Abstract
The purpose of the study was to investigate possible variation of thickness of the cervical spine endplate with respect to endplate orientation (superior or inferior endplate) and level distribution (C4–C7). Six human cervical spine segments C4–C7 were used to create six specimen of C4, C5, C6, and C7, respectively. The bony endplates of each vertebra were cleaned carefully from disc tissue without damaging the endplates. Six endplates with severe degenerative changes were excluded from the study. The posterior elements were removed, and a midaxial cut using a bone saw was performed through each vertebral body, thus producing a superior and inferior half. Each half-vertebra was then glued onto a piece of wood with the endplate oriented upwards and horizontally. For each specimen, four computed tomography scans were taken and thickness of the endplate was measured at five points on each scan perpendicular to the midaxial cut. Factorial analysis of variance (ANOVA) and Scheffe-test were used to detect significant differences. All peripheral regions were significantly thicker than the central point of the endplate if all measuring points were considered for statistical analysis, regardless of scan, endplate orientation or level (Scheffe-test, P<0.001). In both superior and inferior endplates, peripheral areas were thicker than the central region (Scheffe-test, P<0.001). For all levels, the endplate within the peripheral regions was thicker than within the central region and the difference reached significance for the superior and inferior endplate of C4, C5, and C6 and the inferior endplate of C7 (Scheffe-test, P<0.05). The peripheral regions of the cervical spine endplate are usually thicker than its central region, regardless of endplate orientation and level (C4, C5, C6, C7) distribution.
Keywords: Anatomy, Cervical spine, Endplate, Computed tomography
Introduction
Anterior cervical fusion has become an accepted technique in cervical spine surgery for cervical disc disease, radiculopathy and spondylotic myelopathy [1, 2, 3, 4, 5, 16, 19]. The classic procedure involves incision of the anterior longitudinal ligament, removal of the disc, and insertion of an autologous bone graft. Harvesting of the bone graft from the iliac crest, however, has been shown to have a high complication rate [6, 9, 10, 18]. To replace the graft, cages have recently been introduced into cervical spine surgery [14, 20]. Cages are usually inserted in segmental distraction and held in place by a rough surface, spikes or a cutting edge, which perforate the vertebral endplate. To adapt the geometry of the disc space to the shape of the cage, the disc space has to be modified using burrs, thus resulting in an partial or even complete removal of the endplates.
Mechanical behaviour of the cervical spine endplates has been recently investigated. It has been found that its resection significantly reduces load to failure in compression loading [11]. Also, there is evidence, that cervical spine fusion cages tend to collapse into the vertebral body if removal of the endplate is required [21]. Therefore, it seems to be recommendable to respect the integrity of the endplate wherever possible. However, not many data are available on the anatomy of the cervical spine endplate. Panjabi et al. [13] described the detailed anatomy of the endplate around its midsagittal plane, but, to our knowledge, comparable data for the peripheral regions of the endplate have not been published.
The purpose of the study was to describe the variations of thickness of the cervical endplate using computed tomography (CT). In particular, the following questions were investigated:
Are there regional variations in the thickness of the endplates of the cervical spine?
If yes, is it true for both superior and inferior endplates?
If yes, is it true for all cervical levels?
Material and methods
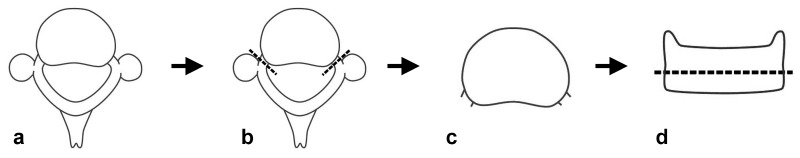
Six human cervical spine segments C4–C7 (mean age 62.7 years, standard deviation 7.5 years) were explanted during routine autopsies from fresh human cadavers, wrapped in double plastic bags, and stored at−20°C. For dissection, they were thawed and the soft tissue was removed from the bony structures. Each vertebra was isolated by discotomy and transection of the posterior ligaments, thus creating six specimens of C4, C5, C6, and C7, respectively (Fig. 1a). The bony endplates of each vertebra were cleaned carefully from disc tissue without damaging the endplates. The posterior bony structures were removed by transsecting the pedicles (Fig. 1b) to create an isolated vertebral body (Fig. 1c). An axial cut using a bone saw was performed through the midsection of each vertebral body, producing a superior and inferior half (Fig. 1d). Each specimen was then glued onto a piece of wood with the endplate oriented upwards and horizontally. Specimens with severe degenerative changes (defined as severe endplate sclerosis and/or osteophytes) were excluded from the study.
Fig. 1 a–d.
Schematic line drawing of a cervical vertebra, view from above onto the superior endplate (a). The posterior elements were cut at the dotted lines (b), producing an isolated cervical vertebral body (c). The vertebral body was then cut into two specimens by an midaxial cut, producing a specimen including the superior and inferior endplate, respectively (d)
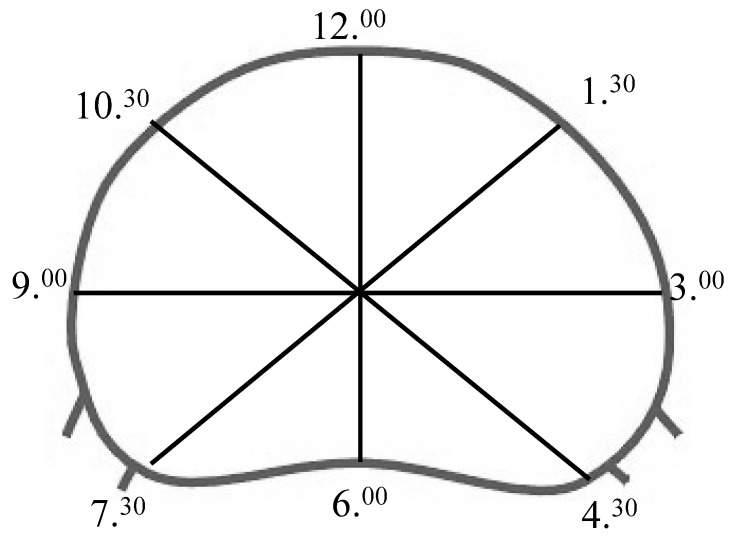
For each of the half vertebral bodies, four high resolution CT scans (Twin–Flash, Elscint Ltd., Haifa, Israel) were taken and named clockwise: the first scan was done in the mid-sagittal plane (6.00–12.00), the second one in the mid-coronal plane (9.00–3.00) and two further scans were taken in an angle of 45° to both the first and second scan (7.30–1.30 and 10.30–4.30), respectively (Fig. 2). Scan parameters were as follows: field of view 180 mm, matrix 512×512, slice thickness 1 mm. Window settings for measurements were as follows: width 2,000 Hounsfield units (HU), centre 500 HU. Digitised data were transferred to a computer and CT scans were enlarged by factor 5. The length of each scan through the vertebral body was set to be 100%. The midpoint of each scan was called “0%”, and the most peripheral points “−50%” and “+50%”. Correspondingly, four additional points were defined at −40%, -20%, 20%, and 40%. Thickness of the endplate was measured at five points of each scan (at −40%, −20%, 0%, 20% and 40%) perpendicular to the midaxial cut (Fig. 3) using the software Medisurf (Algotec Systems Ltd., Raanana, Israel). In the following the points at −40%, −20%, 20%, and 40% are called “peripheral regions” and the point at 0% is called “centre”.
Fig. 2.
Schematic line drawing of a specimen including the superior endplate, view from above onto the superior endplate. Note the lines indicating how the specimens were scanned by computed tomography. The 6.00–12.00 line was defined to be the midsagittal line, the 9.00–3.00 line was defined to be perpendicular to the midsagittal line through the widest portion of the endplate, the 7.30–1.30 and 11.30–4.30 lines were defined to be in an 45° angle to the above mentioned lines
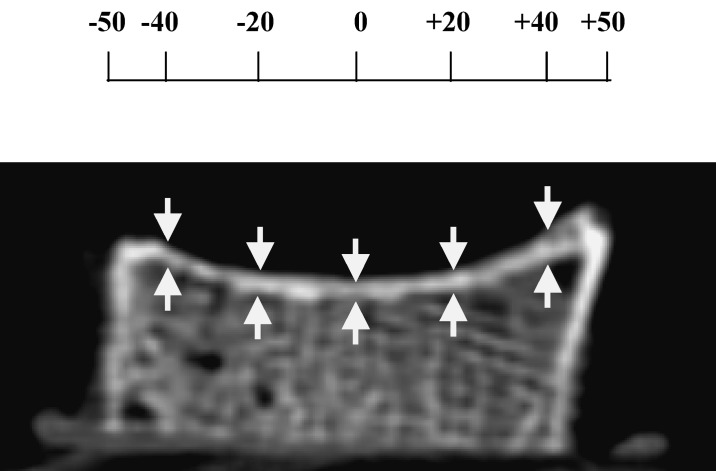
Fig. 3.
Computed tomography scan (6.00–12.00) of a specimen including the inferior endplate. Measurements of the thickness of the endplate were performed at five points: in the centre (0%) and at four points lateral to the centre, called “−40, −20, 20, 40”, indicated by white arrows
Mean value and standard deviation of the thickness of the endplate were calculated for each measuring point (−40%, −20%, 0%, 20%, 40%) with respect to endplate orientation (superior or inferior), vertebral level (C4, C5, C6, C7) and orientation of scan (6.00–12.00, 9.00–3.00, 7.30–1.30, 10.30–4.30). Factorial (with specimen, level, endplate orientation, direction of the scan, measuring points used as factors) analysis of variance (ANOVA) was used to detect significant differences. If significant differences were detected, Scheffe-test was used to detect statistically significant differences within each variable. Statistical significance was assumed for P<0.05. The statistical software package SPSS for Windows, Release 10.0.7, SPSS Incorporation was used for statistical analysis.
Results
Due to severe degenerative changes, two superior and four inferior endplates were excluded from data analysis.
Regional variations of thickness of the cervical spine endplate
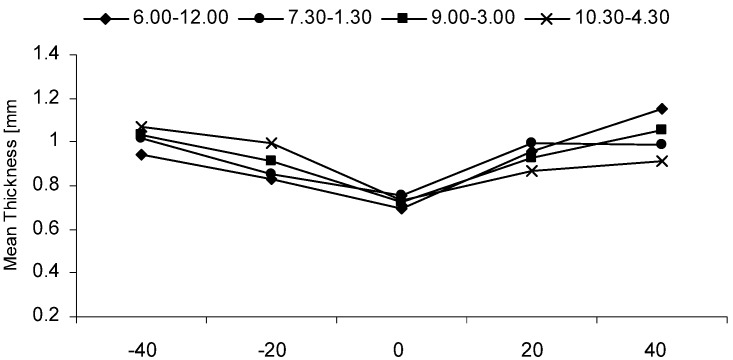
All peripheral regions were significantly thicker (0.72–1.35 mm) than the central point of the endplate (0.65–0.84 mm) if all measuring points were considered for statistical analysis, regardless of endplate orientation or level (Scheffe-test, P<0.001), (Fig. 4). This was also true if the measuring points of the oblique cuts were put together due to symmetry of the vertebral body along its sagittal plane. This variation did not depend on scan orientation ( ANOVA, P=0.9). Mean values and standard deviations for all specimens and all scans are provided in Table 1 for superior endplates and in Table 2 for inferior endplates.
Fig. 4.
Graph, giving the mean overall endplate thickness (mm) for the different regions according to the different scans at the points −40, −20, 20, 40 as defined above. For reasons of clarity, standard deviations are not shown
Table 1.
Mean thickness (standard deviation) of superior endplates. Values are given in millimeters for C4, C5, C6, and C7 specimens, respectively. Measurements were performed at five different locations of the endplate (named −40, −20, 0, 20, 40) of the scans (named 6.00–12.00, 7.30–1.30, 9.00–3.00, 10.30–4.30)
| C4 | C5 | C6 | C7 | ||
|---|---|---|---|---|---|
| 6.00–12.00 | −40 | 0.93 (0.36) | 0.90 (0.31) | 0.92 (0.40) | 0.72 (0.13) |
| −20 | 0.77 (0.36) | 0.85 (0.23) | 0.86 (0.23) | 0.78 (0.18) | |
| 0 | 0.65 (0.24) | 0.73 (0.14) | 0.70 (0.12) | 0.78 (0.07) | |
| 20 | 1.07 (0.28) | 0.98 (0.17) | 0.90 (0.29) | 0.98 (0.17) | |
| 40 | 1.20 (0.29) | 1.17 (0.33) | 1.16 (0.46) | 1.26 (0.21) | |
| 7.30–13.30 | −40 | 1.10 (0.17) | 1.08 (0.50) | 1.04 (0.49) | 0.82 (0.19) |
| −20 | 0.95 (0.14) | 0.78 (0.22) | 1.00 (0.19) | 0.82 (0.07) | |
| 0 | 0.83 (0.21) | 0.77 (0.26) | 0.74 (0.11) | 0.84 (0.08) | |
| 20 | 1.25 (0.22) | 1.02 (0.24) | 1.10 (0.29) | 1.00 (0.11) | |
| 40 | 0.97 (0.22) | 1.10 (0.14) | 1.20 (0.44) | 1.10 (0.18) | |
| 9.00–3.00 | −40 | 1.28 (0.22) | 1.22 (0.35) | 1.12 (0.24) | 1.08 (0.19) |
| −20 | 1.07 (0.23) | 0.90 (0.14) | 0.92 (0.15) | 0.94 (0.08) | |
| 0 | 0.77 (0.18) | 0.70 (0.17) | 0.68 (0.15) | 0.68 (0.13) | |
| 20 | 1.04 (0.13) | 0.98 (0.19) | 0.90 (0.16) | 0.82 (0.20) | |
| 40 | 1.35 (0.14) | 1.23 (0.34) | 1.14 (0.18) | 1.04 (0.15) | |
| 10.30–4.30 | −40 | 1.20 (0.37) | 1.08 (0.27) | 1.18 (0.40) | 1.04 (0.22) |
| −20 | 1.22 (0.28) | 1.12 (0.17) | 1.00 (0.20) | 1.08 (0.13) | |
| 0 | 0.82 (0.15) | 0.70 (0.06) | 0.72 (0.13) | 0.76 (0.08) | |
| 20 | 0.95 (0.23) | 0.88 (0.29) | 0.80 (0.12) | 0.86 (0.10) | |
| 40 | 0.98 (0.20) | 0.87 (0.32) | 0.78 (0.23) | 0.76 (0.10) |
Table 2.
Mean thickness (standard deviation) of inferior endplates (see Table 1)
| C4 | C5 | C6 | C7 | ||
|---|---|---|---|---|---|
| 6.00–12.00 | −40 | 1.12 (0.28) | 0.98 (0.15) | 0.90 (0.21) | 1.10 (0.29) |
| −20 | 0.88 (0.20) | 0.80 (0.21) | 0.82 (0.17) | 0.90 (0.22) | |
| 0 | 0.63 (0.08) | 0.70 (0.10) | 0.60 (0.06) | 0.80 (0.16) | |
| 20 | 0.87 (0.16) | 0.86 (0.15) | 0.86 (0.10) | 1.18 (0.17) | |
| 40 | 1.10 (0.24) | 1.22 (0.19) | 0.86 (0.22) | 1.30 (0.29) | |
| 7.30–13.30 | −40 | 1.07 (0.29) | 0.86 (0.09) | 0.96 (0.10) | 1.20 (0.48) |
| −20 | 0.85 (0.10) | 0.76 (0.18) | 0.74 (0.08) | 0.90 (0.14) | |
| 0 | 0.68 (0.08) | 0.76 (0.21) | 0.60 (0.14) | 0.85 (0.06) | |
| 20 | 0.88 (0.18) | 0.80 (0.14) | 0.86 (0.14) | 1.00 (0.12) | |
| 40 | 0.85 (0.05) | 0.90 (0.12) | 0.78 (0.16) | 1.05 (0.17) | |
| 9.00–3.00 | −40 | 0.92 (0.15) | 0.84 (0.15) | 0.78 (0.07) | 0.93 (0.21) |
| −20 | 0.97 (0.10) | 0.80 (0.16) | 0.76 (0.08) | 0.93 (0.05) | |
| 0 | 0.77 (0.14) | 0.68 (0.16) | 0.68 (0.15) | 0.83 (0.10) | |
| 20 | 1.02 (0.08) | 0.86 (0.35) | 0.80 (0.11) | 1.00 (0.18) | |
| 40 | 1.05 (0.28) | 0.84 (0.19) | 0.78 (0.04) | 0.88 (0.13) | |
| 10.30–4.30 | −40 | 1.13 (0.23) | 0.94 (0.05) | 0.8 (0.06) | 1.15 (0.24) |
| −20 | 0.97 (0.12) | 0.80 (0.22) | 0.72 (0.15) | 1.00 (0.22) | |
| 0 | 0.67 (0.08) | 0.74 (0.11) | 0.68 (0.13) | 0.83 (0.10) | |
| 20 | 0.88 (0.15) | 0.86 (0.09) | 0.78 (0.15) | 0.93 (0.13) | |
| 40 | 1.02 (0.29) | 0.96 (0.19) | 0.84 (0.19) | 1.08 (0.22) |
Variations of thickness of the cervical spine endplate with respect to endplate orientation (superior versus inferior endplate)
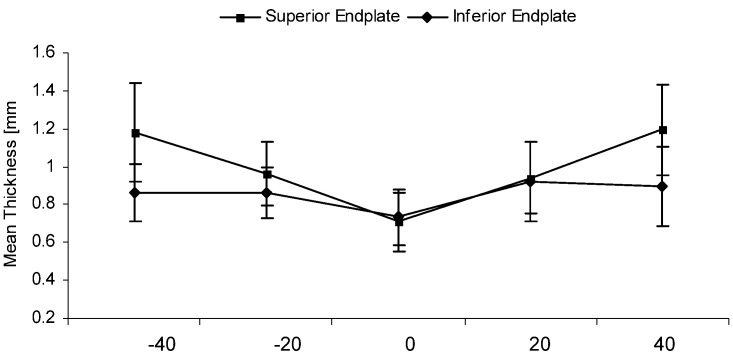
In both superior and inferior endplates, peripheral areas were significantly thicker than the central region (Scheffe-test, P<0.001; Fig. 5). No significant differences were observed for any of the scans between superior and inferior endplates (ANOVA, P=0.9).
Fig. 5.
Graph, giving the mean thickness (mm) of all superior and inferior endplates, measured at five points (−40, −20, 20, 40) of scan 9.00–3.00
Variations of thickness of the cervical spine endplate with respect to the level (C4, C5, C6, C7)
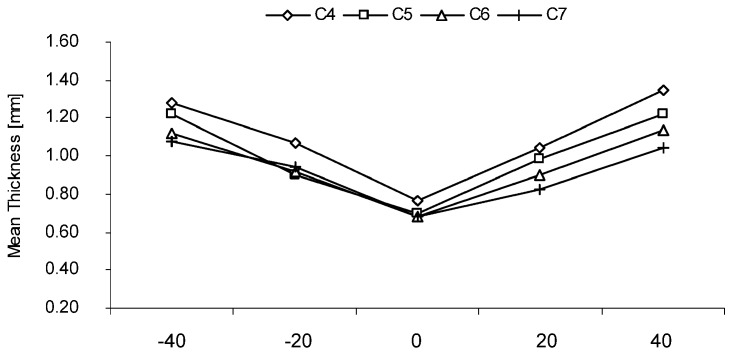
For all levels, the endplate within the peripheral regions was thicker than within the central region (Fig. 6). This difference reached significance for both the superior and inferior endplate of C4, C5, and C6 and the inferior endplate of C7 (Scheffe-test, p<0.05) but was a trend for the superior endplate of C7. Anterior points were always thicker than corresponding posterior points. This difference was always significant (P<0.05) with the exception of +40% compared to −40% in the oblique cut (P=0.159).
Fig. 6.
Graph, giving the mean thickness (mm) of superior cervical spine endplates with respect to vertebral level (C4, C5, C6, C7), measured at five points (−40, −20, 20, 40) at scan 9.00–3.00. For reasons of clarity, standard deviations are not shown
Discussion
Results of the current study
The current study found that the endplates of the middle and lower cervical spine are significantly thicker in the peripheral than in the central regions. This variation of thickness was not dependent on either the orientation of the endplate (superior or inferior) or the level of the vertebra (C4, C5, C6, C7).
Anatomical data for cervical spine endplates
Recently, Panjabi et al. [13] reported detailed anatomical data for the cervical spine endplates, including endplate and cortical shell thickness, peripheral dimensions, indentations, and angular dimensions. The thickness of the cervical spine endplate was measured using digitised radiographs made from sagittal cuts from the central regions of the vertebral bodies. Thickness was measured at 33%, 50%, and 67% of the depth of the vertebral body. Thickness at the centre point (50%) was 0.42–0.58 mm for the superior and 0.53–0.64 mm for the inferior endplate. For the superior endplates, the posterior region (67%) was always thicker than the centre point, and anterior region (33%) was also thicker than the centre point (except for C7). For the inferior endplate, the anterior region (33%) was always thicker than the centre point (except for C3), and the posterior region (67%) was thicker than the central point in C5. Lim et al. [11] also investigated the thickness of the central portion of the cervical spine endplate using CT data. A mean thickness of 0.53–0.63 mm was found.
In the current study, the centre point of both the superior and inferior endplate was shown to usually be the thinnest part of the endplate. This was also shown by Panjabi et al. [13]; however, there are some differences between the current study and the work by Panjabi et al. concerning the inferior endplate, which Panjabi et al. described to be thinner in the anterior region than in the central region. This was not the case in the current study. We also found slightly higher values for the cervical spine endplate thickness than described before [11, 13]. However, it has to be kept in mind that the endplates are thin and these dissimilarities may be explained by the differences in measurement methods, measurement points and software used.
Mechanical importance of the spinal endplate and clinical relevance of the study
Removal of the endplate in the cervical vertebra decreases the load to failure of the vertebral body [11]. However, for the thoracolumbar endplate, Hollowell et al. [8] found no significant effect on load to failure in compression loading if the vertebral endplate was preserved. Steffen et al. [17] performed a study on human lumbar cadaveric spines using two different interbody implants (full-surface implant versus implant with peripheral surface support) and two types of endplate preparation techniques (intact bony endplate versus removal of the central bony endplate). Neither implant design nor endplate preparation techniques affected the ultimate compression. In contrast, Oxland et al. [12] found that removal of the endplate in human lumbar spines reduced both the failure load and stiffness. Therefore, a question of some clinical relevance is “Where may the endplate be removed and where should it be preserved?”. Bone grafts and cages used for cervical spine fusion are in close contact to the endplates. Bone graft and endplate can be modified according to the patients anatomy and surgical considerations. However, if a spacer is used, it usually can not be modified. As a consequence, only the endplate may be drilled to fit the shape of the spacer. As a recommendation based upon the results described here, it seems to be appropriate not to remove the endplate within its thickest parts so as not to weaken the interface between the interbody implant and the adjacent vertebral body. Frequently, the endplates are resected to obtain better sight into the (collapsed) disc space. Better view into the disc space, however, may be obtained by using a microscope and slight overdistraction. Another reason for resection of the endplates has been the shape of the classic tricortical bone graft and some cages. In other words, the disc space had to be adopted to the shape of the graft or cage. A better way, therefore, would be to adopt the geometry of new cages to the geometry of the cleaned disc space in which the endplates have been preserved.
It has been shown that the lateral regions of the lumbar vertebra are significantly stronger than the centre [7] and that the endplate has a significant influence on compression stiffness [12]. Facing the results of the current study, similar mechanical properties could be expected for the cervical vertebral bodies. This, however, must not necessarily be true, and comparable data do not exist for the cervical spine.
Limitations of the study
Silva et al. [15] investigated the thickness of the human lumbar vertebral shell and endplate. They found that the vertebral shell and endplate appear significantly thicker when measured from CT images. Therefore, the results described in the current study may overestimate the thickness of the cervical spine endplate. This especially seems to be true if our results are compared to the results by Panjabi et al. [13], who used digitised radiographs for measurement and found overall slightly smaller values for the thickness of the cervical spine endplate. In addition, endplate thickness may—especially in the lateral aspects—be slightly overestimated by the direction in which the measurement was done. The specimens were glued onto a piece of wood with the central region oriented precisely horizontally. The thickness was measured perpendicular to the horizontal plane at the points described above. Due to the inclination of the endplate in its peripheral regions, the region of interest for measurement of the endplate thickness is longer in the lateral parts were inclination is more pronounced—especially within the uncinatus process. This may also have artificially produced slightly higher values in thickness of cervical spine endplates. Moreover, the pixel size of 0.4 mm is below, but close to the measured distances. This also may result in a possible overestimation in cortical thickness. However, the main objective of the current study was to analyse variations of thickness of the cervical spine endplate more than absolute values to look where the endplate is thickest with special reference to surgical applicability.
Conclusion
The peripheral regions of the cervical spine endplate are usually thicker than its central region. Neither endplate orientation (superior or inferior) nor level (C4, C5, C6, C7) seems to have an influence on this anatomical detail of the endplates.
Acknowledgement
The scientific work was performed at the Neurosurgical Department and Neuroradiology of the University of Saarland, 66421 Homburg/ Saar.
References
- 1.BöhlerJ Trauma 1980202037359594 [Google Scholar]
- 2.Caspar Orthop Praxis. 1984;12:981. [Google Scholar]
- 3.Caspar Neurosurgery. 1989;25:491. doi: 10.1097/00006123-198910000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Cloward J Neurosurg. 1958;15:602. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 5.De Spine. 1987;12:324. doi: 10.1097/00007632-198705000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Fernyhough Spine. 1992;17:1474. doi: 10.1097/00007632-199212000-00006. [DOI] [PubMed] [Google Scholar]
- 7.GrantSpine 20012688911317111 [Google Scholar]
- 8.Hollowell Spine. 1996;21:1032. doi: 10.1097/00007632-199605010-00007. [DOI] [PubMed] [Google Scholar]
- 9.Kuhn Clin Orthop Relat Res. 1986;209:224. [PubMed] [Google Scholar]
- 10.Kurz Spine. 1984;14:1324. doi: 10.1097/00007632-198912000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Lim Spine. 2001;26:951. doi: 10.1097/00007632-200104150-00021. [DOI] [PubMed] [Google Scholar]
- 12.Oxland Spine. 2003;28:771. doi: 10.1097/00007632-200304150-00008. [DOI] [PubMed] [Google Scholar]
- 13.Panjabi Spine. 2001;26:2478. doi: 10.1097/00007632-200111150-00016. [DOI] [PubMed] [Google Scholar]
- 14.PitzenJ Neurosurg 20029712812120636 [Google Scholar]
- 15.Silva Bone. 1994;15:409. doi: 10.1016/8756-3282(94)90817-6. [DOI] [PubMed] [Google Scholar]
- 16.SmithJ Bone Joint Surg Am 19854060713539086 [Google Scholar]
- 17.Steffen Spine. 2000;25:1077. doi: 10.1097/00007632-200005010-00007. [DOI] [PubMed] [Google Scholar]
- 18.Summers J Bone Joint Surg Br. 1989;71:677. doi: 10.1302/0301-620X.71B4.2768321. [DOI] [PubMed] [Google Scholar]
- 19.Tippits Neurosurgery. 1989;22:1008. [Google Scholar]
- 20.Wilke Eur Spine J. 2000;9:410. doi: 10.1007/s005860000168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilke Spine. 2000;25:2762. doi: 10.1097/00007632-200011010-00008. [DOI] [PubMed] [Google Scholar]