Abstract
Purpose
Severe lower extremity trauma presents challenges in decision-making in terms of reconstruction or amputation. While injury severity scores have been developed to aid decision-making in adults, evaluation of their use in children is limited.
Methods
Children presenting with severe lower limb trauma from 2000 to 2010 in a major trauma centre were identified from a trauma registry. Records were reviewed for details of the injury, surgical intervention, amputation and scores for the Mangled Extremity Severity Score, Limb Salvage Index, Predictive Salvage Index, Nerve injury, Ischaemia, Soft tissue injury, Skeletal injury, Shock, Age System and the Hanover Fracture Scale 1998.
Results
Twenty children (average age 8.7 years) were eligible for inclusion. There were three primary amputations and no secondary amputations. All of the scoring systems had poor specificity and would have recommended amputation in several limbs that were successfully reconstructed.
Conclusions
Currently available injury severity scores behave differently in children and adults. In their current format, these scores should not be used as an absolute indication for early amputation in children.
Keywords: Limb trauma, Trauma score, Prognosis, Amputation, Reconstruction
Introduction
Severe lower extremity trauma can present a challenging decision to the treating surgeon. Controversy surrounds the management of the most severely injured limbs as misguided attempts at the reconstruction of a leg which is ultimately amputated result in significantly greater morbidity than primary amputation [1, 2].
Injury severity scoring systems have been developed for assessing adult lower limb trauma to help guide decision-making regarding reconstruction versus primary amputation. The Mangled Extremity Severity Score (MESS) [3], the Limb Salvage Index (LSI) [4], the Predictive Salvage Index (PSI) [5], the Nerve injury, Ischaemia, Soft tissue injury, Skeletal injury, Shock, Age system (NISSSA) [6], and the Hanover Fracture Scale 1998 (HFS-98) [7] have all been evaluated in adult trauma populations and describe a threshold score above which primary amputation is recommended. However, little data exist on the use of these scoring systems in a paediatric population. Only two studies have evaluated the application of the MESS score in children [8, 9].
As part of a study of lower limb trauma at our institution, we retrospectively applied all five of the aforementioned scoring systems to patients with severe lower extremity injury presenting to our major trauma centre over a 10-year period. The study was approved by the institution’s Ethics in Human Research Committee, approval number 31217A.
Materials and methods
Patients presenting with lower limb trauma over a 10-year period from July 2000 to July 2010 were identified from the hospital’s prospectively compiled trauma registry. Hospital records were reviewed for eligibility based on the inclusion and exclusion criteria summarised in Table 1. These criteria were chosen to be similar to the design of the multicentre Lower Extremity Assessment Project (LEAP), the largest prospective study of limb trauma in the literature [10].
Table 1.
Inclusion and exclusion criteria
| Criteria |
|---|
| Inclusion criteria |
| 1. Traumatic amputations of the lower limb |
| 2. Gustillo & Anderson grade IIIB and IIIC compound tibial fractures |
| 3. Gustillo & Anderson grade IIIA compound tibial fractures with: |
| a. >2 procedures |
| b. Severe muscle damage |
| c. Major bone loss |
| d. Major Nerve injury |
| 4. Dysvascular injuries (knee dislocations, divided popliteal artery etc.) |
| 5. Major Soft tissue injuries |
| a. AO IC3-IC5 degloving |
| b. Severe crush injuries with muscle disruption or compartment syndrome |
| 6. Severe foot injuries |
| a. Open IIIB ankle fractures |
| b. Severe hindfoot/midfoot injuries |
| c. Open grade 3 Pilon no. |
| Exclusion criteria |
| 1. Age >16 years at presentation or fused growth plates |
| 2. Impaired Glasgow Coma Scale at discharge |
| 3. Spinal cord injury |
| 4. Developmental delay |
Patient age, mechanism and surgical procedures were recorded, and the scores for the MESS, LSI, PSI, NISSSA and HFS-98 were calculated. Outcome (reconstruction or amputation) was compared to the predictions of the different trauma scores.
Trauma scores
Howe et al. [5] proposed the PSI in 1987 to assess patients with combined orthopaedic and vascular injuries. This index compiles scores for arterial, bony and muscle injury with a score for time from injury to surgery. Scores of ≥8 are recommended for primary amputation on the assumption that this represents a limb that will inevitably require amputation and, consequently, attempts at reconstruction are misguided. The MESS score was described by Johansen et al. in 1990. Scores for skeletal and soft tissue injury, ischaemia, shock and age are combined, and primary amputation is recommended with a score of ≥7. Due perhaps to its simplicity, the MESS is the most widely referenced lower extremity severity score [3]. The LSI was described in 1991 by Russell et al. [4], and the total score is composed of scores for arterial, deep venous, nervous, bony and muscular injuries, in addition to ischaemia. The amputation threshold score for the LSI is ≥6. In 1994 McNamara et al. [6] described the NISSSA score, which addresses nerve injury, ischaemia, soft tissue injury, skeletal injury, shock and age. The inclusion of nerve dysfunction was something the authors felt was lacking in the MESS. The threshold score for primary amputation with NISSSA is ≥11. The HFS-98 was published in 2001 as the latest modification of the Hanover fracture scale, developed to assess risk factors and complications in high-energy limb trauma. It evaluates bone loss, skin injury, muscle injury, wound contamination, periosteal stripping, local circulation, systemic circulation and nerve function [7]. The threshold score for amputation is ≥11.
Results
A total of 26 children were identified as eligible for the study. Two records had insufficient data to calculate the trauma scores, leaving 24 patients available for study. All patients were followed up for at least 1 year (range 1–8 years). There were two female and 22 male patients. The average age was 8.72 years (range 15 months to 15 years).
Mechanisms, sites of injury and trauma scores are summarised in Table 2. There were three primary amputations and no reconstructive failures, in that no patient who had undergone an attempt at reconstruction subsequently underwent secondary amputation.
Table 2.
Summary of scoresa for all patients
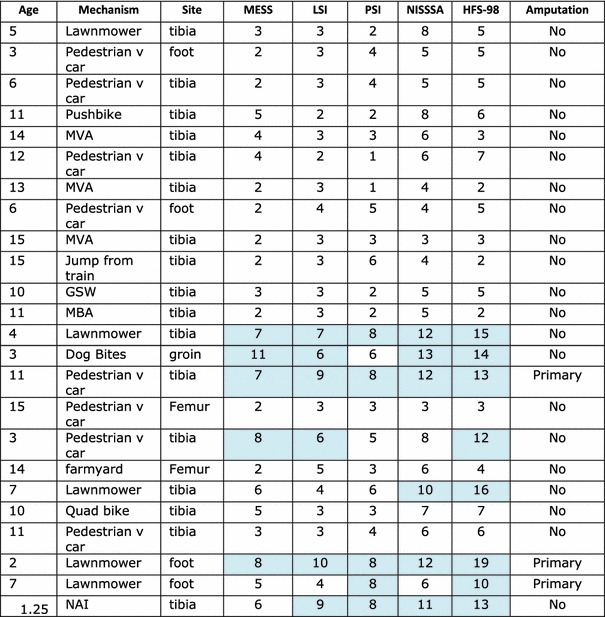
Shaded areas indicate scores at or above amputation threshold
MVA Motor vehicle accident, GSW gunshot wound, MBA motorbike accident, NAI non-accidental injury
aMESS The Mangled Extremity Severity Score,LSI the Limb Salvage Index,PSE the Predictive Salvage Index,NISSSA the Nerve injury, Ischaemia, Soft tissue injury, Skeletal injury, Shock, Age system,HFS-98 the Hanover Fracture Scale 1998. The different scores are described in “Trauma scores”
Sensitivity is the probability that limbs requiring amputation will have scores at or above the amputation threshold. This probability was calculated for each scoring system by dividing the number of patients having an amputation with a score at or above the threshold by the total number of amputations. Specificity is the probability that reconstructed limbs will have scores below the amputation threshold. This probability was calculated for each score by dividing the number of reconstructed limbs with scores below the threshold by the total number of patients with successful reconstruction. The sensitivity and specificity of all scoring systems are summarised in Table 3. Amputation decisions can sometimes be most challenging in tibial trauma, for which the NISSSA and HFS-98 were specifically designed. Therefore, sensitivities and specificities were calculated for the scoring systems in the 17 patients comprising the cohort of tibial trauma (Table 4).
Table 3.
Sensitivities and specificities of scoring systems applied to all patients
| Scoring system | Sensitivity (95 % CI) | Specificity (95 % CI) | Positive predictive value (%) | Negative predictive value (%) |
|---|---|---|---|---|
| MESS | 67 % (±19) | 86 % (±14) | 40 | 94.7 |
| LSI | 67 % (±19) | 81 % (±16) | 33.3 | 94.4 |
| PSI | 100 % | 90 % (±12) | 60 | 100 |
| NISSSA | 67 % (±19) | 81 % (±16) | 33.3 | 94.4 |
| HFS-98 | 100 % | 76 % (±17) | 37.5 | 100 |
CI Confidence interval
Table 4.
Scoring systems applied to patients with tibial trauma only
| Scoring system | Sensitivity (%) | Specificity (95 % CI) | Positive predictive value (%) | Negative predictive value (%) |
|---|---|---|---|---|
| MESS | 100 | 87 % (±16) | 33.3 | 100 |
| LSI | 100 | 81 % (±19) | 25 | 100 |
| PSI | 100 | 87 % (±16) | 33.3 | 100 |
| NISSSA | 100 | 81 % (±19) | 25 | 100 |
| HFS-98 | 100 | 71 % (±22) | 20 | 100 |
The positive predictive value is the proportion of positive test results that are ‘true positives’—in this case, the probability that a score above the amputation threshold reflects a true need for amputation. It is calculated by dividing the true positives (patients having an amputation with a score at or above the threshold) by the positive test results (number of patients scoring at or above the threshold). The negative predictive value is the likelihood that a score below the threshold represents a limb suitable for reconstruction. Positive and negative predictive values are given in Tables 3 and 4.
Discussion
Compared with their performance in adult trauma situations [11], the lower extremity injury severity scores performed differently in our paediatric cohort. There was a higher sensitivity for all scoring systems when compared to the analysis by Bosse et al. [11]. The PSI and the HFS-98 successfully predicted all three amputations and therefore had 100 % sensitivity. When applied to tibial trauma only, all scoring systems correctly identified the one patient requiring amputation. This higher sensitivity may reflect the fact that children have better results from reconstruction and therefore only the most severely injured limbs are amputated.
Most of the scoring systems had poorer specificity than previously described. The PSI achieved 90 % specificity when all patients were included in the analysis, falling to 87 % when only tibial trauma was considered. This specificity was greater than that shown when an adult population was considered.
Ideally a scoring system would have 100 % sensitivity and specificity, and the efficacy of less perfect systems depends on the relative weight given to each. While sensitivity is important so that futile attempts are not made to reconstruct a limb that will ultimately be amputated, higher specificity will avoid salvageable limbs being inappropriately removed. If using these scoring systems for decision-making regarding immediate amputation, between 10 and 14 % of all patients would undergo an avoidable amputation—according to our outcome data.
It has been suggested that in our era of microsurgery the MESS score should simply be updated by raising the amputation threshold, in recognition of the fact that more severely injured limbs are now suitable for reconstruction [12]. In our study, raising the MESS amputation threshold would not increase specificity and would also reduce sensitivity. Similarly, raising the threshold of the PSI would not increase specificity and would reduce sensitivity to zero. The specificity of the HFS-98 could be improved by raising the threshold to 13, but this would reduce overall sensitivity to 67 %. Both the LSI and the NISSSA could achieve improved specificity (95 and 90 %, respectively) by raising the amputation threshold while maintaining the 67 % sensitivity.
Severe limb trauma is rare in children, as reflected in our relatively low numbers over a 10-year period in a major trauma centre. The 95 % confidence intervals for our estimations of the sensitivity and specificity of the trauma scores are correspondingly wide. What this study highlights is that all of the scoring systems studied have a high degree of type 1 error or, if a score above the amputation threshold is taken as a ‘positive’ test for the need for amputation, a high false positive rate. This is illustrated in the low positive predictive values (PPV) of the scores. For example, the HFS-98 has a PPV of 37.5 %, reflecting the potential for five unnecessary amputations.
Compared to the analysis of MESS in children by Fagelman et al. [8], our study has a lower rate of amputation, possibly due to our study being conducted on patients managed from 2000 to 2010 whereas the previous study’s range was 1985–1995. Advances in reconstructive microsurgery have been considerable in the intervening years, and the use of free tissue transfer is more widespread. Mommsen et al. [9] investigated the use of MESS in children, specifically looking at vascular trauma. These authors gave guarded support to the use of MESS in children, achieving 100 % sensitivity but only 66 % specificity, comparable to our findings.
The low number of amputations in this study makes statistical analysis of the efficacy of scoring systems problematic. While we would advocate the attempted reconstruction of the majority of severely injured lower limbs in children given the greater chance of success, the eventual functional outcome is still unknown. A correlation of functional outcome with initial score would allow these scoring systems to be used as a prognostic tool if not for decision-making regarding amputation.
There are several intrinsic problems with the scoring systems when applied to children. The MESS and NISSSA both use age itself as a scoring criterion, thus making differentiation between paediatric patients impossible. MESS, NISSSA and HFS-98 also make use of an evaluation of shock. All three systems specify specific values for systolic blood pressure which are inappropriate in the light of normal values in children. Children are also known to respond differently to hypovolaemia, with hypotension being a later sign than in adults. If a scoring system was to be useful for functional prognosis, it would also need to include several injury specific factors unique to children, in particular damage to physeal cartilage.
Lower extremity injury severity scoring systems behave differently in children than in adults. Consequently, in their current format they should not be used as an absolute indication for early amputation given the lack of specificity and risk of unnecessary amputations of salvageable limbs. Inherent problems in applying the scoring systems mean that simple measures of modification, such as altering the amputation threshold, are not sufficient to make the available scoring systems a viable decision-making tool in the management of children with severe lower limb injuries.
Acknowledgements
The study was supported by the Leslie Eric Paddle Scholarship from the University of Melbourne. The authors would like to acknowledge the contribution of Mary Sheedy.
Conflict of interest
None.
References
- 1.Bosse MJ, MacKenzie EJ, Kellam JF, Burgess AR, Webb LX, Swiontkowski MF, et al. An analysis of outcomes of reconstruction or amputation after leg-threatening injuries. N Engl J Med. 2002;347(24):1924–1931. doi: 10.1056/NEJMoa012604. [DOI] [PubMed] [Google Scholar]
- 2.MacKenzie EJ. Long-term persistence of disability following severe lower-limb trauma. Results of a seven-year follow-up. J Bone Joint Surg. 2005;87A(8):1801–1809. doi: 10.2106/JBJS.E.00032. [DOI] [PubMed] [Google Scholar]
- 3.Johansen K, Daines M, Howey T, Helfet D, Hansen ST. Objective criteria accurately predict amputation following lower extremity trauma. J Trauma. 1990;30(5):568–572. doi: 10.1097/00005373-199005000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Russell WL, Sailors DM, Whittle TB, Fisher DF, Burns RP. Limb salvage versus traumatic amputation. A decision based on a seven-part predictive index. Ann Surg. 1991;213(5):473–480. doi: 10.1097/00000658-199105000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Howe HR, Poole GV, Hansen KJ, Clark T, Plonk GW, Koman LA, et al. Salvage of lower extremities following combined orthopedic and vascular trauma. A predictive salvage index. Am Surg. 1987;53(4):205–208. [PubMed] [Google Scholar]
- 6.McNamara MG, Heckman JD, Corley FG. Severe open fractures of the lower extremity: a retrospective evaluation of the Mangled Extremity Severity Score (MESS) J Orthop Trauma. 1994;8(2):81–87. doi: 10.1097/00005131-199404000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Seekamp A, Köntopp H, Tscherne H. Hannover Fracture Scale ‘98–reevaluation and new prospects for an established score system. Unfallchirurg. 2001;104(7):601–610. doi: 10.1007/s001130170090. [DOI] [PubMed] [Google Scholar]
- 8.Fagelman MF, Epps HR, Rang M. Mangled extremity severity score in children. J Pediatr Orthop. 2002;22(2):182–184. [PubMed] [Google Scholar]
- 9.Mommsen P, Zeckey C, Hildebrand F, Frink M, Khaladj N, Krettek C, Probst C. Traumatic arterial injury in children: epidemiology, diagnostics, treatment and prognostic value of Mangled Extremity Severity Score. J Orthop Surg Res. 2010;15(5):25. doi: 10.1186/1749-799X-5-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.MacKenzie EJ, Bosse MJ, Kellam JF, Burgess AR, Webb LX, Swiontkowski MF, et al. Characterization of patients with high-energy lower extremity trauma. J Orthop Trauma. 2000;14(7):455–466. doi: 10.1097/00005131-200009000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Bosse MJ, MacKenzie EJ, Kellam JF, Burgess AR, Webb LX, Swiontkowski MF, et al. A prospective evaluation of the clinical utility of the lower-extremity injury-severity scores. J Bone Joint Surg. 2001;83A(1):3–14. doi: 10.2106/00004623-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Lin CH, Wei FC, Levin LS. The functional outcome of lower extremity fractures with vascular injury. J Trauma. 1997;43:480–485. doi: 10.1097/00005373-199709000-00015. [DOI] [PubMed] [Google Scholar]


