Abstract
Objectives:
The aim of our study is to determine the changes in quality of life and patient′s perception of esthetic improvement after anterior maxillary osteotomy.
Materials and Methods:
Our prospective study consisted of 14 patients who had been diagnosed of skeletal orthodontic deformity and underwent anterior maxillary osteotomy, along with orthodontic correction. The quality of life was evaluated using questionnaires based on Oral Health Impact Profile-14 questionnaire (OHIP-14) and a 22-item orthognathic quality of life questionnaire. They were evaluated at baseline pre-surgical, 8 weeks postoperatively, and 24 weeks postoperatively.
Results:
Our results showed mild improvement in generic health related quality of life immediately following surgery, while condition-specific quality of life and patient′s perception of esthetic improvement were noted only at 24 weeks following anterior maxillary osteotomy.
Conclusion:
We conclude that anterior maxillary osteotomy had a positive impact on the quality of life. The improvement in patient's perception of esthetics is seen only 2 months after surgery, while improvements in oral health and function were seen within 2 months following surgery. The acceptance and satisfaction of patient toward surgery was more positive 2 months after surgery.
KEY WORDS: Anterior maxillary osteotomy, esthetics, orthognathic surgery, patient perception
Orthognathic surgery (Greek “orthos” means straight and “gnathos” means jaw) is a single or double jaw surgery which is performed to reposition the jaws. During orthognathic surgery, a correct jaw alignment and occlusion, as well as facial harmony are achieved.[1] The motives of patients who request orthognathic operations are many and varied, but a desire for improvement in esthetics and alleviation of functional problems are the two most important reasons.[2]
The most common reason to seek orthodontic correction is proclined maxillary anterior teeth.
Anterior maxillary osteotomy is treatment of choice for cases of maxillary excess. Most of them exhibit skeletal Class II malocclusion with maxillary protrusion and proclined maxillary incisors. In addition to these antero-posterior problems, these cases are often accompanied by excessive vertical growth of the maxilla. This vertical excess causes a long mid-facial appearance and the display of incisors and gingiva during smiling.
Esthetic perception varies from person to person and is influenced by their personal experience and social environment. For this reason, professional opinions regarding evaluation of facial esthetics may not coincide with the perceptions and expectations of patients or lay people. Currently, there is a growing interest in how facial profile esthetics affects quality of life. Measures of facial appearance in quality of life are increasingly used in descriptive population-based research as a means of capturing esthetic aspects of facial profile that seem most relevant to the patients’ overall health and social well-being. Many of the studies found that patients were more self-confident and had more social skills after treatment.[3] Improvement in appearance brought about by orthognathic surgery results in improvement in psychosocial adjustment.[4] Orthognathic operations resulted in subjective estimations of function, appearance, health, and interpersonal relations, which were higher than among untreated control groups. The aim of our study was to elucidate patients’ perception of improvement after orthognathic operations, with regard to esthetic and functional aspects and quality of life.
Materials and Methods
Our prospective study included 14 patients who were treated at or referred to three private dental clinics during 2009–2011. They were diagnosed of vertical anterior maxillary excess. The patients were treated by combined orthodontic therapy with anterior maxillary osteotomy. Patients with bi-jaw surgery and other orthognathic surgical procedures were excluded. The patients were informed about their treatment plan and our study. Approval for the study was given by the regional research ethics committee. Patients willing to participate in the study were included and given questionnaire 1, prior to pre-surgical orthodontic therapy. The age of selected patients ranged from 22 to 34 years, with a mean age of 26 years. The patients then underwent pre-surgical orthodontic therapy and were prepared for anterior maxillary osteotomy. Prior to surgery, they were asked to fill Oral Health Impact Profile-14 (OHIP-14)[3] and a 22-item orthognathic quality of life questionnaire.[5] Following anterior maxillary osteotomy surgery, they were again asked to fill OHIP-14 and a 22-item orthognathic quality of life questionnaire during 8th week and 24th week postoperatively. An additional 2-item satisfaction questionnaire was given to all 14 patients and the patients were asked to fill it 6 months after surgery.
Evaluation Details
Questionnaire 1
Patients recorded their personal data, previous experience, and knowledge of malocclusion and treatment options, and medical and psychological aspects of appearance and function.
Oral health impact profile-14 questionnaire
The OHIP measures people's perceptions of the social impact of oral disorders on their well-being. The OHIP-49 contains 49 questions that capture seven conceptually formulated dimensions based on Locker's theoretical model of oral health adapted from the WHO framework used to classify impairments, disabilities, and handicaps, and the OHIP-14 was developed as a shorter version of the OHIP for settings where the full battery of 49 questions is inappropriate.
The questions covered seven problem areas: functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability, and handicap.
In this model, the consequences of oral disease are hierarchically linked from a biological level (impairment) to a behavioral level (functional limitation, discomfort, and disability) and lastly to the social level (handicap). The OHIP-14, in spite of being a short questionnaire, has been shown to be reliable, sensitive to changes, and to have adequate cross-cultural consistency.
The Oral Health Impact Profile[6] measure focuses on the impact of one's physical and mental status on the quality of life. The questions covered seven problem areas contributing to seven health domains (2 questions per domain): functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability, and handicap. Responses of each item were scored on a Likert-type scale and coded as follows: 0 = never, 1 = hardly ever, 2 = occasionally, 3 = fairly often, and 4 = very often. Overall OHIP-14 scores can range from 0 to 56, where 0 indicates no impact and 56 indicates the worst impact of one's oral health on the quality of life. Individual domain scores can be calculated by summating responses to the items within a domain and can range from 0 to 8, with higher scores indicating greater impact.
22-item orthognathic quality of life questionnaire
The 22 questions were based on four domains attributing to facial esthetics (5 questions), oral function (5 questions), awareness of dentofacial esthetics (4 questions), and social aspects of dentofacial deformity (8 questions). The answers were rated on a 4-point scale, with score ranging from 1 for answers “bothers you a little” to 4 for answers “bothers you a lot.” Higher score indicates lower quality of life and vice versa.
2-item patients’ satisfaction questionnaire
Two questions were used to rate the patient satisfaction and were included in addition to the above questionnaire items for global measures. The patient's satisfaction was recorded using a 4-point scale and the questions were as follows: “How would you rate your facial appearance compared with that before surgery?” and “Would you recommend this surgery to others?” The point scale rated was as follows: score 4 for positive response, score 2 for average/can’t say, and score 0 for negative response. Higher score indicates more satisfaction and acceptance of patient toward surgery. This questionnaire was given to the patient 6 months after surgery and the patient was asked to complete it along with above questionnaires.
Results
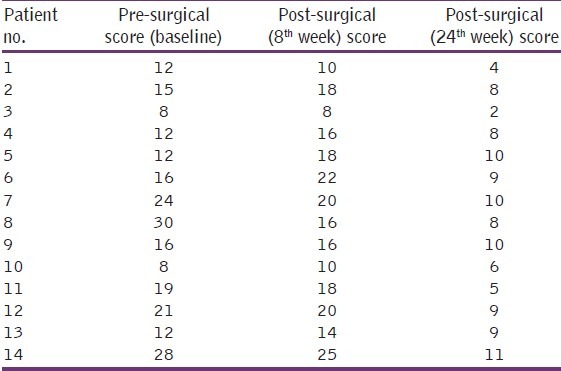
In our study data on OHIP-14, collected prior to surgery, all of the selected 14 members had stated to have problem, with scores ranging from 8 to 30 [Table 1]. The data analysis showed a mean score of 16.6, while the standard deviation was 6.9. This, when compared to 8th week mean value, slightly decreased to 16.5, but the standard deviation drastically decreased to 4.78. The decrease in OHIP-14 mean score denotes mild increase in functional efficiency, while standard deviation indicates the range of improvement was brief. The mean score after 6 months was 7.8 and the standard deviation reduced to 0.65.
Table 1.
Oral health impact profile-14 score
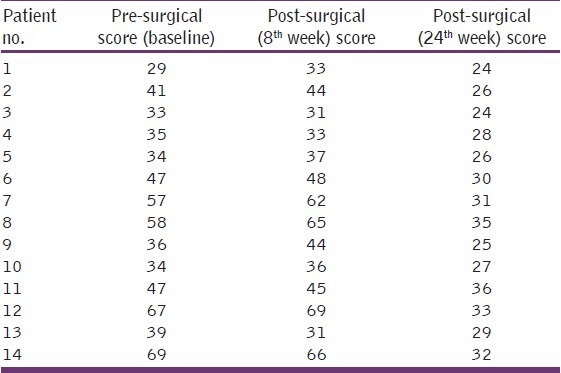
The data analysis of 22-item questionnaire [Table 2] base line score ranged from 29 to 69 out of the maximum score of 88. The mean score was 44.7 prior to surgery. Following surgery, the mean was increased to 46 during the 2nd month but decreased to 29 in the 6th month. The respective standard deviation noted was 13.17 prior to surgery, 13.94 during the 2nd month, and 3.96 in the 6th month postoperative analysis.
Table 2.
22-Item orthognathic quality of life questionnaire
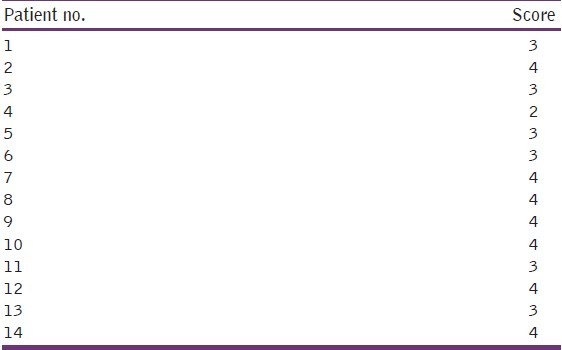
In our data on patient satisfaction questionnaire [Table 3], most of the patients had given a score of 4 (mode) and the average mean was 3.43, indicating a highly positive impact.
Table 3.
Patient satisfaction questionnaire score
Discussion
Incorporating patient perceptions is important in treatment planning, treatment decision-making, and evaluation of treatment outcomes.[5] It also helps in formulation of informed consent, addressing patient's needs, and validating the outcome.[3] There had been various studies pertaining to patient perception of esthetics.[2] The most common chief complaint in India to seek orthodontic treatment is forwardly placed upper front teeth. The vertical maxillary excess is treated by many modalities, including orthodontic intrusion, Le Fort surgery, anterior maxillary osteotomy, and/or a combination of above. Anterior maxillary osteotomy helps to decrease gummy smile and is often the treatment of choice. Pre-surgical orthodontic treatment helps in alignment of the teeth relative to the most desirable position over basal bone, thus aiding surgery.
The score prior to surgery was kept as the baseline score and used to evaluate changes in questionnaires 2 and 3, following surgery. There has been a little change in OHIP-14 score postoperatively. Though the mean score decreased, the change in standard deviation showed more deterioration in health. The deterioration was rather uniformly distributed over physical and mental status. Some had complained about limitation in social activity and mild body pain, headache, and swelling. This is similar to Lee et al.'s[5] report in 2008. However, in contrast, physical functioning and role performance had significantly improved. This contrast may be attributed to the additional 2-week postoperative healing factor. The evaluation was done after 8 weeks by us, allowing more adequate time for post-surgical recovery. The sequel of surgery is responsible for the slight changes noted. The OHIP-14 score at the 6th month clearly demonstrates huge improvement in oral health quality of life; hence, motivation of patient for orthognathic surgery for better physical, social, and mental health is proved and validated. The decrease in standard deviation clearly demonstrates an overall improvement in all fields and acceptance of increased well-being by all our patients.
The 22-item orthognathic quality of life questionnaire score is more esthetic and dental functional oriented. The baseline scores ranged widely up to 69 out of maximum 88. Following surgery, during the 2nd month, the score had nearly decreased by half, but standard deviation had increased, denoting variation in acceptance of surgery. This was due to paresthesia and post-surgical healing factors. Some of the patients complained about decrease in appetite; decrease in esthetics, and swelling, while some people accepted surgery and had given positive response. While graphing the age and sex of patient (not included in the main study), we found that younger male patients had better surgical acceptance during this postoperative period. There was a huge improvement in orthognathic quality of life noted at 6th month postoperatively, and the highest score was limited to 36. The improvement was seen in all the 14 patients who responded positively in the satisfaction questionnaire. Our study observation is supported by the reports of Cunningham et al.[2,3,7,8] and Shermin Lee et al.[5] It proves that the anterior maxillary osteotomy along with orthodontic correction is the widely accepted treatment of choice by patients diagnosed of vertical maxillary excess. The treatment modality improves not only oral health, but also mental and social health, with better functional role. The quality of life improvement following surgery was very high. A comprehensive assessment of quality of life using generic oral health and condition-specific approaches proved to be useful in determining such changes during the trajectory of treatment. We conclude that patients’ perceptions after anterior maxillary osteotomy were generally favorable, but there is a need for improved information to the patients during the treatment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Modig M, Andersson L, Wardh I. Patients’ perception of improvement after orthognathic surgery: Pilot study. Br J Oral Maxillofac Surg. 2006;44:24–7. doi: 10.1016/j.bjoms.2005.07.016. [DOI] [PubMed] [Google Scholar]
- 2.Cunningham SJ, Hunt NP, Feinmann C. Psychological aspects of orthognathic surgery: A review of the literature. Int J Adult Orthodon Orthognath Surg. 1995;10:159–72. [PubMed] [Google Scholar]
- 3.Cunningham SJ, Garratt AM, Hunt NP. Development of a condition-specific quality of life measure for patients with dentofacial deformity: II. Validity and responsiveness testing. Community Dent Oral Epidemiol. 2002;30:81–90. doi: 10.1034/j.1600-0528.2002.300201.x. [DOI] [PubMed] [Google Scholar]
- 4.Pahkala RH, Kellokoski JK. Surgical-orthodontic treatment and patients’ functional and psychosocial well-being. Am J Orthod Dentofacial Orthop. 2007;132:158–64. doi: 10.1016/j.ajodo.2005.09.033. [DOI] [PubMed] [Google Scholar]
- 5.Choi WS, Lee S, McGrath C, Samman N. Change in quality of life after combined orthodontic-surgical treatment of dentofacial deformities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:46–51. doi: 10.1016/j.tripleo.2009.08.019. [DOI] [PubMed] [Google Scholar]
- 6.Slade GD, Spencer AJ. Developing and evaluation of the oral health impact profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 7.Cunningham SJ, Hunt NP. Quality of life and its importance in orthodontics. J Orthod. 2001;28:152–8. doi: 10.1093/ortho/28.2.152. [DOI] [PubMed] [Google Scholar]
- 8.Lee S, McGrath C, Samman N. Impact of orthognathic surgery on quality of life. J Oral Maxillofac Surg. 2008;66:1194–9. doi: 10.1016/j.joms.2008.01.006. [DOI] [PubMed] [Google Scholar]


