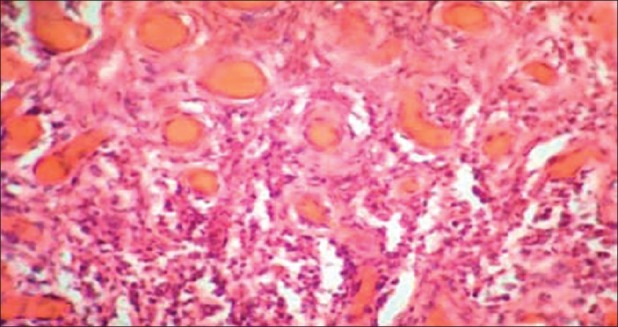
Low-power view showing ulcerated surface with connective comprising numerous proliferating blood vessels with chronic inflammatory cells (H and E, ×10)
Figure 3.
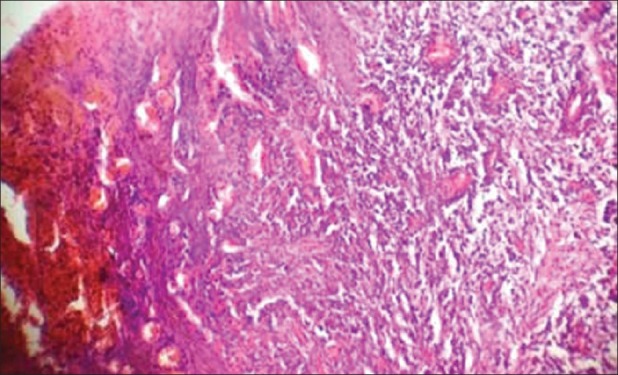
High-power view showing blood vessels lined by endothelial cells, filled with RBC, proliferating into the connective tissue (H and E, ×40)
Discussion
Pyogenic granuloma of the oral cavity is a relatively common entity first described by Poncet and Dor in 1897 as “human botryomycosis.”[10] The name “pyogenic granuloma” was first given by Hartzell in 1904.[7] Pyogenic granulomas commonly occur in the gingiva (keratinized mucosa), often in the anterior segment of the maxillary jaw. Other sites in the head and neck occurring extragingivally in which the lesion tends to occur as a result of trauma include the buccal mucosa, the alveolar mucosa of edentulous ridge, the palate, and the lower lip, which are very rare. The floor of the mouth has not been reported as a site as the tongue provides protection against any traumatic injuries and also due to lack of sufficient connective tissue in the mucosa of this region.[10] In the present case, the consistent trauma inflicted by the sharp attrited edges of the lower incisors could have been the etiology behind the development of this lesion.
The reasons attributed to such connective proliferations vary from trauma to hormonal factors, which along with poor oral hygiene cause gingival irritation and inflammation and contribute to the development. A proper history and clinical examination can aid in the diagnosis of these lesions.
Clinically, the lesion typically appears as red to purple nodular growth depending upon the duration and vascularity of the lesion. The surface of the lesion can show areas of erythema or ulcerations, as was seen in the present case, which indicate impingement of the adjacent teeth during functions such as mastication or speech.
Although pyogenic granuloma can be diagnosed clinically, atypical presentations lead to inappropriate diagnosis and should be further investigated by biopsy to rule any other serious lesions. The histopathology of extragingival pyogenic granuloma is similar to that occurring in the gingiva, showing proliferating vascular core in connective tissue stroma with the presence of acute or chronic inflammatory infiltrates depending on the etiology and duration and of the lesion.[11]
Pyogenic granuloma is treated conservatively by surgical excision and must be followed with oral prophylaxis for lesions occurring on the gingiva. The most common etiology for extragingival lesions being trauma or consistent irritation should be treated. Other forms of treatment such as Nd: YAG laser, flash lamp pulsed dye laser, cryosurgery, intralesional injection of ethanol or corticosteroid, and sodium tetradecyl sulfate sclerotherapy have also been proposed. Recurrence rate is not infrequent which might be due to incomplete excision, failure to remove predisposing factors, or re-injury of the region. Lesions seen on the gingiva must be excised down to the underlying periosteum and etiologic factors must be eliminated in order to achieve a lower recurrence rate.[12,13]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Joseph AR, James JS, Richard CKJ. Oral Pathology, clinical and pathological corelations. 4th edition. Missouri: Saunders Elsevier; 2003. pp. 115–6. [Google Scholar]
- 2.Wood NK, Gauz PW. Differential diagnosis of oral and maxillofacial lesions. 5th edition. Missouri: Mosby Elsevier; 1997. pp. 138–9. [Google Scholar]
- 3.Gnepp DR. Sternberg's Diagnostic Surgical Pathology. 4th edition. Philadelphia: Lippincott Williams; 2004. pp. 183–4. [Google Scholar]
- 4.Disorders of soft tissue, Sternberg's Diagnostic Surgical Pathology. 4th Edition. 2004. pp. 183–184. [Google Scholar]
- 5.Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: A review. J Oral Sci. 2006;48:167–75. doi: 10.2334/josnusd.48.167. [DOI] [PubMed] [Google Scholar]
- 6.Gonçales ES, Damante JH, Fischer Rubira CM, Taveira LA. Pyogenic granuloma on the upper lip: An unusual location. J Appl Oral Sci. 2010;18:538–41. doi: 10.1590/S1678-77572010000500019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parikh K, Shah P, Shah M. Pyogenic Granuloma: A report of three cases. J Dent Sci. 2011;2:53–5. [Google Scholar]
- 8.Martins-Filho PR, Piva MR, Da Silva LC, Reinheimer DM, Santos TS. Aggressive pregnancy tumor (pyogenic granuloma) with extensive alveolar bone loss mimicking a malignant tumor: Case report and review of literature. Int J Morphol. 2011;29:164–7. [Google Scholar]
- 9.Singh VP, Nayak DG, Upoor AS. Pyogenic granuloma associated with bone loss: A case report. J Nepal Dent Assoc. 2009;10:137–9. [Google Scholar]
- 10.Akyol MU, Yalciner EG, Dogan AL. Pyogenic granuloma (lobular capillary hemangioma) of the tongue. Int J Pediatr Otorhinolaryngol. 2001;58:239–41. doi: 10.1016/s0165-5876(01)00425-6. [DOI] [PubMed] [Google Scholar]
- 11.Amirchaghmaghi M, Falaki F, Mohtasham N, Mozafari PM. Extragingival pyogenic granuloma: A case report. Cases J. 2008;1:371. doi: 10.1186/1757-1626-1-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mubeen K, Vijayalakshmi KR, Abhishek RP. Oral pyogenic granuloma with mandible involvement: An unusual presentation. J Dent Oral Hyg. 2011;3:6–9. [Google Scholar]
- 13.Saghafi S, Zare-Mahmoodabadi R, Danesh-Sani SA, Mahmoodi P, Esmaili M. Oral pyogenic granuloma: A retrospective analysis of 151 cases in an Iranian population. Int J Oral Maxillofac Pathol. 2011;2:3–6. [Google Scholar]


