Abstract
A previously undescribed method for posterior fusion of the sacroiliac joint (SIJ) utilizing the Cloward instrumentation is presented, suitable for cases with chronic pain and intact ligamental structures of the SIJ. The advantages of the method in comparison with other described options include minimal disturbance of the periarticular structures, avoidance of introduction of metalwork and preservation of the iliac crest contour. This technique has been used in five cases with follow-up longer than 2 years (mean 29 months, range 25–41 months). In all cases there was resolution of their painful symtomatology.
Keywords: Sacroiliac joint, Fusion, Chronic pain
Introduction
Chronic pain originating from the sacroiliac joint is a rare encounter in the orthopaedic practice. Most commonly it is the result of post-traumatic arthrosis, but on rare occasions it can be caused by ankylosing spondylitis, rheumatoid arthritis or can be idiopathic in nature. Diagnosis can often be challenging as low back pain can be confused with sacroiliac pain, and vice versa [9, 22]. Surgical intervention can be considered in symptomatic cases with functional impairment where all appropriate conservative measures have failed to produce pain relief.
We present a previously undescribed technique for sacroiliac fusion in cases with intact ligamental constrains of the joint that present with chronic pain.
Surgical technique
Analytical discussion over the indications for sacroiliac fusion is beyond the purpose of this article. In our practice, we offer this type of procedure to patients with long-standing symptoms arising from their sacroiliac joint who have failed to respond to conservative management and have experienced temporary relief of their symptoms following injection of their affected joint under image intensification.
The patient is placed in the prone position with adequate support to avoid respiratory compromise. Prophylactic antibiotics are not routinely given as this technique does not formally expose the sacroiliac joint and does not involve introduction of metalwork.
Following skin marking of the anatomical landmarks, a longitudinal incision is performed at the level of the affected sacroiliac joint. The posterior iliac spine is identified and its posterior aspect is exposed subperiosteally by elevating the attachments of gluteus maximus muscle. Specific attention is given not to lift any subcutaneous flaps in order to avoid injury of the superior cluneal nerves.
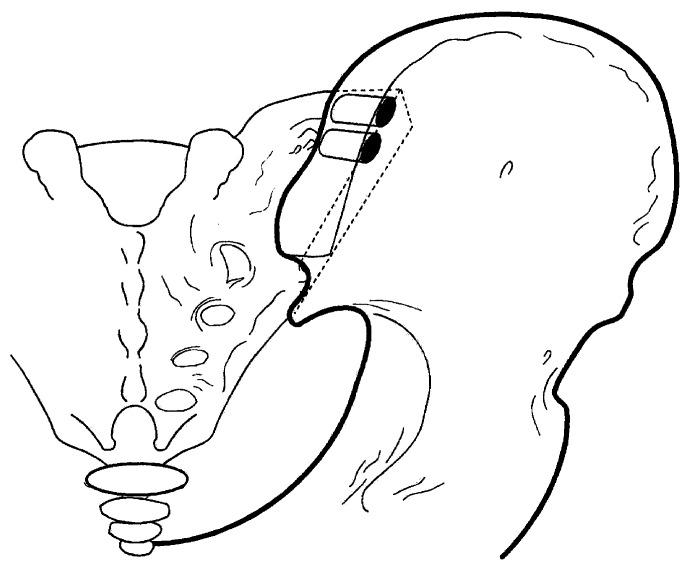
At this stage an image intensifier is placed obliquely in order to identify the exact projection of the sacroiliac joint at the posterior aspect of the ileum. This stage is necessary in order to allow safe removal of the bone plugs without disturbing the subsequent deposition sites. Once this has been achieved, with the assistance of Cloward’s type of instrumentation, two large bicortical bone plugs are removed from the posterior iliac crest to be used as bone grafts (Fig. 1).
Fig. 1.
Area for removal of the two “bone plugs” from the posterior Iliac crest
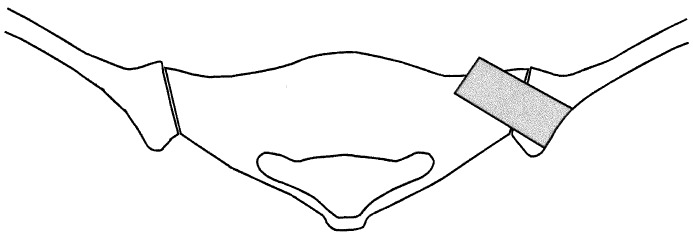
Following this, a large hole is drilled of a slightly smaller diameter to the bone-graft plugs, at the posterior iliac wing aiming to remove the superior part of the sacroiliac joint as identified by the image intensifier. The specimen is examined to make sure that part of the sacroiliac joint has indeed been included at the removed bone plug. The obtained bone-graft plug is then impacted to the hole creating a bridge of cancellous bone at the superior aspect of the sacroiliac joint (Fig. 2). The procedure is then repeated at the inferior aspect of the sacroiliac joint. The wound is closed in layers without use of drains.
Fig. 2.
Deposition of the “bone plugs” as seen on a cross section
Postoperatively, the patient is discharged home as soon as he/she is comfortable to ambulate non-weight bearing on crutches. The patient is allowed to start weight bearing 3 months following the operation. Plain radiographs are not performed for follow-up purposes, as they do not allow reliable assessment of whether the fusion was successful or not.
Case reports
Between 1997 and 2000 we performed sacroiliac fusion with the above-mentioned technique in five patients (Table 1). These patients have been followed-up prospectively.
Table 1.
Demographic characteristics, investigations and outcome of the five presented cases
| Case no. | Age (years) | Gender | Aetiology | Imaging | Tm-99 bone scan | Duration of pain relief | Outcome |
|---|---|---|---|---|---|---|---|
| 1 | 37 | Female | Idiopathic | MRI scan: normal SIJ | No uptake at SIJ | 12 weeks | Complete relief of symptoms |
| 2 | 26 | Male | Fall from height “open-book” type of fracture treated with external fixation | CT scan: SIJ diastasis | Uptake at SIJ | 6 weeks | Complete relief of symptoms |
| 3 | 44 | Female | Road-traffic accident; pelvic injury with isolated inferior pubic ramus fracture | Not performed | Not performed | 2 h | Complete relief of symptoms |
| 4 | 22 | Female | Ski injury; no fracture identified | MRI scan: normal SIJ | No uptake at SIJ | 4 h | Complete relief of symptoms |
| 5 | 24 | Male | Fall from height; undisplaced fracture pubic rami and ipsilateral fracture neck of femur | MRI scan: normal SIJ | No uptake at SIJ | 10 weeks | Resolution of SIJ symptoms Persistence of lower back symptomatology |
All patients presented with localized unilateral sacroiliac joint tenderness. In four cases there was history of trauma with duration of the symptoms ranging between 10 and 40 months. In the remaining case (case 1) the aetiology was considered idiopathic, as all investigations, including thorough rheumatological screening, were negative for any systemic disorder. In all cases conservative measures had failed to produce significant relief. Clinical examination, which included localized sacroiliac joint tenderness, positive sacroiliac rocking (“knee-to-shoulder”) test and positive femoral shear test [12] suggested sacroiliac joint pathology.
Magnetic resonance imaging and Tm-99 bone scans were performed in the majority of the patients, but we found that they were unreliable for identifying the source of the symptoms. All patients had temporary relief of their symptoms following injection of a mixture of local anaesthetic and long-acting corticosteroid with the assistance of an image intensifier. The obtained relief ranged between a few hours and 3 months. Two of the patients (cases 1 and 5) opted for a second injection before considering a surgical procedure.
All operations were performed by the senior author (H.A.M.) who is a specialist in pelvic surgery. There were no documented intra-operative or early postoperative complications. Follow-up ranged between 25 and 41 months (mean 29 months). Detailed clinical examination was performed in all cases 3 months following their procedure and at their longest follow-up appointment. During follow-up, particular attention was given to identify any iatrogenic injury of the superior cluneal nerves and reversal of the above-mentioned sacroiliac stress tests. Subjective satisfaction was measured during their longest follow-up appointment with the aid of a visual analogue.
Four of the patients had complete resolution of their symptoms and were subjectively highly satisfied with the outcome of the operation scoring 10 of 10 at the visual analogue. In the fifth case (case 5) the patient had concomitant evidence of lumbar osteoarthrosis and described only partial resolution of the symptoms. Clinically, there was reversal of the sacroiliac stress tests and subjectively scored 8 of 10 at the visual analogue score. This patient subsequently underwent a CT scan, which demonstrated successful fusion of the sacroiliac joint (Fig. 3).
Fig. 3a, b.
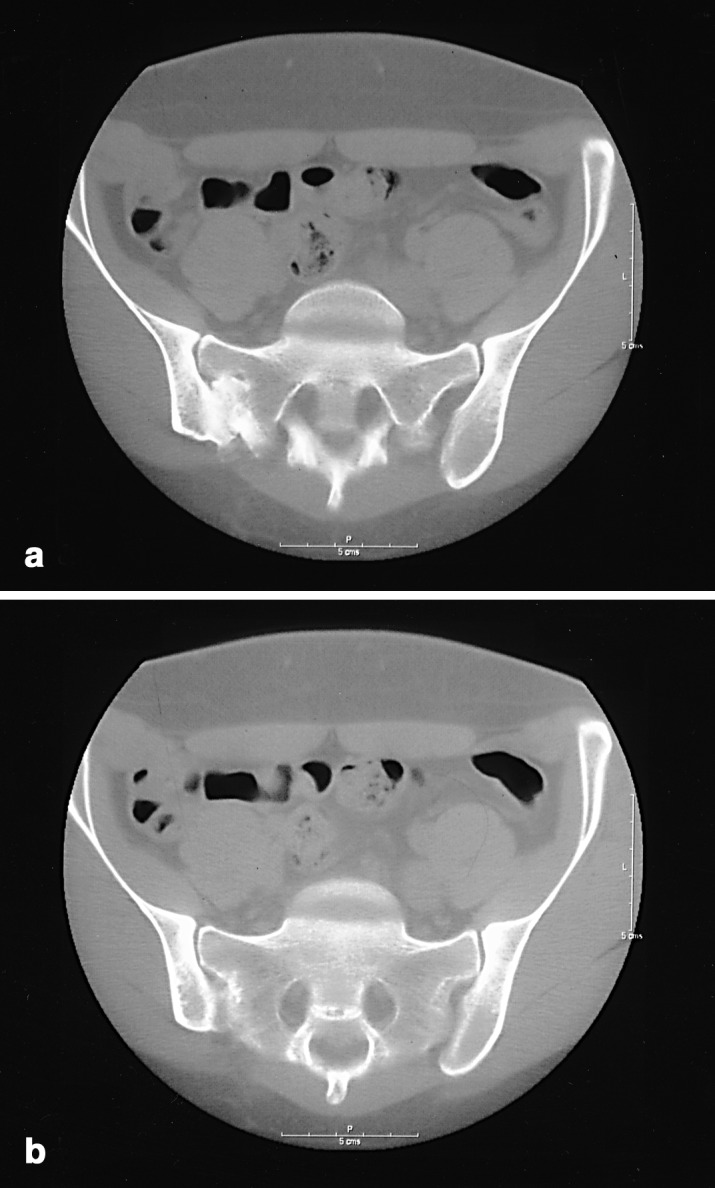
A CT scan imaging demonstrating successful fusion of the affected sacroiliac joint. a Superior bone plug. b Inferior bone plug
Discussion
There is a large number of described surgical options for fusion of the sacroiliac joint in the orthopaedic literature, none of which are universally accepted. A number of them attempt to approach the joint from its anterior aspect [8, 11, 16, 21] exposing the inner table of the ileum following which the articular surface is denuded, bone grafted and the joint is stabilised with plates and screws. Posterior approaches include transiliac bars, a variety of plates, iliosacral lag screws or fixation with pedicle screw type of systems [1, 2, 4, 10, 11, 13, 14, 15, 17, 19, 22]. In addition to these, there have been a number of reports of percutaneous fixation under the guidance of fluoroscopy or computer tomography [3, 6, 7, 18, 20]. Fusion rates in the described series are high; however, in all cases, significant disadvantages and/or complications are emphasised, most of which are related to the exposure of the joint and the metalwork placement. Common ground of all described methods includes exposure and meticulous denudement of the articular surface and, in most cases, the need to introduce some kind of metalwork to allow immobilization and/or compression of the joint. All authors further agree that sacroiliac joint fusion requires a high level of expertise due to the difficulty of the approach and the significant morbidity of any resulted complication.
The method that is described in this article is not suitable for the acute trauma setting and can only be applied in cases in which the stability of the joint has been preserved. It can be considered to introduce two main innovations in comparison with the previously described methods. Firstly, it does not formally expose the sacroiliac joint, as it is approached through its projection at the iliac wing. As a result, none of the ligamental structures of the joint are affected preserving its inherent stability. Furthermore, it minimises all the potential complication that have been associated with the posterior approach such as injury to the erector spinae muscle insertions and the dorsal sensory nerve roots.
The second innovation refers to the lack of need to use any metalwork to stabilize the fusion. This seems to be unnecessary as both the posterior and anterior ligamental structures are unaffected. This fact has significant importance, as the majority of the complications described in the literature are associated with the misplacement of screws, which, in the majority of the cases, has to be performed blindly with reference only to anatomical landmarks.
Other advantages of the method include the preservation of the contour of the posterior iliac crest, the preservation of the cluneal nerves and, most importantly, the simplicity of the operation.
Finally, we feel that if fusion is not achieved by this method, revision surgery should be much easier by any approach as there is no scar formation around the neural structures.
It can be argued whether these patients should remain non-weight bearing, and if so, whether this should be for a period of 3 months. There is no doubt that in any weight-bearing status there are significant forces that are transmitted through the sacroiliac joint [5]. We feel, however, that by requesting a non-weight-bearing status, the patients are forced to restrict their mobility and avoid activities that could lead to excessive loading of the joint.
Finally, we feel that even though the presented results are highly encouraging, more cases are probably required to establish the usefulness of the proposed technique.
References
- 1.Albert J Orthop Trauma. 1993;7:226. doi: 10.1097/00005131-199306000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Balanger J Spinal Disord. 2001;14:118. doi: 10.1097/00002517-200104000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Cecil Spine. 1996;21:875. doi: 10.1097/00007632-199604010-00022. [DOI] [PubMed] [Google Scholar]
- 4.Dabezies Clin Orthop. 1989;246:165. [PubMed] [Google Scholar]
- 5.Dalstra J Biomech. 1995;28:715. doi: 10.1016/0021-9290(94)00125-N. [DOI] [PubMed] [Google Scholar]
- 6.Duwellius J Orthop Trauma. 1992;6:420. doi: 10.1097/00005131-199212000-00005. [DOI] [PubMed] [Google Scholar]
- 7.EbraheimClin Orthop 19943072227924036 [Google Scholar]
- 8.Ebraheim Orthopaedics. 1992;15:1427. doi: 10.3928/0147-7447-19921201-08. [DOI] [PubMed] [Google Scholar]
- 9.Fortin Am J Orthop. 1999;28:687. [PubMed] [Google Scholar]
- 10.Kellam Orthop Clin North Am. 1987;18:25. [PubMed] [Google Scholar]
- 11.LeightonClin Orthop 19863291158769442 [Google Scholar]
- 12.Magee DJ (1987) Pelvic joints. In: Magee DJ (ed) Orthopaedic physical assessment, 2nd edn. Saunders, Philadelphia, pp 308–332
- 13.Marcus R, Hansen S (1984) Bilateral fracture-dislocation of the sacrum. J Bone Joint Surg [Am] 66:1297–1299 [PubMed]
- 14.Matta Clin Orthop. 1989;242:83. [PubMed] [Google Scholar]
- 15.Mears Instr Course Lect. 1988;37:143. [PubMed] [Google Scholar]
- 16.Rand J (1985) Anterior sacro-iliac arthrodesis for post-traumatic sacro-iliac arthritis. J Bone J Surg [Am] 67:157–159 [PubMed]
- 17.Routt Injury. 1996;27:B20. doi: 10.1016/0020-1383(96)89816-0. [DOI] [PubMed] [Google Scholar]
- 18.Routt J Orthop Trauma. 1995;9:207. doi: 10.1097/00005131-199506000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Routt Tech Orthop. 1994;9:300. [Google Scholar]
- 20.Routt J Orthop Trauma. 1997;11:584. doi: 10.1097/00005131-199711000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Simpson J Trauma. 1987;27:1332. doi: 10.1097/00005373-198712000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Waisbrod Arch Orthop Trauma Surg. 1987;106:238. doi: 10.1007/BF00450461. [DOI] [PubMed] [Google Scholar]