Abstract
Progress in understanding the role of bone morphogenetic proteins (BMPs) in craniofacial and tooth development and the demonstration of stem cells in periodontal ligament have set the stage for periodontal regenerative therapy and tissue engineering. Furthermore, recent approval by the Food and Drug Administration of recombinant human BMPs for accelerating bone fusion in slow-healing fractures indicates that this protein family may prove useful in designing regenerative treatments in periodontics. In the near term, these advances are likely to be applied to periodontal surgery; ultimately, they may facilitate approaches to regenerating whole lost periodontal structures.
KEY WORDS: Periodontitis, periodontal regeneration, growth factors, glycoproteins, tissue engineering
Periodontitis, evoked by the bacterial biofilm (dental plaque) that forms around teeth, progressively destroys the periodontal tissue supporting the teeth, including the periodontal ligament, cementum, alveolar bone, and gingiva.[1] Ultimately, this chronic inflammatory disease can lead to loss of the affected teeth. All over the world, this disease remains highly prevalent and is considered to threaten quality of life for middle-aged and older populations as far as “oral” functions are concerned. Some success has been achieved in suppressing progression of periodontitis by mechanically removing bacterial biofilm.[2]
However, removal of the cause, bacterial plaque, with conventional periodontal and/or surgical treatments can, at best, reduce pocket depth and diminish inflammation in the affected region.[3] No such treatment can ever regenerate lost periodontal tissue or normal structure and functionality. Considering that the “mouth” and “teeth” have various esthetic and functional roles to play, establishing a brand new treatment that enables the regeneration and rebuilding of periodontal tissue once destroyed by periodontal disease represents a task of tremendous importance.
Historically, periodontal regeneration research has focused on the quest for a magic filler material. This search has led to the development of techniques utilizing autogenous bone, allografts, xenografts, and various manmade bone substitutes.[4] These techniques revealed limited success in periodontal regeneration. Because of this, the need for a more effective regenerative approach has been developed. This technique resulted in the development of procedures that utilize biological mediators and tissue engineering techniques.[5] Early experimental approaches with biological mediators consisting of growth factors and morphogens were encouraging. With the use of recombinant DNA technology, some of these growth factors and morphogens have been produced in adequate quantities for clinical application.[6] With their introduction, tissue engineering, a relatively new field of reconstructive biology that utilizes mechanical, cellular, and biologic mediators to facilitate reconstruction/regeneration of a particular tissue, is being introduced to dentistry.
Bone morphogenetic proteins (BMPs) are a group of regulatory glycoproteins that are members of the transforming growth factor-beta superfamily. These molecules primarily stimulate differentiation of mesenchymal stem cells into chondroblasts and osteoblasts.[7] At least seven BMPs have been isolated from bovine and human sources. In the field of periodontal regeneration, much of the research interest has focused on BMP-2 (OP-2), BMP-3 (osteogenin), and BMP-7 (OP-1).[8] This review focuses on the various components of BMPs and how they may contribute to the improvement in periodontal regenerative outcomes.
Three Key Elements for Regeneration
Tissue engineering offers a new option to supplement existing treatment regimens for periodontal diseases. Realizing the potential of regenerative treatments for the periodontal structure will require integration of three key elements: inductive morphogenetic signals (morphogens), responding progenitor/stem cells, and the extracellular matrix scaffold, as shown in Figure 1. To induce morphogenesis of the periodontium, these elements must be combined to facilitate a developmental cascade of pattern formation.[5]
Figure 1.
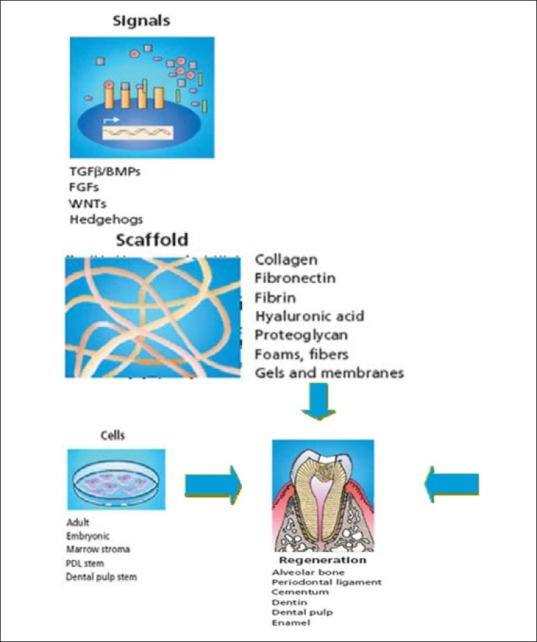
Schematic representation of signalling molecule cells and scaffolds that are used for periodontal regeneration
History
The name BMP was given in 1965 by Urist and colleagues to the active components in demineralizing bone and bone extracts, which are capable of inducing bone formation at ectopic sites (intramuscular). Reddy and Huggins (1972) found that bone extracts induce bone formation in ectopic sites (subcutaneous).[7] In 1988, the first BMPs were isolated and their cDNAs were cloned by Wozney et al.[7]
Structure and Classification
The human genome encodes 20 BMPs. BMPs are dimeric molecules critically dependent on the single intermolecular disulfide bond for biological activity. The monomeric subunit has about 120 amino acids, including seven conserved cysteine residues.[9]
The BMP family can be divided into four distinct subfamilies:
1 stgroup: BMP-2 and BMP-4
2 ndgroup: BMP-3, BMP-3B (growth differentiating factor 10 or GDF-10)
3 rdgroup: BMP-5, BMP-6, BMP-7, BMP-8
4 thgroup: GDF-5, GDF-6, GDF-7 (cartilage-derived morphogenetic protein 1, 2, 3)
BMP-1 is not a member of the BMP family, but rather a procollagen C proteinase enzyme involved in the proteolytic processing of soluble procollagen, leading to the self-assembly of insoluble collagen fibers in the extracellular matrix.
Functions of BMP
It regulates various mesenchymal/osteoblastic activities like the following:[8]
Chemotaxis
Anchorage-dependent cell attachment (fibronectin)
Cell replication (mitosis)
Differentiation of osteoblasts
Alkaline phosphatase activity
Osteocalcin synthesis/mineralization[10]
BMPs also play a critical role in tooth morphogenesis. BMPs 2, 4, and 7 are expressed in dental epithelium, and recombinant BMPs 2 and 4 can be used as a substitute for dental epithelium in inducing mesenchyme differentiation. BMP-3 and BMP-7 have been “immune” localized to developing periodontal ligament, cementum, and alveolar bone. On the other hand, BMP-2 was localized only in alveolar bone during root morphogenesis.[8] A role of BMP-3 in the cementoblast lineage has been suggested by its localization in the root-lining cells.
Receptor for BMPs
A comparison of other growth factors reveals that BMPs are (34-38%) related to the transforming growth factor beta (TGFβ) family. BMPs and TGFβ ligands have cognate BMP type I and II receptors and TGFβ type I and II receptors, respectively, which function as protein kinases[11] as shown in Figure 2.
Figure 2.
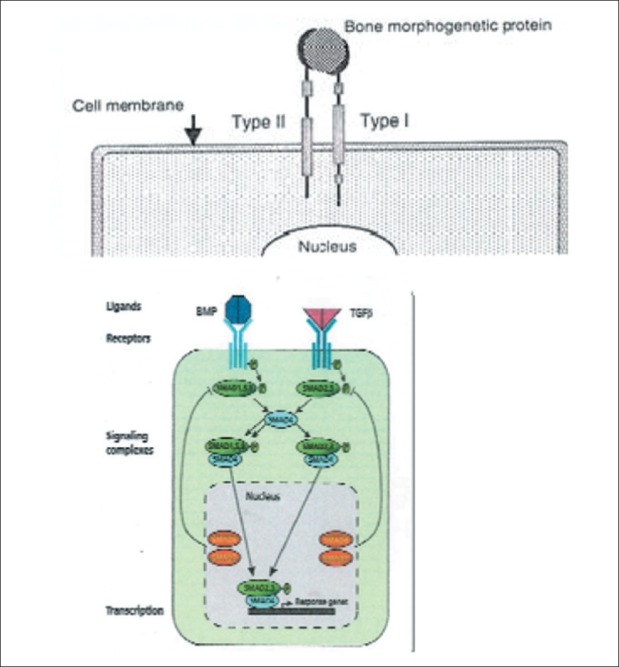
Cell surface receptors type I and II for BMPs
Mechanism of action[4]
The BMP type I receptor protein kinase phosphorylates intracellular signaling substances, Smads (a fusion of the Sma gene in Caenorhabditis. elegans and Mad gene in Drosophila) 1, 5, and 8. The TGFβ type I receptor kinase specifically phosphorylates Smads 2 and 3. The phosphorylated Smads 1, 5, and 8 (BMP-signaling Smads) and Smads 2 and 3 (TGFβ-signaling Smads) partner with Smads 4 to form signaling complexes in the cytosol that enter the nucleus to initiate the transcription of downstream targets. Although BMPs and TGFβ ligands signal via distinct receptors, they act in collaboration during bone and tooth morphogenesis.[12]
Quantity of BMPs
Normally, high concentrations of BMPs are required (i.e. 100-1000 ng/ml) at the local site to produce periodontal regeneration (Yamaguchi A). Approximately 10 kg of bovine bone yields only 2 μg of BMP. It consists of complex mixture of BMPs along with various other proteins. But the recombinant BMPs produced by several cellular systems were tested for regeneration.[13] The partially purified recombinant BMPs consist of 0.5-115 μg to produce cartilage formation within 7 days and bone formation within 14 days.
BMP Carrier Technologies
An absorbable collagen sponge was the first BMP carrier technology to be approved by the United States Food and Drug Administration. Several candidate technologies have been screened using multiple settings to evaluate their efficacy and biocompatibility as carriers for BMPs.[14] These include particulate and putty formulations of inorganic biomaterials from natural or synthetic sources based on hydroxyapatite, b-tricalcium phosphate, calcium sulfates/plaster of Paris, calcium phosphates, calcium carbonates, bioglass technologies, and organic polymers including allogeneic/xenogeneic collagen preparations, hyaluronan, poly-a-hydroxy acids, and methylmethacrylate. These technologies have been used alone or in combinations also including autogenous bone and fibrin.[14]
BMP in Periodontal Regeneration
In the field of periodontal regeneration, much of the research interest has focused on BMP-2 (OP-2), BMP-3 (osteogenin), and BMP-7 (OP-1). The first human study using a BMP to promote periodontal regeneration utilized a single application of BMP-3 (osteogenin) combined with demineralized bone allograft in a submerged tooth model.[15] Experiments utilizing crude and recombinant BMPs′ combination with other growth factors have provided insight as to their potential use. Crude preparations of BMP-2 and BMP-3 applied in surgically induced furcation defects appeared to stimulate periodontal regeneration.[9]
Recent studies have utilized recombinant human BMP to determine their potential for correcting intrabony, supra-alveolar, furcation, and fenestration defects.[16] Histologic analysis revealed periodontal regeneration with areas of ankylosis. Contrary to these findings, BMP-7 augmentation resulted in a significant increase in periodontal regeneration without any ankylosis. Healing through ankylosis has been a concern, so most of the recent research utilizing recombinant human BMPs has involved in the preparation of implant site for ossteointeration.[17]
BMPs also show much promise in promoting dental implant wound healing. A pilot study in non-human primates tested the single application of OP-1 around immediate extraction socket implants and found increased bone growth as measured histologically at 3 weeks.[18] In a recent study, combined adenovirus mediated human BMP-2 (Adv-hBMP-2) gene-modified bone marrow stromal cells (BMSCs) with allograft enhanced the defect healing and improved the strength of implant fixation with osseointegration in 3-mm bone defect around a titanium alloy implant.[12]
Bovine BMP (bBMP) tested in a dog model has shown to increase the rate of osseointegration around cylindrical uncoated endosseous implants as evidenced histomorphometrically 4 weeks after implantation.[19] The tissue reactions to titanium implants coated with bBMP were further assessed by scanning electron microscopy (SEM) for 12 weeks in the same dog model.[20] The results revealed abundant lamellar bone formation around bBMP-coated implants. This bone was found adjacent to the implant threads and frequently entered the implant holes.
Conclusion
BMP regenerative strategies attempt to mimic normal bone regeneration. Proper isolation and delivery of BMP are needed to give significant results for periodontal regeneration. Hence, future investigations may be necessary to develop improved delivery systems, as most of the current vehicles only allow transient (few hours) exposure of periodontal tissues to the growth factors. Ongoing human clinical trials assessing this potential therapeutic use of BMPs may provide the conclusive evidence for periodontal regeneration.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Socransky SS, Haffajee Ad. Dental biofilms: Difficult therapeutic targets. Periodontol 2000. 2002;28:12–55. doi: 10.1034/j.1600-0757.2002.280102.x. [DOI] [PubMed] [Google Scholar]
- 2.Petersilka GJ, Ehmke B, Flemmig Tf. Antimicrobial effects of mechanical debridement. Periodontology 2000. 2002;28:56–71. doi: 10.1034/j.1600-0757.2002.280103.x. [DOI] [PubMed] [Google Scholar]
- 3.Quirynen M, teughels W, De Soete M, van Steenberghe D. Topical antiseptics and antibiotics in the initial therapy of chronic adult periodontitis: Microbiological aspects. Periodontol 2000. 2002;28:72–90. doi: 10.1034/j.1600-0757.2002.280104.x. [DOI] [PubMed] [Google Scholar]
- 4.Wang HL, Cooke J. Periodontal regeneration technique for treatment of periodontal diseases. Dent Clin North Am. 2005;49:637–59. doi: 10.1016/j.cden.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 5.Kao Rt, Murakami S, Beirne OR. The use of biologic mediators and tissue engineering in dentistry. Periodontol 2000. 2009;50:127–53. doi: 10.1111/j.1600-0757.2008.00287.x. [DOI] [PubMed] [Google Scholar]
- 6.Elizabeth A, Wang, Rosen V, Josephine Recombinant human bone morphogenetic protein induces bone formation. Proc Natl Acad Sci USA. 1990;87:2220–4. doi: 10.1073/pnas.87.6.2220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.King GN, Cochran DL. Factors that moderate the effects of bone morphogenetic protein induced periodontal regeneration: A critical review. J Periodontol. 2002;73:925–36. doi: 10.1902/jop.2002.73.8.925. [DOI] [PubMed] [Google Scholar]
- 8.Wozney JM. The Potential Role of Bone Morphogenetic Proteins in Periodontal Reconstruction. J Periodontol. 1995;66:506–10. doi: 10.1902/jop.1995.66.6.506. [DOI] [PubMed] [Google Scholar]
- 9.Ripamonti U, Renton L. Bone morphogenetic protein and the induction of periodontal tissue regeneration. Periodontol 2000. 2006;41:73–87. doi: 10.1111/j.1600-0757.2006.00155.x. [DOI] [PubMed] [Google Scholar]
- 10.Hughes FJ, Turner W, Belibasakis G, Martuscelli G. Effect of growth factors and cytokines on osteoblast differentiation. Periodontol 2000. 2006;41:48–72. doi: 10.1111/j.1600-0757.2006.00161.x. [DOI] [PubMed] [Google Scholar]
- 11.Fiorellini JP, Howell TH, Cochran D, Malmquist J, Lilly LC, Spagnoli D, et al. Randomized study evaluating recombinant human bone morphogenetic protein-2 for extraction socket augmentation. J Periodontol. 2005;76:605–13. doi: 10.1902/jop.2005.76.4.605. [DOI] [PubMed] [Google Scholar]
- 12.Lan J, Wang Z, Wang Y. The effect of combination of recombinant human bone morphogenetic protein-2 and basic fibroblast growth factor or insulin-like growth factor-I on dental implant osseointegration by confocal laser scanning microscopy. J Periodontol. 2006;77:357–63. doi: 10.1902/jop.2006.050016. [DOI] [PubMed] [Google Scholar]
- 13.Yan MN, Dai KR, Tang TT, Zhu ZA, Lou JR. Reconstruction of peri-implant bone defects using impacted bone allograft and BMP-2 gene-modified bone marrow stromal cells. J Biomed Mater Res A. 2010;93:304–13. doi: 10.1002/jbm.a.32464. [DOI] [PubMed] [Google Scholar]
- 14.Margolin MD, Cogan AG, Taylor M, Buck D, McAllister TN, Toth C, et al. Maxillary sinus augmentation in the non-human primate: A comparative radiographic and histologic study between recombinant Human Osteogenic Protein-1 and Natural Bone Mineral. J Periodontol. 1998;69:911–9. doi: 10.1902/jop.1998.69.8.911. [DOI] [PubMed] [Google Scholar]
- 15.Bowers G, Felton F, Middleton C, Glynn D, Sharp S, Mellonig J, et al. Histologic comparison of regeneration in human intrabony defects when osteogenin is combined with demineralized freeze-dried bone allograft and with purified bovine collagen. J Periodontol. 1991;62:690–702. doi: 10.1902/jop.1991.62.11.690. [DOI] [PubMed] [Google Scholar]
- 16.Saito A, Saito E, Handa R, Honma Y, Kawanami M. Influence of residual bone on recombinant human bone morphogenetic protein-2-induced periodontal regeneration in experimental periodontitis in dogs. J Periodontol. 2009;80:961–8. doi: 10.1902/jop.2009.080568. [DOI] [PubMed] [Google Scholar]
- 17.Recombinant Human Bone Morphogenetic Protein-2 for Peri-Implant Bone Regeneration: A Case Report. J Periodontol. 2011;82:1212–8. doi: 10.1902/jop.2011.100626. [DOI] [PubMed] [Google Scholar]
- 18.Rutherford RB, Sampath TK, Rueger DC, Taylor TD. The use of bovine osteogenic protein to promote rapid osseointegration of endosseous dental implants. Int J Oral Maxillofac Implants. 1992;7:297–301. [PubMed] [Google Scholar]
- 19.Wang X, Baolin L, Yan J, Yang X. The effect of bone morphogenetic protein on osseointegration of titanium implants. J Oral Maxillofac Surg. 1993;51:647–51. doi: 10.1016/s0278-2391(10)80264-2. [DOI] [PubMed] [Google Scholar]
- 20.Wang X, Jin Y, Liu B, Zhou S, Yang L, Yang X, et al. Tissue reactions to titanium implants containing bovine bone morphogenetic protein: A scanning electron microscopic study. Int J Oral Maxillofac Surg. 1994;23:115–9. doi: 10.1016/s0901-5027(05)80605-8. [DOI] [PubMed] [Google Scholar]


