Abstract
The purpose of this study was to assess the outcome of peri-radicular infiltration for radicular pain in patients with spinal stenosis and lumbar disc herniation (LDH). Patients with spinal stenosis (n=62) or LDH (n=55) who met our criteria received fluoroscopically guided peri-radicular infiltration of local anaesthetic and steroid at the site of documented pathology. All the patients were followed-up at 3 months. There was a statistically significant difference in the functional outcome between the spinal stenosis group and the LDH group. The mean change in the Oswestry disability index (ODI) score for the spinal stenosis group was 5.5% compared to 12% for the LDH group. The spinal stenosis group had a mean change in visual analogue scales (VAS) of 1.2 compared to 2 for the LDH group. The higher the modified somatic perception score, modified zung depression and age at injection, the less favourable the outcome. There was a significantly better response to peri-radicular infiltration for radicular pain in patients with LDH than the spinal stenosis. Our findings help us to provide a better information for future patients. We do not know if this is a treatment effect or natural history of the pathology, as this is a cohort study and not a randomised controlled trial.
Keywords: Peri-radicular infiltration, Radicular pain, Spinal stenosis, Lumbar disc herniation, Prognostic factors
Introduction
The efficacy of epidural steroid injection for the treatment of sciatica is surrounded by controversy. Its results have been described in more than forty studies with an average success rate of 67% [2]. Koes et al. [13] reviewed the outcome of 12 randomised controlled trials and concluded that its efficacy remains to be established.
Peri-radicular infiltration is a target-specific technique that aims to deliver a small amount of a high concentration of local anaesthetic and steroid to the site of documented pathology. It addresses two of the drawbacks of epidural injection, which include poor penetration to the irritated nerve root [1] and misplacement of epidural injectate [4]. It was first introduced in 1971 as a diagnostic test for patients with clinical findings of nerve root irritation [16]. Tajima et al. [29] later explored its therapeutic value and reported their results in 1980. Four studies conducted by Weiner et al. [33], Lutz et al. [15], Pfirrmann et al. [26] and Karppinen et al. [11] in the last decade have all demonstrated its value in relieving discogenic sciatic pain. However, there are relatively few prospective studies [3, 27] that examine its efficacy in relieving stenotic-type radicular pain.
The natural history of spinal stenosis is favourable in most patients [10], and a non-randomised study confirmed the efficacy of non-operative care [25]. There is a subgroup of patients with intractable radicular pain secondary to peripheral spinal stenosis that fail to resolve with conservative treatment. Our aim was to study the therapeutic value of peri-radicular infiltration for this subgroup of patients. It is a less hazardous alternative to operative intervention as lumbar spinal stenosis usually occurs in an elderly population that may have surgical morbidity. The prognostic value of various factors is also examined in this study.
Patients and methods
We prospectively recruited 125 consecutive patients between February 1995 and August 2002. Of these, 117 patients (93.6%) had a full data set available. Table 1 shows the baseline characteristic of the patients with spinal stenosis and lumbar disc herniation (LDH). All the patients were recruited from a spine specialist clinic and the procedure was performed by the senior author only. No patient refused the treatment offered. The inclusion criteria were as follow: clinical evidence of unilateral radicular pain that lasted despite at least 6 weeks of conservative management, magnetic resonance imaging (MRI) confirmation of nerve root compression secondary to LDH or peripheral degenerative spinal stenosis. The MRI findings of the disc morphology were classified as protrusion, contained herniation (disc herniation not extending through the posterior longitudinal ligament) and extrusion (herniation extruding through the posterior longitudinal ligament). Peripheral degenerative lumbar stenosis was classified as foraminal and far lateral compression secondary to spondylolisthesis. A single experienced MRI radiologist read all the images. The exclusion criteria were a previous spinal operation, cauda equina syndrome, previous epidural injection, anti-coagulation treatment, history of bleeding disorder, pregnancy, or allergy to the treatment agents.
Table 1.
Baseline data of patients with LDH and spinal stenosis, where applicable mean ± SE are shown (LDH lumbar disc herniation, SE standard error)
| LDH | Spinal stenosis | |
|---|---|---|
| No. of patients | 55 | 62 |
| Gender | 26 females | 30 females |
| 29 males | 32 males | |
| Age (years) | 40.2±12.4 | 62±13.5 |
| Employed | 38 | 19 |
| Unemployed | 9 | 2 |
| Retired | 6 | 30 |
| Others (housewife, student) | 2 | 11 |
| Duration of sciatica (months) | 19±21.6 | 28.66±23 |
The pre-injection parameters recorded for this study included gender, age at injection, duration of symptoms, Oswestry disability index score (ODI), low back outcome score (LBOS), visual analogue scales (VAS) for radicular pain, modified Zung depression scale (MZDS) and modified somatic perception questionnaire (MSPQ). The outcome measures include the change in ODI score, change in VAS (i.e. the difference between pre-injection and post-injection score; the greater the reduction in the score, the better the outcome) and the absolute value of the LBOS (the higher the score, the better the functional outcome). The employment status and occupation was categorised as light, medium or heavy according to the level of the physical activity. Multiple regression analysis was performed to determine the significance of the relationship between the predictors and the outcome measures.
All peri-radicular infiltration procedures were performed as a day case without pre-medication in an operating theatre. The patient was prone, and using two-planar image intensifier, a 22- to 25-G spinal needle was guided in the so-called safe triangle [26]. The triangle is defined by the pedicle superiorly, spinal nerve medially and vertebral body laterally. The S1 nerve root infiltration was performed through dorsal S1 foramen. Contrast material [Niopam 300 (iopamidol, 300 mg iodine/ml)] was injected to visualize the particular nerve root (Fig. 1A, B). Satisfactory visualization of nerve root was followed by slow injection of treatment agent, which contained a mixture of 2 ml 0.25% bupivicaine and 40 mg methylprednisolone (Depo-medrone).
Fig. 1.
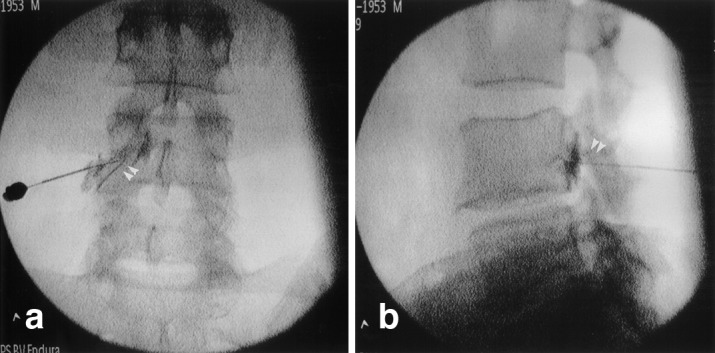
Example of a left L4/L5 peri-radicular infiltration on the anterior-posterior (A) and lateral (B) fluoroscopic projection, demonstrating contrast outlining the existing nerve root (double arrow)
Results
No statistical significant difference was found in the pre-injection level of disability between the LDH and spinal stenosis groups (Table 2). All the rootograms performed were considered to be satisfactory. We have not had any complication of this procedure. Table 3 demonstrates the outcome of peri-radicular infiltration at the 6- and 12-week follow-up. There was a statistically significant difference in the functional outcome between the two groups at 6 and 12 weeks of follow-up. The change in the VAS for two groups of patients was modest throughout follow-up with no statistical significant difference between them. Of patients in the LDH group, 58% had at least a 10% reduction in the ODI score compared to 37% in the spinal stenosis group at final follow-up. The clinical outcome at 3 months for the two groups of patients is shown in Table 4.
Table 2.
Pre-injection level of disability of two groups of patients (ODI Oswestry disability index, LBOS low back outcome score, VAS visual analogue scales)
| Pre-injection parameters (absolute value) | LDH (mean ± SE) | Spinal stenosis (mean ± SE) | Difference between group P value |
|---|---|---|---|
| ODI | 50±2.2 | 51±2.1 | 0.63* |
| LBOS | 25±1.5 | 22±1.5 | 0.17* |
| VAS (mm) | 74±2.4 | 77±1.8 | 0.34* |
*Not statistically significant
Table 3.
Outcome of peri-radicular infiltration at 6 weeks and 12 weeks of follow-up
| Outcome measures | LDH (mean ± SE) | Spinal stenosis (mean ± SE) | Difference between group P value |
|---|---|---|---|
| 6-week follow up | |||
| Change in ODI | 9±2 | 2±1.2 | 0.008* |
| LBOS | 29±2 | 25±1.2 | 0.05* |
| Change in VAS (mm) | 11±3.2 | 7±0.3 | 0.46 |
| 12-week follow up | |||
| Change in ODI | 13±1.8 | 6±1.8 | 0.005* |
| LBOS | 34±2.2 | 26±1.4 | 0.002* |
| Change in VAS (mm) | 20±3.6 | 12±2.5 | 0.07 |
*P value statistically significant
Table 4.
Clinical outcome at 3 months for two groups of patients. Values represent number of cases
| Outcome | LDH | Spinal stenosis |
|---|---|---|
| Discharged | 35 | 35 |
| Operative intervention | 16 | 10 |
| Further root block | 2 | 2 |
| Pain management | 2 | 6 |
| Salmon calcitonin injection | Not applicable | 9 |
There were 17 cases of disc protrusion, 23 cases of contained herniated disc and 15 cases of non-contained herniated disc in the LDH group. In the spinal stenosis group, we recruited 30 cases of radiculopathy secondary to foraminal stenosis and 14 cases secondary to far lateral compression. One-way analysis of variance did not shown a significant overall difference (P=0.09) in the change in ODI at 3 months when patients in the LDH group were sub-classified according to the disc morphology on the MRI. Unpaired t-test also showed no significant difference (P=0.6) in the outcome between foraminal stenosis subgroup and far lateral compression subgroup.
The results of the association between the outcome measures and predictors using simultaneous multiple regression analysis are shown in Table 5. There was a significant negative association between MZDS, MSPQ and age with post-injection LBOS at 3 months follow-up. The age at injection also had a negative predictive value for both the change in ODI score and change in VAS. We have found no predictive value for the duration of symptoms.
Table 5.
Association between predictors and (a) LBOS, (b) change in ODI and (c) change in VAS at 3 months follow-up
| Predictors | Coefficient b ± SE | t−test | P value |
|---|---|---|---|
| a) LBOS | |||
| Duration of sciatica | −6±0.1 | −1.4 | 0.18 |
| MSPQ | −0.6±0.2 | −2.4 | 0.02* |
| MZDS | −0.2±0.1 | −2.0 | 0.02* |
| Age | −0.3±0.1 | −5.0 | 0.00* |
| b) Change in ODI | |||
| Duration of sciatica | −8.0±0.1 | −1.4 | 0.16 |
| MSPQ | −0.3±0.3 | −1.0 | 0.33 |
| MZDS | −0.1±0.1 | −0.9 | 0.40 |
| Age | −0.3±0.1 | −3.6 | 0.00* |
| c) Change in VAS | |||
| Duration of sciatica | −1.7±0.01 | −1.7 | 0.08 |
| MSPQ | −4.5±0.1 | −1.0 | 0.33 |
| MZDS | −2.6±0.02 | −1.3 | 0.22 |
| Age | −2.5±0.01 | −2.0 | 0.05* |
*Statistically significant
The unpaired t-test shows no difference in the clinical outcome at 3 months between the male and female patients (P=0.99). One-way analysis of variance showed no significant overall difference in the clinical outcome between the groups of patients with different employment status (employed, unemployed and retired; P=0.34). Similarly, the level of physical activities (light, medium, heavy) has no influence on the functional results at 3 months (P=0.15).
Discussion
Macnab first introduced the term ‘selective nerve root infiltration’ in 1971 [16]. Since then, various different terminologies have been used in the literature, which include ‘selective lumbosacral block’ [29], ‘selective nerve root blocks’ [14, 26], ‘transforaminal epidural injections’ [15, 28] and ‘peri-radicular infiltration’ [11].
The objective of therapeutic peri-radicular infiltration is to provide temporary relief from peak pain during the time when there may be spontaneous resolution of radiculopathy. Weber et al. [32] have shown that 70% of patients with clinical evidence of radiculopathy resolve within 4 weeks. Karppinen et al. [11] have shown that a single peri-radicular injection only produces a short-term effect of no more than 4 weeks compared to a control group in a randomised controlled trial. However, there is evidence suggesting that multiple peri-radicular infiltration can prolong its effects. Lutz et al. [15] were able to achieve a success rate of 75% at an average of 80-month follow-up when multiple injections are combined with a functional restoration program that emphasized active exercise and education. Riew et al. [27] also found that by implementing multiple injection regimes, 52.7% of the patients can avoid the need for operative intervention for up to 13–28 months. The treatment agent used for this procedure varies between studies. Our study used a mixture of 2 ml 0.25% bupivicaine and 40 mg methylprednisolone, which is the same as the mixture used by Karppinen et al. [11] and Riew et al. [27]. The use of short-term acting injection of 1.5 ml 2% xylocaine with 9 mg betamethasone acetate by Lutz et al. [15] produced a successful outcome with a 50% reduction in VAS in 75% of the patients. We chose methylprednisolone for its predominant anti-inflammatory effect with little sodium-retaining activity. Lutz et al. [15] chose to use betamethasone that is longer acting than methylprednisolone. However, there is currently no study to suggest which is best in terms of the treatment outcome.
Most studies only investigate the efficacy of peri-radicular infiltration on radicular pain. Few authors have documented their experiences in spinal stenosis patients. Botwin et al. [3] reported that 75% of the patients involved had a successful outcome at 1 year. However, only 34 patients were involved in that study and the number of injections received per patient was not standardized. Riew et al. [27] also reported good functional outcome in a prospective trial that involves both LDH group and a stenotic group with a total of 55 patients. The interpretation of the results is difficult, as the proportion of patients in the stenotic group was not mentioned and the number of injections received by each patient was not standardised. They did not find any significant difference in the outcome between the two groups. It may be a type II error as the number of subjects involved is relatively small. Hasue and Kikuchi [12] concluded that cases of lumbar spinal stenosis due to spondylosis or degenerative spondylolisthesis have benefited more than those of disc herniation and spondylolytic spondylolisthesis. This was not our finding. Nevertheless, Lutz et al. [15] found that the patients with moderate to severe lateral recess stenosis respond less favourably and are more likely to require a surgical intervention.
The outcome measures for this study include LBOS, change in ODI and change in VAS for radicular pain only. Both the ODI and LBOS have been validated and their reliability and sensitivity to changes in functional status have been proven [5, 6, 8].
We found that the patients in the stenosis group had a moderate response compared to the LDH group (Table 3). Of patients in the spinal stenosis group, 37% had at least a 10% reduction in ODI. It is not clear at present if this is due to a treatment effect or the natural history of the pathology. A randomised controlled trial is required to determine its efficacy.
There are various possible explanation for the difference in the two groups. In spinal stenosis, chronic mechanical compression and indirect vascular insufficiency lead to nerve root ischaemia and demyelination [31]. In contrast, experimental studies of the effect of LDH on the nerve root have shown that, in addition to mechanical compression, chemical irritation from the immunogenic substance of disc material may have a significant role in radiculopathy [7, 20, 21, 22, 24]. Corticosteroids that have both anti-inflammatory [23] and local anaesthetic properties [9] may have much greater therapeutic value in LDH than in spinal stenosis. Riew et al. [27] found that the group treated with both corticosteroids and local anaesthetics achieved a statistically better outcome than the group treated with local anaesthetic alone.
Short-lived effects of a single injection may reflect the modest improvement in VAS, which is shown at 6 and 12 weeks for both groups of patients. Karppinen et al. [11] found no differences in the post-injection VAS between the group treated with local anaesthetic and steroids and that treated with placebo at 4 weeks of follow-up.
Lutz et al. [15] found that pre-injection sciatic symptoms of more than 24 weeks produce a less favourable outcome. We did not find duration of symptoms to be significant risk factor. The results are also not comparable since Lutz et al. [15] had no stenotic patients.
To date, no study has investigated the influence of psychological factors on the outcome of peri-radicular infiltration for radicular pain. Somatic anxiety and depression are recognised as risk factors for lumbar disc surgery [30]. MSPQ was derived by Main [17] specifically for use with outpatient chronic back pain. MZDS was modified by Main et al. [19] for the distress risk assessment methodology in outpatients with pain-related disability. Main and Waddell [18] found that the use of both MZDS and MSPQ were associated with pain-related disability rather than personality traits. We have found both MSPQ and MZDS to be negative predictors for post-injection LBOS. Age at injection has been associated with less favourable outcome as demonstrated in all the outcome measures.
Conclusion
This prospective cohort study demonstrates that the peri-radicular infiltration is a safe procedure that produces short-term benefit in a significant proportion of the patients with radiculopathy. LDH patients have a greater probability of a clinically significant response than stenotic patients. Further research with a randomised controlled trial and long-term follow up can further clarify the value of this procedure.
References
- 1.Bogduk Spine. 1995;20:845. doi: 10.1097/00007632-199504000-00021. [DOI] [PubMed] [Google Scholar]
- 2.Bogduk N, Brazenor G, Christophides N, Cherry D, Fraser R, Jenkins J, et al (1993) Epidural steroids in the management of low back pain and sciatica of spinal origin. Report of the working party. National Health and Medical Research Council, Sydney, pp 102–106
- 3.Botwin Am J Phys Med Rehabil. 2002;81:898. doi: 10.1097/00002060-200212000-00003. [DOI] [PubMed] [Google Scholar]
- 4.El-khouri Radiology. 1998;168:554. [Google Scholar]
- 5.Fairbank Physiotherapy. 1980;66:271. [PubMed] [Google Scholar]
- 6.Fisher Physiother Theory Practice. 1997;13:67. [Google Scholar]
- 7.Franson Spine. 1992;17:S129. doi: 10.1097/00007632-199206001-00011. [DOI] [PubMed] [Google Scholar]
- 8.Holt Spine. 2002;27:206. doi: 10.1097/00007632-200201150-00017. [DOI] [PubMed] [Google Scholar]
- 9.Johansson Acta Anaesthesiol Scand. 1990;34:335. doi: 10.1111/j.1399-6576.1990.tb03097.x. [DOI] [PubMed] [Google Scholar]
- 10.Johnsson Acta Orthop. 1993;Scand:67. [Google Scholar]
- 11.Karppinen Spine. 2001;26:1059. doi: 10.1097/00007632-200105010-00015. [DOI] [PubMed] [Google Scholar]
- 12.Kikuchi Spine. 1998;13:1327. doi: 10.1097/00007632-198811000-00020. [DOI] [PubMed] [Google Scholar]
- 13.Koes Pain. 1995;63:279. doi: 10.1016/0304-3959(95)00124-7. [DOI] [PubMed] [Google Scholar]
- 14.Krempen J Bone Joint Surg Am. 1974;56:1435. [PubMed] [Google Scholar]
- 15.Lutz Arch Phys Med Rehabil. 1998;79:1362. doi: 10.1016/s0003-9993(98)90228-3. [DOI] [PubMed] [Google Scholar]
- 16.Macnab J Bone Joint Surg Am. 1971;53:891. [PubMed] [Google Scholar]
- 17.Main J Psychosom Res. 1983;27:503. doi: 10.1016/0022-3999(83)90040-5. [DOI] [PubMed] [Google Scholar]
- 18.Main Clin Rehabil. 1987;1:139. [Google Scholar]
- 19.MainSpine 199217421531554 [Google Scholar]
- 20.McCarron Spine. 1987;12:760. doi: 10.1097/00007632-198710000-00009. [DOI] [PubMed] [Google Scholar]
- 21.Nygaard Spine. 1997;22:2484. doi: 10.1097/00007632-199711010-00004. [DOI] [PubMed] [Google Scholar]
- 22.Olmarker Orthop Clin North Am. 1991;22:223. [PubMed] [Google Scholar]
- 23.Olmarker Spine. 1994;19:1803. doi: 10.1097/00007632-199408150-00003. [DOI] [PubMed] [Google Scholar]
- 24.Olmarker Spine. 1995;20:665. doi: 10.1097/00007632-199503150-00006. [DOI] [PubMed] [Google Scholar]
- 25.Ozaki T, Kurihara A, Sha N, et al (1993) Clinical study of conservative and operative treatment in lumbar spinal stenosis. International society of the study of the lumbar spine, Marseille
- 26.Pfirrmann Radiology. 2001;221:704. doi: 10.1148/radiol.2213001635. [DOI] [PubMed] [Google Scholar]
- 27.Riew J Bone Joint Surg Am. 2000;82:1589. doi: 10.2106/00004623-200011000-00012. [DOI] [PubMed] [Google Scholar]
- 28.Shah Transforaminal epidural injections in lumbar. 2000;radiculopathy:prospective. [Google Scholar]
- 29.Tajima Spine. 1980;5:68. doi: 10.1097/00007632-198001000-00013. [DOI] [PubMed] [Google Scholar]
- 30.TiefSpine 200025261611034646 [Google Scholar]
- 31.Watanabe J Neurosurg. 1986;64:64. doi: 10.3171/jns.1986.64.1.0064. [DOI] [PubMed] [Google Scholar]
- 32.Weber Spine. 1993;18:1433. [PubMed] [Google Scholar]
- 33.Weiner J Bone Joint Surg Br. 1997;79:804. doi: 10.1302/0301-620X.79B5.7636. [DOI] [PubMed] [Google Scholar]


