Abstract
A new instrumentation system for ventral stabilization of the spine that can be used for an endoscopic and minimally invasive approach was developed. We describe the implantation technique and report on the first clinical results. This prospective study covers the first 45 patients to undergo this new technique since it was introduced in 1999. In all patients the operation was successfully performed in a completely minimally invasive procedure. Mono- and bisegmental stabilization was performed mainly at the thoracolumbar junction after initial posterior instrumentation in most cases. Lesions varied from fresh/old fractures to metastases (T5–L3). Pre- and postoperative follow-up included clinical examination and radiological visualization via X-ray and computed tomographic scan. Our experience with this minimally invasive procedure demonstrated the feasibility of the method.
Keywords: Thoracolumbar burst fractures, Spinal stabilization, Spinal decompression, Video-assisted thoracoscopic surgery
Introduction
Minimally invasive techniques are becoming more widespread in the surgical subspecialties. Standard open surgical procedures are being modified to become less invasive, with the intention of reducing recovery time, morbidity, and ultimately expenditure. Improvements in technology have allowed the surgeon to enter body cavities and create potential spaces such as the retroperitoneum by diaphragm splitting. Improved fiber optics, light sources, and use of 30° angled optic cameras have resulted in improved visualization of the structures surrounding the spine [1, 3, 4, 5, 6, 7, 8, 9, 10, 11, 13, 15, 16, 17, 18, 20, 21, 22, 23]. Indications for endoscopic spinal surgery are degenerative diseases, infection, tumor, fracture, and ventral release for scoliosis and kyphosis. This minimally incisional technique provides a feasible alternative to thoracotomy or posterolateral approaches for decompression and vertebral body reconstruction. Long distance overbridging by strut graft and stabilization plays an important role, especially in cases of fracture treatment with the need for spinal decompression, sometimes of several segments. However, there is a lack of adequate instrumentation systems. In the early days of endoscopic thoracolumbar fracture treatment, the established standard intervention was performed after dorsal intervention and reduction and secondary mono- or bisegmental ventral strut grafting with overbridging by four-point stabilization with the Z-plate. However, the Z-plate normally is intended for an open implantation technique. Only time-consuming improvisation, such as screw fixation with strings to prevent loosening, make it applicable in these cases [1, 4, 19]. McAfee, Regan and Bühren concluded that the limiting factor in the wide application of the endoscopic technique is the absence of a commercially available internal fixation system for this endoscopic approach [4, 17, 21].
The purpose of this study was to prospectively evaluate the feasibility, safety and efficacy of a newly developed anterior stabilization system that allows a complete video-assisted minimally invasive stabilization from T4 to L3 in patients suffering from fractures or other pathologies.
Materials and methods
Instrumentation system and technique
A new totally endoscopically implantable system for the treatment of fractures from T4 to L3 was developed (Fig. 1). This modular anterior construct system (Modular Anterior Construct System Thoracic Lumbar—MACS TL; Aesculap, Tuttlingen, Germany) allows an endoscopic approach and thoracoscopic instrumentation from T4 to L1, endoscopic diaphragm splitting and thoracoscopic instrumentation to L2, and a minimally invasive retroperitoneal approach to L3/4 for fracture stabilization. As a twin screw concept, it obtains a rigid-angle stable monocortical anchorage by means of two convergent polyaxial screws in each vertebral body and a low-profile plate (<10 mm) or rods. The system is conceived for mono- and multisegmental (rods) stabilization. The self-cutting screws are both connected with the fracture overbridging plate by means of a polyaxial clamping element (Fig. 1). The cannulated posterior polyaxial screw can be inserted over a K-wire, its length ranges from 25 to 50 mm, the diameter is 7.0 mm and the angle of rotation is 14°. The direction of the anterior stabilization screw is given by the clamping element, which ranges in length from 25 to 50 mm and has a diameter of 6.5 mm. A locking mechanism in the clamp prevents the anterior screw from backing out. Plates are available in a variety of lengths, from 45 to 100 mm; rods are available up to 200 mm. Locking nuts and screws guarantee a rigid fixation between overbridging plate, clamping elements, and screws. Additionally, a bone graft clamp can be used to fixate the bone graft with a screw.
Fig. 1.

MACS TL system: twin screw concept
The whole operative endoscopic procedure is performed in a stable lateral position via three intercostal working channels and one optical channel under general anesthesia with one-lung ventilation. The polyaxial clamp and the pre-assembled posterior cannulated screw have to be endoscopically inserted with the help of a centralizer over a K-wire positioned under fluoroscopic control (Fig. 2). This centralizer guarantees an easy application of all implant parts and instruments needed for the endoscopic procedure. The clamping element has to be orientated such that the hole for the anterior stabilization screw comes to lie anteriorly. After K-wire removal through a cannulated instrument, this procedure has to be repeated in the other adjacent vertebral body (Fig. 3). Then discectomy or corpectomy and decompression of the spinal cord can then be achieved and proper preparation of the graft bed and graft placement is done. Measuring the distance between the connecting elements and adding 25 mm established the exact length of the plate. Afterwards, this fitting plate can be laid onto the connecting elements by introducing it lengthwise into the chest cavity and fixated by the fixation nuts (Fig. 3). Now the assembly has to be brought into the final position directly onto the surface of the vertebral bodies by tightening the polyaxial screws. Finally, the anterior screw is fixed in the connecting element and the locking screw guarantees rigid four-point stabilization. Locking nuts have to be tightened with a torque of 15 Nm, locking screws with 10 Nm using an appropriate torque wrench.
Fig. 2.
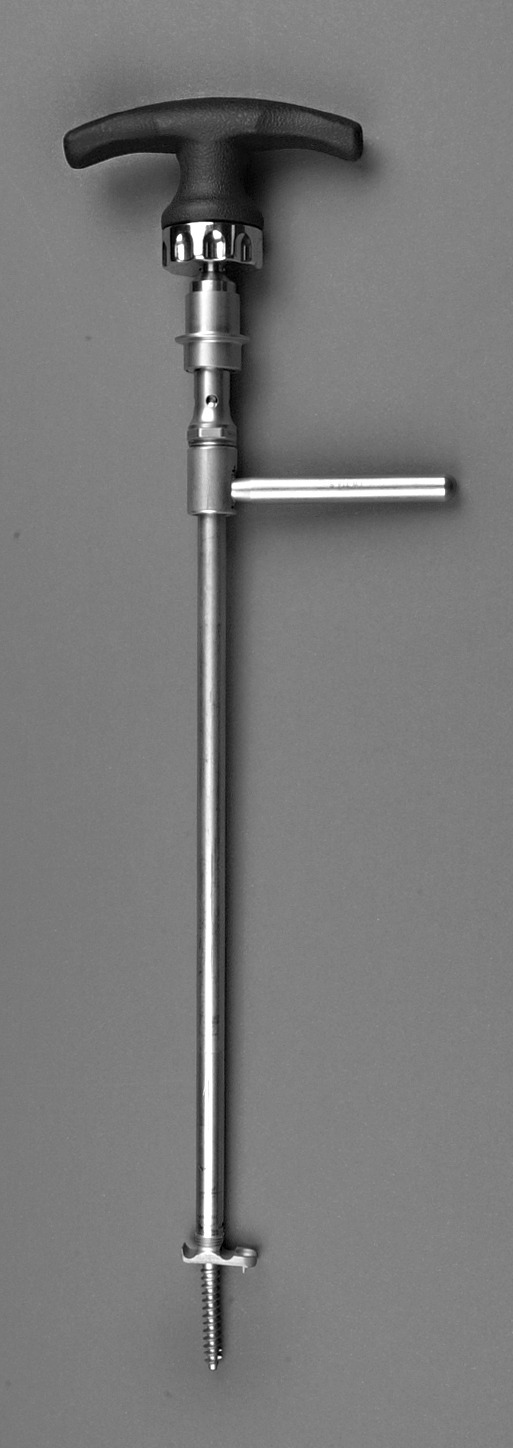
Assembled insertion instruments with centralizer, preassembled clamp and posterior screw
Fig. 3.
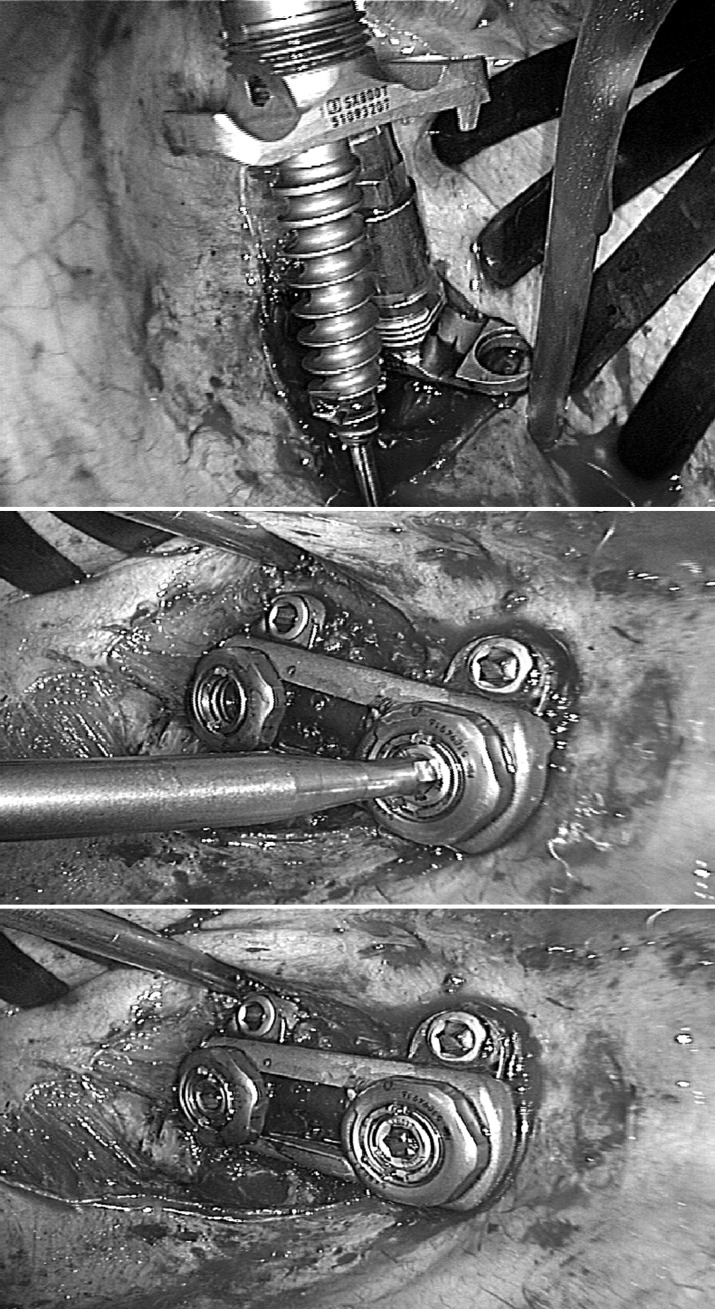
Intraoperative endoscopic view of the insertion of the screw over the K-wire (top), fixation of the plate (middle), and final instrumentation (bottom)
Clinical prospective study
Between December 1999 and December 2002 the authors operated on 45 consecutive patients with the MACS TL system. Patients with fresh fractures (n=33) and other pathologies (n=12) [old fractures (n=2), tumors (n=6), spondylitis (n=3), osteoporotic fractures (n=1)] were treated (Table 1, Table 2). The mean age of the 21 female and 24 male patients was 44 years (range 16–78 years). Indications for operative treatment were restrictively evaluated according to the Magerl classification after preoperative X-ray and computed tomographic scan individually and independently from the technique of an anterior procedure.
Table 1.
Clinical data of the patients with fresh fractures. There were no cases of iatrogenic injury or implant loosening, and only one case of infection and one case where the minimally invasive procedure had to be changed to an open procedure
| Patient | Sex | Age | Follow-up | Level | AO type | Stabilization | Procedure | Spacer | Instrumented level | Time | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | F | (months) | Ventral | Dorsal | Endoscopic | Minimally invasive | Open | Iliac crest | Tutogen | Synex | (min) | |||||
| 1.a HX | x | 55 | 37 | T11 | A33 | x | x | x | T10/ T12 | 130 | ||||||
| 2. FA | x | 46 | 37 | L1 | A33 | x | x | x | x | T12/ L2 | 200 | |||||
| 3. MR | x | 45 | 36 | L2 | C | x | x | x | x | L1/ L3 | 130 | |||||
| 4. KW | x | 40 | 35 | T12 | A33 | x | x | x | x | T11/ L1 | 150 | |||||
| 5. FG | x | 33 | 32 | L1 | A32 | x | x | x | x | T12/ L2 | 110 | |||||
| 6. KM | x | 49 | 35 | L1 | B | x | x | x | x | T12/ L1 | 180 | |||||
| 7. DF | x | 54 | 31 | L1 | A33 | x | x | x | x | T12/ L1 | 180 | |||||
| 8. HM | x | 25 | 31 | L3 | B | x | x | x | x | L2/ L4 | 180 | |||||
| 9. SS | x | 21 | 30 | L3 | A31 | x | x | x | L2/ L3 | 195 | ||||||
| 10. MG | x | 18 | 30 | T12 | A33 | x | x | x | x | T11/ L1 | 110 | |||||
| 11. MW | x | 62 | 28 | T12 | A33 | x | x | x | x | T11/ L2 | 240 | |||||
| 12. BL | x | 16 | 26 | L3 | A33 | x | x | x | x | L2/ L4 | 210 | |||||
| 13. KN | x | 40 | 26 | L2 | A33 | x | x | x | x | L2/ L3 | 130 | |||||
| 14. RJ | x | 28 | 26 | L3 | A32 | x | x | x | L2/ L3 | 150 | ||||||
| 15. FC | x | 54 | 23 | L3 | A33 | x | x | x | x | L2/ L4 | 130 | |||||
| 16. SJ | x | 63 | 23 | L1 | A33 | x | x | x | x | T12/ L1 | 130 | |||||
| 17.b BI | x | 78 | 18 | T12 | A33 | x | x | x | x | x | T11/ L2 | 120 | ||||
| 18. SC | x | 58 | 17 | L1 | A33 | x | x | x | x | T12/ L2 | 210 | |||||
| 19. JV | x | 33 | 16 | T11 | C | x | x | x | x | T10/ T12 | 200 | |||||
| 20. NF | x | 39 | 15 | L1 | A31 | x | x | x | T12/ L1 | 120 | ||||||
| 21. GA | x | 39 | 14 | L1 | A33 | x | x | x | x | T12/ L1 | 120 | |||||
| 22. DH | x | 35 | 12 | L1 | A31 | x | x | x | x | T12/ L1 | 130 | |||||
| 23. SH | x | 60 | 11 | L2 | C | x | x | x | x | L1/ L3 | 160 | |||||
| 24. TU | x | 35 | 10 | L1 | C | x | x | x | x | T12/ L1 | 180 | |||||
| 25. BS | x | 17 | 8 | L1 | A31 | x | x | x | x | T12/ L1 | 120 | |||||
| 26. SE | x | 53 | 7 | L2 | C | x | x | x | x | L1/ L3 | 120 | |||||
| 27. KE | x | 43 | 6 | T12 | A31 | x | x | x | x | T11/ L12 | 120 | |||||
| 28. SS | x | 37 | 5 | L1 | A32 | x | x | x | x | T12/ L2 | 180 | |||||
| 29. XW | x | 39 | 5 | L3 | A33 | x | x | x | x | L2/ L4 | 180 | |||||
| 30. HR | x | 19 | 3 | T8/9 | C | x | x | x | x | T7/ T10 | 150 | |||||
| 31. EF | x | 38 | 3 | L2 | A33 | x | x | x | x | L1/ L3 | 150 | |||||
| 32. KE | x | 44 | 2 | L1 | A33 | x | x | x | x | T12/ L2 | 140 | |||||
| 33. CJ | x | 43 | 1 | T12 | A32 | x | x | x | x | T11/ L1 | 180 | |||||
a Patient suffered a postoperative infection
b Minimally invasive procedure in this patient was changed to an open procedure
Table 2.
Clinical data of the patients with other pathologies [Sp spondylitis, Tu tumor, Cor: secondary correction (old fracture), O osteoporotic fracture]. There was only one case of implant loosening, due to tumor, and one case of iatrogenic injury, requiring switching to an open procedure. In no other patient did the procedure have to be changed, and there were no cases of infection
| Patient | Sex | Age | Follow-up | Level | Pathology | Stabilization | Procedure | Spacer | Instrumented level | Time | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | F | (months) | Ventral | Dorsal | Endoscopic | Minimally invasive | Open | Iliac crest | Tutogen | Synex | (min) | |||||
| 1. EE | x | 74 | 30 | T6/7 | Sp | x | x | x | x | T 3/T7 | 180 | |||||
| 2. PW | x | 31 | 28 | L3/4 | Tu | x | x | x | x | x | x | L2/ L5 | 110 | |||
| 3. HB | x | 34 | 24 | T12/1 | Tu | x | x | x | x | x | T11/ L2 | 180 | ||||
| 4. GM | x | 54 | 21 | T11/12 | Tu | x | x | x | x | x | T10/ L3 | 250 | ||||
| 5. RE | x | 74 | 21 | L2/3 | Sp | x | x | x | x | L1/ L4 | 180 | |||||
| 6. KC | x | 20 | 15 | L2 | Cor | x | x | x | L1/ L3 | 143 | ||||||
| 7. ES | x | 27 | 14 | L1 | Cor | x | x | x | x | L1/ L3 | 145 | |||||
| 8.a LM | x | 49 | 10 | L1 | Tu | x | x | x | x | T12/ L2 | 180 | |||||
| 9. DA | x | 68 | 7 | L2/3 | Tu | x | x | x | x | L1/ L4 | 120 | |||||
| 10. JN | x | 68 | 7 | L2/3 | Sp | x | x | x | x | L1/ L3 | 180 | |||||
| 11. HE | x | 63 | 3 | L1 | Tu | x | x | x | x | T12/ L2 | 130 | |||||
| 12.b WW | x | 71 | 0 | T12 | O | x | x | x | x | T11/ L1 | 150 | |||||
a Tumor led to implant loosening
b Iatrogenic injury of the lung occurred, requiring swapping to an open procedure
According to the nature of the injury and the AO classification, patients with type B and C distraction and rotation elements or patients with a neurological deficit associated with higher-grade structural damage to the vertebral body were stabilized combined. In some type A compression injuries, a ventral procedure was performed either exclusively, or with mono- or bisegmental stabilization. Indications for an additional anterior procedure were a significant narrowing of the spinal canal and/or reconstruction of the weight-bearing column in the case of higher-grade structural damage and anterior malalignment.
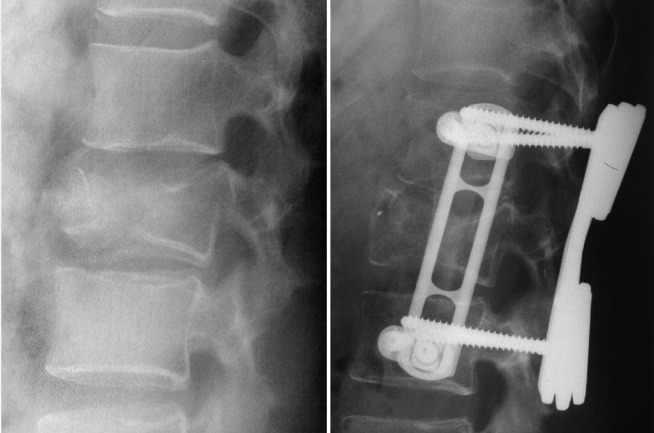
Most patients underwent posterior stabilization under emergency conditions, in cases of neurological deficits with laminectomy, using the Universal Spine System (USS, Stratec Medical, Umkirch, Switzerland) or the Compression Plate System (Litos, Hamburg, Germany) for posterior instrumentation (Fig. 4).
Fig. 4.
Clinical example: fracture of T12 preoperative (left) and postoperative with ventrodorsal stabilization (right)
The patients were followed up with standardized radiographs immediately after surgery and at follow-up, 2, 6, 12 and 24 months after surgery. A CT scan was performed after dorsal stabilization before the anterior procedure and after second-stage ventral stabilization. The functional and subjective outcome was assessed with clinical examinations.
Follow-up outcome parameters used in this initial pilot study included iatrogenic injury to large vessels, injury to central or peripheral nerve structures, sympathetic deafferentation symptoms or sympathectomy syndromes, injury to the organs in the thoracic and upper abdominal cavity, operation time, swapping from the minimal invasive to open procedure, infection, implant loosening or graft dislocation and implant removal.
Operative technique
Due to the organs in the thoracic (heart, vascular situation) and upper abdominal cavity (liver) a left-sided position is preferred for the treatment of lesions from T4 to T8, whereas for the approach to the thoracolumbar junction (T9–L2), right-sided positioning is preferred with a minimal incision of the diaphragm, which allows a retroperitoneal approach down to the level of L2. Lesions affecting the spine below L2 were approached through a minimal retroperitoneal access from the left side. The decision for the approach was taken in each individual case based on the preoperative CT scans.
Double lung intubation was used, which must be checked bronchoscopically, but no other specific anesthesiological monitoring is needed with a thoracoscopic approach. In all cases, except tumor and infection, blood saving techniques by cell saver were used. A single dose of a second-generation cephalosporine was given prior to surgery. According to the NASCI III protocol, steroids were given in all cases of neurology [2].
Before operation the position and free tilt of the C-arm was checked and the projection of the target area as well as the optical and working channels were marked under fluoroscopic control on the skin with a water-resistant pen. The surgeon stands behind the patient together with a camera assistant, the first assistant is located on the opposite side.
In this stable lateral position in general anesthesia with one-lung ventilation, the operation started directly over the target area with a 4- to 6-cm skin incision followed by a mini-thoracotomy. The muscle layers of the thoracic wall were cut through following the directions of the fibers with a zigzag incision, and the opening was gradually widened by the insertion of Langenbeck hooks. The pleura was perforated after collapsing the lung through commencing single-lung ventilation, and a spreader or frame was placed.
The optical channel (10-mm black trocar) was then placed two to three intercostal spaces cranial to the injured vertebra in the spinal axis under video-visualization by the thoracoscope installed in the working channel. The channels for suction/irrigation (10-mm black trocar) and retractor for lung or diaphragm (10-mm black trocar) were placed about 5–10 cm anterior to the working and optical channel. The operating field was identified after illumination by the thoracoscope, and diaphragm or lung tissue were removed with the help of the retractor (Endo Paddle Retract, Auto Suture, Norwalk, US). After orientation and identification of the exact level of the spine by an image intensifier, diaphragm splitting was performed with monopolar cauterization if necessary. Overlying muscle or retroperitoneal fat tissue were dissected bluntly from the lateral side of the vertebral body, taking care not to damage segmental blood vessels. The segmental vessels of the fractured vertebra were mobilized and clipped, and sometimes those of the adjacent vertebra as well, if that was necessary for preparation of the screw placement. The branches of the sympathetic chains were identified and, if possible, preserved. After localization under fluoroscopic control, the K-wire placement was performed, as described above, followed by insertion of the dorsal polyaxial screws in the adjacent vertebrae in case of bisegmental stabilization. The two screws in the adjacent vertebra were landmarks for the following decompression and corpectomy. With the help of these markers, orientation of the spinal axis and distance to the spinal canal is possible. With a long osteotomy, the extent of the planned corporectomy is defined. Resection of the adjacent discs followed, and the fragmented parts were removed carefully under video assistance with long rongeurs. With the help of video magnification, posterior fragments of the vertebra that occupy the spinal canal could be carefully resected. Finally, preparation and measurement of the graft bed, and strut grafting were performed. Autologous tricortical bone graft from the iliac crest or bovine bone cages (Tutogen, Tutogen Medical GmBh, Neunkirchen, Germany) in adequate length in press-fit technique were inserted through the working channel, and a slight reduction was performed manually by pressure on the spinous processes in the case of a single anterior approach. If more correction of the spinal alignment was necessary, extendable cages (Synex, Stratec Medical, Oberdorf, Switzerland) were implanted; the cages were also used in our tumor patients. Afterwards, the instrumentation was finished as described above (Fig. 3). If necessary, the diaphragm was closed with sutures using a common endoscopic technique. A chest tube placed in the costodiaphragmatic recess was inserted. All portals were closed with sutures after removal of the trocars.
In all cases below L2, a video-assisted minimally invasive retroperitoneal open procedure was performed. The approach-related skin incision was up to 10 cm long. Blunt preparation of the retroperitoneal tissue with a wet sponge mounted on a stick and dissection of the muscles in the direction of their fiber orientation (external oblique, internal oblique, transverse abdominal muscles, psoas muscle) followed, taking care to preserve the ilio-hypogastric and ilio-inguinal nerves and the ureter. The created space was kept open with a self-retaining frame retractor (Miaspas Retroperitoneal Retractor System, Aesculap, Tuttlingen, Germany) and illuminated under video assistance with the 30° angled optic. The same previously mentioned procedure was now performed through this minimally invasive retroperitoneal approach with the described endoscopic instruments and minimally invasive implantable stabilization system.
Postoperative care took place in our intermediate care unit for one day while the patients were on a chest tube, after which they were cared for in the normal wards. Mobilization and ventilation training started on the 1st postoperative day without orthesis and with the help of a physiotherapist.
Results
According to the Magerl classification, 25 patients had A3 fractures, 2 had a B-type and 6 a C-type fracture [14]. Twenty-nine patients underwent initial posterior instrumentation in this fracture group (Table 1).
In the group of other pathologies, two patients needed revision of old fractures with kyphotic malalignment, three patients had destruction of the vertebra by spondylitis, six by tumor and one due to osteoporosis (Table 2).
Average total endoscopic operation time of the fracture-affected patients was 152 min, and it was 162 min for retroperitoneal minimally invasive surgery including our learning curve (Table 1). For the other pathologies, the average operation time was 162 min (Table 2).
In 20 patients with fractures, a thoracoscopic approach was chosen; in 13 patients with fractures of and below L2, a video-assisted minimally invasive retroperitoneal approach was performed. Other pathologies were treated as shown in Table 2.
A right-sided approach was chosen in 2 cases, and a left-sided approach in 43 cases. Decompression and clearance of the spinal cord was performed in 37 patients. Autologous iliac crest was inserted in 28 patients, Tutogen bones in 4 and Synex cages in 13. Average blood loss was negligible.
Two intraoperative complications occurred, related in particular to the minimally invasive technique. One approach had to be enlarged to 15 cm in a 78-year-old female patient because of an adhesion of the lung to the pleura, and one iatrogenic injury of the lung occurred during a mini-thoracotomy in a 71-old-patient, which required swapping to open procedure. There were no vascular or visceral complications, and in particular no other injuries of the lung and no iatrogenic neurological injuries. There were no implant components or connection-related intraoperative complications. Bilateral lung ventilation was unproblematic after stabilization. In all cases, lung ventilation and general anesthesia were terminated immediately after the operative intervention. No hernia or paresis of the diaphragm were recorded. One superficial wound infection occurred, which responded well to treatment with vacuum sealing and oral antibiotics.
In the follow-up so far, no implant breakage has occurred, but there was one case of implant loosening and screw loosening in the adjacent vertebra due tumor progress. No radiological or clinical signs of screw loosening were observed in any of the other examined patients (Table 1, Table 2).
Discussion
A new ventral instrumentation system for endoscopic and/or minimally invasive and open treatment for lesions of the spine was developed. In this clinical prospective pilot study, its feasibility was demonstrated in a series of 45 patients with different indications.
Our preliminary results demonstrate that the implantation of the system is safe and easy to perform with a thoracoscopically assisted and/or minimal invasive retroperitoneal approach. Even though our patients varied in the affected levels and types of lesions, no intraoperative complications occurred during fixation of the system. Two approach-related injuries of the lung occurred in elderly patients due to unforeseeable adhesions of the lung to the pleura. There were no implant-related complications such as loosening or failure of the instrumentation in the follow-up. This is accords with the results of a previous in vitro biomechanical study, which found this system had excellent primary stability in comparison to clinically well-established systems [24]. Nevertheless, the problem of sufficient anterior reduction remains unresolved with this new instrumentation system. A ratchet packaged with the system for the distraction maneuvers was shown to be not adequate for the reduction. Therefore, initial dorsal intervention is necessary for reconstruction of the spinal alignment. Furthermore, K-wire and screw placement are difficult in the region of the lower thoracolumbar spine (L2/L3) within a thoracoscopic approach and diaphragm splitting, because of the difficult maneuver angle involved in placing them horizontally and parallel placement to the endplate, especially in the presence of dorsal pedicle screws.
This study also demonstrates that, even using a specially adapted instrumentation system, endoscopic and minimally invasive techniques are unfamiliar procedures for the orthopedic surgeon. Overextended operation times and prolonged learning curves both for surgeons and also highly trained scrub nurses may be the result. In the early days of endoscopic thoracolumbar fracture treatment, the Z-plate was used for stabilization. However, the Z-plate normally is intended for an open implantation technique. Only time-consuming improvisation such as screw fixation with strings to prevent loosening allow it to be used in minimally invasive procedures. These disadvantages have been eliminated with the new system. Furthermore, the ambitious procedures investigated during the initial enthusiasm for endoscopic techniques have since been toned down to techniques that are more practicable and safe for well-trained orthopedic and spine surgeons to perform.
We prefer a minimal open, but still less invasive endoscopically assisted approach in contrast to the minimally invasive ventral technique described by Bühren et al. [4]. In all cases of strut grafting or extendable cages, a larger incision of the working channel must be performed. Therefore, we used this "enlarged" working channel from the start of the operation, with a spreader frame that makes the whole procedure easier to perform and more clear. The intermediate direct three-dimensional view, in contrast to the two-dimensional screen view, prevents disorientation of the surgeon and overestimation of the real situation due to magnification. This guarantees greater safety for the patient. Besides this, the repeated reinstallation of a speculum to enlarge the small skin incision of the working channel during the whole procedure is time consuming and may cause infection. Also, this "open window" makes it easier to manage complications, especially in tumor cases. This trend is favored by other groups, including Kossmann et al. and Mayer and co-workers [12, 15, 16].
In times of technical remodeling to improve minimally invasive endoscopic spine surgery, results of comparisons with open procedures regarding operation times and likely benefits of the minimally invasive operated patients such as blood loss, infection rate, postoperative kyphotic angle, pain reduction, costs and shorter hospitalization seem to be to published at a very early stage. A proper comparative evaluation will require more extended studies. However, our results of this preliminary study are comparable in these points with other studies on minimally invasive techniques [1, 3, 4, 6, 8, 9, 12, 16, 19, 21, 22].
Conclusions regarding the excellent feasibility of the demonstrated instrumentation technique with the new MACS TL system and the good short-term clinical results of this pilot study are warranted. Nevertheless, the ventral procedure should be carefully indicated.
References
- 1.Beisse Unfallchirurg. 1998;101:619. doi: 10.1007/s001130050315. [DOI] [PubMed] [Google Scholar]
- 2.Bracken JAMA. 1997;277:1597. doi: 10.1001/jama.277.20.1597. [DOI] [PubMed] [Google Scholar]
- 3.Buff Ther Umsch. 1997;54:529. [PubMed] [Google Scholar]
- 4.Buhren Chirurg. 1997;68:1076. doi: 10.1007/s001040050326. [DOI] [PubMed] [Google Scholar]
- 5.Connolly J Spinal Disord. 1996;9:453. [PubMed] [Google Scholar]
- 6.Cunningham Spine. 1998;23:1333. doi: 10.1097/00007632-199806150-00008. [DOI] [PubMed] [Google Scholar]
- 7.Hertlein Eur Spine J. 1995;4:302. doi: 10.1007/BF00301040. [DOI] [PubMed] [Google Scholar]
- 8.Huang Surg Endosc. 1997;11:1189. doi: 10.1007/s004649900566. [DOI] [PubMed] [Google Scholar]
- 9.Huang Arch Orthop Trauma Surg. 1998;117:92. doi: 10.1007/s004020050201. [DOI] [PubMed] [Google Scholar]
- 10.Huang World J Surg. 1997;21:358. doi: 10.1007/s002689900188. [DOI] [PubMed] [Google Scholar]
- 11.Karahalios Neurosurg Clin N Am. 1997;8:555. [PubMed] [Google Scholar]
- 12.Kossmann Eur Spine J. 2001;10:396. doi: 10.1007/s005860100330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mack Ann Thorac Surg. 1995;59:1100. doi: 10.1016/0003-4975(95)00112-x. [DOI] [PubMed] [Google Scholar]
- 14.Magerl Eur Spine J. 1994;3:184. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 15.Mayer HM (2000) Minimally invasive spine surgery. A surgical manual. Springer, Berlin Heidelberg New York
- 16.Mayer Spine. 1997;22:691. doi: 10.1097/00007632-199703150-00023. [DOI] [PubMed] [Google Scholar]
- 17.McAfee Surg Laparosc Endosc. 1995;5:339. [PubMed] [Google Scholar]
- 18.McAfee Spine. 1995;20:1624. doi: 10.1097/00007632-199507150-00012. [DOI] [PubMed] [Google Scholar]
- 19.Potulski Orthopade. 1999;28:723. doi: 10.1007/s001320050402. [DOI] [PubMed] [Google Scholar]
- 20.Regan J Spinal Disord. 1998;11:183. [PubMed] [Google Scholar]
- 21.Regan Clin Orthop. 1997;335:122. [PubMed] [Google Scholar]
- 22.Regan Spine. 1995;20:831. [PubMed] [Google Scholar]
- 23.Rosenthal J Neurosurg. 1998;89:224. doi: 10.3171/jns.1998.89.2.0224. [DOI] [PubMed] [Google Scholar]
- 24.Schultheiss Orthopade. 2002;31:362. doi: 10.1007/s00132-001-0276-7. [DOI] [PubMed] [Google Scholar]