Abstract
Background and purpose
The public knowledge of diabetes is important for prevention of disease. This study aimed to evaluate knowledge of diabetes, risk factors, and the common warning signs of diabetes and complications among community participants in a rural Karen ethnic community.
Methods
Participants were asked to answer a questionnaire regarding their knowledge of diabetes. Fasting blood glucose testing, blood pressure measurement, and body mass index (BMI) assessment were provided to the participants. The study was conducted at Thasongyang district, Tak province, Thailand.
Results
A total of 299 Karen rural residents were included in the study. The median age was 45 years and median fasting blood glucose was 88 mg/dL. The response rate to the questionnaires was 91.97%. Half of the participants knew diabetes is a noncommunicable disease needing lifelong treatment. Overall, one-third of the community participants could correctly answer the knowledge assessment questions regarding risk factors and common features of diabetes. whereas the other two-thirds either gave a wrong answer or were “not sure”. Female participants had poorer diabetes knowledge than the males.
Conclusion
The public knowledge of diabetes, as represented by this sample of the Karen ethic community, is alarmingly low. There is significant gender difference in knowledge level. Culturally tailored and gender-sensitive diabetes health education interventions are urgently needed in this minority ethnic community.
Keywords: health education, gender differences, ethnic minority, diabetes, Karen
Background
Diabetes is a globally burdensome noncommunicable disease. Diabetes can cause acute and long-term complications, and is as well, a global risk factor for cardiovascular disease.1 Lifestyle and behavior, as well as individual genetic predisposition, influence the risk of diabetes and prevalence in a community.2 Public knowledge is the basis for lifestyle and behavior in a given community.3 Therefore, the knowledge particular to diabetes is a key determinant of the lifestyle of a community, and can discriminate those who are at risk from those who are free of risk.
Diabetes is increasingly prevalent in ethnic minority groups globally.2,4,5 Recently, Lorga et al6 reported that 16.7% of the Karen rural community had an abnormally high blood glucose level (>100 mg/dL), and that there was a considerable proportion of prediabetic persons (13.04% ) in a cross-sectional survey among the Karen minority. The Karen ethnic rural community along the Thai–Myanmar border is a hard-to-reach population for health promotion services. Karen people use their native language and most of the senior adult population in the community cannot read Thai script. This forms a barrier to health education provided by the national health program. Moreover, in a district like Thasongyang, the population pattern is very dynamic and unstable because of a large migration across the border.7 Karen people are indigenous to, and tend to stay along the Thai-Myanmar border such as area around Tak province. There is limited literature to guide the assessment of health literacy and knowledge of diabetes in such a community.8
The objective of the study was to assess the knowledge of diabetes of the rural Karen residents, and compare the diabetes knowledge between male and female respondents.
Participants, setting, materials, and method
This analysis and article is the third publication generated from our study. The study design was cross-sectional survey. It was conducted from June 2011 to September 2011. The analysis was carried out in April 2012.
This study was approved by the ethical board of the Boromrajonani College of Nursing Nakhon Lampang, Lampang, Thailand, and conducted with the verbal informed consent of participants. It was conducted in Thasongyang, which is a district in the far northwest of Thailand, by the narrow Moei river on the border of Myanmar. The participants were rural residents living in clusters of houses on the hilltops. A total of 299 Karen adults participated in the survey conducted by convenience sampling. All participants were Thai citizens but most of the participants could not read Thai script. None had any prior known diagnosis of diabetes.
Questionnaires
Diabetes knowledge was assessed by a questionnaire that was developed by consensus between native researchers and researchers from the Boromrajonani College of Nursing Nakhon Lampang. The questionnaires were delivered in the Karen language by researchers speaking both Thai and the Karen language, and were completed by the interviewers.
Fasting plasma glucose
Fasting plasma glucose (FPG) measurement was preceded by overnight fasting for 8 hours before the test. FPG level was checked using venous blood samples of the participants. Those who forgot overnight fasting were excluded for examination of FPG. FPG examination was carried out at Thasongyang hospital laboratory.
Body mass index
Body weight and height were measured by the public health officers using a standard measuring scale. Body mass index was calculated by the ratio of body weight in kilograms divided by the square of the height in meters.
Blood pressure
Systolic and diastolic blood pressures were noted after two measurements taken 15 minutes apart. Blood pressure was measured by the community nurses with a sphygmomanometer.
Statistical analysis
Continuous variables were summarized as median, maximum, and minimum values, as the distribution was not normal. The nonparametric test for trend analysis was run by “nptrend” in Stata version 11 (Stata Corp, College Station, TX). “Yes,” “no,” and “not sure” answers in the questionnaires were recoded as categories in order to compare by rank sum test. A correct answer was coded to be 1, and an incorrect answer, or the answer of “not sure,” was coded as zero. Stata version 11 was used for data management and data analysis. Statistical significance was defined as P value less than 0.05, with a 95% confidence interval.
Results
The study had a 99.67%–100% response rate for measurement of the base line parameters. Forty-one percent of respondents were male patients. The average age of the sample was 45 years. Average values of the measured parameters are shown in Table 1.
Table 1.
Characteristics and response rate of the participants in the survey
| Parameter | N (%) surveyed | Median (min-max) |
|---|---|---|
| Age (years) | 299 (100%) | 45 (23–82) |
| Fasting blood glucose (mg/dL) | 299 (100%) | 88 (54–371) |
| Systolic blood pressure (mmHg) | 298 (99.67%) | 110 (70–220) |
| Diastolic blood pressure (mmHg) | 298 (99.67%) | 70 (50–111) |
| Body mass index | 299 (100%) | 20.44 (18.71–22.96) |
Response to questionnaires
The overall response rate was 91.97% for all the questions. We assessed the diabetes knowledge briefly in three parts (1) general knowledge, (2) knowledge about the risk factors, and (3) knowledge about the symptoms, diagnostic signs, and complications of diabetes mellitus.
General knowledge of diabetes was assessed by two questions. Half of the participants did not know diabetes was a noncommunicable disease. Half of respondents answered that diabetes was a curable disease (Table 2).
Table 2.
Diabetes health literacy survey questionnaire results
| Diabetes-related survey questions | Correct % | Wrong % | “Not sure” % |
|---|---|---|---|
| General knowledge | |||
| Diabetes is a communicable disease | 51.84 | 25.42 | 14.72 |
| Diabetes is curable | 29.77 | 49.50 | 12.71 |
| Knowledge of risk factors | |||
| Older age is a risk for diabetes | 36.45 | 22.07 | 33.44 |
| Having a diabetic relative is a risk for diabetes | 37.12 | 18.39 | 36.12 |
| Overweight people tend to have diabetes | 39.80 | 17.06 | 35.12 |
| Overweight children are at risk of diabetes | 34.45 | 21.74 | 35.45 |
| Exercises regularly have less risk of diabetes | 37.12 | 21.07 | 33.78 |
| Pregnant women are at risk of diabetes | 27.09 | 25.08 | 39.80 |
| People who eat fatty food are at risk of diabetes | 41.81 | 16.05 | 34.11 |
| Knowledge of the disease and its complications | |||
| Normal FBS after fasting should not exceed 100 mg/dL | 29.43 | 30.10 | 32.44 |
| Diabetes people usually have thirst and polyuria | 33.78 | 25.75 | 32.11 |
| Numbness of hands and feet is a symptom of diabetes | 34.78 | 21.74 | 35.12 |
| Diabetic people have to take care of feet well | 35.12 | 20.74 | 36.12 |
| Untreated diabetes can lead to blindness | 32.78 | 23.41 | 35.79 |
| Wounds in diabetic patients are slow to heal | 34.78 | 20.40 | 36.12 |
Notes: N = 299, Response rate 91.97% (275). Response percentages were calculated using the denominator of 295.
Abbreviation: FBS, fasting blood sugar.
The knowledge of risk factors for diabetes was assessed by seven questions. One-third of the population answered correctly (range 27.09%–41.81%), and another one-third gave no answer to these questions (range 33.44%–39.80%), whereas another one–third gave a wrong answer. Among the Karen community, 36.45% knew that old age is a risk factor for diabetes, 37.12% knew that they had diabetic relatives, 39.80% knew that obesity can lead to diabetes, 37.12% answered that exercise can prevent diabetes, 25.09% reported that pregnant women can have diabetes, and 41.81% said they should not eat excess fatty food for fear of diabetes.
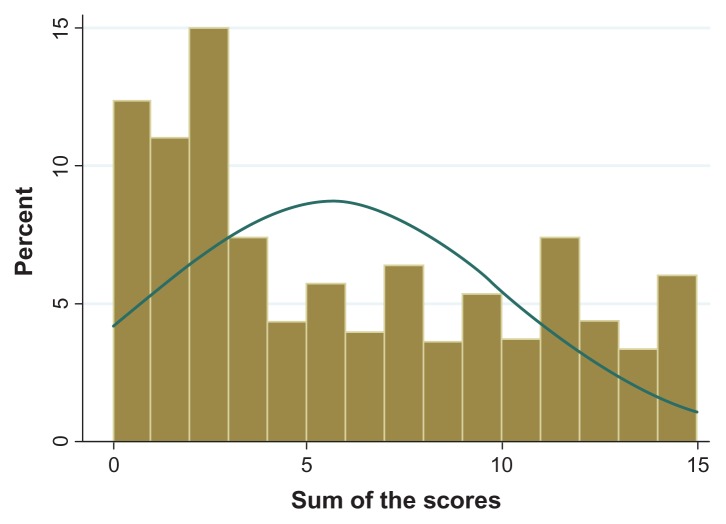
Regarding the symptoms, diagnosis and complications of diabetes, less than 30% knew that fasting blood glucose level should be less than 100 mg%. A few of the rural Karen ethnic residents could correctly answer questions in the third part of the questionnaire. Among the respondents, 33.78% answered that diabetic patients could have thirst and polyuria, 34.78% knew that numbness of the limbs might link to diabetes, 35.12% recognized the importance of foot care in people living with diabetes, 32.78% answered that untreated diabetes could lead to blindness, and 34.78% knew that slow wound healing might be due to diabetes. Overall, one-third of the sample population gave the correct answers (range 32.78%–34.78%) while the other two-thirds were either unsure or gave wrong answers. Overall, public knowledge of diabetes among Karen ethnic rural community is at the lower extreme ( Figure 1).
Figure 1.
Distribution of diabetes knowledge among the Karen ethnic rural community.
Notes: Overall knowledge level was sorted to be a sum of scoring in the histogram, to show the distribution of knowledge. The kurtosis was significant (P < 0.001) and the distribution was totally skewed to the left (P < 0.001). The histogram shows the sum of scoring had a peak around zero to three. The peak score around zero indicated that there were a large proportion of participants who could not correctly answer the questions.
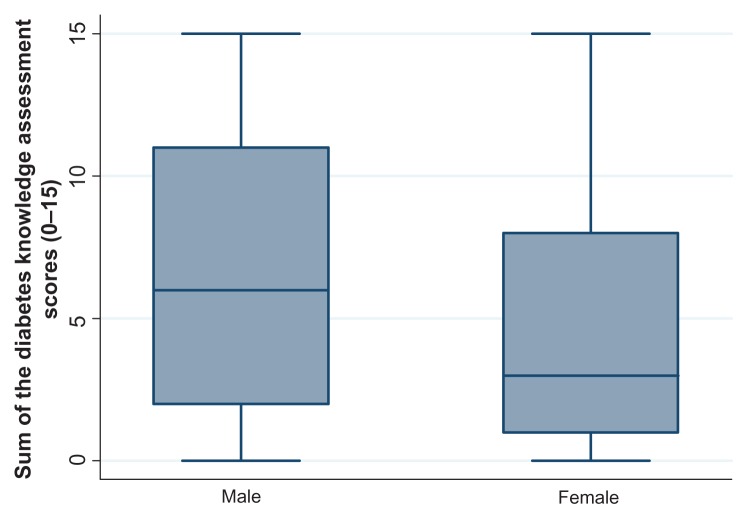
Knowledge level in males and females
Diabetes knowledge was compared between male and female by median sum of the knowledge scores. Female participants had poorer knowledge than male participants. Overall knowledge level in female participants was also lower than in male participants (Figure 2). The median sum of the knowledge scores was 6 (interquartile range: 2–11) among males, and 3 (interquartile range: 1–8) among the females (P for trend = 0.009). There was a significant difference in level of knowledge among females and males.
Figure 2.
Distribution of diabetes knowledge in male and female participants in the survey.
Discussion
The number of diabetes cases is rising worldwide, and the burden of this is more severe in low- and middle-income countries.9,10 “Belonging to an ethnic minority” has been reported as a risk factor for the development of type 2 diabetes.2 Disadvantaged people in these groups are more prone to the consequences of a silent epidemic.11 It is important to assess the public knowledge of diabetes, especially in minority ethnic populations. Today, rising public health education and reduced disparity between groups are compulsory for the prevention and care of diabetes in all settings.12
Risk perception of a community is the basis for healthy behavioral changes within a community.13 Perception of risk among people at risk can prevent the disease. This may lead to early lifestyle modification and the prevention of many diabetes cases. Thus, we assessed the perception of diabetes risk factors among the Karen ethnic rural community. We found only one-third of the study sample had knowledge about diabetes risk factors (Table 2). Most in the Karen community did not know that elderly age, being overweight, and physical inactivity are risk factors for diabetes. This may be the consequence of poor risk communication to the Karen ethnic community. Initiation of measures to educate this minority population, including use of mass media, and printed materials in the local language, might be a useful strategy for risk communication.
We assessed the public knowledge about symptoms of diabetes and blood glucose test results. Knowledge of diabetes symptoms is important for early diagnosis and accessing care. Recognizing the symptoms of diabetes and its complications may bring the diabetic individuals to seek health care service. Abnormal blood glucose level is also an easily noticeable marker for persons at risk. Symptoms of diabetes complications are common presentations, even though these might be indicators of late diagnosis, or poor glycemic control. Individuals lacking knowledge of these may not seek medical care in time, and consequently will have complications of diabetes.14 We assessed such knowledge in Karen ethnic community (Table 2). We found that overall, less than 40% of people had this knowledge.
The histogram of knowledge scoring was skewed to the left and peaked at lower end of the scoring (Figure 1). In contrast, the similar histogram for public knowledge of diabetes in Singapore, was reported as totally skewed to the right side.15 The knowledge distribution among the Karen ethnic sample was at the lower end, and pointed out a need for intervention.
We identified an inequality of diabetes knowledge between men and women. In fact, diabetes and its consequent cardiovascular disease risk are higher in women.7 There is also increasing concern about gestational diabetes;16 however, our observations pointed out that diabetes knowledge among female Karen participants was lower than among males. This type of health inequality has also been reported in many other diseases.17 Type 2 diabetes is more common in disadvantaged groups of women, such as those with least income and who are least educated.18 Risk behaviors for type 2 diabetes have been highly prevalent even in the developed setting;19 moreover, poor women in the developing world tend to delay seeking care until symptoms are too severe.17 In the particular setting of this study, it is likely that women usually work in the home at housekeeping, and become housebound and sedentary. A television education program in the local language might reach these women.19 Lack of diabetes knowledge can cause missed diagnosis, late diagnosis, and higher incidence of diabetes complications. Creation of a peer-group gathering place for women, such as a health education club for mothers, and exercise club for housewives, may promote women’s knowledge of diabetes and sharing of information.
In contrast to the current study findings, in a previous study, the public knowledge among Thai people was reported to be fairly high and there was no gender gap between Thai men and women.20 It is obvious that diabetes health education is poor among the Karen ethnic community. This might be due to a language barrier, which is a major obstacle to educating minority groups, as in other parts of Asia.21 Existing evidence suggests that such a situation calls for a culturally tailored and well-designed health education strategy.22
Limitations of the study
As this was a pilot study swiftly conducted to provide important information, there were weaknesses in the current study. We did not get a 100% response rate. The questionnaire used in this study was made easily comprehensible for rural Karen residents, and study findings may not be generalizable to other settings. Albeit, the findings are the first of their kind to our knowledge, and are meant to assist in guiding further studies.
Conclusion
Despite these limitations, this investigation contributed to our understanding of the health disparity in an ethnic minority population. It provided insights into the need for health education interventions for the prevention of diabetes in a rural ethnic community. The result of this study showed that Karen ethnic men and women were less knowledgeable about all aspects of diabetes. Public education about diabetes in this setting should be started urgently and carefully, to overcome language and cultural barriers and prevent diabetes epidemic among these rural people. Our study finding is expected to be a step forward, in minimizing the disparity in diabetes health education.
Acknowledgment
The staff of Baan Rekati Health Station, Thasongyang and Thasongyang Hospital, Tak, Thailand are heartily acknowledged for their support. Richard Lawrence Mann is acknowledged for refining the English language in this paper. Payom Thinuan, Suwattana Kumsuk, Sireewat Ar-yuwat and Prissana Naunboonruang are acknowledged for discussions with the author.
Footnotes
Author contributions
TL and MNA were lead authors. The manuscript was drafted and finalized by MNA, read and confirmed by all the authors.
Disclosure
The authors have no conflicts of interest to declare.
References
- 1.WHO. Diabetes Programme [web page on theinternet] [Accessed August 14, 2012.]. Updated 2012. Available from: http://www.who.int/diabetes/en/
- 2.Egede LE, Dagogo-Jack S. Epidemiology of type 2 diabetes: focus on ethnic minorities. Med Clin North Am. 2005;89(5):949–975. doi: 10.1016/j.mcna.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 3.Matthaei S, Munro N, Zinman B for Global Partnership for Effective Diabetes Management. Raising diabetes awareness in the public domain. Int J Clin Pract Suppl. 2007;61(Suppl 157):S31–S37. doi: 10.1111/j.1742-1241.2007.01611.x. [DOI] [PubMed] [Google Scholar]
- 4.Jovanovic L, Harrison RW., 3rd Advances in diabetes for the millennium: diabetes in minorities. MedGenMed. 2004;6(Suppl 3):2. [PMC free article] [PubMed] [Google Scholar]
- 5.Oldroyd J, Banerjee M, Heald A, Cruickshank K. Diabetes and ethnic minorities. Postgrad Med J. 2005;81(958):486–490. doi: 10.1136/pgmj.2004.029124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lorga T, Aung MN, Naunboonruang P, et al. Predicting prediabetes in a rural community: a survey among the Karen ethnic community, Thasongyang, Thailand. Int J Gen Med. 2012;5:219–225. doi: 10.2147/IJGM.S27876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.United Nations High Commissioner for Refugees. UNHCR country operations profile – Thailand [Web page on the Internet] 2012. [Accessed August 14, 2012.]. Updated 2012. Available from: http://www.unhcr.org/pages/49e489646.html.
- 8.Naqshbandi M, Harris SB, Esler JG, Antwi-Nsiah F. Global complication rates of type 2 diabetes in Indigenous peoples: A comprehensive review. Diabetes Res Clin Pract. 2008;82(1):1–17. doi: 10.1016/j.diabres.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 9.Danaei G, Finucane MM, Lu Y, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2·7 million participants. Lancet. 2011;378(9785):31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 10.World Diabetes Foundation. Diabetes facts [Web page on the Internet] [Accessed August 14, 2012.]. Updated 2011. Available from: http://www.worlddiabetesfoundation.org/composite-35.htm.
- 11.WHO. Global atlas on cardiovascular disease prevention and control [Web page on the Internet] [Accessed August 14, 2012.]. Updated 2012. Available from: http://www.who.int/cardiovascular_diseases/publications/atlas_cvd/en/
- 12.WHO. Diabetes action online: a web based resource for diabetes health care planning [Web page on the Internet] [Accessed August 14, 2012.]. Updated 2012. Available from: http://www.who.int/diabetes/action_online/dao_brochure.pdf.
- 13.Gianinazzi F, Bodenmann P, Izzo F, Voeffray Favre AC, Rossi I, Ruiz J. Risk perception and communication: from diabetes to cardiovascular diseases. Rev Med Suisse. 2010;6(252):1182–1184. 1186–1187. French. [PubMed] [Google Scholar]
- 14.Jackson DMA, Wills R, Davies J, Meadows K, Singh BM, Wise PH. Public awareness of the symptoms of diabetes mellitus. Diabet Med. 1991;8(10):971–972. doi: 10.1111/j.1464-5491.1991.tb01540.x. [DOI] [PubMed] [Google Scholar]
- 15.Wee HL, Ho HK, Li SC. Public awareness of diabetes mellitus in Singapore. Singapore Med J. 2002;43(3):128–134. [PubMed] [Google Scholar]
- 16.Ferrara A. Increasing prevalence of gestational diabetes mellitus: a public health perspective. Diabetes Care. 2007;30(Suppl 2):S141–S146. doi: 10.2337/dc07-s206. [DOI] [PubMed] [Google Scholar]
- 17.Vlassoff C. Gender differences in determinants and consequences of health and illness. J Health Popul Nutr. 2007;25(1):47–61. [PMC free article] [PubMed] [Google Scholar]
- 18.Dasgupta K, Khan S, Ross NA. Type 2 diabetes in Canada: concentration of risk among most disadvantaged men but inverse social gradient across groups in women. Diabet Med. 2010;27(5):522–531. doi: 10.1111/j.1464-5491.2010.02982.x. [DOI] [PubMed] [Google Scholar]
- 19.Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA. 2003;289(14):1785–1791. doi: 10.1001/jama.289.14.1785. [DOI] [PubMed] [Google Scholar]
- 20.Pongmesa T, Li SC, Wee HL. A survey of knowledge on diabetes in the central region of Thailand. Value Health. 2009;12(Suppl 3):S110–S113. doi: 10.1111/j.1524-4733.2009.00641.x. [DOI] [PubMed] [Google Scholar]
- 21.Wilson E, Wardle EV, Chandel P, Walford S. Diabetes education: an Asian perspective. Diabet Med. 1993;10(2):177–180. doi: 10.1111/j.1464-5491.1993.tb00038.x. [DOI] [PubMed] [Google Scholar]
- 22.Hawthorne K, Robles Y, Cannings-John R, Edwards AG. Culturally appropriate health education for Type 2 diabetes in ethnic minority groups: a systematic and narrative review of randomized controlled trials. Diabet Med. 2010;27(6):613–623. doi: 10.1111/j.1464-5491.2010.02954.x. [DOI] [PubMed] [Google Scholar]