Abstract
An earlier paper by Becker and Reed provided an in-depth review of the pharmacology of local anesthetics. This continuing education article will discuss the importance to the safe and effective delivery of these drugs, including needle gauge, traditional and alternative injection techniques, and methods to make injections more comfortable to patients.
Key Words: Local anesthetics, Dentistry, Techniques, Needle gauge, Warming, Buffering, Novel devices
Local anesthesia forms the backbone of pain control techniques in the dental profession. Local anesthetics represent the safest and most effective method for managing pain associated with dental treatment. They are the only drugs that prevent the nociceptive impulse from reaching the patient's brain.
Local anesthetics need to be deposited as close to the nerve as possible so that optimal diffusion of the drug may occur, providing profound anesthesia and a pain-free dental experience. The importance of this is demonstrated by the fact that when patients are asked to list the most important factors used when selecting a dentist, the 2 most important are: (1) a dentist who does not hurt and (2) a painless injection.1 Unfortunately, for painless dentistry to be accomplished, local anesthetics need to be injected using a cartridge, syringe, and needle. This leads to the major problem of fear of needles (trypanophobia) and its consequences, ie, the occurrence of syncope or other medical emergencies during injection of the local anesthetic. More than 50% of medical emergencies occurring in dental offices happen during or immediately following administration of a local anesthetic.2
An earlier paper by Becker and Reed3 provided an in-depth review of the pharmacology of these invaluable drugs. In the present paper we will discuss issues of importance to the safe and effective delivery of these drugs, including needle gauge, traditional and alternative injection techniques, and methods to make injections more comfortable for patients (eg, warming, buffering, novel delivery devices). In addition, we will look at the future of local anesthesia in dentistry.
NEEDLE GAUGE
Gauge refers to the diameter of the lumen of the needle; the smaller the number, the greater the diameter of the lumen. A 30-gauge needle has a smaller internal diameter than a 25-gauge needle, for example. There is a trend among dentists toward the use of smaller-diameter needles on the assumption that they are less traumatic to the patient than larger-diameter needles. However, studies dating back to 1972 show this assumption to be unwarranted.4–9 Hamburg4 reported that patients are unable to differentiate among 23-, 25-, 27-, and 30-gauge needles. Fuller and colleagues5 reported no significant differences in the perception of pain produced by 25-, 27-, and 30-gauge needles during inferior alveolar nerve blocks in adults. Lehtinen6 compared 27- and 30-gauge needles and found that, although insertion of the 30-gauge needle required significantly less force, the difference in pain perception was less remarkable.8 To prevent accidental intravascular injection, aspiration must be performed before the deposition of any significant volume of local anesthetic. Trapp and Davies10 and Delgado-Molina and colleagues11 reported that no significant differences existed in the ability to aspirate blood through 25-, 27-, and 30-gauge dental needles. However, there is increased resistance to aspiration of blood through a thinner needle (eg, 30-gauge) compared with a larger-diameter needle (eg, 27- or 25-gauge). Needle deflection along the axis of the bevel and breakage must also be examined. The smaller the diameter of the needle, the more it deflects. Thirty-gauge needles deflect significantly, whereas 25-gauge needles essentially do not deflect at all. Likewise, 25-gauge needles very rarely, if ever, break during an intraoral injection, and 99% of the needles that do break are 30-gauge needles.12
TECHNIQUES
Posterior Superior Alveolar
The posterior superior alveolar (PSA) injection will anesthetize the maxillary molars except for the mesiobuccal aspect of the first molar (Figure 1). The periodontal ligament (PDL), bone, periosteum, and buccal soft tissue adjacent to these teeth are also anesthetized.13 Clinically, the PSA injection is given with the insertion point at the height of the buccal vestibule at a point just distal to the malar process. The needle is inserted distally and superiorly at approximately 45 degrees to the mesiodistal and buccolingual planes. The depth of insertion is approximately 15 mm, and following careful aspiration, 1.0 mL of solution is slowly deposited.14,15
Figure 1.
Posterior superior alveolar (PSA) nerve block.
Middle Superior Alveolar
The middle superior alveolar (MSA) injection will anesthetize the mesiobuccal aspect of the maxillary first molar, both premolars, PDL, buccal bone, and periosteum, along with the soft tissue lateral to this area13 (Figure 2). Penetration for the MSA injection is at the height of the buccal vestibule lateral to the maxillary second premolar. The needle tip should approximate the apex of the tooth, which usually requires a penetration of about 5 mm. One milliliter of anesthetic solution should slowly be introduced after careful aspiration.14–16 NOTE: In many patients, the MSA nerve is absent. If this is the case, the anterior superior alveolar (ASA) injection will anesthetize the premolar region.
Figure 2.
Middle superior alveolar (MSA) nerve block.
Anterior Superior Alveolar
The ASA injection will anesthetize the PDL, alveolar bone, periosteum, buccal soft tissue, and teeth from the canine to the midline13 (Figure 3). The depth of penetration is similar to that of the MSA injection; however, the penetration is over the maxillary canine. Slow deposition of 1.0 mL of solution after aspiration is generally sufficient.14–16 Crossover innervation must always be considered in case of inadequate anesthesia near the midline.
Figure 3.
Anterior superior alveolar (ASA) nerve block.
Greater Palatine
The greater palatine (GP) injection will anesthetize the tissues of the hard palate from its most distal aspect, anteriorly to the distal of the canine, and laterally to the midline13 (Figure 4). The entrance to the greater palatine foramen may be palpated as a depression or soft spot in the posterior area of the hard palate. It is usually located halfway between the gingival margin and the midline of the palate, approximately opposite the distal of the maxillary second molar.14–16 Anatomically, this is generally 5 mm anterior to the junction of the hard and soft palates. Penetration will occur through the epithelium, and the needle will appear to “fall into” a space of less resistance. The needle should be inserted until bone is contacted. The depth of penetration is variable, but usually less than 5 mm is sufficient. After aspiration, 0.5 mL of anesthetic solution is very slowly deposited.
Figure 4.
Greater palatine (GP) nerve block.
Nasopalatine
The nasopalatine (NP) injection will anesthetize the tissues of the palatal aspect of the premaxilla13 (Figure 5). The entrance to the nasopalatine foramen is at the incisive papilla, which may be visualized posterior to the maxillary central incisors. The most comfortable way to perform this injection is to first deposit 0.3 mL of local anesthetic in the maxillary anterior midline. Then, with the needle at a 90-degree angle to the soft tissue, the attached keratinized tissue can be slowly penetrated and anesthetic solution forced ahead of the needle. Once the nasopalatine area is blanched, the final needle puncture is given. The needle tip should contact soft tissue at the lateral aspect of the incisive papilla with a depth of penetration of <5 mm and bony endpoint. Approximately 0.25 mL may be very slowly introduced after aspiration.14–16 NOTE: Some patients also have a contribution from this nerve to the pulpal tissue of the maxillary incisors.
Figure 5.
Nasopalatine (NP) nerve block.
Inferior Alveolar
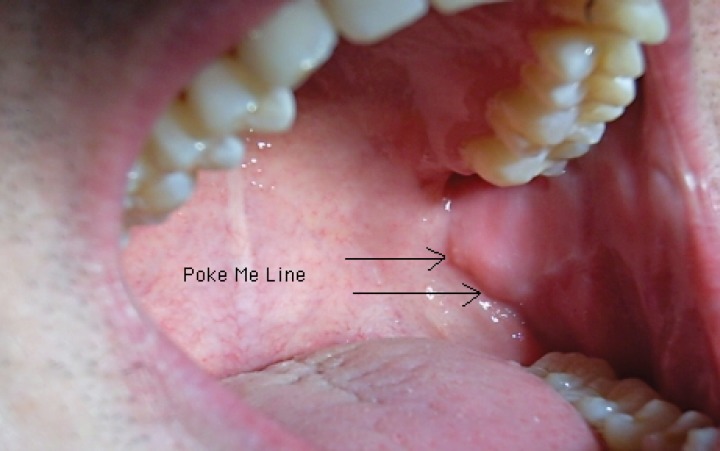
The inferior alveolar (IA) injection will anesthetize the mandibular teeth from the third molar to the midline, the buccal soft tissue from the premolars anteriorly, the body of the mandible, the periosteum, the PDL, and the skin and subcutaneous tissues of the chin and lower lip, all on the ipsilateral side13 (Figure 6). In an IA block, a long needle is positioned parallel to the mandibular occlusal plane from the contralateral premolar area to a point on the soft tissue approximately 1.5 cm above the mandibular occlusal plane. Traditionally, the IA injection is described with an insertion point 1.0 cm above the mandibular occlusal plane. The use of a 1.5-cm puncture point should increase the success rate from approximately 84% to 96%.17 The mucosa is pierced at a point between the pterygomandibular raphe and the deep tendon of the temporalis muscle, and the needle is advanced until bone is contacted, usually about 25 mm.14–16 The best way to visualize the lateral positioning of the needle prior to penetrating soft tissue is to look for the depression seen on the immediate lateral aspect of the pterygomandibular raphe. The author has termed this the “poke me line” (Figure 7). Once the needle is advanced and bone contacted, the tip should now be just superior to the lingula. The needle should be withdrawn 1–2 mm so it is no longer under the periosteum. After careful aspiration, 1.5 mL of solution may be deposited. As the needle is being removed, when it is approximately halfway out, the lingual nerve is injected with the remaining solution, unless a buccal nerve block will be done. In that case, a few drops of local anesthetic should be reserved. Frequently, even without this last step, the lingual nerve will be anesthetized. This injection has the highest frequency of positive aspiration of all intraoral injections.
Figure 6.
Inferior alveolar (IA) nerve block.
Figure 7.
The “poke me” line.
Lingual
The lingual nerve block will anesthetize the lingual gingiva, floor of the mouth, and tongue from the third molar anteriorly to the midline.13 This nerve may be anesthetized as described earlier or directly, by inserting the needle as in the IA to approximately 10 mm and injecting.
Buccal
The buccal injection will anesthetize the buccal soft tissue lateral to the mandibular molars.13 The needle is inserted into the tissue in the distobuccal vestibule opposite the second or third mandibular molar just medial to the coronoid notch until bone is contacted (approximately 1 to 3 mm), and 0.25 mL of anesthetic is deposited.
Second Division
The entire maxillary division of the trigeminal nerve is anesthetized from either of 2 intraoral approaches, but most frequently the second division (V2) is approached via the GP canal (Figure 8). The V2 block injection anesthetizes the maxillary teeth and periodontium, hard and soft palates, sinuses, and portions of the nose, orbit, upper cheek, lower eyelid, and side of the face.13 The entrance to the foramen is located at the distolateral aspect of the same depression felt during palpation before the GP injection. This foramen generally is located halfway between the gingival margin and the midline of the palate, approximately 5 mm anterior to the junction of the hard and soft palates. After a good GP injection is administered (0.3 mL), a long needle is used to probe the canal entrance gently. Angulation is mostly superior, with slight distal and lateral components.14–16 The most effective position of the needle for administration of the V2 block injection generally is such that a 45-degree angle exists between the needle and the soft tissue. The needle is inserted to a depth of approximately 30 mm. After aspiration, the contents of the cartridge are slowly deposited.18 Up to 15% of patients have anatomical deviations that make this approach ineffective, since the needle cannot physically be manipulated up the canal to the proper depth.
Figure 8.
Second division (V2) nerve block.
Gow-Gates
George A. E. Gow-Gates first published this technique in 197318 (Figure 9). Significant advantages of the Gow-Gates technique over the IA nerve block include its higher success rate, its lower incidence of positive aspiration, and the absence of problems with accessory sensory innervation to the mandibular teeth. The Gow-Gates injection anesthetizes the inferior alveolar, lingual, auriculotemporal, buccal (75% of the time), and mylohyoid nerves. The injection blocks the nerves at a point that is proximal to their division into inferior alveolar, buccal, and lingual nerves. The needle endpoint is the lateral aspect of the anterior portion of the condyle, just inferior to the insertion of the lateral pterygoid muscle. The injection is performed by having the patient open the mouth as widely as possible to rotate and translate the condyle forward. The condyle is palpated with the fingers of the nondominant hand while the cheek is retracted with the thumb. Beginning from the contralateral canine, the needle is positioned so that a puncture point is made approximately at the location of the distobuccal cusp of the maxillary second molar. A 25-gauge long needle is inserted slowly to a depth of 25 to 30 mm; the endpoint is inferior and lateral to the condylar head. The injection must not be performed unless bone is contacted to ensure proper needle placement. After the needle is withdrawn 1–2 mm, the clinician aspirates and injects the contents of the cartridge. This injection is unique among intraoral injections because the operator does not attempt to get as close as possible to the nerve to be anesthetized. In fact, the needle tip should be approximately 1.0 cm directly superior to the nerve, in the superior aspect of the pterygomandibular space.
Figure 9.
Gow-Gates (GG) nerve block.
Vazirani-Akinosi
This form of injection, also known as the closed-mouth mandibular block, anesthetizes the inferior alveolar, lingual, buccal, and mylohyoid nerves18 (Figure 10). This injection is useful for patients with trismus because it is performed while the jaw is in the physiologic rest position. A 25-gauge long needle is inserted parallel to the maxillary occlusal plane at the height of the maxillary buccal vestibule. The bevel should be oriented away from the bone of the mandibular ramus so that deflection occurs toward the ramus. The depth of penetration is approximately half the mesiodistal length of the ramus, which is about 25 mm in adults (measured from the maxillary tuberosity). The depth of insertion will vary with the anteroposterior size of the patient's ramus. The Vazirani-Akinosi injection is performed “blindly” because no bony endpoint exists. However, in adult patients, a rule of thumb is that the hub of the needle should be opposite the mesial aspect of the maxillary second molar. After aspiration, the contents of the cartridge can be deposited slowly.
Figure 10.
Vazirani-Akinosi nerve block.
Mental/Incisive
The mental and incisive nerves are terminal branches of the IA nerve. The mental nerve exits the mental foramen at or near the apices of the mandibular premolars. The incisive nerve continues anteriorly in the incisive canal. Both nerves will be anesthetized after a successful mandibular nerve block, but this injection technique can be useful when bilateral anesthesia is desired for procedures on premolars and anterior teeth. The lingual tissues are not anesthetized with this block. The initial technique for the mental and incisive nerve blocks is the same. A 25- or 27-gauge short needle is inserted at the mucobuccal fold at or just anterior to the mental foramen, which is typically located between the apices of the 2 premolars. The bevel of the needle should be oriented toward the bone and the tissue penetrated to a depth of 5 to 6 mm. After aspiration, approximately one third to one half of the cartridge (0.6–0.9 mL) should be deposited. The difference between the mental nerve block and the incisive nerve block is that the incisive nerve block requires pressure to direct local anesthetic solution into the mental foramen. This can be accomplished by maintaining gentle pressure at the injection site for approximately 2 minutes following deposition of the solution.
Periodontal Ligament
The PDL injection method of anesthetizing an individual tooth is utilized to avoid the undesirable consequences of regional block anesthesia. A 27-gauge short needle with the bevel toward the tooth is inserted through the gingival sulcus on the mesial of the tooth to be anesthetized and inserted as far apically as possible. Approximately 0.2 mL of anesthetic solution is deposited over a minimum of 20 seconds. Then the same technique is performed on the distal of the tooth. This injection may be uncomfortable if the rate of injection is too rapid or the tissues are inflamed. The duration of pulpal anesthesia is extremely variable, so repeated PDL injections may be necessary to complete a procedure.
Intraosseous
When conventional block and infiltration injections are ineffective, an intraosseous injection may be used to anesthetize a single tooth or multiple teeth in one quadrant (Figure 11). Originally, intraosseous anesthesia required the use of a round bur to provide entry into interseptal bone, which is still an acceptable technique. Once the hole had been made, a needle would be inserted into this hole and local anesthetic deposited. Now, specialized devices help to ease this injection technique. The Stabident System (Fairfax Dental Inc) comprises a slow-speed handpiece-driven perforator and a solid 27-gauge wire with a beveled end that, when activated, drills a small hole through the cortical plate. The anesthetic solution is delivered to cancellous bone through the 27-gauge ultrashort injector needle placed into the hole made by the perforator. The X-Tip (Dentsply) anesthesia delivery system consists of an X-Tip that separates into 2 parts: a drill and a guide sleeve. The drill (a special hollow needle) leads the guide sleeve through the cortical plate until it is separated and is then withdrawn. The remaining guide sleeve is designed to accept a 27-gauge needle to inject anesthetic solution. The guide sleeve is removed after the intraosseous injection is complete. The site for this technique is 2 mm apical to the intersection of lines drawn horizontally along the gingival margins of the teeth and a vertical line through the interdental papilla. The site should be distal to the tooth to be treated, and care should be taken to avoid the area of the mental foramen. The amount of anesthetic injected ranges from one third to three quarters (0.6 to 1.2 mL) of the cartridge. The onset of anesthesia is immediate, and pulpal anesthesia will last for 15–45 minutes.
Figure 11.
Intraosseous (X-Tip) anesthesia.
Intrapulpal
For a variety of reasons, profound anesthesia during an endodontic procedure may not be easily obtained. Once the pulp has been exposed, anesthetic may be placed directly into the pulp. A 27-gauge short needle is inserted into the pulp chamber and wedged firmly into the root canal. A small volume (0.2 to 0.3 mL) of local anesthetic is injected. While this technique may prove uncomfortable for the patient, it invariably works to provide effective pain control. In most cases, the duration is adequate to permit extirpation of the pulpal tissues.
Intraseptal
The intraseptal injection can be a useful technique for achieving osseous and soft tissue anesthesia and hemostasis for scaling and root planing and surgical flap procedures. A 27-gauge short needle is inserted at the center of the interdental papilla (about 2 mm apical to the gingival margin) adjacent to the tooth to be treated. The bevel should be oriented toward the apex of the tooth. The needle should be at a 45-degree angle to the long axis of the tooth and at a 90-degree angle to the gingiva. The dentist should slowly inject a few drops of anesthetic as the needle enters the soft tissue and then advance the needle until contact with bone is made. While gentle pressure is applied to the syringe, the needle is pushed slightly deeper (1 to 2 mm) into the interdental septum and 0.2 to 0.4 mL of anesthetic is deposited over a minimum of 20 seconds. The duration of anesthesia is variable. This injection technique should not be used if there are any signs of infection.
INCREASING COMFORT DURING THE INJECTION
Warming
There is conflicting evidence in the medical literature that warming local anesthetics to body temperature (37°C) diminishes the pain from injection.19,20 Warming local anesthetic cartridges does not appear to significantly reduce the pain associated with intraoral injections.21–23 Indeed, it may occasionally produce problems. Overheating the local anesthetic solution can lead to discomfort for the patient and destruction of a heat-labile vasoconstrictor (producing a shorter duration of anesthesia) over a period of time. It has been demonstrated that, after the warmed glass cartridge is removed from the cartridge warmer and placed into a metal syringe and the solution is forced through a fine metal needle, it has cooled nearly to room temperature.24 Cartridge warmers do not appear to be beneficial.
Buffering
The pH of local anesthetic solutions without vasoconstrictors is approximately 6.5. The addition of epinephrine (or levonordefrin) and the antioxidant sodium bisulfite lowers the pH into the range of 3.5 (lemon juice has a pH of 3.4). In the cartridge, the local anesthetic solution exists in 2 ionic forms: the tertiary form (B) and the quaternary form (BH+). The lower the pH of the solution, the greater the percentage of BH+ in the solution. For example, according to the Henderson-Hasselbach equation, at a pH of 3.5, 99.994% of a lidocaine solution is BH+. This is of clinical significance in that it is the tertiary form of the drug (B) rather than the BH+ form that is lipid soluble and able to diffuse across the lipid-rich nerve membrane entering into the nerve, where it then picks up a H+, which converts it into the quaternary form of the drug (BH+), which then enters into sodium channels and blocks nerve conduction.3
When a small percentage of B is available, the speed of onset of anesthesia would be considerably slowed were it not for the body's buffering capability. Once injected into the tissues, the natural process of buffering occurs. The normal pH of tissues is 7.4. A drug with a lower pH (e.g. 3.5) that is injected into tissues will be buffered by the body, and the pH of the injected solution will be slowly increased toward 7.4. As this process continues, the percentage of B ions in the solution steadily increases. For example, at a pH of 6.5, 3.83% of lidocaine ions are B, while at a pH of 7.4, this figure is 24.03%.
If the pH of the local anesthetic solution in the dental cartridge could be increased to 7.4 prior to injection, the speed of onset of the anesthetic should increase, as well as the comfort to the patient during the injection. (Local anesthetics at a pH of 3.5 produce a “burning” sensation as they are injected, and higher-pH solutions are rated by patients as more comfortable.) A third advantage to buffering the local anesthetic solution would be the 6,000-fold increase in the number of B molecules available to enter into the nerve, which would theoretically provide a more profound anesthetic effect.
Sodium bicarbonate is a commonly used buffer in medicine. It has been used in managing acidosis associated with medical conditions, such as prolonged cardiac arrest.25 Additionally, sodium bicarbonate is used by surgeons administering local anesthetic into the skin to assuage the pain commonly associated with the injection.26 In the medical profession, when multiple-dose vials of local anesthetics are used, sodium bicarbonate is added to the anesthetic immediately before injection. Studies have demonstrated both excellent and poor results.27,28 There are many reasons for these mixed findings; however, a major one is the tremendous variation in the pH of the actual sodium bicarbonate solution found in multiple-dose vials. Labels read that “the pH of this solution may range from 7.0 to 8.5.” Without knowledge of the precise pH of the buffer, it is impossible for the practitioner to guarantee a resulting pH of the local anesthetic solution of 7.4. When the pH of a lidocaine solution exceeds 7.6, a solid precipitate forms. In 2011, a stabilized solution of sodium bicarbonate was introduced into dentistry for use with lidocaine. The system, Onset (Onpharma, Inc), consists of a multiple-dose cartridge of sodium bicarbonate, a mixing pen, and a transfer adapter that allows a volume of sodium bicarbonate to enter the dental cartridge while simultaneously removing an equal volume of local anesthetic. The process takes less than 15 seconds, after which the now-buffered cartridge is placed in the syringe and the dental injection is administered.
In a small clinical trial (N = 18) comparing the onset of pulpal anesthesia following inferior alveolar nerve block of unbuffered lidocaine 2% with epinephrine 1:100,000 (pH ∼3.5) to that obtained with buffered lidocaine 2% with epinephrine 1:100,000 (pH 7.4), 71% of the patients achieved pulpal anesthesia (as determined by electric pulp testing) in under 2 minutes, compared with 12% with the unbuffered solution.29
Of the patients receiving the buffered local anesthetic solution, 44% rated their injection pain as “0,” compared with just 6% of patients who received the unbuffered solution using a visual analog scale (0 indicating “felt nothing” to 10 indicating “worst pain imaginable”).29 From the results of this small clinical trial, buffering local anesthetic solutions in this manner does appear to diminish the discomfort of injection and increase the speed of onset of profound anesthesia.
Novel Devices
Many patients feel that a good dentist should be able to administer profound local anesthesia comfortably. However, the fear and anxiety associated with local anesthetic administration can be challenging for the practitioner. There have been novel devices developed in this area that may aid in patient comfort.
The Single-Tooth Anesthesia System
This system (Milestone Scientific) is a computerized local anesthesia delivery system controlled by a foot pedal. It works by delivering local anesthetic at a constant pressure and controlled volume, regardless of the resistance in the tissues. A clinical study indicated that 48 of 50 dentists who volunteered to receive palatal injections with this system experienced a significant decrease in the level of discomfort, compared to the use of a traditional syringe for the identical injection. The operators also experienced reduced stress levels during administration of the palatal injection.30 This device is especially popular because of its efficacy in comfortably administering “single tooth anesthesia” into the PDL space. An additional difference of this system is that, compared to traditional methods of performing a PDL injection, which involve high pressure and low volume, it is a high-volume, low-pressure technique that leads to increased patient comfort.
The Comfort Control Syringe
This syringe (Dentsply) is an electronic preprogrammed anesthesia delivery device that uses a 2-stage delivery rate. The rate of injection varies based on the injection technique chosen. It begins with a slow rate; the flow then increases to a preprogrammed technique-specific rate selected by the dentist. The operation of this syringe (initiation and termination of the injection, controlled aspiration and flow rate) is controlled by a button on the handpiece. A disposable cartridge sheath is required for each patient, but a standard dental needle and anesthetic cartridge can be used with this device.
FUTURE DIRECTIONS
Where do we go next in the area of pain control in dentistry? We now have the ability to make local anesthetics work faster (buffering), to more rapidly reverse residual soft tissue anesthesia (phentolamine mesylate [Oraverse]),3 and to make injections more comfortable (eg, buffering, computer-controlled local anesthetic delivery systems such as The Wand and the Single-Tooth Anesthesia System).31
Intranasal Local Anesthesia
The major problem that remains is the patient's fear of the needle. Phase 3 clinical trials on the use of a nasal spray to provide pulpal anesthesia to maxillary teeth are ongoing at the time of writing (April 2012). The ability to provide pulpal anesthesia without the need for injection would be a significant improvement. Cocaine and tetracaine have been commonly used intranasally to provide anesthesia (both drugs) or vasoconstriction (cocaine only) prior to surgical procedures in otolaryngology in the extremely vascular nasal cavity or prior to passage of a tube through the nares (nasotracheal intubation). Other vasoconstrictors (phenylephrine, oxymetazoline) are frequently sprayed into the nasal cavity to relieve nasal congestion. Spraying a combination of tetracaine and oxymetazoline into the nares has been successful in providing pulpal anesthesia of the maxillary anterior teeth (incisors, canines, and premolars). Administered bilaterally in a phase 2 clinical trial (N = 48), profound pulpal anesthesia of 10 teeth was achieved with 100% success. Additionally, anesthesia of the maxillary first molars developed in 84% of patients.32 A control group received traditional injections of 2% lidocaine with 1:100,000 epinephrine and a 94% success rate was achieved from the first molar to the contralateral first molar.10 Given that fear of injection because of the fear of the needle is commonplace in dentistry, the ability to provide profound anesthesia without the need for injection appears to have a promising future.
Articaine by Mandibular Infiltration in Adults
The inferior alveolar nerve block, the injection technique that remains the “standard” when mandibular anesthesia is sought, is one of the most frustrating and least effective injections administered in dentistry.33 Difficulties in achieving reliable anesthesia in the mandible are related to: (1) the thickness of the cortical plate of bone in adults and (2) an inability to consistently locate the inferior alveolar nerve while it remains in soft tissue and before it enters (disappears) into the mandibular foramen. A recent review in the Journal of the American Dental Association34–36 considered the question, “Is the mandibular block passé?” Given its less-than-stellar success rate, numerous alternative techniques have been developed to help achieve mandibular anesthesia. These include the Gow-Gates mandibular nerve block, the Vazirani-Akinosi closed-mouth mandibular nerve block, the PDL injection (intraligamentary injection), and intraosseous anesthesia. These techniques were reviewed here.
In 2006 and 2007, independently conducted well-designed clinical trials were conducted to determine the efficacy of local anesthetics when administered by infiltration in the mandibles of adult patients. Primary comparisons were between 2% lidocaine and 4% articaine. Following infiltration of 2.2 mL37 or 1.8 mL38 in the buccal fold adjacent to the mandibular first molar, both investigators found that articaine with epinephrine was statistically superior to lidocaine with epinephrine in providing pulpal anesthesia to the first molar37 and second and first molars and to the second and first premolars.38 Other studies demonstrated the superiority of articaine to lidocaine by buccal infiltration, lingual infiltration, or buccal and lingual infiltration in the mandibular incisor region.39,40 However, to date there are no studies that demonstrate the superiority of articaine over any other local anesthetic when used in any of the mandibular blocks.
CONCLUSIONS
This paper is the second of a 2-part series on local anesthesia. Part 1 provided a review and update of essential pharmacology for the various local anesthetic formulations in current use. Technical considerations are addressed in this paper. We have discussed issues of importance to the safe and effective delivery of local anesthetics, including needle gauge; traditional, advanced, and alternative injection techniques; and techniques, devices, and agents to make the local anesthetic injection more comfortable for patients. We have examined current and future local anesthesia in dentistry, and it appears that the future is exciting and bright indeed.
CONTINUING EDUCATION QUESTIONS
-
1.
Which of the following statements is true concerning the gauge of needles?
-
A.
Needle gauge refers to the radius of the lumen of the needle.
-
B.
A 30-gauge needle has a larger internal diameter than a 25-gauge needle.
-
C.
The smaller the number, the greater the diameter of the lumen of the needle.
-
D.
27-gauge needles have the highest rate of deflection and breakage in dentistry.
-
2.
The term “trypanophobia” refers to the fear of which of the following?
-
A.
The dentist
-
B.
Needles
-
C.
The sound of the dental handpiece
-
D.
Radiographs
-
3.
What is the approximate pH of local anesthetic solutions without vasoconstrictors?
-
A.
3.5
-
B.
6.5
-
C.
7.4
-
D.
10
-
4.
Over 50% of medical emergencies occurring in a dental office occur following which procedure?
-
A.
Extraction
-
B.
Root canal therapy
-
C.
Periodontal surgery
-
D.
Local anesthetic administration
REFERENCES
- 1.de St. Georges J. How dentists are judged by patients. Dent Today. 2004 23:96, 98–99. [PubMed] [Google Scholar]
- 2.Malamed SF. Malamed SF. Handbook of Medical Emergencies. 6th ed. St Louis: The CV Mosby Co;; 2007. Introduction. In. 7. [Google Scholar]
- 3.Becker DE, Reed KL. Local Anesthetics: review of pharmacological considerations. Anesth. Prog. 2012;59:90–102. doi: 10.2344/0003-3006-59.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hamburg HL. Preliminary study of patient reaction to needle gauge. N Y State Dent J. 1972;38:425–426. [PubMed] [Google Scholar]
- 5.Fuller NP, Menke RA, Meyers WJ. Perception of pain to three different intraoral penetrations of needles. J Am Dent Assoc. 1979;99:822–824. doi: 10.14219/jada.archive.1979.0384. [DOI] [PubMed] [Google Scholar]
- 6.Lehtinen R. Penetration of 27- and 30-gauge needles. Int J Oral Surg. 1983;12:444–445. doi: 10.1016/s0300-9785(83)80036-2. [DOI] [PubMed] [Google Scholar]
- 7.Browbill JW, Walker PO, Bourcy BD, et al. Comparison of inferior dental nerve block injections in child patients using 30-gauge and 25-gauge short needles. Anesth Prog. 1987;34:215–219. [PMC free article] [PubMed] [Google Scholar]
- 8.Lipp MD. Local Anesthesia in Dentistry. Vol. 106 Chicago: Quintessence Publishing;; 1993. [Google Scholar]
- 9.Jeske AH, Blanton PL. Misconceptions involving dental local anesthesia. Part 2: Pharmacology. Tex Dent J. 2002;119:310–314. [PubMed] [Google Scholar]
- 10.Trapp LD, Davies RO. Aspiration as a function of hypodermic needle internal diameter in the in-vivo human upper limb. Anesth Prog. 1980;27:49–51. [PMC free article] [PubMed] [Google Scholar]
- 11.Delgado-Molina E, Tamarit-Borras M, Berini-Aytes L, et al. Evaluation and comparison of 2 needle models in terms of blood aspiration during truncal block of the inferior alveolar nerve. J Oral Maxillofac Surg. 2003;61:1011–1015. doi: 10.1016/s0278-2391(03)00312-4. [DOI] [PubMed] [Google Scholar]
- 12.Malamed SF, Reed KL, Poorsattar S. Needle breakage: incidence and prevention. Dent Clin North Am. 2010;54:745–756. doi: 10.1016/j.cden.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 13.Phillips WH. Anatomic considerations in local anesthesia. J Oral Surg. 1943;1:112–121. [Google Scholar]
- 14.Malamed SF. Handbook of Local Anesthesia. 5th ed. St Louis: The CV Mosby Co;; 2004. [Google Scholar]
- 15.Jastak JT, Yagiela JA. Regional Anesthesia of the Oral Cavity. St Louis: The CV Mosby Co;; 1981. [Google Scholar]
- 16.Evers H, Haegerstam G. Introduction to Dental Local Anesthesia. 2nd ed. St Louis: The CV Mosby Co;; 1990. [Google Scholar]
- 17.Watson JE. Appendix: some anatomic aspects of the Gow-Gates technique for mandibular anesthesia. Oral Surg Oral Med Oral Pathol. 1973;36:328–330. doi: 10.1016/0030-4220(73)90209-0. [DOI] [PubMed] [Google Scholar]
- 18.Reed KL. Advanced techniques of local anesthetic injection. Gen Dent. 1994;42:248–251. [PubMed] [Google Scholar]
- 19.Martin S, Jones J, Wynn B. Does warming local anesthetic reduce the pain of subcutaneous injection? Am J Emerg Med. 1996;14:10–12. doi: 10.1016/S0735-6757(96)90003-0. [DOI] [PubMed] [Google Scholar]
- 20.Bainbridge LC. Comparison of room temperature and body temperature local anesthetic solutions. Br J Plast Surg. 1991;44:147–148. doi: 10.1016/0007-1226(91)90050-t. [DOI] [PubMed] [Google Scholar]
- 21.Rood JP. The temperature of local anaesthetic solutions. J Dent. 1977;5:213–214. doi: 10.1016/0300-5712(77)90006-9. [DOI] [PubMed] [Google Scholar]
- 22.Oikarinen VJ, Ylipaavalniemi P, Evers H. Pain and temperature sensations related to local analgesia. Int J Oral Surg. 1975;4:151–156. doi: 10.1016/s0300-9785(75)80063-9. [DOI] [PubMed] [Google Scholar]
- 23.Meechan JG, Day PF. A comparison of intraoral injection discomfort produced by plain and epinephrine-containing lidocaine local anesthestic solutions: a randomized, double-blind, split-mouth, volunteer investigation. Anesth Prog. 2002;49:44–48. [PMC free article] [PubMed] [Google Scholar]
- 24.Malamed SF. Handbook of Local Anesthesia. 4th ed. St Louis: The CV Mosby Co;; 1997. [Google Scholar]
- 25.Bjerneroth G. Alkaline buffers for correction of metabolic acidosis during cardiopulmonary resuscitation with focus on Tribonat. Resuscitation. 1998;37:161–171. doi: 10.1016/s0300-9572(98)00051-3. [DOI] [PubMed] [Google Scholar]
- 26.Burns CA, Ferris G, Feng C, Cooper JZ, Brown MD. Decreasing the pain of local anesthesia: a prospective, double-blind comparison of buffered, premixed 1% lidocaine with epinephrine versus 1% lidocaine freshly mixed with epinephrine. J Am Acad Dermatol. 2006;54:128–131. doi: 10.1016/j.jaad.2005.06.043. [DOI] [PubMed] [Google Scholar]
- 27.Catchlove RFH. The influence of CO2 and pH on local anesthetic action. J Pharmacol Exp Ther. 1972;181:298–309. [PubMed] [Google Scholar]
- 28.Scarfone RJ, Jasani M, Gracely EJ. Pain of local anesthetics: rate of administration and buffering. Ann Emerg Med. 1998;31:36–40. doi: 10.1016/s0196-0644(98)70278-1. [DOI] [PubMed] [Google Scholar]
- 29.Malamed SF, Falkel M. Advances in local anesthetics: pH buffering and dissolved CO2. Dent Today. In press. [PubMed] [Google Scholar]
- 30.Hochman M, Chiarello D, Hochman CB, et al. Computerized local anesthetic delivery vs. traditional syringe. Subjective pain response. N Y State Dent J. 1997;64:24–29. [PubMed] [Google Scholar]
- 31.Hochman MN. Single-tooth anesthesia: pressure sensing technology provides innovative advancement in the field of dental local anesthesia. Compendium. 2007;28:186–193. [PubMed] [Google Scholar]
- 32.Ciancio S, Ayoub F, Pantera E, et al. Poster presentation at International Association for Dental Research (IADR) General Session, July 14–17. Nasal spray for anesthesia of maxillary teeth. 2010 Barcelona, Spain. [Google Scholar]
- 33.Malamed SF. Is the mandibular block passé? J Am Dent Assoc. 2011;142:3S–7S. doi: 10.14219/jada.archive.2011.0340. [DOI] [PubMed] [Google Scholar]
- 34.Haas DA. Alternative mandibular nerve block techniques: a review of the Gow-Gates and Akinosi-Vazirani closed-mouth mandibular nerve block techniques. J Am Dent Assoc. 2011;142:8S–12S. doi: 10.14219/jada.archive.2011.0341. [DOI] [PubMed] [Google Scholar]
- 35.Moore PA, Cuddy MA, Cooke MR, Sokolowski CJ. Periodontal ligament and intraosseous anesthetic injection techniques: alternatives to mandibular nerve blocks. J Am Dent Assoc. 2011;142:13S–18S. doi: 10.14219/jada.archive.2011.0342. [DOI] [PubMed] [Google Scholar]
- 36.Meechan JG. The use of the mandibular infiltration anesthetic technique in adults. J Am Dent Assoc. 2011;42:19S–26S. doi: 10.14219/jada.archive.2011.0343. [DOI] [PubMed] [Google Scholar]
- 37.Kanaa MD, Whitworth JM, Corbett IP, Meechan JG. Articaine and lidocaine mandibular buccal infiltration anesthesia: a prospective randomized double-blind cross-over study. J Endod. 2006;32:296–298. doi: 10.1016/j.joen.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 38.Robertson D, Nusstein J, Reader A, Beck M. The anesthetic efficacy of articaine in buccal infiltration of mandibular posterior teeth. J Am Dent Assoc. 2007;138:1104–1112. doi: 10.14219/jada.archive.2007.0324. [DOI] [PubMed] [Google Scholar]
- 39.Yonchak T, Reader A, Beck M, et al. Anesthetic efficacy of infiltrations in mandibular anterior teeth. Anesth Prog. 2001;48:55–60. [PMC free article] [PubMed] [Google Scholar]
- 40.Meechan JG, Ledvinka JI. Pulpal anesthesia for mandibular central incisor teeth: a comparison of infiltration and intraligamentary injections. Int Endod J. 2002;35:629–634. doi: 10.1046/j.1365-2591.2002.00532.x. [DOI] [PubMed] [Google Scholar]