Abstract
Purpose
A double osteotomy for correcting tibial deformity in combination with medial plateau elevation is recommended for the management of neglected Blount disease cases. We report our clinical experience with the application of this surgical technique and describe the long-term follow-up of the patients who were operated on.
Methods
During a 10-year period, eight children (8 boys) with mean age of 12 years (range 9–14 years) underwent surgery (9 operations) due to neglected infantile tibia vara. All patients suffered from stage V or VI Blount disease according to the Langenskiold and Riska classification. Two simultaneous combined osteotomies were performed for medial plateau elevation and for correction of the tibial deformity. The correction was immediate using K-wires for stabilization and a long-leg cast for immobilization. The mean duration of follow-up was 10 years (range 5–15 years), and the evaluations were based on clinical and radiological criteria.
Results
At the latest follow-up, there was no observable knee flexion or extension restriction and no signs of instability or lateral thrust. All patients had returned to a higher activity level. Leg-lengthening surgery was performed in one child, but the length discrepancy was already present before the double osteotomy was performed. No other complications were noticed. All the angles measured on X-rays had been corrected, and this correction was retained until the latest follow-up.
Conclusions
This method results in very good outcomes in patients who suffer from Blount disease of stage V or greater. With this technique, the tibial deformity is corrected, the articular surface is restored, and future recurrence is prevented.
Keywords: Neglected Blount disease, Tibia vara, Tibial plateau elevation, Pediatric knee, Double osteotomy
Introduction
Blount published his classical article on what is now known as Blount disease in 1937 [1], and it has since become a well-studied entity. This entity has two different types; the infantile or early onset form which appears before the age of 3 years and the adolescence or late onset form which appears in children older than 10 years [2]. When the infantile disease is not managed early, the varus and the internal torsion of the tibia are accompanied by depression of the medial tibial plateau [3–6]. In 1964, Langenskiold and Riska proposed elevating the medial plateau for cases of infantile Blount disease that presented late [3]. The indication for this additional procedure is the significant incongruity of the joint surface due to depression of the medial part of the tibial plateau [2]. This technique has been studied, evaluated, and modified in the intervening time since first being proposed [7–12]. In addition to the medial plateau elevation, the varus of the tibia is now corrected by a valgus tibia osteotomy, either simultaneously or in a separate operation. The term “double elevating osteotomy” was proposed by Gregosiewicz et al. who used the bony wedge removed from the tibial valgus osteotomy to support the medial plateau elevation [10].
The etiology of this disease remains unknown. However, the varus deformity is probably the reason why the normal enchondral ossification is disrupted in the medial aspect of the metaphysis and growth is defective in the medial part of the physis [2, 3, 6]. The mechanical regulation of the physis is often referred as the “Hueter-Volkmann Law,” which dictates that the longitudinal growth from the growth plates of long bones is retarded by increased compression forces and stimulated by increased distraction forces across the growth plate [13]. In late onset Blount’s disease, the inhibition of growth may result in premature medial physeal arrest [7], which basically accounts for the success of a single valgus osteotomy for the management of the most early onset cases (60–75 %) and its lack of efficacy in cases of children with the late onset form. In these latter cases, repeated osteotomies are needed in the majority of the children (60–65 %) [4, 6].
The aim of this study is to report our clinical experience with the application of this surgical technique and to describe the long-term follow-up of the patients who were operated on.
Materials and methods
During a 10-year period (1995–2004), eight children (8 boys) with a mean age of 12 years (range 9–14 years) were operated on due to neglected infantile tibia vara. Nine operations were performed because one child had been affected bilaterally. The time interval between the operations for the bilateral case was 6 months. All patients suffered from stage V or VI Blount disease according to Langenskiold and Riska classification. Patients’ data are presented in Table 1. Two osteotomies was performed simultaneously in every case: one for medial plateau elevation combined with the insert of bone graft and one for the correction of tibial deformity. Both osteotomies were performed using the technique described below, and the operations were performed by the same experienced surgeon (A.G.). The mean follow-up was 10 years (range 5–15 years). The correction of varus, the presence of leg length discrepancy, and the stability and range of motion of the knee joint were evaluated clinically. Pain was measured on the visual analog scale from 0 (no pain) to 10 (worst pain ever experienced). A questionnaire consisting of 20 questions in four categories (general satisfaction, mobility, sports activity, happiness) was used to rate patients’ satisfaction and subjective opinion concerning their quality of life. The design of the questionnaire was based on the Pediatric Outcomes Data Collection Instrument (PODCI), which has been developed by the following societies: American Academy of Orthopaedic Surgeons, Pediatric Orthopaedic Society of North America, American Academy of Pediatrics, and Shriner’s Hospitals [14]. For each question, each young patient is asked to select the most accurate response from five options, ranging from “very happy” to “very unhappy”. In terms of radiological criteria, the same radiological views (face and profile) were taken pre-operatively, immediately postoperatively, and at the latest follow-up. All views were obtained in the standing position. The angle between the tibial and the femoral shaft, the angle between femoral condyles and the tibial shaft, and the angle of the medial tibial plateau depression were assessed (Fig. 1) and compared (pre-operatively vs. the latest follow-up). For the evaluation of the correction of the mechanical axis, two weight-bearing full-length anteroposterior (AP) radiographs of both lower extremities were taken (providing the proper protection to young patients), the first pre-operatively and the second 6 weeks postoperatively after plaster removal.
Table 1.
Patients’ data
| Case no. | Age (years) | Gradea | Follow-up (years) | Angles measured (degrees) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Between tibial and femoral shaftb | Between femoral condyles and tibial shaft | Medial tibial plateau depression | |||||||
| Pre-operation | Latest follow-up | Pre-operation | Latest follow-up | Pre-operation | Latest follow-up | ||||
| 1 | 14 | VI | 15 | 32 | 2 | 57 | 86 | 40 | 9 |
| 2 | 12 | V | 14 | 28 | −5 | 64 | 84 | 39 | 2 |
| 3 | 13 | VI | 12 | 27 | −1 | 47 | 74 | 54 | 18 |
| 4 | 12 | VI | 11 | 42 | −4 | 52 | 87 | 49 | 6 |
| 5 | 12 | VI | 9 | 28 | −8 | 56 | 85 | 60 | 22 |
| 6 | 9 | V | 9 | 25 | −4 | 49 | 87 | 30 | 6 |
| 7 | 13 | VI | 6 | 33 | −1 | 51 | 83 | 44 | 7 |
| 8 | 11 | V | 6 | 29 | 2 | 70 | 92 | 45 | 6 |
| 9 | 12 | V | 5 | 34 | −1 | 53 | 82 | 50 | 9 |
aAccording Langenskiold and Riska classification [3]
bNegative values indicate valgus, positive values indicate varus
Fig. 1.
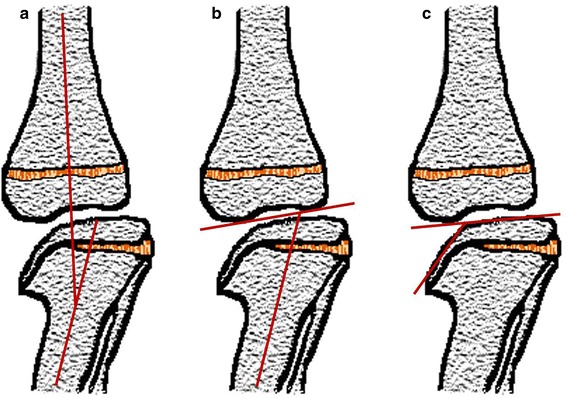
Angles measured on X-rays. a The angle between the tibial and the femoral shaft, b the angle between femoral condyles and the tibial shaft, c the angle of medial tibial plateau depression
Surgical technique
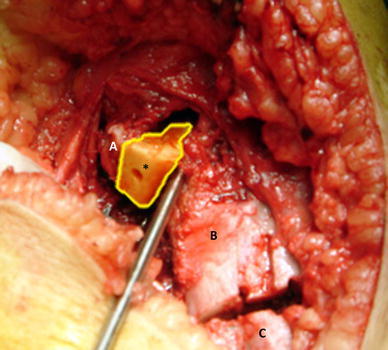
Under general anesthesia with the use of tourniquet, a mid to distal fibular osteotomy (1–2 cm) is made through a lateral incision. Both tibial osteotomies are performed through the same anteromedial curved incision (Fig. 2). A wedge-shaped osteotomy is initially performed about 5 cm distally of the tibial joint line, below the tibial tuberosity (Fig. 3a). A bony wedge is removed for correcting the varus and the internal torsion of the tibia. Overcorrection up to 5–10 degrees of valgus is addressed for reducing the pressure of the medial physis in order to avoid recurrences. Fixation is achieved by staples, K-wires, and plates, but other more sophisticated devices can be used. The second osteotomy for the medial plateau elevation is made just below the “beak” that is formed under image intensifier control (Fig. 4). A wide chisel is used to target the indercondylar area without crossing the articular cartilage (Fig. 3b). Special care is taken for the cut to be parallel to the physis. If a bony bridge has been formed, it is totally removed. During osteotomy, the knee is in flexion for minimizing the risk of provoking neurovascular damage. Thus, a fracture is provoked in the non-weight-bearing indercondylar area and the medial tibial plateau is mobilized. Thereafter, both the bony wedge removed from the first osteotomy and the excised fibula are used as a strut for supporting the new medial plateau position with respect to the continuity of the articular surface (Figs. 3c, 5). Kirschner wires are used for stabilizing and anchoring the interposed bony material. Eventually, the layers of surgical wounds are closed, and a long-leg cast (Plaster of Paris) is used for immobilization. Care is taken to avoid closing the fascia too tightly for the prevention of compartment syndrome.
Fig. 2.

Both tibial osteotomies are performed through the same anteromedial curved incision. The proximal osteotomy is made for medial plateau elevation and is combined with the distal osteotomy for correcting the varus and the internal torsion of the tibia.A Proximal part of proximal osteotomy,B distal part of proximal osteotomy,C proximal part of distal osteotomy,D distal part of distal osteotomy
Fig. 3.
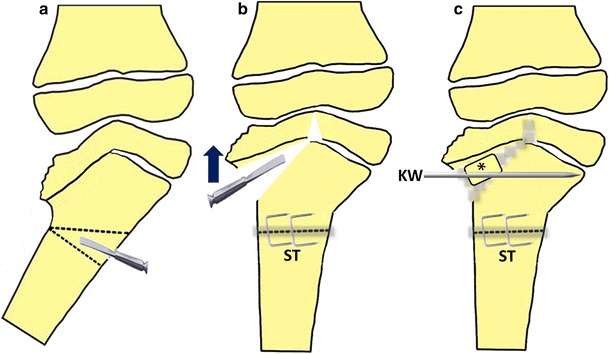
Drawing of surgical technique applied. a Distal wedge-shaped osteotomy, b proximal osteotomy for medial plateau elevation, c bony wedge removed from the first osteotomy and/or the excised part of fibula are used as a strut for supporting the new medial plateau position with respect to the continuity of the articular surface. A Kirschner wire is used for stabilization of the interposed bony material. ST Staples, KW Kirschner wire,asterisk strut graft
Fig. 4.

The osteotomy for the medial plateau elevation is made just below the “beak” that has been formed under image intensifier control with a wide chisel, targeting the indercondylar area without crossing the articular cartilage
Fig. 5.
The bony wedge removed from the distal osteotomy us used as a strut for supporting the new medial plateau position.A Proximal part of proximal osteotomy,B distal part of proximal osteotomy,C proximal part of distal osteotomy,D distal part of distal osteotomy
Rehabilitation protocol
The rehabilitation protocol consisted of mobilizing the patients without weight bearing starting from the first post-operative day. Strengthening exercises for quadriceps and hamstrings were performed. The cast was removed after 6 weeks, when partial weight bearing was allowed; full weight bearing was allowed after 10–12 weeks.
Results
During the latest follow-up, we observed no knee flexion or extension restriction, and no signs of instability (neither AP nor mediolateral) were observed during the clinical evaluation. The varus deformation was corrected to neutral or to slight valgus in seven knees, but two of the nine knees were in slight varus of 2 degrees (Table 1). In comparison to their per-operative state, all of the young patients referred to a notable improvement in their gait and a return to a higher activity level. Based on the patients’ answers to the questionnaire, these were the two factors explaining their satisfaction and improvement in their life quality, while the cosmetic result was the third (Figs. 6–8). Even if pain is not a dominant complaint in this entity, improvement in pain relative to the pre-operative assessment was noted whether it was assessed prospectively or retrospectively. In terms of walking, no patient was observed with lateral thrust nor did any patient have a leg-length discrepancy of >1 cm. In one child leg lengthening had been performed in a separate operation, 3 years after the double osteotomy. This child had a leg-length discrepancy of 3 cm prior to the double osteotomy due to coexisting pathology, and the amount of lengthening was 6 cm. No other short-term or long-term complication was observed.
Fig. 7.

Clinical appearance and radiological evaluation 1 year postoperatively of the same patient shown in Fig. 4. X-rays show incomplete correction of the proximal tibia deformity with compensation by the associated distal femoral valgus, but the clinical appearance is more impressive
Fig. 6.
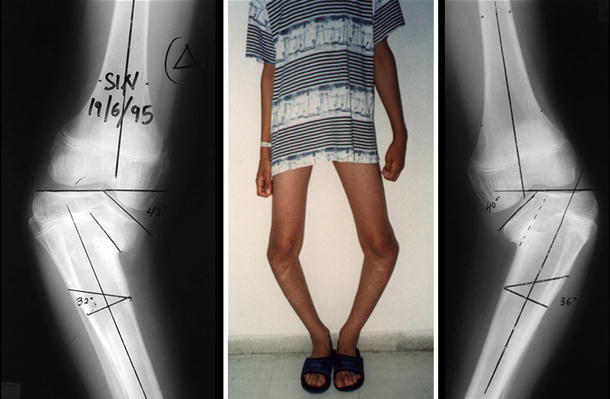
Pre-operative photo of a 13-year-old boy with bilateral Blount disease and radiological evaluation of both knees. This child had been operated bilaterally with single osteotomies but the deformity relapsed
Fig. 8.

Left Pre-operative photo and radiological evaluation of a 14-year-old boy with unilateral Blount disease. Right Clinical appearance and radiological evaluation 6 years postoperatively
With respect to the radiological findings (Table 2), the mean angle between the tibial and the femoral shaft was corrected from 31 degrees of varus (range 25–42 degrees) pre-operatively to 2 degrees of valgus (range 2–8 degrees) at the latest follow-up. The mean angle between the femoral condyles and the tibial shaft was corrected from 55 degrees pre-operatively (range 47–70 degrees) to 84 degrees at the latest follow-up (range 74–92 degrees). Eventually, the mean angle of the medial tibial plateau depression was corrected from 46 degrees (range 30–60 degrees) preoperatively to 10 degrees (range 2–22 degrees) at the latest follow-up (Figs. 6–8).
Table 2.
Radiological parameters measured
| Radiological parameter | Pre-operative mean value (range) | Last follow-up mean value (range) |
|---|---|---|
| Angle between tibial and femoral shaft | 31 (25–42) | −2 (−8 to 2)a |
| Angle between femoral condyles and tibial shaft | 55 (47–70) | 84 (74–92) |
| Angle of medial tibial plateau depression | 46 (30–60) | 10 (2–22) |
aNegative values indicate valgus while positive values indicate varus
Discussion
Patients suffering from Blount disease should be managed operatively as soon as the entity is diagnosed because deformities are aggravated when the condition is left untreated [4, 11]. However, even with early management, varus recurs in 55 % of the cases [2, 4]. In these cases, a tibial valgus osteotomy is not adequate for correcting the deformity, and additional elevation of the depressed tibial plateau is required. The term “double elevating osteotomy” that originated from Gregosiewicz et al. [10] is not accurate since elevation characterizes only the osteotomy of the medial plateau, as van Huyssteen et al. also pinpoint in their article [12]. The other type of osteotomy is a valgus osteotomy (wedge, dome) of the tibial shaft. Thus, the term “double corrective osteotomy of the tibia with medial plateau elevation” more accurately describes this procedure.
The bony wedge removed from the valgus wedge osteotomy or/and tricortical iliac graft can be used to support the elevated medial plateau. In our series, the bony fragment removed from the precedent fibula osteotomy was also used. Slight overcorrection (5–10 degrees of valgus) should be addressed for avoiding recurrences. Adequate fixation can be achieved with a horizontally placed Kirschner wire, while the distal osteotomy can be fixed with two crossed Steinmann pins, staples, or plates. The limb should be immobilized with a long-leg cast until the osteotomies are healed. These materials were available during the period that our patients were operated on, and given the successful outcome such materials can be considered to be appropriate during periods of economic crisis when more expensive devices are not available. Other internal or external fixation materials can be used, depending on availability and/or surgeon’s preferences.
The use of the Ilizarov Frame [15–17], the Taylor Spatial Frame [18–20], and a Multi-Axial Correction external fixation system [21] are modern therapeutical options, although significantly more expensive than our procedure. These systems enable gradual correction [20], in contrast to our cases, for whom correction was imminent. Using these techniques weight bearing is allowed throughout the entire period of treatment. The advantages of these systems are the potential correction of multiplane deformities and simultaneous leg lengthening. However, as Jones et al. report they are more complicated and time-consuming treatment strategies, they depend on the cooperation of the patients and their parents, attention must be paid to avoiding premature consolidation of the proximal osteotomy, and daily care is required to avoid pin-site infection [15, 22]. More specifically, Jones et al. also report that in their study premature consolidation of the elevation osteotomy occurred in three of seven patients. In the same article, 100 % of the patients had problems with pin-site infection. The high incidence of this complication has been confirmed by other authors [16, 17, 19, 23].
Leg lengthening was required in one of our cases, but the discrepancy existed before the double corrective osteotomy. No other patient had a leg-length discrepancy of >1 cm. In bilateral cases, leg-length discrepancy is not usually a problem. In unilateral cases, if the patient had an operation close to the age of skeletal maturity, no intense problem of leg-length discrepancy should be expected. Considering that the maximum acceptable shortening of a limb is 6 cm [24], the minimum skeletal age for the operation is 7 years for girls and 8 years for boys, based on the relative growth charts [25].
Some authors report that concomitant epiphysiodesis of the lateral part of the proximal tibial physis should be performed [3, 9, 11, 12], but this should not be viewed as a routine procedure. Specifically, when the operation is performed close to skeletal maturity, children can successfully undergo the surgery without re-establishing varus. All potential problems and their solutions should be considered by the pediatric orthopaedic surgeon and should be performed individually as needed, since the more complicated an operation, the higher the complication’s rate. In addition, cases with neglected Blount disease are characterized by multiple and complicated deformities. Thus, a detailed individualized pre-operative plan should be designed for each patient; regular follow-up is mandatory. It is the experienced pediatric orthopaedic surgeon who will decide if any intervention is required.
The subjective surgical outcome of this procedure is combined with patient’s satisfaction, which is turn is based on the combination of three parameters: improvement in patient’s gait, ability to participate in activities at a higher level, and the cosmetic result. Among our patients, even those with remaining varus deformity were satisfied with the operative results due to the upgrading of these three parameters. It is remarkable that even if pain is not a dominant complain in this entity, improvement was noticed between pre-operative and postoperative assessments. This improvement was greater when patients asked to remember and rate their pre-operative status during the latest follow-up, revealing their level of satisfaction. This observation supports the results of the study of Jones et al. that the correction of the angles measured shows a significant correlation with patient’s pain score and satisfaction score [23].
The methodology of this study has several limitations. First, only a small number of cases were available for analysis. Patients with neglected cases of tibia vara fortunately do not present often due to proper management and thorough follow-up in earlier stages of the condition. Secondly, our study was retrospective in nature. The use of several different fixation devices, as well as a non-standard one, did not allow a comparison between the devices in order to determine the proper fixation device. Moreover, the correction of the plateau depression in our cases was imminent. Thus, we were unable to compare our approach with techniques that allow gradual correction. For a proper comparison, prospective trials in which patients with tibia vara would be randomly assigned to each fixation group should be performed. Due to the retrospective nature of our study, various results, such as the IKDC score, answers to quality-of-life questionnaires, magnetic resonance imaging scans, or gait analysis, were not available for all of the patients. Studies with a prospective design would be able to obtain these data at onset, providing further information for comparison.
In summary, the management of neglected cases of infantile Blount disease requires both varus correction and medial plateau elevation. It is a very demanding procedure and a relatively high-risk operation. Despite the technical difficulties, it achieves a very good outcome in patients who suffer from Blount disease of stage V or greater according to the Langenskiold and Riska classification. With this technique the deformity is corrected, the articular surface is restored, and future recurrence can be prevented. However, extra care should be taken postoperatively to avoid injury of the adjacent neurovascular structures that could provoke serious complications. Our experience from the management and the long-time follow-up of patients who suffered from this entity indicate our surgical technique as a reliable solution for the management of similar cases.
Conflict of interest
None.
Contributor Information
Andreas Gkiokas, Email: chrisan1@otenet.gr.
Emmanuel Brilakis, Phone: +30-69-73717069, Email: emmanuel.brilakis@gmail.com.
References
- 1.Blount WP. Tibia Vara. Osteochondrosis deformans tibiae. J Bone Joint Surg Am. 1937;19:1–29. [Google Scholar]
- 2.Herring JA. Tachdjian’s pediatric orthopaedics. Philadelphia: Saunders Elsevier; 2008. [Google Scholar]
- 3.Langenskiöld A, Riska EB. Tibia vara (osteochondrosis deformans tibiae): a survey of seventy-one cases. J Bone Joint Surg Am. 1964;46:1405–1420. [PubMed] [Google Scholar]
- 4.Loder RT, Johnston CE., 2nd Infantile tibia vara. J Pediatr Orthop. 1987;7:639–646. doi: 10.1097/01241398-198707060-00002. [DOI] [PubMed] [Google Scholar]
- 5.Hofmann A, Jones RE, Herring JA. Blount’s disease after skeletal maturity. J Bone Joint Surg Am. 1982;64:1004–1009. [PubMed] [Google Scholar]
- 6.Doyle BS, Volk AG, Smith CF. Infantile Blount disease: long-term follow-up of surgically treated patients at skeletal maturity. J Pediatr Orthop. 1996;16:469–476. doi: 10.1097/01241398-199607000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Siffert RS. Intraepiphyseal osteotomy for progressive tibia vara: case report and rationale of management. J Pediatr Orthop. 1982;2:81–85. doi: 10.1097/01241398-198202010-00012. [DOI] [PubMed] [Google Scholar]
- 8.Støren H. Operative elevation of the medial tibial joint surface in Blount’s disease. One case observed for 18 years after operation. Acta Orthop Scand. 1969;40(6):788–796. doi: 10.3109/17453676908989543. [DOI] [PubMed] [Google Scholar]
- 9.Sasaki T, Yagi T, Monji J, Yasuda K, Kanno Y. Transepiphyseal plate osteotomy for severe tibia varus in children: follow-up study of four cases. J Pediatr Orthop. 1986;6:61–65. doi: 10.1097/01241398-198601000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Gregosiewicz A, Wosko I, Kandzierski G, Drabik Z. Double-elevating osteotomy of tibiae in the treatment of severe cases of Blount’s disease. J Pediatr Orthop. 1989;9:178–181. [PubMed] [Google Scholar]
- 11.Schoenecker PL, Johnston R, Rich MM, Capelli AM. Elevation of the medial plateau of the tibia in the treatment of Blount disease. J Bone Joint Surg Am. 1992;74:351–358. [PubMed] [Google Scholar]
- 12.Van Huyssteen AL, Hastings CJ, Olesak M, Hoffman EB. Double-elevating osteotomy for late-presenting infantile Blount’s disease: the importance of concomitant lateral epiphysiodesis. J Bone Joint Surg Br. 2005;87(5):710–715. doi: 10.1302/0301-620X.87B5.15473. [DOI] [PubMed] [Google Scholar]
- 13.Stokes IA. Mechanical effects on skeletal growth. J Musculoskelet Neuronal Interact. 2002;2(3):277–280. [PubMed] [Google Scholar]
- 14.American Academy of Orthopaedic Surgeons, Pediatric Orthopaedic Society of North America, American Academy of Pediatrics, Shriner’s Hospitals (2005) Adolescent (self reported) Outcomes Questionnaire. Available in: http://www.aaos.org/research/outcomes/Adolescent_Self.pdf. Revised, renumbered, reformatted: Aug 2005
- 15.Jones S, Hosalkar HS, Hill RA, Hartley J. Relapsed infantile Blount’s disease treated by hemiplateau elevation using the Ilizarov frame. J Bone Joint Surg Br. 2003;85:565–571. doi: 10.1302/0301-620X.85B4.13602. [DOI] [PubMed] [Google Scholar]
- 16.Hefny H, Shalaby H. A safer technique for the double elevation osteotomy in severe infantile tibia vara. Strategies Trauma Limb Reconstr. 2010;5(2):79–85. doi: 10.1007/s11751-010-0088-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hefny H, Shalaby H, El-Kawy S, Thakeb M, Elmoatasem E. A new double elevating osteotomy in management of severe neglected infantile tibia vara using the Ilizarov technique. J Pediatr Orthop. 2006;26(2):233–237. doi: 10.1097/01.bpo.0000218530.59233.ab. [DOI] [PubMed] [Google Scholar]
- 18.Bar-On E, Weigl DM, Becker T, Katz K. Treatment of severe early onset Blount’s disease by an intra-articular and a metaphyseal osteotomy using the Taylor Spatial Frame. J Child Orthop. 2008;2(6):457–461. doi: 10.1007/s11832-008-0140-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eidelman M, Bialik V, Katzman A. The use of the Taylor spatial frame in adolescent Blount’s disease: is fibular osteotomy necessary? J Child Orthop. 2008;2(3):199–204. doi: 10.1007/s11832-008-0099-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Feldman DS, Madan SS, Ruchelsman DE, Sala DA, Lehman WB. Accuracy of correction of tibia vara: acute versus gradual correction. J Pediatr Orthop. 2006;26:794–798. doi: 10.1097/01.bpo.0000242375.64854.3d. [DOI] [PubMed] [Google Scholar]
- 21.Pandya NK, Clarke SE, McCarthy JJ, Horn BD, Hosalkar HS. Correction of Blount’s disease by a multi-axial external fixation system. J Child Orthop. 2009;3(4):291–299. doi: 10.1007/s11832-009-0172-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Accadbled F, Laville JM, Harper L. One-step treatment for evolved Blount’s disease: four cases and review of the literature. J Pediatr Orthop. 2003;23:747–752. doi: 10.1097/01241398-200311000-00012. [DOI] [PubMed] [Google Scholar]
- 23.Jones JK, Gill L, John M, Goddard M, Hambleton IR. Outcome analysis of surgery for Blount disease. J Pediatr Orthop. 2009;29(7):730–735. doi: 10.1097/BPO.0b013e3181b768d9. [DOI] [PubMed] [Google Scholar]
- 24.Moseley CF. Leg length discrepancy. In: Morrissey RT, Weinstein SL, editors. Lovell and winter’s paediatric orthopaedics. Philadelphia: Lippincott Williams & Wilkins; 2001. pp. 1105–1150. [Google Scholar]
- 25.Anderson M, Green WT, Messner MB. Growth and predictions of growth in the lower extremities. J Bone Joint Surg Am. 1963;45(1):1–14. [PubMed] [Google Scholar]


