Abstract
Anterior lumbar interbody fusion (ALIF) is a widely accepted tool for management of painful degenerative disc disease. Recently, the modern laparoscopic surgical technique has been combined with ALIF procedure, with good early postoperative results being reported. However, the benefit of laparoscopic fusion is poorly defined compared with its open counterpart. This study aimed to compare perioperative parameters and minimum 2-year follow-up outcome for laparoscopic and open anterior surgical approach for L5–S1 fusion. The data of 54 consecutive patients who underwent anterior lumbar interbody fusion (ALIF) of L5–S1 from 1997 to 1999 were collected prospectively. More than 2-years’ follow-up data were available for 47 of these patients. In all cases, carbon cage and autologous bone graft were used for fusion. Twenty-five patients underwent a laparoscopic procedure and 22 an open mini-ALIF. Three laparoscopic procedures were converted to open ones. For perioperative parameters only, the operative time was statistically different (P=0.001), while length of postoperative hospital stay and blood loss were not. The incidence of operative complications was three in the laparoscopic group and two in the open mini-ALIF group. After a follow-up period of at least 2 years, the two groups showed no statistical difference in pain, measured by visual analog scale, in the Oswestry Disability Index or in the Patient Satisfaction Index. The fusion rate was 91% in both groups. The laparoscopic ALIF for L5–S1 showed similar clinical and radiological outcome when compared with open mini-ALIF, but significant advantages were not identified, despite its technical difficulty.
Keywords: Laparoscopic ALIF, L5–S1 fusion, Carbon cage
Introduction
Anterior lumbar interbody fusion (ALIF) is a widely accepted tool for management of painful degenerative disc disease, despite the wide range of success rates [2, 3, 6, 9, 11, 16, 17, 19]. A transperitoneal or retroperitoneal approach to the spine can avoid paravertebral muscle injury, traction on nerve roots, and epidural scarring, which are common undesirable complications of the posterior approach. Recently, the modern laparoscopic surgical technique was combined with the ALIF procedure, which was made possible through the efforts of early investigators [12, 13, 21]. Early clinical reports for laparoscopic fusion were encouraging. It has been reported that laparoscopic discectomy with interbody fusion is not only feasible, but also appears to give good results during the early postoperative period [10, 22, 23, 27]. The effectiveness and safety of laparoscopic ALIF were comparable to open procedures [24, 26].
However, the benefit of laparoscopic fusion is poorly defined compared with its open counterpart. Most authors mention technical difficulties related to the laparoscopic approach, which involves dissection and retraction of great vessels [8, 12, 24, 26]. Usually the spine surgeon cannot reach the anterior aspect of lumbar spine without the help of a laparoscopic surgeon. Even with the laparoscopic surgeon, the procedure is associated with a learning curve and may be time consuming. Zdeblick and David [26] found no objective benefit of laparoscopic ALIF compared with the mini open procedure in their prospective study of 25 patients after considering the high complication rate and long operative time.
Moreover, Riley et al. [25] reported greater stiffness in their open group and less extensive discectomy and bone growth in the implant in their laparoscopic group in a biomechanical and histological analysis of the open versus laparoscopic technique in a pig model. Their report highlights some of the potential shortcomings of the early clinical reports of laparoscopic lumbosacral fusion. These studies involved a small number of patients with short-term follow-up.
Therefore, there is a need for a long-term prospective study comparing laparoscopic to open ALIF and evaluation of laparoscopic ALIF as a minimally invasive procedure.
The authors conducted a prospective comparative study of laparoscopic and open mini-ALIF to investigate minimum 2-year follow-up outcome and to determine any objective benefit of laparoscopic ALIF as a minimally invasive procedure.
Materials and methods
The study cohort consisted of 54 consecutive patients with a diagnosis of painful L5–S1 degenerative disc disease, who were enrolled into this prospective study. The patients were randomly assigned into one of the two surgical groups: fusion by anterior approach laparoscopic procedure (group 1) or anterior approach open mini-ALIF procedure (group 2). The operations were performed between April 1997 and June 1999.
Operative indication
Inclusion criteria were discogenic pain at L5–S1 by degenerative disc disease or internal disc disruption. The diagnosis was made by plain radiograph, magnetic resonance imaging, and concordant provocation of pain by discography. The symptomatic indications were disabling back pain that caused life-style alteration and failure of nonoperative treatment for more than 6 months. Patients with spondylolisthesis, spinal infection, severe osteoporosis, spinal stenosis, and previous spinal fusion operation were excluded.
In Group 1, the L5–S1 disc space was approached by the laparoscopic transperitoneal technique, as previously described. For fusion, a Brantigan carbon cage packed with autologous bone was used. Laparoscopic exposure was performed by the general surgeon (third author).
In Group 2, a midline extraperitoneal approach was used to expose the L5–S1 space between the iliac vessels. The typical length of the skin incision was 5 cm, and was located just inferior to the umbricus. Two hand-held and one robotic retractor were used in the procedures. Carbon cages and autologous bone graft were incorporated in the fusion surgeries.
Pre- and postoperative evaluation
All patients were permitted to stand or walk from the first postoperative day forward and were advised to wear a lumbar brace for 3 months. Regular follow-ups with flexion/extension lumbar radiographs were scheduled postoperatively at 3 months, and then every 6 months. Data were collected regarding operative parameters such as operative time, blood loss, duration of postoperative hospital stay, and operative complications. For clinical outcome assessment, the Oswestry Disability Index (ODI) [4], ten-point visual analog scale (VAS) for back pain (0–10) and Patient Satisfaction Index (PSI) [1] were recorded immediately before and 2 years after the operation. The Patient Satisfaction Index is scored from the patient’s answer to the question: “Would you undergo the same operation for the same result?” The answers were categorized as follows: 1 = definitely no, 2 = probably no, 3 = I don’t know, 4 = probably yes, 5 = definitely yes. Radiological fusion was determined with plain flexion/extension radiographs. The fusion was regarded as successful when definite bony continuity, or increase in bone density between the L5 and S1 vertebrae without motion was seen on flexion/extension radiographs. All patients were assessed by an independent observer who had no role in the treatment of the patients at any stage. In statistical analysis, the t-test, Chi-square, and Fisher’s exact test were used to compare results of the laparoscopic versus the open mini-ALIF. A P-value of less than 0.05 was considered statistically significant.
Results
Patient population
Patients’ demographic data are summarized in Table 1.
Table 1.
Characteristics of the patients in the laparoscopic and open mini-anterior lumbar interbody fusion (ALIF) groups
| Laparoscopic | Mini-open | Statistics | |
|---|---|---|---|
| No. of cases | 22 | 22 | |
| Sex: M/F | 5/17 | 6/16 | NS* |
| Mean (range) age: years | 49 (27–67) | 50 (31–66) | NS* |
| Abdominal surgery history: n | 4 | 5 | |
| Disc surgery historya: n | 1 | 2 | |
| Mean (range) follow-up: months | 43 (36–49) | 30 (24–40) | NS* |
*Not significant; chi-square test for sex ratio, t-test for age and follow-up
a History of L5–S1 disc surgery by posterior approach
Of the 54 cases originally identified for the study, ten were not included in the analysis of final outcome: three cases in group 1 were converted to open procedure and, among the rest, five were lost to follow up in group 1 and two in group 2. Thus 22 patients in group 1 and 22 patients in group 2 were included in the analysis. The reasons for open conversion were malposition of the cage, excessive bleeding from the middle sacral vessels, and trocar site bleeding.
In group 1 there were 5 men and 17 women with a mean age of 49 years (range 27–67 years). Among them, four patients had a history of previous abdominal operation and one had undergone a posterior approach for L5–S1 discectomy. The mean follow-up duration was 43 months (range 36–49 months).
In group 2 there were 6 men and 16 women with a mean age of 50 years (range 31–66 years). Among them, five patients had a history of previous abdominal operation and two of posterior approach for L5–S1 discectomy. The mean follow-up duration was 30 months (range 24–40 months). The difference in sex ratio, mean age, and follow-up duration between the two groups was not statistically significant.
Perioperative parameters
The mean operative time was 158 min (range 90–330 min) in group 1 and 83 min (range 40–150 min) in group 2. The difference was statistically significant (t-test, P=0.001). Blood loss and postoperative hospital stay did not differ significantly (Table 2).
Table 2.
Perioperative parameters of the cases: mean (range) values and statistical significance
| Laparoscopic (N=27) | Mini-open (N=24) | P-value | |
|---|---|---|---|
| Operative time (min) | 158 (90–330) | 83 (40–150) | 0.001 |
| Estimated blood loss (ml) | 85 (10–300) | 68 (50–150) | NS* |
| Hospital stay after operation (days) | 3.9 (2–7) | 3.4 (2–6) | NS* |
*Not significant (t-test)
Clinical and radiological outcome
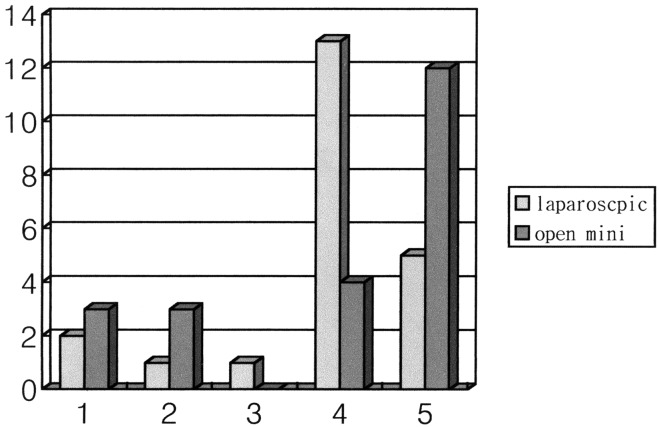
The results are summarized in Table 3. There was no statistical difference between the groups in preoperative or postoperative pain score, nor in the change between pre- and postoperative pain score or ODI score. Results on the PSI are shown in Fig. 1. Five patients in group 1 and 12 in group 2 recorded the top score for satisfaction. Satisfactory outcome, defined as 4 or 5 on the PSI, was achieved in 82% (18/22) and 73% (16/22) in the respective groups. The difference was not significant (Fisher’s exact test).
Table 3.
Outcome and operative complications of the cases: mean (range) values and statistical significance (Δ change from preoperative value, VAS ten-point visual analog pain score, ODI Oswestry Disability Index, Cx complications)
| Laparoscopic | Mini-open | P-value | |||||
|---|---|---|---|---|---|---|---|
| Preop | Postop | Δ | Preop | Postop | Δ | ||
| VAS | 9.1 (5–10) | 4.0 (1–10) | 5.1 (0–8) | 9.4 (7–10) | 3.7 (1–10) | 5.5 (0–9) | NS* |
| ODI | 41 (14–68) | 25 (2–62) | 38 (−20–93) | 43 (22–62) | 23 (0–60) | 47 (−53–100) | NS* |
| Cx | 3 | 2 | |||||
| Nonunion | 2 | 2 | |||||
* Not significant (t-test)
Fig. 1.
Patient Satisfaction Index in laparoscopic and open mini-ALIF groups, scored from the patient’s answer to the question: “Would you undergo the same operation for the same result?” The answers were categorized as follows: 1 = definitely no, 2 = probably no, 3 = I don’t know, 4 = probably yes, 5 = definitely yes
In group 1 there were three perioperative complications: one cage malposition, one case of retrograde ejaculation, and one case of bladder dysfunction. In group 2 there was one case of deep vein thrombosis and one case of bladder dysfunction. Ultimately, the patient with cage malposition developed symptomatic pseudoarthrosis.
The operative scar was confined to a small dimple near the umbilicus in group 1, while definite scarring with some wrinkling was common in group 2.
Discussion
Surgical approaches using an endoscopic technique are becoming more widespread in spine surgeries. The development of laparoscopic ALIF is the result of the established effectiveness of ALIF in the treatment of degenerative disc disease, internal disc disruption, and pseudoarthrosis, and advancement of modern endoscopic equipment and technique development. Most reports in the literature conclude that the results of laparoscopic surgery are promising and encouraging [12, 13, 18, 22, 23, 24, 27]. Since Obenchain [17] first performed laparoscopic discectomy in 1991, Mathews et al. [13], Olsen et al. [18], Regan et al. [22], and Zucherman et al. [27] have all reported on the technical feasibility of laparoscopic ALIF of L5–S1. Mahvi and Zdeblick [12] first reported the approach to L4–5 in 1996. Although there were technical difficulties in exposing the L4–5 space, Regan et al. [23] proved the feasibility of the technique and demonstrated promising perioperative results in their series of 58 cases. Moreover, Regan et al. [24] reported a prospective multicenter study for laparoscopic ALIF of L4–5 and L5–S1. It was concluded that the laparoscopic procedure is associated with a learning curve, but once mastered, it is effective and safe when compared with open techniques of fusion.
However, there are several points for consideration. The purpose of minimally invasive surgery is not a simple reduction in the size of the skin incision, but rather reducing to a minimum the physical trauma inflicted on the patient, while achieving the maximum therapeutic result [5, 15]. Endoscopic access procedures may be unfamiliar to the surgeon and may result in an overextended operation time compared to open procedures. The endoscopic views are two-dimensional and may cause disorientation due to magnification and lack of physical verification by the surgeons. Laparoscopic fusion involves dissection or retraction of major organs such as great vessels, intestine and sympathetic trunk. These factors may lead to a high incidence of complications [10, 12, 13, 18, 24, 26]. Moreover, the biomechanical stability provided by anterior interbody fusion cages has often been questioned [7, 20], and a wide range of successful fusion rates have been reported [2, 3, 6, 9, 11, 16, 17]. With a laparoscopic approach, it has proven to be more difficult to achieve sufficient immediate stability for a high rate of fusion [25].
Open but less invasive techniques are also available. With properly designed self-holding spreaders, the open mini-ALIF can be performed using a skin incision of less than 5 cm [14, 15]. Because the laparoscopic approach needs four 1-cm-long stab wounds, the length of total skin incision is similar.
The purpose of this study was to compare perioperative parameters and long-term clinical and radiological outcome between patients treated with laparoscopic fusion and those treated with open mini-ALIF for L5–S1 fusion with the same intervertebral device, and if possible, to find any objective benefit of laparoscopic fusion.
Examination of perioperative parameters revealed that only the operative time differed significantly between the two groups, while blood loss and postoperative hospital stay did not. The mean operative time in the laparoscopic approach was nearly double that of open mini-ALIF, but it was similar to previous reports. A shorter operative time in the open mini–ALIF group compared to previous reports made the difference greater [24]. Among the complications, we think our one case of malpositioned cage was due to a loss of cage orientation.
To summarize the results after a follow-up of more than 24 months, the clinical outcomes of the patients in the two groups were not significantly different in pain scores or ODI. The fusion rate was not lower in the laparoscopic group. The proportions of patient who ranked their surgical result as satisfactory or highly satisfactory were similar in the two groups. These results, when taken together, indicate that laparoscopic ALIF has similar effectiveness in the treatment of L5–S1 discogenic pain to open surgery. However, the results of PSI indicate that the percentage of highly satisfied patients in the open mini-ALIF group was higher than that in the laparoscopic group. This may be a disappointing result to a surgeon who performed a surgery that is technically demanding and time-consuming, since one of the main goals of minimally invasive surgery is to achieve higher patient satisfaction.
There may be several factors that influence patient satisfaction as juxtaposed to the surgical results. These may include the degree of improvement of the main symptom, suffering from postoperative pain, size of operation scar, functional status at present, and compensation status. Yet, based on the results presented here, we cannot conclude that the laparoscopic approach was more successful in achieving higher satisfaction than the open approach.
The ideal surgical approach for lumbar fusion remains undetermined, despite the efforts of many investigators. To achieve a better surgical outcome, we should continue to develop minimally invasive techniques such as endoscopic approaches, open but less invasive techniques, or any combination of these. However, the authors believe that the techniques should be regularly evaluated for their effectiveness and safety, and should not be used for expanded inappropriate indications.
Conclusion
Laparoscopic ALIF for L5–S1 showed similar clinical and radiological outcome when compared with open mini-ALIF, but significant advantages were not identified in spite of its technical difficulty.
References
- 1.Barrick Spine. 2000;25:853. doi: 10.1097/00007632-200004010-00014. [DOI] [PubMed] [Google Scholar]
- 2.Chow Spine. 1980;5:452. doi: 10.1097/00007632-198009000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Crock Clin Orthop. 1982;165:157. [PubMed] [Google Scholar]
- 4.Fairbank Physiotherapy. 1980;66:271. [PubMed] [Google Scholar]
- 5.Fitzpatrick Br J Surg. 1990;77:721. doi: 10.1002/bjs.1800770702. [DOI] [PubMed] [Google Scholar]
- 6.Greenough Eur Spine J. 1994;3:225. doi: 10.1007/BF02221598. [DOI] [PubMed] [Google Scholar]
- 7.Holte Eur Spine J. 1994;3:32. doi: 10.1007/BF02428314. [DOI] [PubMed] [Google Scholar]
- 8.Katkhouda N, Campos GM, Mavor E, Mason RJ, Hume M, Ting A (1999) Is laparoscopic approach to lumbar spine fusion worthwhile? Am J Surg 178:458–461 [DOI] [PubMed]
- 9.KimSpine 19992481210222534 [Google Scholar]
- 10.Lieberman Spine. 2000;25:509. doi: 10.1097/00007632-200002150-00019. [DOI] [PubMed] [Google Scholar]
- 11.Loguidice Spine. 1988;13:366. doi: 10.1097/00007632-198803000-00027. [DOI] [PubMed] [Google Scholar]
- 12.Mahvi Ann Surg. 1996;224:85. doi: 10.1097/00000658-199607000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mathews Spine. 1995;20:1797. doi: 10.1097/00007632-199508150-00009. [DOI] [PubMed] [Google Scholar]
- 14.Mayer Spine. 1997;22:691. doi: 10.1097/00007632-199703150-00023. [DOI] [PubMed] [Google Scholar]
- 15.Mayer Eur Spine J. 2000;9:S35. doi: 10.1007/PL00010020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.NewmanSpine 1992178311502649 [Google Scholar]
- 17.Obenchain J Laparoendosc Surg. 1991;1:145. doi: 10.1089/lps.1991.1.145. [DOI] [PubMed] [Google Scholar]
- 18.Olsen Surg Endosc. 1996;10:1158. doi: 10.1007/s004649900270. [DOI] [PubMed] [Google Scholar]
- 19.Penta Spine. 1997;22:2429. doi: 10.1097/00007632-199710150-00021. [DOI] [PubMed] [Google Scholar]
- 20.Rathonyi Eur Spine J. 1998;7:400. doi: 10.1007/s005860050097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reddick Surg Endosc. 1989;3:131. doi: 10.1007/BF00591357. [DOI] [PubMed] [Google Scholar]
- 22.Regan Surg Laparosc Endosc. 1996;6:459. doi: 10.1097/00019509-199612000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Regan Spine. 1999;24:2171. doi: 10.1097/00007632-199910150-00018. [DOI] [PubMed] [Google Scholar]
- 24.Regan Spine. 1999;24:402. doi: 10.1097/00007632-199902150-00023. [DOI] [PubMed] [Google Scholar]
- 25.Riley Spine. 1997;22:1407. doi: 10.1097/00007632-199706150-00021. [DOI] [PubMed] [Google Scholar]
- 26.Zdeblick Spine. 2000;25:2682. doi: 10.1097/00007632-200010150-00023. [DOI] [PubMed] [Google Scholar]
- 27.Zucherman Spine. 1995;20:2029. doi: 10.1097/00007632-199509150-00015. [DOI] [PubMed] [Google Scholar]