Abstract
Objective: The purpose of this study was to measure the kinematics of the lower limbs of Chinese people during normal kneeling activity, as such data could be valuable in designing joint prosthesis and arthroplasty that meet the needs of Chinese citizens’ daily activities. Methods: Thirty young and twenty elderly Chinese participants with no personal history of joint diseases were recruited, and matched by age (average age: 23.8 years for the young group, 60.8 years for the elderly group). Each participant performed six trials during which three-dimensional (3D) kinematics data were collected and the means of the 3D angles of the ankle, knee, and hip joints of two groups were calculated. Results: There were no obvious differences between the two groups in the knee and ankle joints. The mean range of knee flexion was 139.6° for the young group and 140.9° for the elderly group. The mean range of ankle flexion was 35.7° for the young group and 37.6° for the elderly group. The maximal eccentric flexion at the hip joint was 67.5° for the young group compared to 100.5° for the elderly group. Conclusions: The elderly uses more hip flexion angles than the young when assuming the kneeling posture. The ranges of motion obtained during kneeling activity are greater than the reported mean ranges of motion achieved following joint arthroplasty. The data could be valuable in establishing criteria for lower limb prosthetics and rehabilitation protocol for the Chinese population.
Keywords: Joint angle, Kneeling, Kinematics, Chinese people
1. Introduction
The population of China exceeds one billion people. Certain lifestyle choice requires the Chinese to utilize a higher range of motion (ROM) than what is typically required in Western populations. In fact, Ahlberg et al. (1988) demonstrated the diversity of joint ROM across cultural groups. For example, kneeling is among the most commonly assumed postures by the Chinese for traditional ceremonies, particularly by Buddhists during prayer (there are a great number of Buddhists living in China today). However, the commonly used joint arthroplasty designed by the West does not account for persistent kneeling activity. Therefore, it is necessary to research whether the joint arthroplasty would be able to meet the lifestyle requirements of Chinese patients.
The joint arthroplasty is designed to help patients to return to an active state, so it is necessary to obtain the kinematics of joint motion of the general population, in order to meet the specific needs of patients. Although some studies have examined joint motion in kneeling activity (Mulholland and Wyss, 2001), there have been few studies which have assessed kinematics of the knee, hip, and ankle joints simultaneously, and even fewer studies looking at the kinematics of kneeling activity at these joints in the three axial planes (Hemmerich et al., 2006). To our knowledge, most studies have solely focused on kneeling activity at the knee joint (Ahlberg et al., 1988; Baltzopoulos, 1995; Hefzy et al., 1998; Nakagawa et al., 2000; Kanekasu et al., 2004; Moro-Oka et al., 2008), and the kinematics of knee having total knee arthroplasty (Coughlin et al., 2007; Hamai et al., 2008; Nakamura et al., 2010). These studies have been used to improve the design of the joint arthroplasty; however, there are insufficient data for all three lower extremity joints to support the joint prosthesis design.
In this study, we presented the ROM of hip, knee, and ankle joints during kneeling activity in healthy Chinese adults (young and old). Furthermore, we compared the kinematics of three joints of the younger adults with that of the older adults. This research identified the necessary requirements for the joint arthroplasty to carry out this activity, and clarified whether the joint arthroplasty is safe in practice. This research is a part of a series of biomechanical investigations designed for the joint arthroplasty suited to Chinese populations.
2. Materials and methods
Fifty healthy Chinese participants were recruited. The sample was comprised of 25 males and 25 females. They were further subdivided into the young group (≤30 years) and the elderly group (≥60 years). The young group included 15 males and 15 females, while the elderly group was comprised of 10 males and 10 females. The characteristics of the participants are presented in Table 1. Most of the participants were recruited from the staff and students of Shanghai Jiao Tong University, China, and the elderly participants were recruited from outside the University. All participants have lived Chinese lifestyle, and had no history of injury or pain to the lower limbs, any type of lower extremity surgery, neuromuscular disease, or balance problems. The study was approved by the ethics committee of Shanghai Jiao Tong University and all participants signed a consent form before participating. This study was carried out in the Laboratory of Biomedical Manufacturing and Life Quality Engineering of Shanghai Jiao Tong University, China.
Table 1.
Participants’ parameters
| Group | Height (cm) | Mass (kg) | Age (year) |
| Young | 166.86±6.89 | 57.18±9.04 | 23.83±1.64 |
| Elderly | 163.45±8.39 | 62.37±9.34 | 60.75±2.51 |
Data are expressed as mean±standard (SD)
Prior to data collection, all participants performed various activities on a special gait test platform which is 15 cm in height. Kinematic recordings were collected by the Optotrak® Certus™ 3020 three-imensional (3D) active tracking system (Northern Digital Inc., Waterloo, Canada). The 3D accuracy was 0.15 mm, and the resolution was set to 0.01 mm. In order to gain a more effective detect range, we used three Optotrak 3020 position sensors. Because the sampling rate decreased when tracking markers increased, 95 Hz is the highest frequency that the tracking system can achieve when 48 tracking markers are used. Thus, the motion data was collected at a sampling rate of 95 Hz.
In order to achieve clear results, all participants wore shorts to allow for secure attachment of the tracking rigid plates onto the skin of the body. Seven optical tracking rigid plates were used to capture the 3D coordinate, each one of which consisted of four non-collinear infrared markers. These rigid plates were placed on feet (bilateral instep), shanks (bilateral surface of tibia), thighs (bilateral surface of the thigh, below hand swing), and pelvis (over the center point between both posterior superior iliac spines). Rigid plates were firmly attached to the lateral surface of the participant’s foot, shank, and thigh by using the flexible cohesive elastic bandage (BandMax™, China). Tracking rigid plates were attached to the pelvis and fixed by the Velcro fasteners on the waist band. In order to prevent the bandage from loosening and avoid the relative displacement of the markers and skin, the rigid plates and limbs were secured by a common non-elastic medical bandage.
We defined a local coordinate system for each lower limb segment through digitized palpated bony landmarks on the lower limb segments using a digital probe, where the bony landmarks included left/right ilium anterior superior (LIAS/RIAS), left/right prominence of the greater trochanter external surface (LGT/RGT), left/right femur lateral/medial epicondyle (LFLE/RFLE, LFME/RFME), left/right fibula apex of lateral malleolus (LFAL/RFAL), left/right tibia apex of medial malleolus (LTAM/RTAM), left/right dorsal aspect of first metatarsal head (LFM/RFM), and left/right dorsal aspect of fifth metatarsal head (LVM/RVM). The local coordinate system was then linked to the segment’s individual tracking plate by means of coordinate transformations. Once tracking markers did obstruct by the participants’ body, the trial would not be used for any further analysis.
All participants were instructed to stand facing the foam cushion, and assumed the kneeling posture from an initial upright position. Each participant descended and stood up according to the research assistant’s command. All participants hit the ground on their knees at their natural pace. In order to acquire the maximum flexion angle, the participants were asked to hold the kneeling position motionless for approximately 3 s, and then move against gravity to return to the standing position. Each participant conducted at least six effective kneeling trials. Fig. 1 shows the participants assuming the kneeling posture in the resting phase.
Fig. 1.
Photographs showing that the participants are performing the kneeling activity in the resting phase
Participants completed the activity without the help of instruments or the research assistant. It was observed that the younger group was able to execute their trials without the use of their hands; however, the trials were a bit more challenging for individuals in the elderly group, as well as those who were obese, and use of their hands was necessary. For the resting phase, kneeling posture includes two kinds of kneeling positions: one is the dorsi-flexed kneeling and the other is the plantar-flexed kneeling. For the purpose of obtaining kinematics of kneeling in daily life, this study did not dictate which position the participants should take.
The raw kinematic data were entered into the Visual-3D software Version 3.91.2 (C-Motion Inc., Gaithersburg, MD, USA), then filtered using a software integrated digital filter, with a cut-off frequency of 6 Hz. The start of the kneeling trial was triggered by the movement of any one of the three joints, while the end of trial was defined as the termination of motion of all three joints. The kneeling cycles were extended or compressed in time to yield a normalized activity cycle of 101 equally spaced data points. All kneeling cycles were expressed as a function of a unit (100%) cycle length irrespective of the actual time for a trial. Some data of kneeling trial were misleading because of the influence of unsmoothed kneeling activity, resulting in unusual corresponding motion curves mapped data as compared with the overall curves. For example the waveform of curves was inconsistent with that of the overall curves or the measured values were far greater than the average values. These inconsistent kneeling data were not collected or were excluded from statistical analysis. Thus, only data from effective trials were used for the kinematics analyses. Local coordinate systems were defined for the foot, shank, thigh, and pelvis segments to enable the calculation of the floating axis angles at the ankle, knee, and hip joints (Grood and Suntay, 1983). The relative joint angles were defined by using a Cardan sequence (x-y-z rotation). The local x, y, and z axes corresponded respectively to flexion/extension, abduction/adduction, and internal/external rotation for the hip and knee joints, and dorsi/plantar flexion, eversion/inversion, and internal/external rotation at the ankle joint. The flexions of the hip and knee and the ankle dorsi flexion were positive; hip, knee, and ankle adductions were positive; hip, knee, and ankle external rotations were positive. The kinematic results were saved in ASCII format and transferred to Excel and Graphpad Version 5.00 (Prism 5 for Windows).
For qualitatively examining the mean angles generated during kneeling activity, the angles of all three joints in all planes as well as all the joint angle curves were produced. Six trials for each participant were averaged and mean joint angles of each participant were calculated. These individual data were then averaged to provide the mean value and standard deviation (SD) for each group. Correspondingly, the mean kinematic curves for each participant were used to create an ensemble mean curve for two groups. The mean values of the peak ankle, knee, and hip in the three planes (sagittal, frontal, and transversal planes) were used for statistical analysis. Data presented in this study were relative to the dominant leg—the leg that participants use to kick a ball. For all calculated joint angles, unpaired t-tests were performed to test the difference between the young and elderly groups by using GraphPad Version 5.00, and the significance level was set to α=0.05.
3. Results
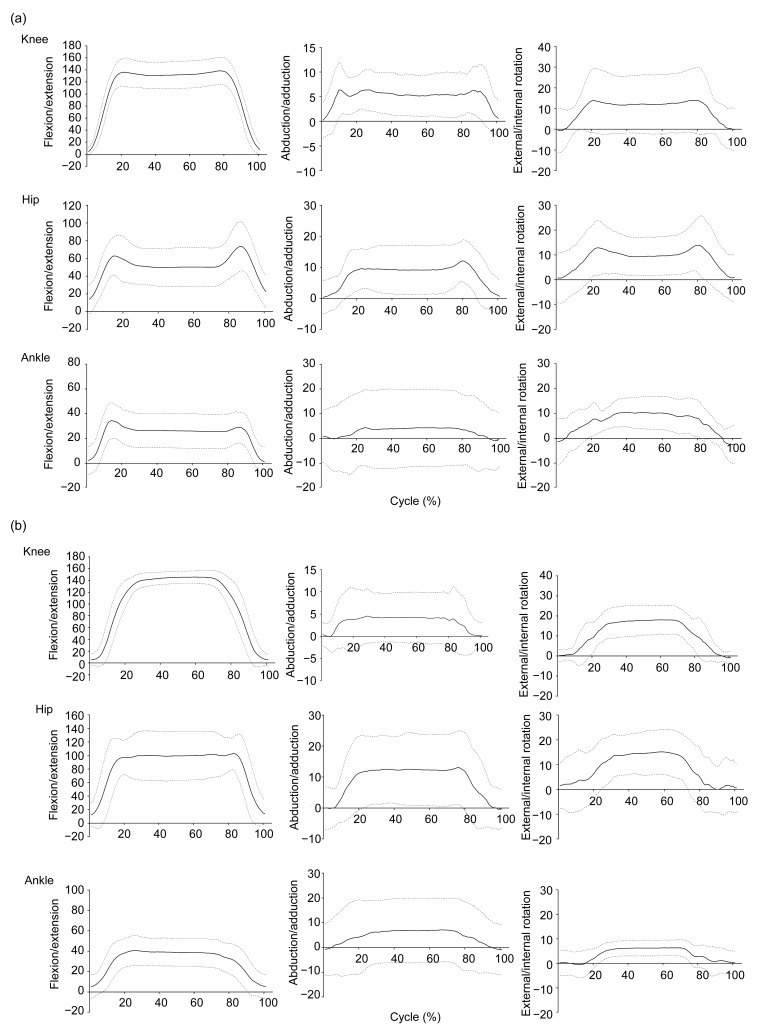
3D hip, knee, and ankle joint angles of the kneeling position are presented in Tables 2 and 3 by age category. The ensemble mean joint angle curves and SDs for each group are presented in Fig. 2. For the flexion/extension motion, the SDs at the hip, knee, and ankle are smaller than those for the abduction/adduction and internal/external rotation. The ROM in the sagittal plane was 139.6° at the knee joint (P=0.5387) and 35.7° at the ankle joint (P=0.9163) in the young group, while in the elderly group we observed 140.9° at the knee joint and 37.6° at the ankle joint. No significant differences were found between the two groups in these angles; however, the ROM at the hip joint was significantly different between the two groups at 67.5° in the young group and 100.5° in the elderly group (P<0.0001). In the frontal plane, the maximum ROM of the knee abduction/adduction was 11.6° (P=0.0856) in the young group, and 9.1° in the elderly group. In the transversal plane, the maximum ROM of the knee internal/external rotation and the maximum ROM of the hip internal/external rotation were 23.3° and 28.2°, respectively, in the elderly group. In the young group, we observed 22.7° (P=0.7514) and 21.3° (P=0.7367), respectively. No statistically significant difference was found between the two groups.
Table 2.
Mean kinematics for the kneeling activity in the three axial planes of the young group
| Motion | n | Maximum angle (°) | Minimum angle (°) | ROM (°) |
| FL/EX | ||||
| Ankle | 11 | 40.2±10.5 | 4.5±8.7 | 35.7±5.6 |
| Knee | 21 | 142.5±21.7 | 2.9±7.0 | 139.6±18.7 |
| Hip | 25 | 81.3±26.8 | 13.9±16.3 | 67.5±22.5 |
| AB/AD | ||||
| Ankle | 15 | 7.8±14.7 | −4.7±12.5 | 12.4±6.1 |
| Knee | 19 | 10.3±4.6 | −1.3±3.5 | 11.6±4.3 |
| Hip | 21 | 14.4±6.3 | −1.6±4.5 | 15.9±5.8 |
| ER/IR | ||||
| Ankle | 7 | 12.3±6.4 | −4.2±6.9 | 16.5±7.8 |
| Knee | 17 | 18.6±13.9 | −4.1±10.6 | 22.7±9.5 |
| Hip | 22 | 19.1±10.6 | −2.2±8.7 | 21.3±9.7 |
Data are expressed as mean±SD. FL/EX: flexion/extension; AB/AD: abduction/adduction; ER/IR: external rotation/internal rotation; ROM: range of motion
Table 3.
Mean kinematics for the kneeling activity in the three axial planes of the elderly group
| Motion | n | Maximum angle (°) | Minimum angle (°) | ROM (°) |
| FL/EX | ||||
| Ankle | 12 | 41.9±15.2 | 4.4±11.5 | 37.6±12.0 |
| Knee | 17 | 146.1±10.4 | 5.3±9.4 | 140.9±6.2 |
| Hip | 16 | 110.5±26.1 | 10.0±14.3 | 100.5±19.7 |
| AB/AD | ||||
| Ankle | 13 | 8.3±13.1 | −2.6±10.9 | 10.9±5.1 |
| Knee | 12 | 7.6±6.0 | −1.5±3.7 | 9.1±4.4 |
| Hip | 13 | 14.7±11.4 | −2.7±7.1 | 17.4±10.4 |
| ER/IR | ||||
| Ankle | 16 | 6.5±5.9 | −2.1±4.1 | 8.5±5.3 |
| Knee | 13 | 20.1±7.4 | −3.2±3.1 | 23.3±6.9 |
| Hip | 14 | 20.2±7.8 | −8.0±7.3 | 28.2±9.3 |
Data are expressed as mean±SD. FL/EX: flexion/extension; AB/AD: abduction/adduction; ER/IR: external rotation/internal rotation; ROM: range of motion
Fig. 2.
Kneeling mean angles (solid lines) and standard deviations (dashed lines) at the three joints in the three axial planes of the young (a) and elderly (b) groups
4. Discussion
Kneeling is a complex movement, in which higher flexion of the lower limb joints is required. Kneeling is difficult for the obese, which could be attributed to the compression of the posterior soft tissues (skin, fat, muscle, and posterior capsule) between the calf and the thigh, and their excess weight appears to play a role in influencing this movement during the rising and descending phases. Because the excess weight is always difficult to control and perform, obese individuals will consume more energy in the moving stage, and have greater pressure at the joints as compared to individuals who are not obese. This study included three obese participants.
In the sagittal plane, no statistically significant differences were found between the two groups on the ROM or maximum flexion angles of the knee joint (P=0.5387). The sagittal values were similar to the results of previously conducted studies, which used bi-planar radiographs method (Hefzy et al., 1998). The majority of the elderly kneeled with their buttocks resting on their heels (17/20), and when the heel reached the posterior surface of the upper thigh, the limbs became fully flexed. Some of the individuals in the younger group kept their thighs erect (19/30), resulting in a larger SD in the younger group as compared to the older group. Expectedly, the curves of the young group reached their maximum values faster than those of the elderly group since the young individuals can complete the rising and descending phases much quicker than the older individuals.
Statistically significant differences between the two groups were found at the hip joint. The maximum hip flexion demand was significantly lower in the young group (67.5°±22°) as compared with the elderly group (100.5°±20°, P<0.0001). The differences in kneeling style between the younger and elderly groups may account for this significant difference. Almost all the elderly adults preferred to kneel with their ankles dorsi-flexed making their buttocks rest on their heels and then put their hands on their thigh upside, as a result making their upper body bend forward. Conversely, almost all young adults dropped their hands to their side during kneeling, keeping their torso upright, resulting in a low hip flexion angle. Furthermore, the waveforms of the curves of the hip joint angles were different between the two groups. The curve for the young group had two peaks, one being 60° at ~14% of the cycle, and the other 75° at ~86% of the cycle; alternatively, the curve for the elderly group had no peak (Fig. 2). This difference may be explained in part by the fact that the younger adults performed their trials without the assistance of their hands, resulting in a shock force of the body weight in the descending phase and the force against gravity in the rising phase producing two peak values. The elderly group, however, had much slower movements, and used their hands, which resulted in most of their weight being shared by their upper limbs during the descending and rising phases. As a result, the force carried by the lower limbs was significantly reduced, causing a smooth kinematic curve (i.e., no peaks).
The maximum values of the hip and ankle flexions occurred approximately at the same time, before the knee was fully flexed. In the young group, hip and ankle flexions increased with knee flexion, and reached maximum values when the knee flexion increased to 116°. Even though the time from standing to resting position was longer in the elderly group, hip and ankle flexions reached maximum values when the knee flexion was 118° (Fig. 2).
In the frontal plane, the hip and knee displacements in the two groups were approximately similar. The ROM of the knee abduction/adduction was 9.1° in the elderly group compared to 11.6° in the young group (P=0.0856). The ROM of the hip abduction/adduction was 17.4° in the elderly group compared to 15.9° in the young group (P=0.9163, Tables 2 and 3). Ankle joint repeatability is slightly lower; the main reason is that there is no limit on the kneeling style in this study.
In the transversal plane, the displacements of the hip and knee joints in the elderly group were slightly higher than those of the younger group. The ROM of the knee internal/external rotation was 23.3° in the elderly group compared to 22.7° in the young group (P=0.7514). The ROM of the hip internal/external rotation was 28.2° in the elderly group compared to 21.3° in the young group (P=0.7367, as shown in Tables 2 and 3). The appearance was suspected to be relative to the higher ROM of the hip flexion in the elderly group. In the frontal and transversal planes, the repeatability was lower and the kinematic curves had relatively large SDs. Previous studies have advised to pay a close attention when interpreting data in the transverse and frontal planes since the soft tissue artifact produces spurious rotational effects that have magnitudes comparable with the relevant joint rotations during movement (Prost, 1974).
Kneeling has higher requirements for the hip and knee joints on the flexion motion in the sagittal plane. At the hip joint, the mean ROM of flexion was 100.5° for the healthy individuals in the older group. Nevertheless, the reported mean maximum ROM of flexion achieved following total hip arthroplasty (THA) was 99.8° (SD=15.3°) with a range of 48° to 121° (Krushell et al., 1991; McGrory et al., 1995). This implies that the postoperative maximum ROM of flexion of THA is close to the flexion value necessary for common kneeling activity. Although the flexion of THA can approach what is required for keeling activity, it is not safe for the patients who have undergone THA to perform this activity. There is a greater risk at the knee joint, because the mean ROM of flexion arrives at 140.9° in common kneeling, which clearly exceeds the mean maximum ROM of flexion achieved following total knee arthroplasty (Ahlberg et al., 1988; Unnanantana, 1997; Hamai et al., 2008; Nakamura et al., 2010). Therefore, patients who have undergone knee or hip arthroplasty should not perform this activity.
This study indicates that for patients who have undergone joint arthroplasty, safely assuming the kneeling position cannot be guaranteed; therefore, it is necessary to design a joint prosthesis with a higher ROM, in addition to improving surgical techniques for joint arthroplasty. In the future, joint arthroplasty should meet joint kinematic requirements and empower patients with better physical ability. The results of this study can be used for reference to design better joint prosthetics to meet various activity needs.
Errors associated with measurement of human movement need to be taken into consideration. Soft tissue artifact is the most common source of error in human movement analysis (Leardini et al., 2005). It has been shown that movement of the soft tissue occurs mainly in the areas close to the joint. For compensating soft tissue artifact effectively, one method is to characterize parameters from a large series of measurements on different subject populations (Prost, 1974). Another method, developed by Angeloni et al. (1992), reported that mounting markers onto the rigid plates as opposed to directly on the skin, would result in less soft tissue artifact. Therefore, in order to obtain the most accurate kinematic data in this study, we achieved a large sample size of 50 participants, and placed markers on the rigid plates, which were strapped onto the distal halves of the thigh and shank.
5. Conclusions
The present study collected kinematic data of hip, knee, and ankle joints during kneeling activity to explore the ROM of kneeling activity in a healthy Chinese population. The data of the current study provided baseline information about Chinese populations for physicians and therapists concerned with the surgical and functional rehabilitation, as well as to help engineers engaged in prosthetics design establish the criteria for lower limb prosthetics which is suit for Chinese populations.
Footnotes
Project supported by the National Natural Science Foundation of China (No. 30810103908), the Science Foundation of Shanghai (No. 09441900300), and the State Key Fundamental Research Program of China (No. 2011CB711000)
References
- 1.Ahlberg A, Moussa M, Al-Nahdi M. On geographical variations in the normal range of joint motion. Clin Orthop Relat Res. 1988;9(234):229–231. [PubMed] [Google Scholar]
- 2.Angeloni C, Cappozzo A, Catani F, et al. Quantification of Relative Displacement between Bones and Skin and Plate-mounted Marker. VIII Meeting on European Society of Biomechanics; Rome, Italy. 1992. p. 279. [Google Scholar]
- 3.Baltzopoulos V. A videofluoroscopy method for optical distortion correction and measurement of knee-joint kinematics. Clin Biomech (Bristol Avon) 1995;10(2):85–92. doi: 10.1016/0268-0033(95)92044-M. [DOI] [PubMed] [Google Scholar]
- 4.Coughlin KM, Incavo SJ, Doohen RR, Gamada K, Banks S, Beynnon BD. Kneeling kinematics after total knee arthroplasty: anterior-posterior contact position of a standard and a high-flex tibial insert design. J Arthroplasty. 2007;22(2):160–165. doi: 10.1016/j.arth.2006.05.023. [DOI] [PubMed] [Google Scholar]
- 5.Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105(2):136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 6.Hamai S, Miura H, Higaki H, Matsuda S, Shimoto T, Sasaki K, Yoshizumi M, Okazaki K, Tsukamoto N, Iwamoto Y. Kinematic analysis of kneeling in cruciate-retaining and posterior-stabilized total knee arthroplasties. J Orthop Res. 2008;26(4):435–442. doi: 10.1002/jor.20512. [DOI] [PubMed] [Google Scholar]
- 7.Hefzy MS, Kelly BP, Cooke TD. Kinematics of the knee joint in deep flexion: a radiographic assessment. Med Eng Phys. 1998;20(4):302–307. doi: 10.1016/S1350-4533(98)00024-1. [DOI] [PubMed] [Google Scholar]
- 8.Hemmerich A, Brown H, Smith S, Marthandam SS, Wyss UP. Hip, knee, and ankle kinematics of high range of motion activities of daily living. J Orthop Res. 2006;24(4):770–781. doi: 10.1002/jor.20114. [DOI] [PubMed] [Google Scholar]
- 9.Kanekasu K, Banks SA, Honjo S, Nakata O, Kato H. Fluoroscopic analysis of knee arthroplasty kinematics during deep flexion kneeling. J Arthroplasty. 2004;19(8):998–1003. doi: 10.1016/j.arth.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 10.Krushell RJ, Burke DW, Harris WH. Range of motion in contemporary total hip arthroplasty. The impact of modular head-neck components. J Arthroplasty. 1991;6(2):97–101. doi: 10.1016/S0883-5403(11)80002-1. [DOI] [PubMed] [Google Scholar]
- 11.Leardini A, Chiari L, Della Croce U, Cappozzo A. Human movement analysis using stereophotogrammetry—Part 3. Soft tissue artifact assessment and compensation. Gait Posture. 2005;21(2):212–225. doi: 10.1016/j.gaitpost.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 12.McGrory BJ, Morrey BF, Cahalan TD, An KN, Cabanela ME. Effect of femoral offset on range of motion and abductor muscle strength after total hip arthroplasty. J Bone Joint Surg Br. 1995;77(6):865–869. [PubMed] [Google Scholar]
- 13.Moro-Oka TA, Hamai S, Miura H, Shimoto T, Higaki H, Fregly BJ, Iwamoto Y, Banks SA. Dynamic activity dependence of in vivo normal knee kinematics. J Orthop Res. 2008;26(4):428–434. doi: 10.1002/jor.20488. [DOI] [PubMed] [Google Scholar]
- 14.Mulholland SJ, Wyss UP. Activities of daily living in non-Western cultures: range of motion requirements for hip and knee joint implants. Int J Rehabil Res. 2001;24(3):191–198. doi: 10.1097/00004356-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Nakagawa S, Kadoya Y, Todo S, Kobayashi A, Sakamoto H, Freeman MA, Yamano Y. Tibiofemoral movement 3: full flexion in the living knee studied by MRI. [Comparative Study Research Support, Non-U.S. Gov′t] J Bone Joint Surg Br. 2000;82(8):1199–1200. doi: 10.1302/0301-620X.82B8.10718. [DOI] [PubMed] [Google Scholar]
- 16.Nakamura S, Takagi H, Asano T, Nakagawa Y, Kobayashi M, Nakamura T. Fluoroscopic and computed tomographic analysis of knee kinematics during very deep flexion after total knee arthroplasty. J Arthroplasty. 2010;25(3):486–491. doi: 10.1016/j.arth.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 17.Prost JH. Varieties of human posture. Hum Biol. 1974;46(1):1–19. [PubMed] [Google Scholar]
- 18.Unnanantana A. Press-fit-condylar total knee replacement: experience in 465 Thai patients. J Med Assoc Thai. 1997;80(9):565–569. [PubMed] [Google Scholar]