Abstract
Back pain (BP) has been rated among the most important factors affecting physical health status in old age. Yet there is an under-representation of the older population in the BP literature. We present extensive interview data from the Longitudinal Study of Aging Danish Twins, dealing with a population-based sample of Danish twins aged 70–102, and describing the 1-month prevalence of BP and the development of BP over time. The associations between BP and education, self-rated health, other health problems, lifestyle factors, and physical and mental function were also investigated. Data were analysed in a cross-sectional analysis for all answers given at entry into the study and in a longitudinal analysis for participants in all four surveys. Associated factors were analysed for the cross-sectional sample using univariate and multivariate analysis accounting for the non-independence of twins in complete pairs. The overall 1-month prevalence of BP was 25% and differed significantly between men and women. The variations in prevalence between the age groups and over time were negligible. The majority of participants in all four surveys had either not experienced BP during the previous month or had done so on one occasion only. Education was not associated with BP. Self-rated health was associated with BP in a significant "dose-response" like pattern. BP was associated with bone and joint disorders, migraine headaches, lung disease, cardiovascular disorders and gastric ulcer, but not neurologic or endocrinologic diseases. BP sufferers had significantly lower scores on physical but not on mental functioning. We conclude that BP is a common symptom in old age; however, the prevalence does not change with increasing age. BP may be part of a more general syndrome of poor health among the old.
Keywords: Back pain, Co-morbidity, Epidemiology, Geriatrics, Prevalence
Introduction
A recent survey of over 100,000 Medicare beneficiaries aged 65 and older showed that heart and lung disease and back pain (BP) were the most important factors affecting the average physical health status of older Americans [6]. Yet out of the total body of publications on BP, surprisingly little research has focused on BP in old age, and there is an under-representation of the older population in the BP literature [3]. Furthermore, the authors of the most extensive review so far dealing with the prevalence of BP in old age found that results of published studies were difficult to interpret and compare, due to varying definitions of BP among the studies [3]. Consequently, at present it is not known with certainty how common BP is in senior age groups.
Little information is also available on the development and prognosis of BP over time late in life. In several cross-sectional studies the prevalence of BP has been estimated for old versus very old persons (i.e. 75–80- vs 81–85-year-olds), but results have been conflicting, ranging from a higher prevalence in oldest age groups [7, 17] over no difference [9], to a decreased prevalence with increasing age [1, 16, 24]. In none of these studies, however, were identical, repeated measurements performed in the same cohort, and the actual development of BP over time late in life has yet to be established.
BP in old age has been associated with osteoporosis [21] and, in particular, with vertebral fractures following osteoporosis [17, 20, 21]. However, BP appears to be highly associated with decreased physical functioning also in persons without osteoporosis or fractures [6, 27]. A closer look at patterns of co-occurrence of BP with other health conditions, lifestyle, socio-economic factors and self perceived health is therefore of interest in order to determine whether BP is a common but unique, and maybe negligible, symptom or whether it might be considered an indicator of more general poor health late in life.
BP, and in particular low back pain, are among the most prevalent conditions in the population as a whole, affecting some 70% of the population in their lifetime [26, 28] and resulting in staggering costs to society [2]. BP is, however, rarely a life-threatening condition, and the majority of these costs are related to disability payments and production losses [29], factors with little relevance in older age groups. This might explain the low priority assigned to BP in old age by both researchers and society as a whole. People aged 65 and older are, however, the fastest growing segment of the population all over the Western world [34], and more precise knowledge about the prevalence and impact of BP in this age group is desirable.
The present study is based on a large, population-based prospective cohort of Danish twins aged 70–102 years. We report data describing the 1-month prevalence of BP and the possible association with an extensive list of health problems, lifestyle factors, education and self-rated health. We also describe the development of BP over time among the survivors both at the group and at the individual level.
Materials and methods
Study population and data collection
The Danish Twin Registry includes twin pairs born in Denmark between 1870 and 1910 and same-sex twin pairs born between 1911 and 1930 [15]. The Danish Twin Registry is the basis for the Longitudinal Study of Aging Danish Twins (LSADT), which has previously been described in detail [4]. In brief, the first wave of LSADT comprised Danish twins who were aged 75 or older on 1 January 1995 (regardless of whether the co-twin was alive), a total of 3099 individuals. Face-to-face interviews were completed during a 3-month period (February–April 1995) by 100 trained interviewers; 2401 interviews were conducted, corresponding to a participation rate of 77% (7% completed by proxy) (Fig. 1). The response rate was significantly higher in men than in women (81 vs 74%) (P<0.01). The responders and non-responders were similar in terms of age. The mean age for responders and non-responders in both sexes was within 0.6 year of 81 years [4]. Two years later, the survey was repeated among the survivors from the 1995 wave, and among an additional 779 twins aged 73–76. The overall response rate in LSADT-97 was 79% (6% completed by proxy). In 1999, all surviving 1997 participants were contacted, as were twins who had turned 70 in the meantime. LSADT-99 had an overall participation rate of 70% (3% completed by proxy). Finally, in 2001, surviving 1999 participants plus twins who had turned 70 since 1999 were contacted. LSADT-01 had an overall participation rate of 80.7% (4% completed by proxy). The reason for proxy interview was most often that the participant suffered from dementia, and therefore data from all proxy interviews were excluded in the present study.
Fig. 1.
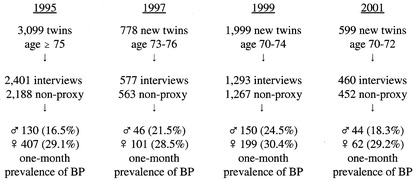
Overview of participation and self-reported 1-month prevalence of back pain (BP) at intake in the 1995, 1997, 1999, and 2001 waves of the Longitudinal Study of Aging Danish Twins (LSADT)
Back pain assessment
Back pain was assessed in all waves using the same question: "Have you during the past month suffered from back pain, acute low back pain or lumbago?"
Health and education
In all surveys the participants were asked whether a physician had ever told them that they suffered from various diseases. Participants who answered "Yes, previously" or "Yes, currently" were subsequently asked to confirm that this was a diagnosis made by a doctor, before the answer was accepted as valid. Participants were also asked about current or past smoking habits, years of school and education after school and self-rated health.
Functional abilities
Assessment of functional abilities was based on self-report, which has generally been found to be reliable and valid [18]. The instrument used has previously been validated in Denmark, and it has been shown to discriminate levels of functional abilities among community-dwelling elderly persons [31]. The instrument was expanded to further include information on the need for equipment or aids in relation to functional abilities [30], as well as all items from the Katz Index of Activities of Daily Living [22]. All items were rated on a 1 to 4 scale: 4 = can do without fatigue; 3 = can do with fatigue or minor difficulties; 2 = can do with aid or major difficulties; 1 = cannot do. Eleven items were after a factor analysis averaged into a Strength score [5]. The Strength score was adjusted for age and sex by subtracting an age-sex specific mean [5].
Cognitive state and functioning was measured using the Mini Mental State Examination (MMSE) [11].
Data analysis
BP prevalence was first assessed in a cross-sectional analysis, then in a longitudinal analysis both at the group and at the individual level, and, finally, associated factors were analysed using univariate and multivariate analysis.
Prevalence of back pain
Results from the four LSADT surveys were combined and answers given at entry into the study, i.e. the first time a subject participated in a survey, were used in the cross-sectional analysis. Sex-specific prevalence estimates with 95% confidence intervals (CI) were calculated for five-year age groups.
In the longitudinal analysis, prevalence rates of BP for subjects aged 75–84 in 1995 and participating again in the 1997, 1999 and 2001 waves were calculated to investigate whether the 1-month prevalence of LBP tended to change over time among the survivors. The number of times each individual survivor reported BP was also tabulated to study whether BP was most often a persistent or a passing symptom.
Co-morbidity and factors associated with BP
Co-morbidity and factors associated with BP were assessed using the cross-sectional sample, i.e. answers at intake into any of the four waves.
We compared co-occurring health indicators in participants with BP against those in participants without BP. The association of co-occurring health indicators and BP was estimated using a logistic regression model for categorical indicators (self-reported diseases, self-reported health, education, and smoking), and a multivariate linear regression model for continuous indicators (MMSE score, Strength score) controlling for age and sex.
To account for the non-independence of twins, twins from intact pairs (both twins in a pair participating) were analysed in clusters of two in all regression models.
For all analyses, the Stata statistical software package, release 6.0, was used [32].
Results
Prevalence
Out of 4486 participants included in the analysis (i.e. answers not provided by proxy) 4484 answered the question regarding BP within the past month. The overall 1-month prevalence of BP in this population-based sample of twins aged 70–102 years was 25% (95% CI 24–27%). The prevalence was significantly different for men and women [20% (CI 18–22%) vs 29% (CI 28–31%), P<0.00001] (Fig. 2). No statistically significant differences or consistently increasing or decreasing trends were found between the 5-year age groups in the cross-sectional analysis (Fig. 2). Similarly, in the longitudinal analysis, prevalence varied negligibly over time among the survivors from the 1995 wave both for men and women (Fig. 3). At the individual level, the vast majority of participants in all four LSADT waves had either not experienced BP during the month prior to any of the interviews (49%) or had done so on only one occasion (21%) (Table 1).
Fig. 2.
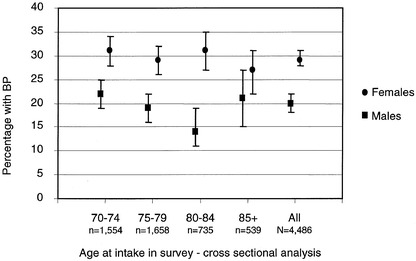
Prevalence of BP at intake according to age and sex among Danish twins aged 70+ from the 1995, 1997, 1999, and 2001 waves of the LSADT: cross-sectional analysis
Fig. 3.
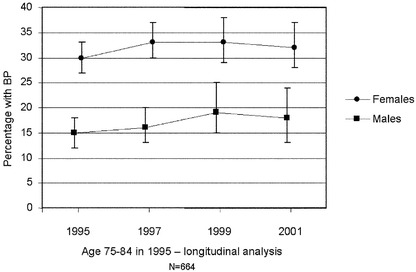
Prevalence of BP at four time points for participants in all LSADT waves (1995, 1997, 1999, and 2001): longitudinal analysis
Table 1.
Number (percentage) of participants in all four waves (1995, 1997, 1999 and 2001) of the Longitudinal Study of Aging Danish Twins who reported back pain (BP) within the past month, according to the number of episodes of BP in that period
| No. of BP episodes | N | % |
|---|---|---|
| 0 | 323 | 49 |
| 1 | 137 | 21 |
| 2 | 89 | 13 |
| 3 | 59 | 9 |
| 4 | 43 | 6 |
| Missing | 13 | 2 |
| Total | 664 | 100 |
Co-morbidity
Lower levels of self-rated health were associated with BP prevalence in a significant dose-response like relationship, strongest among women, where participants rating their own health as "poor" were more than seven times as likely to also have experienced BP within the past month compared to women rating their health as "excellent" (Table 2).
Table 2.
Number of participants with BP and odds ratios (OR) for BP, with 95% confidence intervals (CI), according to self-rated health among 4484a Danish twins aged 70–102 years
| Self-rated health | n | OR (95% CI) | ||
|---|---|---|---|---|
| Male + female | Male | Female | ||
| Excellent | 1319 | 1.00 | 1.00 | 1.00 |
| Very good | 1716 | 1.90 (1.57–2.30) | 1.69 (1.24–2.31) | 2.06 (1.61–2.62) |
| Good | 1034 | 3.47 (2.84–4.24) | 2.80 (2.00–3.92) | 3.83 (2.97–4.92) |
| Fair | 305 | 4.90 (3.72–6.44) | 4.33 (2.76–6.80) | 5.21 (3.68–7.38) |
| Poor | 106 | 6.34 (4.14–9.70) | 4.54 (2.11–9.75) | 7.13 (4.23–12.02) |
P<0.00001 for all regression models according to Wald test
a Information on self-rated health missing for eight participants
BP was associated with an extensive list of co-occurring diseases both in the univariate and the multivariate analysis (Table 3): most noticeably, bone and joint disorders (degenerative joint disease, disc prolapse, osteoporosis, vertebral fracture, rheumatoid arthritis, gout). However, migraine, lung diseases (asthma, chronic bronchitis), cardiovascular disorders (hypertension, angina pectoris, coronary attack), and gastric ulcer were also significantly associated with BP. Neurologic disorders (epilepsy, Parkinsons disease) and endocrinological disorders (diabetes, Graves disease, Hashimotos disease) were not significantly associated with BP, although for men both Parkinsons disease and Graves disease exhibited borderline significance for association (Table 3).
Table 3.
Disease prevalence (%) according to BP status, prevalence proportion ratio (PPR) and odds ratio (with 95% CI) among 4484 Danish twins aged 70–102 years
| Disease | Prevalence (%) | PPRa | OR (95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| +BP | −BP | |||||||||
| ♂+♀ | ♂ | ♀ | ♂+♀ | ♂ | ♀ | ♂+♀ | ♂ | ♀ | ♂+♀b | |
| Degenerative joint disease | 47 | 36 | 53 | 23 | 17 | 28 | 2.04 | 2.11 | 1.89 | 2.65*** (2.24–3.14) |
| Disc prolapse | 16 | 18 | 15 | 5 | 7 | 4 | 3.20 | 2.57 | 3.75 | 3.40*** (2.73–4.23) |
| Osteoporosis | 15 | 6 | 20 | 4 | 1 | 6 | 3.75 | 6.00 | 3.33 | 4.36*** (3.39–5.59) |
| Vertebral fracture | 8 | 8 | 8 | 2 | 2 | 2 | 4.00 | 4.00 | 4.00 | 3.41** (1.50–7.79) |
| Rheumatoid arthritis | 8 | 7 | 9 | 5 | 4 | 6 | 1.60 | 1.75 | 1.50 | 1.67*** (1.30–2.15) |
| Gout | 8 | 10 | 6 | 4 | 6 | 3 | 2.00 | 3.33 | 2.00 | 2.11*** (1.59–2.81) |
| Migraine | 15 | 5 | 15 | 9 | 3 | 9 | 1.67 | 1.67 | 1.67 | 1.72*** (1.38–2.15) |
| Chronic bronchitis | 13 | 20 | 13 | 9 | 12 | 9 | 1.44 | 1.67 | 1.44 | 1.69*** (1.39–2.05) |
| Asthma | 11 | 14 | 11 | 8 | 10 | 8 | 1.38 | 1.40 | 1.38 | 1.44*** (1.20–1.73) |
| Hypertension | 31 | 24 | 31 | 26 | 19 | 26 | 1.19 | 1.26 | 1.19 | 1.21*** (1.06–1.39) |
| Angina pectoris | 10 | 7 | 10 | 5 | 5 | 5 | 2.00 | 1.40 | 2.00 | 1.90*** (1.48–2.45) |
| Coronary attack | 8 | 11 | 8 | 6 | 10 | 6 | 1.33 | 1.10 | 1.33 | 1.33** (1.08–1.64) |
| Gastric ulcer | 14 | 18 | 14 | 9 | 12 | 9 | 1.56 | 1.50 | 1.56 | 1.70*** (1.40–2.07) |
| Epilepsy | 1 | 1 | 1 | 1 | 2 | 1 | 1.00 | 0.50 | 1.00 | 1.19 (0.89–1.60) |
| Parkinsons disease | 1 | 4 | 1 | 1 | 1 | 1 | 1.00 | 4.00 | 1.00 | 1.05 (0.99–1.12) |
| Diabetes | 8 | 9 | 8 | 8 | 8 | 8 | 1.00 | 1.13 | 1.00 | 1.15 (0.94–1.42) |
| Graves disease | 7 | 2 | 7 | 5 | 1 | 5 | 1.40 | 2.00 | 1.40 | 1.18 (0.97–1.45) |
| Hashimoto's disease | 5 | 1 | 5 | 3 | 1 | 3 | 1.67 | 1.00 | 1.67 | 1.15 (0.94–1.39) |
*P<0.05; **P<0.005; ***P<0.0001
aPrevalence proportion ratio between +BP and −BP
bAdjusted for sex and age, complete twin pairs analysed in clusters of two
Living alone was associated with BP only for men (OR 1.19, 95% CI 1.00–1.42); however, the increased risk was very modest. Neither current nor past smoking was associated with BP in either of the sexes, and nor was increasing body mass index. Years of school and education after school were found not to be associated with BP (data not shown).
Having BP was significantly associated with lower Strength scores (2.78 for participants with BP vs 3.16 for participants without BP; OR for lower Strength score: 1.39, 95% CI 1.27–1.52); however, no association was found between BP and MMSE scores (OR for lower MMSE score among participants with BP: 1.00, 95% CI 0.99–1.02).
Discussion
BP is a common symptom in younger age groups and it remains common in old age, with roughly 25% of the population experiencing BP every month. For both men and women, prevalence does not appear to increase with increasing age, and around half (49%) of participants in this study had not experienced BP during the month prior to any of the four interviews. We found four previous studies reporting on the 1-month prevalence of BP in this age group [7, 14, 16, 17]; however, they were all cross-sectional. In all papers overall 1-month prevalence rates similar to ours (between 20 and 30%) were reported; however, both Croft and Rigby [7] and Huang et al. [17] reported higher rates in the oldest age groups. Contrary to this, Heliövaara et al. found significantly lower rates in the 74+ age group compared to the group aged 65–74 years [16], and Hagen et al. only reported a combined prevalence for the 65- to 79-year age group (22%) [14]. Thus the present study is, to our knowledge, the first study employing both a cross-sectional and longitudinal analysis in the same sample with identical measurements at four different time points, and we found no evidence for any change in prevalence with increasing age using either approach.
Lower education has been associated with a higher frequency of BP in many epidemiologic studies published over the past 30 years [8], probably due to the association between low education and physically demanding jobs. We did not find a significant association between few years of school or lower education after school and BP. It may be that the effect of education or physically demanding jobs on BP is not detectable after retirement; however, our data do not justify firm conclusions with respect to these questions.
BP is not an isolated health problem in old age. In fact, the symptom of pain in the back is associated with a long list of co-occurring health problems, mainly bone and joint diseases (both inflammatory and non-inflammatory), migraine headaches, lung and heart diseases and gastric ulcer. It is hardly surprising that degenerative joint disease, disc prolapse, osteoporosis (with and without vertebral fracture), rheumatoid arthritis and gout are associated with BP, since they all to some extent involve the osseous structures and joints of the vertebral column. Nevertheless, the relationship between, for instance, vertebral fractures and BP in old age is not entirely clear. Huang et al. reported that, among post-menopausal Japanese-American women, a "dose-response" like relationship existed between the number of vertebral fractures and BP [17]. Contrary to this, Kanis and McCloskey found that, even though women experienced a 20-fold increase in risk for vertebral fractures between the ages of 60 and 90, half of these fractures were asymptomatic [21], and Zetterberg et al. concluded that the major explanation for longstanding BP in the elderly was not related to osteoporosis, since only half as many cases with vertebral fractures following osteoporosis reported BP compared to matched controls without any fractures [35]. Finally, Joakimsen et al., after reviewing 222 scientific articles on vertebral fractures, concluded that vertebral deformities following fractures represent only a minor public health problem, and that less than 8% of BP cases among the elderly can be attributed to such fractures [19]. One explanation for these apparently paradoxical findings might be that different types of fracture, i.e. total, anterior, posterior or central collapse of the vertebral body, and location of these fractures, i.e. spinal level, may produce different symptomatology.
The association between lung disease and BP might be explained by the effect of frequent coughing causing repeated increase in spinal pressure which, over time, might lead to pain, as suggested by Gyntelberg almost 30 years ago [13]. BP and cardiovascular diseases have been shown to share a number of risk factors [33], and BP has been linked to atherosclerotic changes in the posterior wall of the abdominal aorta in older persons [23]. Probably the most important cause and common denominator for these problems is smoking, which has also been associated with BP in many studies, even though evidence for a direct causal link between the two is lacking [12, 25]. Curiously, in this study we did not find any association between either present or past smoking and BP. It may be that too few smokers with lung and heart disease lived long enough to be included in this study.
Poorer self-rated health exhibits a strong relationship of the "dose-response" type with increasing risk for experiencing BP. In fact around half of the persons with BP during the past month considered their health as "poor"—the lowest category. This is hardly surprising considering the long list of co-morbidities in BP sufferers. In fact, we do not believe BP to be the sole cause of this perception of poor health. Rather, BP should be considered part of larger syndrome of poor health in old age and, bearing in mind the strong relationship with self-rated health, maybe self-reported BP could be considered as an easily accessible indicator for health status in senior citizens.
We found the level of daily physical functioning to be significantly lower in participants experiencing BP than in participants without BP. This finding is in concurrence with recent studies. Fanuele et al. found that the impact of spinal problems on physical functional status was similar to the impact of conditions like congestive heart failure or to functional status prior to primary total hip arthroplasty or prior to primary total knee arthroplasty in a population-based sample of more than 17,000 people aged 17–98 years [10]. In the older population, both Leveille et al. and Lavsky-Shulan et al., in population-based studies, found that the presence of BP significantly influenced physical functional abilities of older people [24, 27]. The question, of course, remains whether these limitations in physical functioning are caused by BP as an isolated symptom, or whether they are due to a combined effect of several health problems, one of which is BP.
The prevalence of a condition may vary depending on how the condition is defined. In their extensive review, Bressler et al. pointed out that definitions of BP varied greatly between studies [3], and Edmond and Felson found that the prevalence of BP in old age varied between ambulatory and non-ambulatory patients [9]. Our study is population based, and all interviews were conducted in the homes of the participants, excluding only answers given by proxy, i.e. in cases where the participant was unable to answer on his/her own, and we used a broad definition of BP. Further, the question regarding BP was nested in an extensive general interview, thereby probably avoiding focusing attention (causing overestimation) on any one specific health problem. We therefore consider our estimate of the 1-month prevalence to be robust and reliable for men and women aged 70 and older.
Future studies need to address more specific issues related to BP that could not be addressed using the present data. Among these are the exact location of such pain—i.e. mid-back, low-back or pelvis, all over—and the consequences of BP—i.e. the need for assistance to perform daily activities, seeking of health care and the effect of such care, etc. Probably the greatest challenge will be to disentangle the complicated relationship between BP and other health problems in order to rationally address the issues of prevention and treatment of this common symptom in the most rapidly growing segment of the population.
Conclusion
BP is a common symptom in old age, affecting around 20% of men and around 30% of women on a monthly basis. The vast majority of people (70%), however, experienced only one episode or none at all, prior to any of the four interviews. Prevalence estimates remained constant with increasing age in both a cross-sectional and a prospective analysis. BP is associated with a long list of co-occurring health problems and poor self-rated health. BP sufferers had significantly lower scores on a validated physical functioning test, but cognitive scores were unaffected.
Footnotes
Supported by the US National Institute on Aging Research Grant NIA-P01-AG08761, the Danish Research Councils, and the Danish National Research Foundation
References
- 1.Bergstrom Br J Rheumatol. 1986;25:333. doi: 10.1093/rheumatology/25.4.333. [DOI] [PubMed] [Google Scholar]
- 2.Bigos SJ, Bower O, Braen G (1994) Acute low back problems in adults. Clinical practice guideline no. 14. 95–0642. Agency for Health Care Policy and Research (AHCP), Rockville
- 3.Bressler Spine. 1999;24:1813. doi: 10.1097/00007632-199909010-00011. [DOI] [PubMed] [Google Scholar]
- 4.Christensen J Aging Health. 1999;11:49. doi: 10.1177/089826439901100103. [DOI] [PubMed] [Google Scholar]
- 5.Christensen J Gerontol A Biol Sci Med Sci. 2000;55:M446. doi: 10.1093/gerona/55.8.m446. [DOI] [PubMed] [Google Scholar]
- 6.Cooper Age Ageing. 2001;30:495. doi: 10.1093/ageing/30.6.495. [DOI] [PubMed] [Google Scholar]
- 7.Croft J Epidemiol Community Health. 1994;48:166. doi: 10.1136/jech.48.2.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dionne J Epidemiol Community Health. 2001;55:455. doi: 10.1136/jech.55.7.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Edmond J Rheumatol. 2000;27:220. [PubMed] [Google Scholar]
- 10.Fanuele JC, Birkmeyer NJ, Abdu WA, et al (2000) The impact of spinal problems on the health status of patients: have we underestimated the effect? Spine 25:1509–1514 [DOI] [PubMed]
- 11.Folstein J Psychiatr Res. 1975;12:189. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 12.Goldberg Spine. 2000;25:995. doi: 10.1097/00007632-200004150-00016. [DOI] [PubMed] [Google Scholar]
- 13.Gyntelberg Dan Med Bull. 1974;21:30. [PubMed] [Google Scholar]
- 14.Hagen J Rheumatol. 1997;24:1703. [PubMed] [Google Scholar]
- 15.Hauge Acta Genet Med Gemellol. 1968;2:315. doi: 10.1017/s1120962300012749. [DOI] [PubMed] [Google Scholar]
- 16.Heliovaara Ann Med. 1989;21:327. doi: 10.3109/07853898909149216. [DOI] [PubMed] [Google Scholar]
- 17.Huang J Bone Miner Res. 1996;11:1026. doi: 10.1002/jbmr.5650110721. [DOI] [PubMed] [Google Scholar]
- 18.Jette AM (1987) The functional status index: reliability and validity of a self-report functional disability measure. J Rheumatol 14 [Suppl 15]:15–19 [PubMed]
- 19.Joakimsen Tidsskr Nor Laegeforen. 2001;121:598. [PubMed] [Google Scholar]
- 20.Johansson Acta Orthop Scand. 1993;64:25. doi: 10.3109/17453679308994521. [DOI] [PubMed] [Google Scholar]
- 21.Kanis JA, McCloskey EV (1992) Epidemiology of vertebral osteoporosis. Bone 13 [Suppl 2]:1–10 [DOI] [PubMed]
- 22.Katz JAMA. 1963;185:94. [Google Scholar]
- 23.Kauppila Spine. 1997;22:1642. doi: 10.1097/00007632-199707150-00023. [DOI] [PubMed] [Google Scholar]
- 24.Lavsky-Shulan J Am Geriatr Soc. 1985;33:23. doi: 10.1111/j.1532-5415.1985.tb02855.x. [DOI] [PubMed] [Google Scholar]
- 25.Leboeuf-Yde Spine. 1999;24:1463. doi: 10.1097/00007632-199907150-00012. [DOI] [PubMed] [Google Scholar]
- 26.Leboeuf-Yde Spine. 1996;21:1518. doi: 10.1097/00007632-199607010-00005. [DOI] [PubMed] [Google Scholar]
- 27.Leveille J Gerontol A Biol Sci Med Sci. 1999;54:M487. doi: 10.1093/gerona/54.10.m487. [DOI] [PubMed] [Google Scholar]
- 28.Loney Phys Ther. 1999;79:384. [PubMed] [Google Scholar]
- 29.Maniadakis Pain. 2000;84:95. doi: 10.1016/S0304-3959(99)00187-6. [DOI] [PubMed] [Google Scholar]
- 30.Manton Gerontologist. 1993;33:168. doi: 10.1093/geront/33.2.168. [DOI] [PubMed] [Google Scholar]
- 31.Schulz-Larsen J Clin Epidemiol. 1992;45:1315. doi: 10.1016/0895-4356(92)90172-j. [DOI] [PubMed] [Google Scholar]
- 32.StataCorp (2000) Stata Statistical Software (6.0). Stata Corporation, College Station
- 33.SvenssonSpine 198382776226118 [Google Scholar]
- 34.Vaupel Science. 1998;280:855. doi: 10.1126/science.280.5365.855. [DOI] [PubMed] [Google Scholar]
- 35.Zetterberg Spine. 1990;15:783. [PubMed] [Google Scholar]


