Abstract
Insertion of pedicle screws in the thoracic spine is technically difficult and may lead to major complications. Although many computer-assisted systems have been developed to optimize pedicle screw insertion, these systems are expensive, not user-friendly and involve significant radiation from pre-operative computed tomographic (CT) scan imaging. This study describes and evaluates a transpedicular drill guide (TDG) designed to assist in the proper placement of pedicle screws in the thoracic spine. Pilot holes were made manually using the TDG in the thoracic spine (T1–T11) of three human cadavers before inserting 4.5-mm-diameter screws. CT scans followed by visual inspection of the spines were performed to evaluate the position of the screws. Five of 66 screws (7.6%) violated the pedicle wall: two (3.0%) medially and three (4.5%) laterally. The medial and lateral perforations were within 1 mm and 2 mm of the pedicle wall, respectively. The medial perforations were not at risk of causing neurological complications. No screw penetrated the superior or inferior pedicle wall. The TDG is easy to use and can decrease the incidence of misplaced thoracic pedicle screws. The TDG could be used as a complement to fluoroscopy in certain applications, especially for training surgeons.
Keywords: Internal fixators, Pedicle screws, Spinal instrumentation, Surgery, Thoracic vertebrae
Introduction
The use of pedicle screws is gaining increasing popularity for instrumentation of the thoracic spine. Biomechanically, thoracic pedicle screws have been shown to offer more strength and stiffness than hooks [13]. Potential applications of thoracic pedicle screw instrumentation include fracture, segmental instability, hyperkyphosis, scoliosis, infection and tumor [2, 3, 4, 10, 12, 20]. However, insertion of pedicle screws in the thoracic spine is technically difficult and may lead to major complications [6, 12, 16, 19, 21, 22].
Placement of thoracic pedicle screws based solely on anatomical knowledge is variable and can result in a high failure rate. Vaccaro et al. [22] found that the failure rate was highly variable between surgeons and that most of their own 41.1% misplaced screws violated the medial wall, some by as much as 8.5 mm. Xu et al. [25] showed a decreased incidence of pedicle perforation with the open lamina technique (16.0%), as compared to the Roy-Camille technique (54.7%). Cinotti et al. [5] obtained a 15.6% rate of pedicle violation by combining morphological data with a specific insertion point. Xu et al. [26] obtained a failure rate of 16.3% guided by individualized morphometric CT scan measurements. Although pre-operative CT scan allows proper determination of the pedicle anatomy, the visual matching between the pre-operative CT scans and the exposed spine can be misleading. In addition, CT scans of the thoracic spine involve significant radiation exposure, especially if a long segment needs to be explored.
Pedicle instrumentation in the thoracic spine can also be aided by intra-operative image intensification, although the interference from the rib cage limits their use [11]. With this technique, the in vivo rate of pedicle perforation ranges from 3.0 to 43.0% [2, 3, 12, 20]. Due to this significant variability in accuracy and to the major potential complications of pedicle screw insertion in the thoracic spine, some surgeons use CT-based navigation systems that have proved to be safe and accurate [2, 4, 11, 27]. However, these systems are expensive, require pre-operative CT scans and intra-operative registration, involve a marked learning curve [11] and are not widely available.
In search of a new technique to assist in the safe placement of pedicle screws in the thoracic spine, a transpedicular drill guide (TDG) was designed. The purpose of this cadaveric study was to describe and evaluate the TDG before clinical use.
Materials and methods
The TDG is composed of a sublaminar pedicle finder and a drill sleeve that can be moved along an arc of circle (Fig. 1). The pedicle finder and the drill sleeve are constrained within the same plane so that the drilling axis is always centered between the prongs of the pedicle finder in the transverse plane (Fig. 2A). Furthermore, for any position of the drill sleeve on the arc of circle, the distance between the drilling axis and the tip of the pedicle finder is always constant in the sagittal plane (Fig. 2B).
Fig. 1.

Transpedicular drill guide (TDG) for pedicle screw insertion in the thoracic spine
Fig. 2.

A The drilling tool is always centered between the prongs of the pedicle finder (in the transverse plane). B The distance between the drilling tool and the tip of the pedicle finder is always constant in the sagittal plane (d1=d2)
The use of the TDG can be summarized as follows. The pedicle finder of the TDG is engaged under the lamina in order to anchor the TDG to the pedicle (Fig. 3A). If the TDG cannot be properly inserted under the lamina, a small osteotome can be used to partially remove the inferior facet at a right angle (partial facetectomy), so as to allow the prongs of the pedicle finder to reach the inferior surface of the pedicle. The laminar blocker limits the foramen and canal encroachment by the prongs of the pedicle finder. The TDG is then adjusted depending on the desired insertion point for drilling (Fig. 3B). The drill sleeve is moved to the desired drilling angle in the sagittal plane (Fig. 3C) before drilling the pilot hole (Fig. 3D). According to reported morphometric data [28], the sagittal orientation of normal pedicles lies between 15° and 20° for all thoracic levels. For this cadaveric study, the sagittal angle for pilot hole preparation was kept at 15° for all vertebrae. The angle of drilling in the transverse plane is set automatically by the TDG. It is always formed by the line joining two specific landmarks (Fig. 4): the insertion point selected by the surgeon and the center of the pedicle section intersected by the pedicle finder. The second landmark is the main feature of the TDG and is due to the fact that the drilling axis is always centered between the prongs of the pedicle finder in the transverse plane (Fig. 2A). Image intensification was not used prior to or during pilot hole preparation in the present study, but may be used as an additional safety procedure.
Fig. 3.

Steps required for pilot hole preparation with the TDG. A Engage the pedicle finder under the lamina. B Adjust the TDG to obtain the desired insertion point for drilling. C Adjust the TDG depending on the desired drilling angle in the sagittal plane. D Drill the pilot hole
Fig. 4.
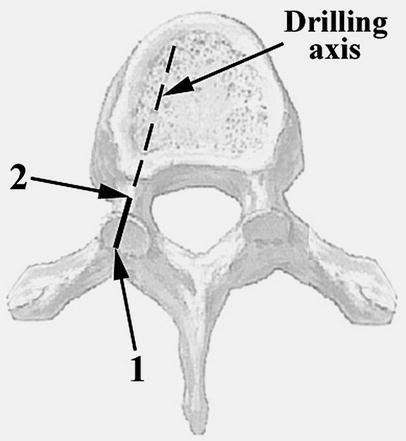
Angle of drilling in the transverse plane is based on two specific landmarks: 1) insertion point selected by the surgeon and 2) center of the pedicle section intersected by the pedicle finder
The cadaveric study was performed at the Laboratory for Functional Anatomy of the University of Brussels, using three elderly cadavers (one male, two female) embalmed according to a modified Dankmeyer's technique [23]. Two of them had thoracic hyperkyphosis associated with osteoporosis. The cadavers were positioned prone and the thoracic spine was exposed as for a posterior spine surgery. Pilot holes (a total of 66) were made bilaterally from T1 to T11 using the TDG and a 3.2-mm straight handheld probe. For optimal stability, one assistant held the TDG while the surgeon manually drilled the pilot holes using two hands. The surgeon was not allowed to use a depth gauge either to palpate the pedicle walls or to redirect the drilling, but had to follow the drilling path given by the TDG once it was adjusted. The insertion point for drilling was located at the intersection between the superior border of the transverse process and the lateral two-thirds of the superior facet [5]. AO cortical screws of 4.5 mm diameter (38 mm length) were inserted into all pilot holes, since this represents the smallest screw diameter available with most spinal instrumentation systems. Pedicle instrumentation was performed by a senior orthopedic surgeon (H.L.), well trained in the routine use of pedicle screws in the thoracolumbar and lumbar areas, but with a more limited experience in thoracic pedicle screws insertion above T10.
Following placement of the pedicle screws in all three cadavers, spiral CT scans (CT Twin Flash, Elscint, Haifa, Israel) were obtained for each specimen. Screw position was verified on overlapping CT scan slices (increment of 1.5 mm, thickness of 2.7 mm). After the CT scans, each spine was harvested and the posterior vertebral arch was removed in order to confirm by visual inspection any medial, inferior or superior pedicle wall violation. The rib head was not removed for visual examination of the lateral pedicle wall.
Results
Overall, only five (7.6%) of the 66 screws violated the pedicle wall (Table 1). Two screws (3.0%) were medial to the pedicle and three (4.5%) were lateral. All medial perforations were within 1 mm of the pedicle wall, with only part of the threads outside the pedicle. Two screws misplaced laterally were within 1 mm of the lateral wall, while the third screw violated the pedicle wall by less than 2 mm (part of the screw shaft was visible). No screw penetrated the superior or inferior pedicle wall. No evidence of injury to the dura mater or spinal cord was found during the visual examination. The visual inspection also showed that the screws that had perforated the lateral pedicle wall, as seen on the CT scans, remained within the costo-vertebral articulation without violating the surrounding soft tissues.
Table 1.
Occurrence and extent of pedicle wall perforations for each vertebral level. The total perforation rate was 7.6% (5 of 66). (M medial wall, L lateral wall)
| Vertebral level | Perforations/no. of pedicles | Pedicle wall perforation | ||
|---|---|---|---|---|
| <1 mm | ≥1 mm, <2 mm | ≥2 mm | ||
| T1 | 1/6 | 1M | – | – |
| T2 | 0/6 | – | – | – |
| T3 | 0/6 | – | – | – |
| T4 | 1/6 | 1L | – | – |
| T5 | 0/6 | – | – | – |
| T6 | 0/6 | – | – | – |
| T7 | 0/6 | – | – | – |
| T8 | 1/6 | 1M | – | – |
| T9 | 1/6 | – | 1L | – |
| T10 | 1/6 | 1L | – | – |
| T11 | 0/6 | – | – | – |
| Total | 5/66 | 2M/2L | 1L | – |
Discussion
The AO Study Group developed in 1993 a device that allowed placement of pedicle screws with respect to a pedicle localizer (International patent #A 61B 17/16). The drill guide presented in this study uses a similar concept by combining a conventional sublaminar pedicle finder with a mobile drill sleeve. In contrast to the device introduced by the AO Study Group, the TDG allows variable orientation of the sagittal drilling angle and can be adjusted according to the pedicle height.
The TDG was found to be simple and easy to use on straight spines. It gave additional control and stability to the drilling process because the pedicle finder allowed a firm anchorage to the vertebrae. However, in case of deformed or rotated spines (e.g. scoliosis), the engagement of the pedicle finder could be difficult due to interference between the arc of circle and the soft tissues. Interference between the arc of circle and the occiput could also limit the use of the TDG for upper thoracic vertebrae, especially in cases of hyperkyphosis, although this did not occur in the current study. These limitations are important, and this is why a new design allowing adjustment and modification of the arc of circle was made after completion of this study. The latest version of the TDG also avoids the need for a partial facetectomy. Less than 15 min of explanations and practice were necessary before using the instrument. Apart from the simple adjustments to the TDG, no modification to the surgical technique was required. The transition from the conventional anatomical technique to the TDG would be particularly easy for surgeons familiar with pedicle hook systems, since the correct use of the TDG is mainly based on an adequate anchoring of the pedicle finder to the pedicle. In addition, the TDG can adapt to any drilling tool (handheld probe or drill bit). The TDG is not recommended for the T12 vertebra because the pedicles at this level are transitional between thoracic and lumbar configurations, making it difficult to use unless an extensive facetectomy is performed. For this reason, the TDG was not used for the T12 vertebra in this study.
Adequate anchoring of the pedicle finder to the pedicle was sometimes difficult to obtain because the cadaveric spines were much stiffer and less mobile than normal, due to the effect of the preservation solution on the soft tissues. This may perhaps explain some of the misplaced screws. Engagement of the pedicle finder is easier in live patients with normal vertebral mobility. However, the correct use of a sublaminar pedicle finder is complex and requires significant anatomical knowledge and technical skills on behalf of the surgeon in order to avoid injury to the spinal cord or nerves, since the pedicle finder involves a spinal canal intrusion, as does a pedicle hook. This is a recognized limitation of the TDG.
The open-lamina technique described by Xu et al. [25] allows direct visualization and palpation of the medial and superior pedicle walls. Although this technique gives additional anatomical information to the surgeon, it does not provide the anatomical alignment featured by the TDG. This may explain the higher accuracy achieved with the TDG (7.6% perforation rate) as compared to the open-lamina technique (16.0% perforation rate).
The overall pedicle violation rate (7.6%) was in the same range as those reported with CT-based navigation systems. Kim et al. [11] inserted 120 thoracic pedicle screws on five cadavers using a CT-based navigation system and obtained an overall pedicle violation rate of 19.2%, with 65.0% of the perforations being medial. Youkilis et al. [27] reported 9.8% cortical violations for 183 image-guided thoracic pedicle screws (T1–T11) placed in 47 patients. In their case series, Amiot et al. [2] had only 1.4% misplaced screws (1 of 74 screws from T1 to T11) using their navigation system, as compared to 14.8% (8 of 54 screws from T1 to T11) with fluoroscopy. Compared to CT-based navigation systems, the TDG is more affordable, simpler to use and does not require pre-operative CT. Furthermore, CT-based navigation systems require additional staff and equipment in the operating room, and are associated with a considerable learning curve [11].
Fluoroscopic navigation is gaining popularity in spine surgery. It has been shown to provide real-time multiplanar surgical guidance at low radiation exposure [8, 15]. There are, however, some limitations to this technique that mainly arise from current limitations of fluoroscopic imaging [8]. In a previous work, it was demonstrated that fluoroscopic images were often unreliable for determining the angle of screw insertion and for evaluating placement success, although the study was performed using cadaveric spines from T11 to S1 that were cleaned of all soft tissues [24]. This problem is even worse for thoracic pedicle screws, because of the interference from the rib cage. Translation of two-dimensional images to three-dimensional (3D) anatomy is complex and mostly depends on the surgeon's skills and experience. Conversely, the TDG provides direct anatomical feedback of the 3D position of the pedicle from the pedicle finder. This feature of the TDG may be particularly helpful for the correct orientation of drilling in the transverse plane, and may therefore compensate for the lack of reliable information provided by fluoroscopic imaging regarding the transverse plane anatomy. Another drawback of fluoroscopic navigation is the need for an optoelectronic navigator that requires a constant line of sight with the tracked markers, which cannot currently be assured during the entire procedure [15].
The transverse screw angle is a critical issue for safe insertion of pedicle screws in the thoracic spine [7]. Even a very slight discrepancy between the pedicle and screw medio-lateral inclinations can lead to pedicle wall perforation [3]. There is some controversy about the acceptability of medially misplaced pedicle screws in the thoracic spine. Anatomical studies have shown that the distance between thoracic pedicles and the dural sac is non-existent or minimal in normal human cadavers [6, 21]. However, Reynolds et al. [18] have demonstrated evidence of a 2-mm lateral epidural space from T7 to L4 by contrast injection into the epidural space. Based on in vivo data, Gertzbein and Robbins [9] extrapolated that 4 mm of canal encroachment in straight spines could be tolerated without impinging on the spinal cord between T10 and L4. This ''safe zone'' of 4 mm was demonstrated on CT myelogram to be composed of a 2-mm epidural space and a 2-mm subarachnoid space. For scoliotic spines, Liljenqvist et al. [14] demonstrated a shift of the dural sac towards the concavity, with the epidural space measuring less than 1 mm on the concave side of the thoracic apex and between 3 mm and 5 mm on the convex side of the curve. Recently, Papin et al. [16] reported a case of spinal cord compression in a scoliotic patient due to pedicle screws at T8 and T10 that were medially misplaced by exactly 4 mm. These last findings suggest that the ''safe zone'' described by Gertzbein and Robbins [9] is not applicable to deformed spines.
The main advantage of the TDG is that it automatically sets the optimal transverse angle for pilot hole preparation by constraining the drilling axis inside the pedicle (Fig. 4). This is how the TDG decreased the incidence and extent of medial perforations in particular, which are the most feared event because of the risk of spinal cord injury [6, 12, 16, 19, 21, 22]. Only two of 66 screws (3.0%) perforated the medial wall, and in both cases the perforations were by less than 1 mm. These medial perforations would be unlikely to cause a spinal cord injury, since many authors have reported such minor medial wall perforations of thoracic pedicles without any evidence of neurological injury for in vivo cases [2, 9, 12, 20, 27]. Furthermore, the visual inspection did not reveal any injury of the dura mater or spinal cord at the site of medial perforations. However, as pointed out by Aebi [1], the inspection of cadaveric dura mater and spinal cord can be misleading because, in a cadaver, there is no tissue turgor, and maybe even some shrinkage. Therefore, the integrity of the dura at the sites of medial wall perforations may theoretically have been related to some in vitro factors, and this should be kept in mind when facing in vivo applications. The post-mortem reabsorption of cerebrospinal fluid (CSF) could also affect the epidural space. At the laboratory for Functional Anatomy of the University of Brussels, the fixation of the brain and spinal cord was performed by injecting a solution directly into the subarachnoid space through a small hole drilled in the frontal bone, since the fixation solution cannot cross the brain-blood barrier. There was no aspiration or significant flow of CSF before the injection of 20 cc of fixation solution. There are no detailed data in the literature concerning the post-mortem reabsorption of CSF, but the authors do not think that it is significant after fixation.
The TDG has been validated on straight spines only. Scoliosis is associated with a distorted anatomy involving all parts of the vertebrae [17]. The insertion point and medio-lateral angle of insertion commonly used for normal spines may not be appropriate in scoliosis. The use of the TDG ensures that the drilling axis will be centered with respect to the pedicle section intersected by the pedicle finder, whether the vertebra is normal or not. Due to this specific feature of the TDG and to the relatively short length of a pedicle, the insertion point and medio-lateral angle of insertion become less critical, since the TDG constrains the drilling axis inside the pedicle (Fig. 5). The risk of pedicle wall perforation is thus theoretically reduced for both normal and deformed spines if the TDG is correctly engaged. However, insertion of pedicle screws in the scoliotic spine should be performed with extreme caution, especially in the concave side of the curve where the pedicles are distorted and the epidural space is reduced [14, 17]. For these difficult cases, we recommend the use of adequate preoperative and/or intraoperative imaging in combination with the TDG. The real efficiency of the TDG for scoliotic cases has to be evaluated in another study involving scoliotic spines.
Fig. 5.

Possible insertion points and drilling paths (1–3) in the transverse plane for a scoliotic vertebra. The drilling path always crosses the center of the pedicle section intersected by the pedicle finder
Conclusions
The TDG is non-invasive, easy to use and can decrease the incidence of misplaced thoracic pedicle screws from T1 to T11. In the present study, its accuracy was similar to the existing CT-based navigation systems. The TDG can be used as a complement to any existing technique of pedicle screw insertion in order to increase control, stability and accuracy during pilot hole preparation in thoracic pedicles, especially for training surgeons. The authors do not, however, suggest using the TDG alone, but recommend the use of intraoperative fluoroscopy to control the drilling axes.
References
- 1.Aebi Spine. 1997;22:1557. doi: 10.1097/00007632-199707150-00003. [DOI] [Google Scholar]
- 2.AmiotSpine 20002560610749638 [Google Scholar]
- 3.Belmont Spine. 2001;26:2340. doi: 10.1097/00007632-200111010-00010. [DOI] [PubMed] [Google Scholar]
- 4.Bolger C, Wigfield C (2000) Image-guided surgery: applications to the cervical and thoracic spine and a review of the first 120 procedures. J Neurosurg 92 [Spine 2]:175–180 [DOI] [PubMed]
- 5.Cinotti Spine. 1999;24:114. doi: 10.1097/00007632-199901150-00003. [DOI] [PubMed] [Google Scholar]
- 6.Ebraheim Spine. 1997;22:1553. doi: 10.1097/00007632-199707150-00002. [DOI] [PubMed] [Google Scholar]
- 7.Ebraheim Spine. 1997;22:233. doi: 10.1097/00007632-199702010-00001. [DOI] [PubMed] [Google Scholar]
- 8.Foley Spine. 2001;26:347. doi: 10.1097/00007632-200102150-00009. [DOI] [PubMed] [Google Scholar]
- 9.GertzbeinSpine 199015112326693 [Google Scholar]
- 10.JonssonEur Spine J 19965368689415 [Google Scholar]
- 11.Kim Spine. 2001;26:360. doi: 10.1097/00007632-200102150-00011. [DOI] [PubMed] [Google Scholar]
- 12.Liljenqvist Spine. 1997;22:2239. doi: 10.1097/00007632-199710010-00008. [DOI] [PubMed] [Google Scholar]
- 13.Liljenqvist Acta Orthop Belg. 2001;67:157. [PubMed] [Google Scholar]
- 14.Liljenqvist J Bone Joint Surg Am. 2002;84:359. doi: 10.2106/00004623-200203000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Nolte Eur Spine J. 2000;9:S78. doi: 10.1007/PL00010026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Papin Eur Spine J. 1999;8:156. doi: 10.1007/s005860050147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parent Spine. 2002;27:2305. doi: 10.1097/00007632-200211010-00002. [DOI] [PubMed] [Google Scholar]
- 18.Reynolds Neurosurgery. 1985;17:905. doi: 10.1227/00006123-198512000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Roy-Camille Orthop Clin North Am. 1986;17:147. [PubMed] [Google Scholar]
- 20.Suk Spine. 1995;20:1399. [PubMed] [Google Scholar]
- 21.Ugur J Spinal Disord. 2001;14:39. doi: 10.1097/00002517-200102000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Vaccaro J Bone Joint Surg Am. 1995;77:1200. doi: 10.2106/00004623-199508000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Van Surg Radiol Anat. 1992;14:325. doi: 10.1007/BF01794759. [DOI] [PubMed] [Google Scholar]
- 24.Weinstein Spine. 1988;13:1012. doi: 10.1097/00007632-198809000-00008. [DOI] [PubMed] [Google Scholar]
- 25.Xu Spine. 1998;23:1065. doi: 10.1097/00007632-199805010-00021. [DOI] [PubMed] [Google Scholar]
- 26.Xu J Spinal Disord. 1999;12:222. [PubMed] [Google Scholar]
- 27.Youkilis Neurosurgery. 2001;48:771. doi: 10.1097/00006123-200104000-00015. [DOI] [PubMed] [Google Scholar]
- 28.Zindrick Spine. 1987;12:160. doi: 10.1097/00007632-198703000-00012. [DOI] [PubMed] [Google Scholar]


