Abstract.
This study aimed to evaluate the use of mobility-provocation radiostereometry (RSA) in anterior cervical spine fusions and compare the results to deformation studies on the same patients and plain flexion-extension radiographs. Mobility-provocation RSA was used to evaluate anterior cervical spine fusions in 45 patients. The motions recorded at 3 and 12 months postoperatively were compared to RSA measurements of deformation of the fusion over time and to plain flexion-extension radiographs in the same patients taken 3 months postoperatively. Studies of rotations from right to left revealed ten cases with significant motion at 3 months, and three at 12 months. With motion from flexion to extension, ten cases showed significant motion at 3 months and three at 12 months. In only three cases was the mobility-provocation RSA considered to add any information on the stability of the fusions compared to that obtained with the deformation studies. In 37 patients mobility-provocation radiography in flexion-extension using conventional technique was done to evaluate the accuracy. The mean difference between angular motions recorded on plain radiographs and rotations around the transverse axis in flexion to extension recorded with RSA was 1.6° (range 0.04°–8.04°, SD 2.1°). The corresponding 95% and 99% confidence limits for the difference between the two methods were 5.8° and 7.2°. The study showed that the use of mobility-provocation RSA did not add any information over that obtained by deformation RSA studies. Conventional radiography is too inaccurate to measure inducible displacement in this patient population.
Keywords. Anterior cervical fusion, Radiostereometry, Radiographs
Introduction
Abnormal motion on flexion-extension radiographs (mobility-provocation radiography) is often used to indicate instability in the cervical spine [12]. This method is also used to evaluate healing after fusion [1]. Correct interpretation of these radiographs is important, because an unhealed fusion is potentially unstable and eventually a source of pain. Several methods exist to measure motion between vertebrae on radiographs [5, 8, 12]. Lind et al. [5] used lines drawn along the inferior endplates, and estimated the intra-observer error of this method to be at least 1.8°, and the corresponding inter-observer error, at least 1.2°. However, no evaluation of repeat examinations was done, and a more accurate method acting as a reference was not available. In the lumbar spine, the accuracy of conventional functional radiographs has varied from 1.5° to 5° in rotation [2, 7]. The true size of measurement error using conventional radiography to examine motions of the vertebrae in the cervical spine is not known.
RSA is a proven method for detecting small motions with a high accuracy for both translation and rotation [4]. This method enables measurement of three-dimensional motion between different end positions (mobility-provocation RSA). The end points chosen may include not only flexion-extension, but also other positions. In earlier studies on the same patients, RSA was used to measure deformations over a period of time after anterior cervical spinal fusion [14, 15]. No comparison between conventional radiography and RSA during mobility provocation test of cervical spine motion has been previously carried out.
This study aimed to evaluate whether mobility-provocation RSA is more useful for analyzing the time of healing of a fusion compared with the previous deformation studies. Both types of evaluation were applied to previously presented materials of one- or two- level fusions of the cervical spine [14, 15]. In these studies the patients were randomized to fixation with or without plate. We also compared the results of flexion-extension provocation measured on conventional radiographs with measurements based on the RSA technique.
Materials and methods
The study includes 45 consecutive patients referred to our department between January 1994 and October 1995 with neck pain and arm radiculopathy, who were operated with disc excision and anterior fusion. All patients had pain and neurological symptoms corresponding to a magnetic resonance imaging (MRI) verified herniated disc and/or spondylosis on one or two levels. There were 23 women and 22 men with a mean age of 42 (range 25–60) years. Twenty-four of the patients were randomized to stabilization with a graft and a CSLP plate (Synthes, Switzerland) and 21 patients to grafting without any internal fixation. Twenty-seven patients were operated on one level, 15 with plate fixation (WP) and 12 without plate fixation (WOP), and 18 on two levels (9 WP, 9 WOP). Randomization was done using sealed envelopes opened the day before surgery. The cervical spine was approached through an anterior transverse incision on the left side of the neck. The anterior longitudinal ligament was excised over the disc space, and the anterior half of the disc was removed macroscopically. The remaining posterior part of the nucleus pulposus and the herniated fragment was removed using a microscope. A tricortical bone graft was harvested from the left anterior iliac crest [9]. Before grafting, three to seven tantalum markers (0.5 or 0.8 mm in diameter) were implanted in the adjacent vertebrae after pre-drilling through the cortex.
After surgery, patients operated without a plate were treated with a Philadelphia collar for 6 weeks, and those operated with plate fixation wore a soft collar for 6 weeks as recommended in the literature [13].
Radiostereometric analysis
Mobility provocation was obtained by examination of the patients in four different end positions of motion (flexion, extension, rotation right and left) using RSA. The patient’s head was passively moved to the different end points by the examiner. Data from these examinations, done at 3 and 12 months postoperatively, were compared with deformations of the fusions on the same patients over time (between the postoperative and the subsequent follow up examinations at 6 weeks, and 3, 6, 12 and 24 months) [14, 15].
The provocation stereoradiographs were obtained with the patient standing, using a uniplanar technique [3]. At subsequent evaluations, the three-dimensional coordinates of the patient markers were determined at each examination.
Motions occurring between maximum flexion to extension and maximum rotation of the head from right to left were computed.
For the mathematical evaluation of the radiographic examinations, we used a software package (UmRSA, RSA Biomedical Innovations, Umeå, Sweden), mainly based on RSA measurement techniques according to Selvik [10]. The most distal vertebra was used as a fixed reference segment. All motions were related to the laboratory coordinate system defined by the cage. Rotations of the more proximal vertebra were calculated in the order:
Flexion-extension (rotations around the transverse axis)
Left-right rotation of the head (longitudinal axis), and
Left-right bending (anterior-posterior axis)
The relative translation of the center of gravity of the markers in the most proximal vertebra was recorded in all but ten cases (five with plate fixation), where only two markers were available in the motion segment. In these cases, the mean value of the two markers represented translations, whereas rotations could not be evaluated. Translations were measured as:
Medio-lateral translations (left-right)
Proximal-distal translations (distraction-compression), and
Anterior-posterior translations
The precision of the measurements has previously been determined in 36 double examinations (Table 1 ) [14, 15]. The motions were determined as significant if they exceeded the 99% confidence limits of the error calculated in Table 1 .
Table 1.
The 99% confidence limits of radiostereometry (RSA) in the cervical spine in 36 double examinations [14, 15]
| One level | Two levels | |
|---|---|---|
| Translations (mm) | ||
| Anterior-posterior | 0.56 | 0.43 |
| Proximal-distal | 0.27 | 0.34 |
| Medial-lateral | 0.81 | 0.85 |
| Rotations (degrees) | ||
| Transverse axis | 3.6 | 4.0 |
| Longitudinal axis | 4.2 | 3.7 |
| Sagittal axis | 1.3 | 2.0 |
The accuracy of the RSA is dependent on several factors. Some of the most important are the stability, spacing and number of the markers. The degree of marker instability is expressed in millimeters as the mean error of rigid body fitting [10], and the spacing of the markers in terms of a condition number [11]. The values of these parameters did not differ from those previously presented for this material [14, 15].
In relation to the deformation studies, the mobility provocation RSA radiographs were considered either to add information or provide insufficient information during the following circumstances. Information was added if significant motion (>99% confidence limits) was recorded, despite the longitudinal recordings of deformation during the immediately previous time period (6 weeks–3 months’ or 6–12 months’ evaluation in the supine position) having indicated that the fusion was stable. Insufficient information was obtained if no motion was detected, despite significant deformations being recorded during the subsequent time periods (3–6 months or 12–24 months). Two patients were excluded from the study because of unstable markers. Both were operated on two levels without a plate.
Conventional radiography
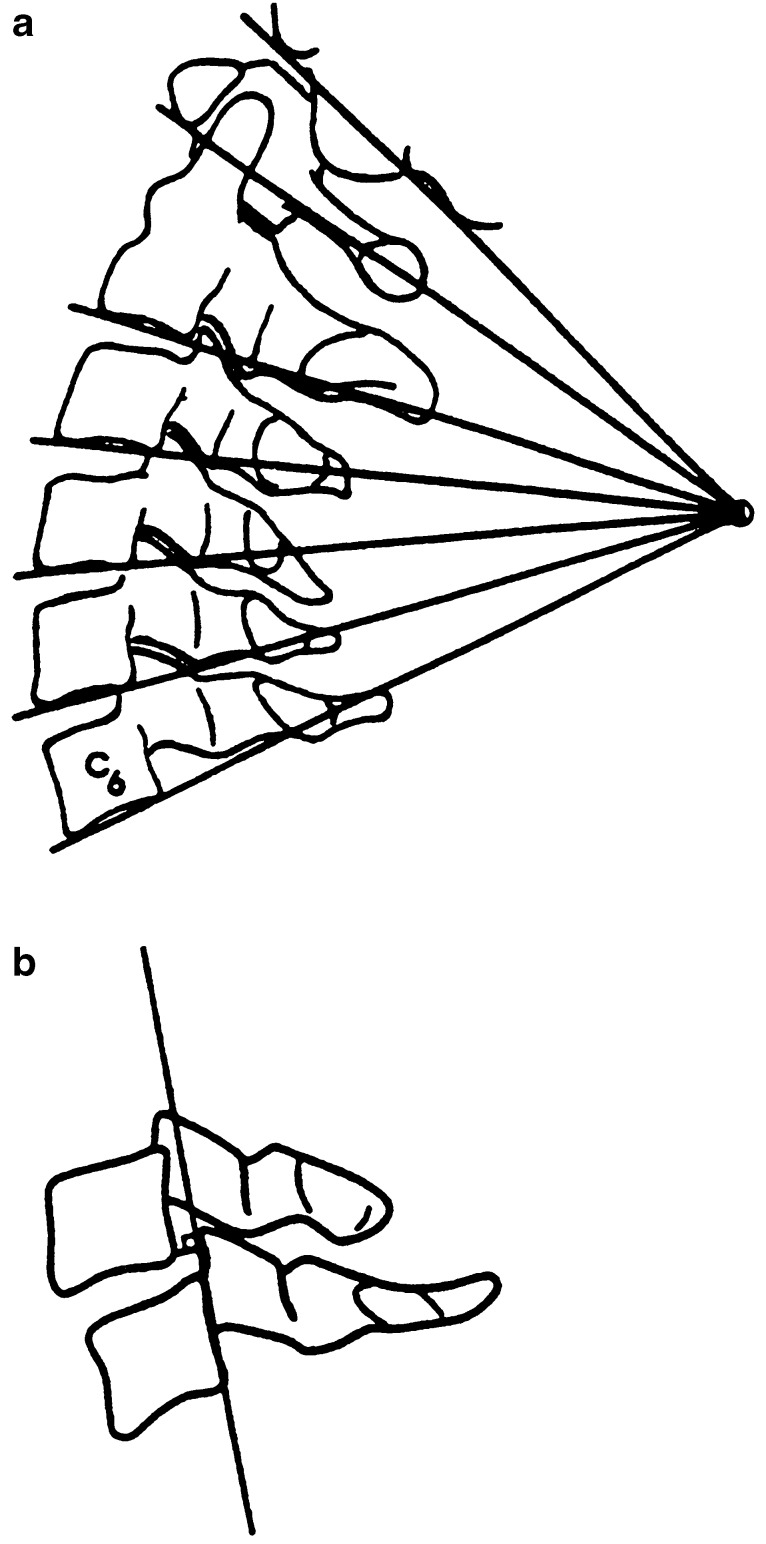
At 3 months, 37 cases were examined with mobility provocation in flexion and extension corresponding to two of the end points used at the RSA studies. This examination was done immediately after the RSA examination. The angular motion between the flexion and extension radiographs was recorded using a pencil, a ruler and a goniometer, by recording the angulation between lines drawn along the inferior endplates of the vertebrae included in the fusion [5]. The lower anterior and posterior corners of the most distal and the most proximal vertebrae in the fusion were used as preset points on the radiographs. Sagittal translation was measured as the shortest distance between the lower posterior margin of the upper vertebra and a line drawn along the posterior wall of the lower vertebra (Fig. 1).
Fig. 1.
Measurement of A segmental angulation and B translational displacement
The study was approved by the local human ethical committee
Statistical methods
The statistical methods used are indicated in the text for each calculation.
Results
Mobility provocation radiostereometry versus deformation
Rotation right-left test
The three-dimensional motions between the vertebrae did not differ between patients operated with a plate and those operated without plate fixation (Table 2 , Mann-Whitney U-test). Ten cases showed significant motion at 3 months. Of these ten cases, five also showed significant motion in the flexion to extension mobility provocation RSA test. In two cases, significant motion was revealed despite there being no significant deformation between 6 weeks and 3 months postoperatively (Table 3 ). In 11 cases this mobility test did not reveal any significant motions, even though a continuous deformation between the vertebrae during the following 3 months was noted.
Table 2.
Motions recorded with mobility provocation RSA: rotation, right to left
| Fusion one levelb | Fusion two levelsc | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No plate | Plate | No plate | Plate | |||||||
| n | Median (range) | n | Median (range) | n | Median (range) | n | Median (range) | |||
| Rotations | ||||||||||
| Transverse axis | ||||||||||
| 3 months | 9 | 0.7 (–2.5;2.5) | 11 | –0.5 (–1.7;2.5) | 5 | 0.4 (–2.0;1.3) | 7 | –0.1 (–1.6;12.8) | ||
| 12 months | 8 | 0.2 (–1.3;2.2) | 12 | 0.5 (–1.4;1.6) | 4 | 0 (3.3;1.6) | 8 | 0.3 (–2.7;1.63) | ||
| Longitudinal axis | ||||||||||
| 3 months | 9 | –0.5 (–2.6;5.7) | 11 | –1.3 (–3.4;0.8) | 5 | –1.5 (–2.6;–0.2) | 7 | 0.3 (–4.4;14.62) | ||
| 12 months | 8 | 0.3 (–0.7;1.2) | 12 | 0 (–2.0;0.9) | 4 | –0.8 (–1.3;0.4) | 8 | –0.8 (–1.3;2.1) | ||
| Anterior-posterior axis | ||||||||||
| 3 months | 9 | 1.1 (–0.8;2.6) | 11 | 1.6 (–0.2;3.0) | 5 | 0.7 (0.2;2.5) | 7 | 0.7 (–2.6;2.7) | ||
| 12 months | 8 | 0.1 (–0.5;1.0) | 12 | 0.1 (–0.4;2.6) | 4 | 1.9 (–0.1;4.2) | 8 | 0.2 (–0.6;1.4) | ||
| Translations | ||||||||||
| Transverse axis | 11 | –0.1 (–0.4;0.1) | 14 | 0 (–0.8;0.2) | 7 | 0 (–0.2;0.3) | 8 | –0.3 (–0.3;2.6) | ||
| 3 months | 10 | 0 (–0.3;0.1) | 15 | –0.1 (–0.7;0.4) | 6 | –0.1 (–0.6;0.1) | 8 | 0 (–0.5;0.8) | ||
| 12 months | ||||||||||
| Longitudinal axis | ||||||||||
| 3 months | 11 | 0 (–0.1;0.2) | 14 | 0 (–0.4;0.3) | 7 | 0 (–0.2;0.3) | 8 | 0 (–0.5;0.2) | ||
| 12 months | 10 | 0 (–0.2;0.1) | 15 | 0 (–0.1;0.1) | 6 | 0 (–0.3;0) | 8 | 0 (–0.2;0.5) | ||
| Anterior-posterior axis | ||||||||||
| 3 months | 11 | 0 (–0.5;0.4) | 14 | 0 (–0.2;0.5) | 7 | 0.1 (–0.3;0.3) | 8 | 0.5 (–0.6;1.6) | ||
| 12 months | 10 | 0 (–0.2;0.6) | 15 | 0 (–0.1;0.5) | 6 | –0.3 (–0.7;0.1) | 8 | 0 (–0.9;0.6) | ||
| No. of cases with significant motiona | ||||||||||
| 3 months | 3 | 4 | 1 | 2 | ||||||
| 12 months | 0 | 2 | 1 | 0 | ||||||
Table 3.
Number of patients who showed presence/absence of inducible displacement at 3 months related to findings of deformation studies [14, 15]
| Flexion-extension | Rotation left-right | |
|---|---|---|
| No information added | ||
| In accordance with deformation studies | ||
| Deformation up to 3 months | ||
| No inducible displacement | 12 | 13 |
| Inducible displacement | 3 | 3 |
| Deformation up to 6 months | ||
| Inducible displacement | 7 | 6 |
| No deformation 6 w to 3 months | ||
| No inducible displacement | 8 | 7 |
| Not in accordance with deformation studies | ||
| Deformation up to 6 months | ||
| No inducible displacement | 8 | 11 |
| Information added | ||
| Not in accordance with deformation studies | ||
| No deformation 6 weeks to 3 months | ||
| Inducible displacement | 1 | 2 |
At 12 months, 3 patients showed significant motion in right to left rotation of the head, with only one of them showing significant motion on the extension to flexion test. One of these three patients displayed a significant deformation up to the 12-month follow-up. The other two patients displayed no deformation after 3 months.
Flexion to extension test
The use of plate fixation did not influence the “inducible” motions at either of the two follow-up occasions with this test (Table 4 , Mann-Whitney-U test). In one case, significant motion was revealed (at 3 months) despite there being no deformation after 6 weeks on deformation studies. In eight cases the flexion-extension RSA test did not reveal any motion, despite there being a continuous deformation over the fusion during the subsequent follow-up at 3 months (Table 3 ). One of these cases showed significant motion on the rotation right to left test.
Table 4.
Motion recorded with mobility provocation RSA: flexion-extension
| Fusion one levelb | Fusion two levelsc | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| No plate | Plate | No plate | Plate | ||||||
| n | Median (range) | n | Median (range) | n | Median (range) | n | Median (range) | ||
| Rotations | |||||||||
| Transverse axis | |||||||||
| 3 months | 9 | –1.4 (–7.1;1.6) | 11 | –1.0 (–8.1;9.0) | 5 | 1.1 (–7.6;8.6) | 6 | –2.1 (–4.9;2.2) | |
| 12 months | 9 | –1.0 (–3.1;0.3) | 12 | –0.1 (–5.5;2.2) | 3 | –2.4 (–2.8;1.1) | 8 | 0 (–1.0;1.5) | |
| Longitudinal axis | |||||||||
| 3 months | 9 | 0.1 (–0.8;1.3) | 11 | –0.6 (–3.7;2.0) | 5 | 0.1 (–3.3;1.4) | 6 | 0.9 (–1.2;1.7) | |
| 12 months | 9 | –0.2 (–1.3;0.6) | 12 | –0.1 (–3.6;1.3) | 3 | 0.3 (–0.7;2.3) | 8 | 0 (–1.0;1.5) | |
| Anterior-posterior axis | |||||||||
| 3 months | 9 | –0.1 (–0.6;1.5) | 11 | 0.1 (–1.4;2.1) | 5 | 0.3 (–0.1;0.5) | 6 | –0.6 (–2.5;1.0) | |
| 12 months | 9 | –0.2 (–1.0;0.6) | 12 | 0 (–2.0;1.8) | 3 | –0.1 (–0.3;0.7) | 8 | 0.2 (–1.5;1.12) | |
| Translations | |||||||||
| Transverse axis | 11 | 0 (–0.7;0.2) | 14 | 0 (–0.6;0.3) | 7 | 0 (–0.4;0.3) | 7 | 0 (–0.3;0.9) | |
| 3 months | 11 | 0 (–0.3;0.9) | 15 | 0 (–0.5;0.3) | 6 | 0.2 (–0.1;0.4) | 8 | 0 (–0.5;0.3) | |
| 12 months | |||||||||
| Longitudinal axis | |||||||||
| 3 months | 11 | 0 (–0.4;0.3) | 14 | 0 (–0.4;0.3) | 7 | 0.1 (–0.3;1.2) | 7 | 0 (–0.2;0.3) | |
| 12 months | 11 | 0 (–0.2;0.1) | 15 | 0 (–0.1;0.4) | 6 | 0 (0;0.2) | 8 | 0 (–0.1;0.4) | |
| Anterior-posterior axis | |||||||||
| 3 months | 11 | –0.1 (–0.9;0.4) | 14 | 0 (–1.7;0.8) | 7 | 0.1 (–1.0;2.0) | 7 | –0.6 (–2.0;–0.2) | |
| 12 months | 11 | –0.1 (–0.5;0.2) | 15 | 0 (–1.3;0.5) | 6 | 0 (–0.4;0.5) | 8 | –0.3 (–1.2;0.1) | |
| No. of cases with significant motiona | |||||||||
| 3 months | 3 | 4 | 2 | 1 | |||||
| 12 months | 0 | 3 | 0 | 0 | |||||
At 12 months, three patients showed significant motion in flexion to extension. Only one of them showed significant motion on the rotation right to left test. The mobility provocation test was considered to add information in two of these cases, where deformation studies had indicated stability between 3–12 months and 6–12 months, respectively. However, subsequent deformation studies in these two cases revealed significant motion during the interval 12–24 months in one of them. This was the only patient who displayed significant deformation between 1 and 2 years measured with RSA. The plate is intact, and there are no screws loosening at 2 years postoperatively. One patient who was operated with plate fixation developed pseudoarthrosis and was reoperated after 12 months. This patient did not show any significant motion on the mobility provocation RSA or plain flexion-extension radiographs at 3 months, but showed significant deformations throughout the 1st postoperative year.
Conventional radiography versus radiostereometry
Mobility provocation in flexion-extension
The mean angular motion between flexion and extension measured with the conventional method at 3 months was 1.7° (range 0°–5°, SD 1.2°). No translations could be detected on plain flexion-extension radiographs. The mean difference between angular motions recorded on plain radiographs and rotations around the transverse axis in flexion to extension recorded with RSA was 1.6° (range 0.04°–8.04°, SD 2.1°). The corresponding 95% and 99% confidence limits for the difference between the two methods were 5.8° and 7.2° respectively.
Discussion
In the present study several patients displayed significant motions on the 3-month (20 patients) and 12-month (4 patients) mobility provocation RSA examinations. These inducible motions were not significantly influenced by the use of a plate. There was, however, a tendency for the patients operated without a plate to stabilize earlier than the patients with plate fixation, when only one level had been fused. This is in accordance with our previous studies on continuous deformation over the fused segments [14, 15]. In these studies, we noted that there often was continuous compression over the fused area in patients with plate fixation up to 1 year postoperatively. In patients operated without a plate, the fusion usually stabilized between 3 and 6 months postoperatively. These observations support theories that this non-dynamic plate could delay the time to healing by preventing postoperative compression.
The addition of mobility provocation RSA to the evaluation of patients in the study group did not add much information about the healing time of the fusion. On the contrary, in 12 patients there was no significant motion on the mobility provocation RSA at 3 months, but on the subsequent studies of deformation, these fusions were found to display continuous motion (Table 3 ). The lack of repeat measurement mobility provocation RSA weakens the results as presented here, as the reproducibility of these results is uncertain.
In only two patients did the mobility provocation RSA display significant motion despite the presence of significant deformation before or after the 3-month follow-up. These observations lead to the conclusion that mobility provocation RSA is probably not a reliable method for evaluating the time for healing in cervical spine fusion. It is more accurate to use only longitudinal RSA examinations (deformation studies) to study when a fusion becomes stable.
In conventional radiography it is difficult or impossible to achieve precisely the same positions of the vertebrae in relation to the roentgen beam in flexion versus extension. Other errors of measurement are related to the procedure of measuring angles with the use of a pencil, ruler and a goniometer. One would assume that the use of a digitizing table might result in a better precision, but this was not verified by Malchau et al. [6] in a comparative study between RSA and conventional radiographs of hip prostheses. In the present study there were two patients with comparatively large rotations at the flexion-extension mobility provocation using RSA radiographs (7.5° and 8.6°). On conventional flexion-extension radiographs, the largest motion in these same two patients was 5°, which is less than the 95% confidence interval for significant motions. Thus, the fusion in these two patients would be regarded as stable on conventional radiography. This means that even if no significant motion can be demonstrated on conventional flexion-extension radiographs, the fusion is not necessarily stable. Furthermore, motion between the cervical vertebrae on rotation right to left of the head is almost impossible to detect using conventional radiography.
The small motions recorded with mobility provocation RSA of cervical spine fusions and the poor precision of conventional radiography question the use of these methods for evaluating postoperative healing, unless there is a gross instability. The use of RSA in routine settings is, however, not cost effective. RSA is time consuming and quite expensive, and can therefore only be used for research purposes. As clinicians, we still have to use conventional flexion-extension radiographs to evaluate fusions, but with an increased awareness of its limitations.
In conclusion, when RSA was used, we found small movements during provocation of the head in flexion-extension and rotation right to left. However, these examinations added little information compared to the previous RSA studies of deformation. The reproducibility of conventional flexion-extension radiography was found to be poor. The use of this latter method to routinely evaluate stabilization of a cervical spine fusion is insufficient. Thus, there is still a need to find a more accurate and easily performed evaluation method of intervertebral motion in the cervical spine.
Acknowledgements.
This study was supported with grants from: the Göteborg Medical Society; the Greta and Einar Askers Foundation; Bertha and Felix Neubergh’s Foundation and Gothenburg University.
References
- 1.CauthenSpine 199821889474724 [Google Scholar]
- 2.Drerup J Biomech. 1985;18:369. doi: 10.1016/0021-9290(85)90292-1. [DOI] [PubMed] [Google Scholar]
- 3.Kärrholm Acta Orthop Scand. 1989;60:491. doi: 10.3109/17453678909149328. [DOI] [PubMed] [Google Scholar]
- 4.KärrholmClin Orthop 1997344949372762 [Google Scholar]
- 5.Lind Arch Phys Med Rehabil. 1989;70:692. [PubMed] [Google Scholar]
- 6.Malchau Acta Orthop Scand. 1995;66:418. doi: 10.3109/17453679508995578. [DOI] [PubMed] [Google Scholar]
- 7.PanjabiSpine 1992172001553591 [Google Scholar]
- 8.Penning AJR. 1964;91:1036. [PubMed] [Google Scholar]
- 9.Robinson Bull Johns Hopkins Hosp. 1955;96:223. [Google Scholar]
- 10.Selvik G (1989) Roentgen stereophotogrammetry. A method for the study of the kinematics of the skeletal system. Acta Orthop Scand 60 [Suppl 232] [PubMed]
- 11.Söderkvist I (1993) Computing parameters in nonlinear least squares models. Thesis, University of Umeå
- 12.White Spine. 1976;1:15. [Google Scholar]
- 13.Whitecloud T (1989) Management of radiculopathy and myelopathy by the anterior approach. In: Cervical Research Society (eds) The Cervical Spine. Lippincott, Philadelphia, pp 644–658
- 14.Zoëga Acta Orthop Scand. 1998;69:363. doi: 10.3109/17453679808999048. [DOI] [PubMed] [Google Scholar]
- 15.Zoëga Eur Spine J. 1998;7:302. doi: 10.1007/s005860050079. [DOI] [PMC free article] [PubMed] [Google Scholar]