Abstract.
Combined IGF-I and TGF-β1 application by a poly-(D,L-lactide) (PDLLA) coated interbody cage has proven to promote spine fusion. The purpose of this study was to determine whether there is a dose-dependent effect of combined IGF-I and TGF-β1 application on intervertebral bone matrix formation in a sheep cervical spine fusion model. Thirty-two sheep underwent C3/4 discectomy and fusion. Stabilisation was performed using a titanium cage coated with a PDLLA carrier including no growth factors in group 1 (n=8), 75 µg IGF-I plus 15 µg TGF-β1 in group 2 (n=8), 150 µg IGF-I plus 30 µg TGF-β1 in group 3 (n=8) and 300 µg IGF-I plus 60 µg TGF-β1 in group 4 (n=8). Blood samples, body weight and temperature were analysed. Radiographic scans were performed pre- and postoperatively and after 1, 2, 4, 8, and 12 weeks. At the same time points, disc space height and intervertebral angle were measured. After 12 weeks, the animals were killed and fusion sites were evaluated using quantitative computed tomographic (CT) scans to assess bone mineral density, bone mineral content and bony callus volume. Biomechanical testing was performed and range of motion, and neutral and elastic zones were determined. Histomorphological and histomorphometrical analysis were carried out and polychrome sequential labelling was used to determine the time frame of new bone formation. In comparison to the group without growth factors (group 1), the medium- and high-dose growth factor groups (groups 3 and 4) demonstrated a significantly higher bony callus volume on CT scans, a higher biomechanical stability, an advanced interbody bone matrix formation in histomorphometrical analysis, and an earlier bone matrix formation on fluorochrome sequence labelling. Additionally, the medium- and high-dose growth factor groups (groups 3 and 4) demonstrated a significantly higher bony callus volume, a higher biomechanical stability in rotation, and an advanced interbody bone matrix formation in comparison to the low-dose growth factor group (group 2). No significant difference could be determined between the medium- and the high-dose growth factor groups (groups 3 and 4, respectively). The local application of IGF-I and TGF-β1 by a PDLLA-coated cage significantly improved results of interbody bone matrix formation in a dose-dependent manner. The best dose-response relationship was achieved with the medium growth factor dose (150 µg IGF-I and 30 µg TGF-β1). With an increasing dose of these growth factors, no further stimulation of bone matrix formation was observed. Although these results are encouraging, safety issues of combined IGF-I and TGF-β1 application for spinal fusion still have to be addressed.
Keywords. Cervical spine, Sheep, Animal model, Interbody fusion, IGF-I, TGF-β1, Growth factor, Surgery, Dose
Introduction
More than 30 years ago, Urist [55] determined the osteoinductive capacity of demineralized bone matrix. Advances in protein isolation and molecular cloning technology subsequently yielded several soluble, low-molecular-weight growth factors, like transforming growth factors (TGFs), bone morphogenetic proteins (BMPs), platelet-derived growth factors (PDGFs), insulin-like growth factors (IGFs), fibroblast growth factors (FGFs) and epidermal growth factors (EGFs) [54]. Meanwhile, many of these growth factors are available as recombinant molecules in virtually unlimited quantities using genetically modified cell lines. However, only some of these growth factors have demonstrated a significant osteoinductive capacity, and only two of these growth factors have been precisely evaluated in experimental spine fusion. Presently, only BMP-2 [4, 5, 6, 9, 12, 16, 22, 34, 35, 46, 47, 60, 61] and OP-1 (BMP-7) [15, 30] have proven to accelerate spinal fusion and to overcome the disadvantages of an autologous bone graft.
However, provisos have been expressed due to side effects associated with the use of BMPs in spinal fusion. BMPs are able to induce de novo bone in ectopic soft tissue sites even in the absence of bone marrow elements [2, 61]. Some authors have postulated that there is a necessity for a growth factor to induce ectopic bone to promote interbody fusion sufficiently [4, 34, 35]. However, this characteristic of BMP-2 or BMP-7 might also be harmful. In previous studies new bone formation induced by BMP-2 in the ligamentum flavum resulted in flattening of the spinal cord [36]. Additionally, Hoshi et al. [19] was able to show that ossifications of the spinal ligaments induced by BMP-2 can even lead to spinal cord compression. Other authors have suggested that the BMPs might play an important role in the ossification of spinal ligaments, especially the posterior longitudinal ligament [19, 28]. Therefore, the optimum growth factor or growth factor combination to promote spinal fusion is still a matter of discussion.
In an earlier study we were able to show an increased intervertebral bone matrix formation with IGF-I and TGF-β1 application compared to an autologous tricortical iliac crest bone graft, in a sheep cervical spine interbody fusion model [26]. Additionally, we demonstrated analogous biomechanical and histological results comparing BMP-2 and combined IGF-I and TGF-β1 application in this model [27]. Due to these results, combined IGF-I and TGF-β1 application seems to be very promising for bone induction in the field of spine surgery. However, to our knowledge, no studies have been performed to determine whether a dose-dependent effect of combined IGF-I and TGF-β1 application on intervertebral fusion exists.
Therefore, the purpose of this study was to determine whether there is a dose-dependent effect of combined IGF-I and TGF-β1 application on intervertebral bone matrix formation in a sheep cervical spine interbody fusion model. This study was additionally designed to define a dose that might be suitable for further experimental evaluation of this growth factor combination.
Materials and methods
Study design
Thirty-two adult female merino sheep (2 years old) underwent C3/4 discectomy and fusion. The sheep were randomly assigned to the following groups:
Group 1: titanium cage coated with a biodegradable poly-(D,L-lactide) PDLLA carrier (n=8)
Group 2 (low-dose group): titanium cage coated with a biodegradable PDLLA carrier including IGF-I (2.5% w/w=75 µg) and TGF-β1 (0.5% w/w=15 µg) (n=8)
Group 3 (medium-dose group): titanium cage coated with a biodegradable PDLLA carrier including IGF-I (5.0% w/w=150 µg) and TGF-β1 (1.0% w/w=30 µg) (n=8)
Group 4 (high-dose group): titanium cage coated with a biodegradable PDLLA carrier including IGF-I (10% w/w=300 µg) and TGF-β1 (2.0% w/w=60 µg) (n=8)
After 12 weeks all sheep were sacrificed and radiographic, biomechanical and histological evaluations were performed. All animal experimental work was approved by local authorities.
Coating of the cages
Poly-(D,L-lactide) (PDLLA, Boehringer Ingelheim, Germany) was chosen as drug carrier system. The properties of the PDLLA coating and the coating technique have been described previously [17, 48]. In groups 2–4, recombinant human insulin like growth factor I (IGF-I, R&D Systems) was incorporated in the PDLLA coating at a level of 2.5, 5 and 10% w/w for group 1, group 2 and group 3 respectively, and recombinant human transforming growth factor-beta 1 (TGF-β1, R&D Systems) was incorporated at a level of 0.5, 1 and 2% w/w) respectively. The average PDLLA coating mass of the cages was 3.02±0.12 mg. There was no difference between the total coating mass of the different groups. Therefore, approximately 75, 150 and 300 µg IGF-I plus 15, 30 and 60 µg TGF-β1 were incorporated in the coating of the respective cages.
Surgical technique and postoperative care
The animals underwent the surgical procedure under general endotracheal anaesthesia. The anterior part of the neck was prepped in a sterile fashion and a left anterolateral approach to the cervical spine was carried out through a longitudinal skin incision. The longus colli muscle was incised in the midline, and the intervertebral disc C3/4 was exposed. After distraction of the motion segment with a Caspar distractor, anterior discectomy C3/4 was performed. The endplates were uniformly shaved with a 2-mm high-speed diamond drill down to bleeding bone. For interbody stabilization, the coated meshed titanium cages (Motech GmbH, Schwenningen, Germany, height 8 mm, diameter 14 mm) including the growth factors were inserted uniformly into the intervertebral space. Finally, the wound was irrigated with saline and the longus colli muscle, the subcutaneous tissue and the skin were reapproximated with sutures and a soft bandage was applied to the neck.
After surgery, the animals were maintained under observation until fully recovered from general anaesthesia. They received two doses of 0.5 g metamizol-natrium (Novaminsulfon, Lichtenstein) per day for 5 days intramuscularly. Clinical examination was performed daily for the first 10 days, then weekly. The sheep were allowed ad libitum activity for the remainder of the experiment. Fluorochrome sequential labels were administered at 3, 6, and 9 weeks postoperatively, consisting of oxytetracyclin (25 mg/kg IV) at 3 weeks, calcein green (15 mg/kg IV) at 6 weeks, and xylenol orange (90 mg/kg IV) at 9 weeks. Twelve weeks after surgery, the animals were killed after induction of anaesthesia by an intravenous injection of potassium chloride. The complete cervical spine, including parts of the occiput and T1, was then excised and cleaned from the surrounding tissue.
Blood and serum analysis
Blood and serum samples were taken from the saphenous vein of the hind leg of the sheep pre- and postoperatively and after 1, 2, 4, 8, and 12 weeks. The blood samples were analysed for routine laboratory parameters (blood count, electrolytes, alkaline phosphatase, thyroid values and glucose).
Body weight and body temperature analysis
Preoperatively, and after 1, 2, 4, 8, and 12 weeks, rectal body temperature and body weight were determined.
Radiographic analysis
Radiographic evaluations have been described in detail earlier [24]. Lateral and posteroanterior digital radiographic scans (X-ray unit: Mobilett Plus, Siemens AG, Germany; X-ray films: Fuji CR 24×30, Fuji, Germany) were performed pre- and postoperatively, and after 1, 2, 4, 8, and 12 weeks. At the same time periods, anterior, middle and posterior intervertebral disc space heights (DSH) and intervertebral angle (IVA) of the motion segment C3/4 were measured on lateral radiographic scans. Average intervertebral DSH was calculated from anterior, middle and posterior DSH measurements (anterior, middle and posterior DSH/3). All radiographic measurements were evaluated by three independent observers.
Quantitative CT analysis
Quantitative CT scans (QCT) were performed using a Siemens Somatom plus 4 scanner (Siemens Inc., Erlangen, Germany). Axial cuts with 1 mm slice thickness were made parallel to the intervertebral disc space. Bone mineral density (BMD) and bone volume measurements of the callus have been described in detail earlier [24]. BMD measurements were calibrated with a six-point bone mineral density phantom and were performed using software specific to the scanner (Sienet Magic View VA 30A, Siemens, Inc., Erlangen, Germany). Bony callus volume (BCV) was measured using an image analysing system (Zeiss KS 400, Zeiss GmbH, Germany). Bone mineral content (BMC) was calculated from BMD and BCV measurements (BMC=BCV×BMD). All CT measurements were evaluated by three independent observers.
Biomechanical analysis
After euthanasia, biomechanical testing was performed by a non-destructive flexibility method using a non-constrained testing apparatus described in detail earlier [23, 24, 25]. Pure bending moments of 6 Nm load were applied to the motion segments C3/4 using a system of cables and pulleys to induce flexion, extension, left and right lateral bending and left and right axial rotation. Tension was applied to the cables with a uniaxial testing machine (1456, Zwick GmbH, Ulm, Germany). Three-dimensional displacement of each motion segment was measured using an optical measurement system (Qualysis Inc., Sävebalden, Sweden). Triangular markers with three diodes (Qualysis Inc.) were attached to the bodies of C3 and C4. Marker positions were detected with two cameras and recorded with a computerized motion analysis system (PC-Reflex, Qualysis Inc.). Angular displacement of the upper vertebra (C3) in relation to the lower vertebra (C4) was calculated from marker positions using custom-made computer software. The measurement error associated with this method was ±0.1° [25]. Range of motion (ROM), and neutral (NZ) and elastic (EZ) zones were determined.
Histomorphological, histomorphometrical and fluorochrome analysis
All C3/4 motion segments were harvested at 12 weeks for bone histology. The motion segments had been fixed for 7 days in 10% normal buffered formaldehyde followed by dehydration in ascending concentrations of ethanol and embedded undecalcified in methylmethacrylate (Technovit 9100, Heraeus Kulzer GmbH, Germany).
For histomorphological and histomorphometrical analysis, longitudinal sections in the sagittal plane were cut at 6 µm with a Leica SM 2500S microtome and a 40° stainless steel knife. Afterwards, the residual parts of the cages were removed and the following stains were used: (1) Safranin-O/Lightgreen, (2) Safranin-O/van Kossa, (3) Astrablue, and (4) Masson-Goldner.
Masson-Goldner stainings were used for histomorphological analysis. Histomorphometrical parameters were measured on Safranin-O/Lightgreen, Safranin-O/van Kossa and Astrablue stainings using a Leica DM-RB microscope and an image analysing system (Zeiss KS 400, Zeiss GmbH, Germany). Parameters were measured at a magnification of ×1.6.
The sagittal diameter distance (S) of C3 and the average preoperative DSH were determined to define the size of the region of interest (ROI) for histomorphometrical evaluation [26, 27]. The complete intervertebral fusion area was included in this ROI. The following structural indices were calculated in the ROI: bone volume/total volume (BV/TV), cartilage volume/total volume (CV/TV), mineralised cartilage volume/cartilage volume (mCV/CV).
For fluorochrome analysis, longitudinal sections in the parasagittal plane were cut at 400 µm with a precise macro grinding machine (Fa. Exact, Norderstedt, Germany). These slices were then ground to a thickness of 80 µm using a precise micro grinding machine (Fa. Exact). Fluorochrome markers were analysed under appropriate lightning conditions using a Leica DM-RB microscope and an image analysing system (Zeiss KS 400, Zeiss GmbH). Parameters were measured at a magnification of ×1.6.
Fluorochrome analysis of intervertebral fusion areas has been described in detail previously [60]. The first appearance of the marker served to time formation of new bone matrix. The presence or absence of each marker around or within the cage was used to determine the relative time frame of new bone formation.
Statistical analysis
Comparison of data was performed using one way ANOVA for independent samples followed by TUKEY post-hoc analysis for multiple comparison procedures with Bonferroni correction for multiple measurements. Intraobserver variability for radiographic, functional radiographic evaluation and CT measurements was determined using kappa statistics. Statistically significant differences were defined at a 95% confidence level. The values are given as mean ± standard deviation. SPSS (release 10.0, SPSS Inc. Chicago, Illinois) software supported statistical evaluation.
Results
Blood and serum analysis results
Full blood count did not show any significant differences between the groups and throughout the experiment. Levels of electrolytes (Na, K, Cl, Ca) did not show significant changes during the experimental period. Furthermore, no differences of thyroid hormones, alkaline phosphatase and glucose levels were found throughout the observation period and between all groups.
Body weight and body temperature
No significant differences were found between all groups in mean body temperature and body weight throughout the experimental period. Postoperatively, a slight and constant increase in body weight for all sheep of all groups was determined.
Radiographic results
Intraobserver agreement for radiographic measurements was good, showing kappa values ranging between 0.78 and 0.94. Preoperative baseline values of all radiographic parameters did not show any differences between the groups. No significant differences were found for average disc space height and intervertebral angle between all groups throughout the observation period. After a slight postoperative increase of disc space height and intervertebral angle due to intervertebral cage stabilization, these parameters decreased to preoperative values within 2 weeks. After these first 2 weeks no significant further loss of disc space height and intervertebral angle occurred.
Quantitative computed tomographic results
Intraobserver agreement for CT measurements was excellent, showing kappa values ranging between 0.88 and 0.98. After 12 weeks, bony callus volume (BCV) was significantly lower in the cage group without growth factors (group 1) than in any other group (P<0.05) (Table 1 ). Additionally, the medium- and high-dose growth factor groups (groups 3 and 4) showed a significantly (P<0.05) higher BCV than the low-dose growth factor group (group 2). There were no significant differences in bone mineral content (BMC) between the cage group without growth factors (group 1) and the low-dose growth factor group (group 2). However, the medium- and high-dose growth factor groups (groups 3 and 4) demonstrated a significantly (P<0.05) higher BMC than both other groups (groups 1 and 2). There was no significant difference for bone mineral density of the callus (BMD) between all groups.
Table 1.
After 12 weeks, quantitative computed tomographic analysis (QCT) was performed to measure bone mineral density (BMD), bone mineral content (BMC) and bony callus volume (BCV) [PDLLA poly-(D,L-lactide]
| QCT (parameters) | Group 1 (n=8) cage + PDLLA | Group 2 (n=8) cage + PDLLA + IGF-I (0.5%) + TGF-β1 (2.5%) | Group 3 (n=8) cage + PDLLA + IGF-I (1%) + TGF-β1 (5%) | Group 4 (n=8) Cage + PDLLA + IGF-I (2%) + TGF-β1 (10%) |
|---|---|---|---|---|
| BMD (g/cm3) | 0.62±0.03 (0.59–0.66) | 0.62±0.03 (0.58–0.66) | 0.64±0.04 (0.59–0.68) | 0.65±0.04 (0.60–0.69) |
| BMC (g) | 2.1±0.5 (1.3–2.6) | 2.6±1.5 (2.7–5.8) | 3.4±1.6a (2.4–5.5) | 3.5±1.6a (2.4–5.5) |
| BCV (cm3) | 3.4±0.9 (2.5–4.3) | 4.2±1.1a (4.4–7.1) | 5.2±1.2a,b (4.1–6.8) | 5.4±1.0a,b (4.1–6.8) |
aP<0.05 in comparison to group 1
bP<0.05 in comparison to group 2
Biomechanical results
Biomechanical results for range of motion (ROM), neutral zone (NZ) and elastic zone (EZ) are depicted in Table 2 . Lowest ROM, NZ and EZ values were constantly found for the high-dose growth factor group (group 4). ROM in all directions, except flexion, and NZ and EZ in rotation and lateral bending were significantly (P<0.05) lower in the medium- and high-dose growth factor groups (groups 3 and 4) than in the cage group without growth factors (group 1). No significant difference for ROM, NZ and EZ in any direction was found between the cage without growth factor group (group 1) and the cage plus low dose growth factors (group 2). Additionally, no significant difference was found between the medium (group 3) and high (group 4) -dose growth factor group. In comparison to the low-dose growth factor group (group 2), the medium- and high-dose growth factor groups (groups 3 and 4) showed a significantly (P<0.05) lower ROM in rotation and lateral bending and a significantly (P<0.05) lower NZ and EZ in rotation.
Table 2.
Biomechanical analysis: after 12 weeks, biomechanical analysis was performed to measure range of motion (ROM), neutral (NZ) and elastic zone (EZ) for the different test modes
| Test modes (degrees) | Group 1 (n=8) cage + PDLLA | Group 2 (n=8) cage + PDLLA + IGF-I (0.5%) + TGF-β1 (2.5%) | Group 3 (n=8) cage + PDLLA + IGF-I (1%) + TGF-β1 (5%) | Group 4 (n=8) cage + PDLLA + IGF-I (2%) + TGF-β1 (10%) |
|---|---|---|---|---|
| Flexion | ||||
| ROM | 3.0±0.9 | 2.9±1.0 | 2.9±1.2 | 2.7±1.0 |
| NZ | 0.5±0.7 | 0.5±0.7 | 0.7±0.7 | 0.6±0.5 |
| EZ | 2.5±0.9 | 2.4±0.9 | 2.3±0.8 | 2.1±0.8 |
| Extension | ||||
| ROM | 3.3±1.2 | 3.0±1.1 | 2.2±0.7a | 2.2±0.8a |
| NZ | 1.4±1.0 | 1.1±0.6 | 0.6±0.5 | 0.5±0.6 |
| EZ | 1.9±0.3 | 1.9±0.6 | 1.6±0.3 | 1.7±0.5 |
| Right rotation | ||||
| ROM | 2.4±0.8 | 2.0±0.3 | 1.4±0.3a,b | 1.2±0.4a,b |
| NZ | 0.4±0.3 | 0.4±0.3 | 0.2±0.1a,b | 0.2±0.1a,b |
| EZ | 2.0±0.6 | 1.6±0.3 | 1.2±0.3a,b | 1.0±0.3a,b |
| Left rotation | ||||
| ROM | 2.3±0.5 | 1.9±0.5 | 1.5±0.4a,b | 1.2±0.4a,b |
| NZ | 0.3±0.1 | 0.3±0.1 | 0.2±0.1a,b | 0.2±0.1a,b |
| EZ | 2.0±0.5 | 1.8±0.5 | 1.3±0.3a,b | 1.0±0.4a,b |
| Right bending | ||||
| ROM | 4.1±1.0 | 3.2±0.7 | 2.5±0.7a,b | 2.4±0.6a,b |
| NZ | 0.7±0.4 | 0.6±0.3 | 0.6±0.3a | 0.5±0.3a |
| EZ | 3.4±0.9 | 2.8±0.8 | 1.9±0.7a | 1.9±0.6a |
| Left bending | ||||
| ROM | 4.2±0.7 | 3.3±0.6 | 2.5±0.8a,b | 2.3±0.7a,b |
| NZ | 0.8±0.7 | 0.8±0.3 | 0.5±0.4a | 0.4±0.2a |
| EZ | 3.4±0.8 | 2.5±0.5 | 2.0±0.5a | 1.9±0.7a |
aP<0.05 in comparison to group 1
bP<0.05 in comparison to group 2
Histomorphological results
Histomorphological analysis supported the findings of computed tomographic and biomechanical examinations (Fig. 1). In the cage plus PDLLA group (group 1), mainly fibroblasts and occasionally cartilage cells were observed between the endplates. Cages were surrounded by a distinct thin line of fibroblasts interrupted by some small bony islands. Group 2, stabilised with cages including a low dose of IGF-I and TGF-β1, showed some bony islands between the endplates with cartilage and fibrous tissue components. The tissue surrounding the cages appeared similar to group 1. Groups 3 and 4, stabilised with cages including medium and high doses of IGF-I and TGF-β1, showed extensive callus formation and large bony islands or complete bony bridging between the endplates with small cartilage and fibrous tissue components. Most of the callus was seen inside the cage. These findings were accompanied by capillary ingrowth and small resorptive lacunae without major differences between the two groups. Cages were surrounded by bone; however, in some areas a distinct thin line of fibroblasts was obvious. Beside that, no ossifications of the spinal ligaments were investigated in any group.
Fig.1A–E.
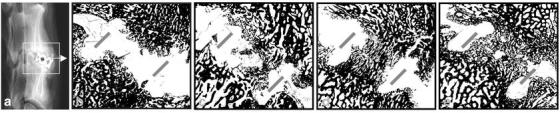
Histomorphological analysis of the intervertebral fusion area. After 12 weeks, interbody fusion was evaluated histomorphologically and histomorphometrically on midsagittal slides. Depicted is a digitalized view of a Safrin-O/van Kossa staining of the intervertebral fusion area (magnification ×1.6). Lateral radiograph of the sheep motion segment C3/4 (A) shows orientation of slides B–E. B is representative of group 1 (n=8) cage + poly-(D,L-lactide) (PDLLA), C of group 2 (n=8) cage + PDLLA + IGF-I (0.5%) + TGF-β1 (2.5%), D of group 3 (n=8) cage + PDLLA + IGF-I (1%) + TGF-β1 (5%), and E of group 4 (n=8) cage + PDLLA + IGF-I (2%) + TGF-β1 (10%). The grey bars represent the location of the branches of the cage
Histomorphometrical results
The results of histomorphometrical analysis are presented in Table 3 . Histomorphometrical analysis showed no significant differences in sagittal diameter index (baseline) between all groups. Compared to the cage without growth factor group (group 1) and the low-dose growth factor group, histomorphometrical parameters revealed a significantly (P<0.05) higher bone volume/total volume ratio in the medium- and high-dose growth factor groups (groups 3 and 4). No differences in the bone volume/total volume ratio were found between the medium- (group 3) and high-dose (group 4) growth factor group. There were no differences in the other histomorphometrical parameters for all groups.
Table 3.
After 12 weeks, histomorphometrical analysis was performed and the following structural indices were calculated in the region of interest (ROI): sagittal diameter distance (SDD, baseline), bone volume/total volume (BV/TV), cartilage volume/total volume (CV/TV), mineralised cartilage volume/cartilage volume (mCV/CV)
| Indices | Group 1 (n=8) cage + PDLLA | Group 2 (n=8) cage + PDLLA + IGF-I (0.5%) + TGF-β1 (2.5%) | Group 3 (n=8) cage + PDLLA + IGF-I (1%) + TGF-β1 (5%) | Group 4 (n=8) cage + PDLLA + IGF-I (2%) + TGF-β1 (10%) |
|---|---|---|---|---|
| SDD (mm) | 25.9±1.6 (24.3–27.8) | 25.7±1.4 (24.0–27.1) | 26.6±1.1 (25.3–28.3) | 26.1±1.3 (24.6–28.1) |
| BV/TV (%) | 41.8±3.2 (31.7–50.2) | 42.1±2.4 (33.7–46.3) | 43.3±2.8a,b (33.8–51.4) | 43.6±2.8a,b (33.8–51.4) |
| CV/TV (%) | 4.4±2.1 (1.9–9.2) | 4.3±1.8 (2.1–8.0) | 4.8±2.4 (0.8–14.6) | 4.7±2.2 (1.3–11.2) |
| mCV/CV (%) | 3.6±1.0 (1.9–5.8) | 3.0±1.1 (1.4–5.5) | 3.2±1.2 (1.8–5.7) | 3.7±1.1 (2.0–5.4) |
aP<0.05 in comparison to group 1
bP<0.05 in comparison to group 2
Fluorochrome analysis results
The results of fluorochrome analysis are depicted in Table 4 . The IGF-I/TGF-β1 coated cages (groups 2, 3 and 4) exhibited earlier new bone formation both within and around the cages compared to the group without growth factors (group 1). There were no differences in fluorochrome marker appearance between all groups after 6 and 9 weeks.
Table 4.
After 12 weeks, fluorochrome analysis was performed. Depicted are the number of fusion sites (of the different groups at different time points) in which the fluorochrome marker was present adjacent or within the cage or bone graft, respectively
| Indices | Group 1 (n=8) cage + PDLLA | Group 2 (n=8) cage + PDLLA + IGF-I (0.5%) + TGF-β1(2.5%) | Group 3 (n=8) cage + PDLLA + IGF-I (1%) + TGF-β1 (5%) | Group 4 (n=8) cage + PDLLA + IGF-I (2%) + TGF-β1 (10%) | ||||
|---|---|---|---|---|---|---|---|---|
| Adjacent | Within | Adjacent | Within | Adjacent | Within | Adjacent | Within | |
| 3 weeks | 0 | 0 | 2 | 2 | 2 | 2 | 2 | 3 |
| 6 weeks | 3 | 6 | 3 | 4 | 4 | 4 | 4 | 5 |
| 9 weeks | 5 | 6 | 5 | 5 | 6 | 6 | 6 | 7 |
Discussion
Recently, in vitro and in vivo studies have demonstrated an osteoinductive effect of IGF-I and TGF-β1 application by direct and indirect mechanisms [31, 32, 37, 51, 52, 54]. IGF-I stimulates angiogenesis, the replication of osteoblasts and the synthesis of bone matrix [18, 20, 52]. TGF-β1 regulates differentiation and proliferation of different cell types that are directly involved in bone remodelling and bone matrix formation, like mesenchymal cells, chondrocytes, osteoblasts, and osteoclasts [29, 42, 45]. In vivo studies have shown that decreased levels of IGF-I or TGF-β1 are associated with bone loss and osteoporosis [1, 56, 58], whereas the local application of IGF-I or TGF-β1 can positively influence fracture healing [21, 38, 50]. In contrast to the BMPs, IGF-I and TGF-β1 are said to be unable to induce de novo bone in the absence of bone marrow elements [49, 50]. Therefore, both growth factors might be able to overcome the disadvantages, especially the ossification of spinal ligaments, associated with the use of BMPs in experimental spinal fusion.
Furthermore, in vitro and in vivo studies have demonstrated a significant osteoinductive effect combining IGF-I with growth factors of the TGF-superfamily [20, 26, 27, 49, 59]. Illi and Feldmann [20], for example, combined the application of IGF-I with BMP-2 in an osteotomy model of the metacarpal bone in juvenile calves. Yeh et al. [59] demonstrated that combined OP-1 (BMP-7) and IGF-I application has a synergistic stimulatory effect on fetal rat calvaria cells, by OP-1 induced regulation of IGF-binding proteins (IGFBP's). Schmidmaier et al. [49] demonstrated that the combined application of IGF-I and TGF-β1 had a significantly higher stimulating effect on bone matrix formation in rat tibia fractures than a single application of IGF-I or TGF-β1. They concluded that both growth factors had synergistic effects on fracture healing. Similar conclusions were drawn by other authors [33, 43].
These synergistic effects of IGF-I and TGF-β1 have been explained by interactions between the IGF and TGF systems [8, 11, 53, 57]. Tremollieres et al. [53] demonstrated that TGF-β1 is a potent modulator of IGF-I secretion. Kveiborg et al. [29] showed that TGF-β1 exerts a significant stimulatory effect on the IGF system, especially IGFBP-3, and concluded that this might represent a mechanism mediating TGF-β1 effects on the biological functions of cells. Additionally, a feedback mechanism between IGFBP-6 and TGF-β1 regulating the bone microenvironment was assumed [14]. Finally, O'Keefe et al. [40] demonstrated that IGF-I was able to augment the effects of TGF-β1 on cartilage cells.
Due to these synergistic effects, the combined application of IGF-I and TGF-β1 seems to be very promising for induction of bone matrix formation in the field of spine surgery. Additionally, in vivo studies have already demonstrated a significant osteoinductive effect of combined IGF-I and TGF-β1 application in a sheep cervical spine interbody fusion model [26, 27]. Kandziora et al. [26] were able to show an increased biomechanical stiffness and an accelerated intervertebral bone matrix formation comparing combined IGF-I and TGF-β1 application with an autologous tricortical iliac crest bone graft. Additionally, they demonstrated analogous osteoinductive effects comparing similar doses of BMP-2 and combined IGF-I and TGF-β1 application [27]. The results of these previous studies are in concordance with the results presented in this study. In comparison to the cage without growth factors (group 1), the medium- and high-dose growth factor groups (groups 3 and 4) demonstrated a significantly higher bony callus volume on CT scans, a higher biomechanical stability, an advanced interbody bone matrix formation in histomorphometrical analysis, and an earlier interbody bone matrix formation on fluorochrome sequence labelling. Although the medium- and high-dose growth factor groups (groups 3 and 4) showed an earlier and accelerated interbody bone matrix formation in comparison to the group without growth factors (group 1), the loss of disc space height and lordosis (intervertebral angle) was similar in all these groups. Therefore, especially in the first 2 weeks, loss of disc space height seems to be primarily related to the interbody implant and widely independent from the amount of new-formed bone.
For isolated application of IGF-I or TGF-β1, a positive correlation between increasing dose and stimulatory effects on bone matrix formation has already been described [3, 13]. IGF-I and TGF-β1 have dose-dependent effects on the activity of enzymes associated with bone matrix mineralisation [7, 44]. Panagakos [41] showed that TGF stimulated a dose-dependent increase in chemotaxis of osteoblasts. Fujimoto [13] and Noda [39] demonstrated that in vivo effects of TGF-β1 on bone matrix formation in rat varied depending on concentration. However, both authors also determined nearly similar osteoinductive effects of TGF-β1 in a wide range of concentrations [13, 39]. Additionally, Ebeling et al. [10] demonstrated analogous effects of four different doses of IGF-I on bone turnover in normal women. Although dose-dependent effects for isolated IGF-I and TGF-β1 application are sufficiently documented, to our knowledge, no study has been performed to determine whether a dose-dependent effect of combined IGF-I and TGF-β1 application on bone matrix formation exists.
Currently, the "ideal" concentrations to induce spinal fusion for any growth factors are unknown. This is due to the fact that each growth factor or growth factor combination has to be adapted to the local biological environment (anterior or posterior spinal fusion) and to the used carrier system. Some anterior spinal fusion models have shown good results, with BMP-2 doses ranging between 100 and 250 µg [4, 16, 60]. Other studies [27] demonstrated that equal doses of BMP-2 and IGF-I/TGF-β1 showed nearly similar osteoinductive capacities. Additionally, the 5:1 ratio of IGF-I and TGF-β1 applied by a PDLLA-coated implant has proven to be most effective [26, 27, 49]. Therefore, three different doses of a 5:1 ratio of IGF-I and TGF-β1 were evaluated in this anterior interbody fusion model.
In comparison to the low-dose growth factor group (group 2), the medium- and high-dose growth factor groups (groups 3 and 4) demonstrated a significantly higher bony callus volume on CT scans, a higher biomechanical stability in rotation, and an advanced interbody bone matrix formation (bone volume/total volume ratio) in histomorphometrical analysis. Although there was no difference between the low-dose growth factor group (group 2) and the medium- and high-dose growth factor groups (groups 3 and 4) in the appearance of fluorochrome markers using fluorochrome sequence labelling, the amount of new-formed bone was significantly higher with higher growth factor doses. However, no significant difference was determined between the medium- and high-dose growth factor groups (groups 3 and 4, respectively). Additionally, hardly any difference was determined between the low-dose growth factor group (group 2) and the group without growth factors (group 1). Therefore, the best dose-response relationship in this study was achieved with the medium growth factor dose (150 µg IGF-I plus 30 µg TGF-β1). As a further result of this study, the effective dose of IGF-I and TGF-β1 in this interbody fusion model was defined as between 75 and 150 µg IGF-I and between 15 and 30 µg TGF-β1. With increasing dose of these growth factors, no further stimulation of bone matrix formation was achieved. Due to the fact that no difference in blood and serum analysis, body weight and temperature and no acute illness of the sheep were determined in this study, the lethal doses for local combined IGF-I and TGF-β1 application must be significantly higher than 300 µg IGF-I plus 60 µg TGF-β1.
Currently, the reasons for these dose-dependent effects of combined IGF-I and TGF-β1 application on bone matrix formation in this sheep cervical spine fusion model are unknown. However, due to the interaction of the IGF-I and TGF systems, some inhibitory feedback mechanism activated with increasing doses of these growth factors might be possible.
Conclusion
The local application of IGF-I and TGF-β1 by a PDLLA coated cage significantly improved results of interbody bone matrix formation in this sheep cervical spine fusion model. The best dose-response relationship was achieved with the medium growth factor dose (150 µg IGF-I plus 30 µg TGF-β1). With an increasing dose of these growth factors, no further stimulation of bone matrix formation was observed. The effective dose of combined IGF-I and TGF-β1 application could be defined as between 75 and 150 µg IGF-I, and between 15 and 30 µg TGF-β1. Although these results are encouraging, further studies are essential to determine safety issues of combined IGF-I and TGF-β1 application for spinal fusion.
Footnotes
This study was carried out with the support of the MBI – Max Biedermann Institut der Steinbeis Stiftung (RS/KF-82042).
References
- 1.Ammann P, Bourrin S, Bonjour JP, Meyer JM, Rizzoli R (2000) Protein undernutrition-induced bone loss is associated with decreased IGF-I levels and oestrogen deficiency. J Bone Miner Res 15:683–669 [DOI] [PubMed]
- 2.Aspenberg P, Turek T (1996) BMP-2 for intramuscular bone induction. Effect on squirrel monkeys is dependent on implantation site. Acta Orthop Scand 67:3–6 [DOI] [PubMed]
- 3.Beck L, Amento E, Xu Y, Deguzman L, Lee W, Nguyen T, Gillet N (1993) TGF-beta 1 induces bone closure of skull defects – temporal dynamics of bone formation in defects exposed to rhTGF-beta 1. J Bone Miner Res 8:753–761 [DOI] [PubMed]
- 4.Boden SD, Martin GJ Jr, Horton WC, Truss TL, Sandhu HS (1998) Laparoscopic anterior spinal arthrodesis with rh BMP-2 in a titanium interbody threaded cage. J Spinal Disord 11:95–101 [PubMed]
- 5.Boden SD, Martin GJ Jr, Morone MA, Ugbo JL, Moskovitz PA (1999) Posterolateral lumbar intertransverse process spine arthrodesis with recombinant human bone morphogenetic protein 2/hydroxyapatite-tricalcium phosphate after laminectomy in the nonhuman primate. Spine 24:1179–1185 [DOI] [PubMed]
- 6.Boden SD, Zdeblick TA, Sandhu HS, Heim SE (2000) The use of rhBMP-2 in interbody fusion cages. Definitive evidence of osteoinduction in humans: a preliminary report. Spine 25:376–381 [DOI] [PubMed]
- 7.Bonewald LF, Schwartz Z, Swain LD, Ramirez V, Poser J, Boyan I (1990) Stimulation of plasma membrane and matrix vesicle enzyme activity by transforming growth factor-beta in osteosarcoma cultures. J Cell Physiol 145:200–206 [DOI] [PubMed]
- 8.Canalis E, Pash J, Gabbitas B, Rydziel S, Varghese S (1993) Growth factors regulate the synthesis of insulin-like growth factor-I in bone cell cultures. Endocrinology 133: 33–38 [DOI] [PubMed]
- 9.David SM, Gruber HE, Mayer RA Jr, Murakami T, Tabor OB, Howard BA, Wozney JM, Hanley EN Jr (1999) Lumbar spinal fusion using recombinant human bone morphogenetic protein in the canine. A comparison of three dosages and two carriers. Spine 24:1973–1979 [DOI] [PubMed]
- 10.Ebeling PR, Jones JD, O'Fallon WM, Janes CH, Riggs BL (1993) Short-term effects of recombinant human insulin-like growth factor I on bone turnover in normal women. J Clin Endocrinol Metab 77:1384–1387 [DOI] [PubMed]
- 11.Elford PR, Lamberts SW (1990) Contrasting modulation by transforming growth factor-beta 1 of insulin like growth factor-I production in osteoblasts and chondrocytes. Endocrinology 127:1635–1639 [DOI] [PubMed]
- 12.Fischgrund JS, James SB, Chabot MC, Hankin R, Herkowitz HN, Wozney JM, Shirkhoda A (1997) Augmentation of autograft using rhBMP-2 and different carrier media in the canine spinal fusion model. J Spinal Disord 10:467–472 [PubMed]
- 13.Fujimoto A, Tanizawa T, Nishida S, Yamamoto N, Soshi S, Endo N, Takahashi HE (1999) Local effects of transforming growth factor-beta 1 on rat calvaria: changes depending on the dose and the injection site. J Bone Miner Metab 17:11–17 [DOI] [PubMed]
- 14.Gabbitas B, Canalis E (1997) Growth factor regulation of insulin-like growth factor binding protein-6 expression in osteoblasts. J Cell Biochem 66:77–86 [DOI] [PubMed]
- 15.Grauer JN, Patel TC, Erulkar JS, Troiano NW, Panjabi MM, Friedlaender GE (2001) 2000 Young Investigator Research Award winner. Evaluation of OP-1 as a graft substitute for intertransverse process lumbar fusion. Spine 26:127–133 [DOI] [PubMed]
- 16.Hecht BP, Fischgrund JS, Herkowitz HN, Penman L, Toth JM, Shirkhoda A (1999) The use of recombinant human bone morphogenetic protein 2 (rhBMP-2) to promote spinal fusion in a nonhuman primate anterior interbody fusion model. Spine 24:629–636 [DOI] [PubMed]
- 17.Hermann R, Schmidmaier G, Markl B, Resch A, Hahnel I, Stemberger A, Alt E (1999) Antithrombogenic coating of stents using a biodegradable drug delivery technology. Thromb Haemost 82:51–57 [PubMed]
- 18.Hock J, Centrella M, Canalis E (1998) Insulin like growth factor I has independent effects on bone matrix formation and cell replication. Endocrinology 122:254–260 [DOI] [PubMed]
- 19.Hoshi K, Amizuka N, Sakou T, Kurokawa T, Ozawa H (1997) Fibroblasts of spinal ligaments pathologically differentiate into chondrocytes induced by recombinant human bone morphogenetic protein-2: morphological examinations for ossification of spinal ligaments. Bone 21:155–162 [DOI] [PubMed]
- 20.Illi OE, Feldmann CP (1998) Stimulation of fracture healing by local application of humeral factors integrated in biodegradable implants. Eur J Pediatr Surg 8:251–255 [DOI] [PubMed]
- 21.Isgaard J, Nilson A, Lindahl A, Jansson J, Isaksson O (1986) Effects of local administration of GH and IGF-I on longitudinal bone growth in rats. Am J Physiol 250:367–372 [DOI] [PubMed]
- 22.Itoh H, Ebara S, Kamimura M, Tateiwa Y, Kinoshita T, Yuzawa Y, Takaoka K (1999) Experimental spinal fusion with use of recombinant human bone morphogenetic protein 2. Spine 24:1402–1405 [DOI] [PubMed]
- 23.Kandziora F, Kerschbaumer F, Starker M, Mittlmeier T (2000) Biomechanical assessment of transoral plate fixation for atlantoaxial instability. Spine 25:1555–1561 [DOI] [PubMed]
- 24.Kandziora F, Pflugmacher R, Scholz M, Schnake K, Schröder R, Mittlmeier T (2001) Comparison between sheep and human cervical spines: an anatomic, radiographic, bone mineral density, and biomechanical study. Spine 26:1028–1037 [DOI] [PubMed]
- 25.Kandziora F, Pflugmacher R, Schäfer J, Duda G, Haas NP, Mittlmeier T (2001) Biomechanical comparison of cervical spine interbody fusion cages. Spine 26:1850–1857 [DOI] [PubMed]
- 26.Kandziora F, Schmidmaier G, Schollmeier G, Bail H, Pflugmacher R, Görke T, Wagner M, Raschke M, Mittlmeier T, Haas NP (2002) IGF-I and TGF-β1 application by a poly-(D,L-lactide) coated cage promotes intervertebral bone matrix formation in the sheep cervical spine. Spine 27:1710–1723 [DOI] [PubMed]
- 27.Kandziora F, Pflugmacher R, Scholz M, Knispel C, Hiller T, Schiollmeier G, Bail H, Schmidmaier G, Duda G, Raschke M, Haas NP (2002) Comparison of BMP-2 and combined IGF-I/TGF-β1 application in a sheep cervical spine fusion model. Eur Spine J 11:482–493 [DOI] [PMC free article] [PubMed]
- 28.Kon T, Yamazaki M, Tagawa M, Goto S, Terakado A, Moriya H, Fujimura S (1997) Bone morphogenetic protein-2 stimulates differentiation of cultured spinal ligament cells from patients with ossification of the posterior longitudinal ligament. Calcif Tissue Int 60:291–296 [DOI] [PubMed]
- 29.Kveiborg M, Flyvbjerg A, Eriksen EF, Kaasem M (2001) Transforming growth factor beta 1 stimulates production of insulin-like growth factor-I and insulin-like growth factor-binding protein-3 in human bone marrow stromal osteoblast progenitors. J Endocrinol 169:549–561 [DOI] [PubMed]
- 30.Laursen M, Hoy K, Hansen ES, Gelineck J, Christensen FB, Bunger CE (1999) Recombinant bone morphogenetic protein-7 as an intracorporal bone growth stimulator in unstable thoracolumbar burst fractures in humans: preliminary results. Eur Spine J 8:485–490 [DOI] [PMC free article] [PubMed]
- 31.Lind M (1998) Growth factor stimulation on bone healing. Effects on osteoblasts, osteotomies, and implants fixations. Acta Orthop Scand Suppl 283:2–37 [PubMed]
- 32.Lind M, Schuhmacker B, Soballe K, Keller J, Melson F, Bunger C (1993) Transforming growth factor-beta enhances fracture healing in rabbit tibiae. Act Orthop Scand 64:553–556 [DOI] [PubMed]
- 33.Ma ZJ, Misawa H, Yamaguchi M (2001) Stimulatory effect of zinc on insulin-like growth and transforming growth factor beta 1 production with bone growth of new-born rats. Int J Mol Med 8:623–628 [DOI] [PubMed]
- 34.Martin GJ Jr, Boden SD, Marone MA, Marone MA, Moskovitz PA (1999) Posterolateral intertransverse process spinal arthrodesis with rhBMP-2 in a nonhuman primate: important lessons learned regarding dose, carrier, and safety. J Spinal Disord 12:179–186 [PubMed]
- 35.Meyer RA Jr, Gruber HE, Howard BA, Tabor OB Jr, Murakami T, Kwiatkowski TC, Wozney JM, Hanley EN Jr (1999) Safety of recombinant human bone morphogenetic protein-2 after spinal laminectomy in the dog. Spine 24:747–754 [DOI] [PubMed]
- 36.Mimatsu K, Kishi S, Hashizume Y (1997) Experimental chronic compression on the spinal cord of the rabbit by ectopic bone formation in the ligamantum flavum with bone morphogenetic protein. Spinal Cord 35:740–746 [DOI] [PubMed]
- 37.Mohan S, Baylink D (1991) Bone growth factors. Clin Orthop Rel Res 263:30–48 [PubMed]
- 38.Nielson H, Isgaard J, Lindahl A, Peterson L, Isaksson O (1987) Effects of unilateral arterial infusion of GH and IGF-I on tibial longitudinal bone growth in hypophysectomized rats. Calcif Tissue Int 40:91–96 [DOI] [PubMed]
- 39.Noda M, Camilliere JJ (1989) In vivo stimulation of bone formation by transforming growth factor-beta. Endocrinology 124:2991–2994 [DOI] [PubMed]
- 40.O'Keefe RJ, Crabb ID, Puzas JE, Rosier RN (1994) Effects of transforming growth factor-beta 1 and fibroblast growth factor on DNA synthesis in growth plate chondrocytes are enhanced by insulin-like growth factor-I. J Orthop Res 12:299–310 [DOI] [PubMed]
- 41.Panagakos FS (1994) Transforming growth factor alpha stimulates chemotaxis of osteoblasts and osteoblast-like cells in vitro. Biochem Mol Biol Int 33:643–650 [PubMed]
- 42.Pfeilschifter J, Oechsner M, Naumann A, Gronwald R, Minne H, Ziegler R (1990) Stimulation of bone matrix apposition in vitro by local growth factors: a comparison between insulin-like growth factor I, platelet derived growth factor and transforming growth factor beta. Endocrinology 127:69–75 [DOI] [PubMed]
- 43.Pfeilschifter J, Laukhuf F, Muller Beckmann B, Blim WF, Pfister H, Ziegler R (1995) Parathyroid hormone increases the concentration of insulin-like growth factor-I and transforming growth factor beta 1 in rat bone. J Clin Invest 96:767–774 [DOI] [PMC free article] [PubMed]
- 44.Richman C, Baylink DJ, Lang K, Dony C, Mohan S (1999) Recombinant human insulin-like growth factor-binding protein 5 stimulates bone formation parameters in vitro and in vivo. Endocrinology 140:4699–4705 [DOI] [PubMed]
- 45.Roberts A, Sporn M, Bolander M (1990) Transforming growth factor-beta and the initiation of chondrogenesis in the rat femur. J Cell Biol 110:2195–2207 [DOI] [PMC free article] [PubMed]
- 46.Sandhu HS, Kanim LE, Kabo JM, Toth JM, Zeegen EN, Liu D, Delamater RB, Dawson EG (1996) Effective doses of recombinant human bone morphogenetic protein-2 in experimental spinal fusion. Spine 21:2115–2122 [DOI] [PubMed]
- 47.Sandhu HS, Kanim LE, Toth JM, Kabo Jm, Liu D, Delamarter RB, Dawson EG (1997) Experimental spinal fusion with recombinant human bone morphogenetic protein-2 without decortication of osseous elements. Spine 22:1171–1180 [DOI] [PubMed]
- 48.Schmidmaier G, Wildemann B, Stemberger A, Haas NP, Raschke M (2001) Biodegradable poly-(D,L-lactide) coating of implants for continuous release of growth factors. J Biomed Mat Res 58:449–455 [DOI] [PubMed]
- 49.Schmidmaier G, Wildemann B, Stemberger A, Haas NP, Raschke M (2001) Local application of growth factors (insulin-like growth factor-I and transforming growth factor-beta1) from a biodegradable poly(D,L-lactide) coating of osteosynthetic implants accelerates fracture healing in rats. Bone 28:341–350 [DOI] [PubMed]
- 50.Steinbrech DS, Mehrara BJ, Rowe NM, Dudziak ME, Luchs JS, Saadeh PB, Gittes GK, Longaker MT (2000) Gene expression of TGF-beta, TGF-beta receptor, and extracellular matrix proteins during membranous bone healing in rats. Plast Reconstr Surg 105:2028–2038 [DOI] [PubMed]
- 51.Terrell TG, Working PK, Chow CP, Green JD (1993) Pathology of recombinant human transforming growth factor-beta 1 in rats and rabbits. Int Rev Exp Pathol 34B:43–67 [DOI] [PubMed]
- 52.Thaller S, Hoyt J, Tesluck H, Holmes R (1993) The effect of insulin growth factor-I on calvarial sutures in Sprague-Dawley rat. J Craniofac Surg 4:35–39 [DOI] [PubMed]
- 53.Tremollieres FA, Strong DD, Baylink DJ, Mohan S (1991) Insulin-like growth factor II and transforming growth factor beta 1 regulate insulin-like growth factor I secretion in mouse bone cells. Acta Endocrinol 125:538–546 [DOI] [PubMed]
- 54.Trippel S, Coutts R, Einhorn T, Mundy R, Rosenfeld R (1996) Growth factors as therapeutic agents. J Bone Joint Surg Am 78:1272–1286
- 55.Urist MR (1965) Bone: formation by autoinduction. Science 150:893–899 [DOI] [PubMed]
- 56.Wilton P (1992) Treatment with recombinant human insulin-like growth factor I of children with growth hormone receptor deficiency (Laron syndrome). Kabi Pharmacia Study Group on insulin-like growth factor I treatment in growth hormone insensitivity syndromes. Acta Paediatr Suppl 383:137–142 [PubMed]
- 57.Yaeger PC, Masi TL, de Oritz JL, Binette F, Tubo R, Mc Pherson J (1997) Synergistic action of transforming growth factor-beta and insulin-like growth factor-I induces expression of Type II collagen and aggrecan genes in adult human articular chondrocytes. Exp Cell Res 15:318–325 [DOI] [PubMed]
- 58.Yamada Y, Harada A, Hosoi T, Miyauchi A, Ikeda K, Otha H, Shiraki M (2000) Association of transforming growth factor beta 1 genotype with therapeutic response to active vitamin D for postmenopausal osteoporosis. J Bone Miner Res 15:415–420 [DOI] [PubMed]
- 59.Yeh LC, Adamo ML, Olson MS, Lee JC (1997) Osteogenic protein-1 and insulin-like growth factor I synergistically stimulate rat osteoblastic cell differentiation proliferation. Endocrinology 138:4181–4190 [DOI] [PubMed]
- 60.Zdeblick TS, Ganayem AJ, Rapoff AJ, Swain C, Bassett T, Cooke ME, Markel M (1998) Cervical interbody fusion cages. An animal model with and without bone morphogenetic protein. Spine 23:758–765 [DOI] [PubMed]
- 61.Zegzula HD, Buck DC, Brekke J, Wozney JM, Hollinger JO (1997) Bone formation with use of rhBMP-2 (recombinant human bone morphogenetic protein-2). J Bone Joint Surg Am 79:1778–1790 [DOI] [PubMed]


