Abstract
Objectives:
To review the evidence of the involvement of the Wnt signalling pathway in mood disorders and in the action of drugs used to treat these disorders.
Methods:
We performed a careful PubMed search using as keywords all possible terms relevant to the Wnt pathway and crossing them with each of four areas, i.e., developmental effects, behavioural effects, mood disorders, and drugs used in their treatment. Papers were selected on the basis of their content and their data used for discussion.
Results:
Neurodevelopmental and behavioural data point to the possibility of involvement of the Wnt pathway in the pathophysiology of mood disorders. Clinical and post-mortem data are not sufficient to corroborate a definite role for Wnt alterations in any mood disorder. Combining genetic and pharmacological data, we may state that glycogen synthase kinase is the key molecule in bipolar disorder, as it is connected with many other signalling pathways that were shown to be involved in mood disorders, while Wnt molecules in the hippocampus appear to be mainly involved in depressive disorders.
Conclusions:
Altered Wnt signalling may play a role in the pathophysiology of mood disorders, although not a central one. It is premature to draw conclusions regarding the possible usefulness of Wnt manipulations in the treatment of mood disorders.
Keywords: Wingless (Wnt) signalling, Mood Disorders, Bipolar Disorder, Major Depression, Antidepressant Drugs, Mood Stabilising Agents, Antipsychotic Drugs.
1. INTRODUCTION
The Wnt signalling pathway or armadillo chain owes its name to wingless and Int-1, two proto-oncogenes that produce wingless mutations in Drosophila [1]. Wnt glycoproteins regulate morphogenesis in the developing central nervous system (CNS), and can also affect neuronal functions in adulthood [2,3]. In addition, abnormalities of the Wnt signalling pathway have been implicated in the pathophysiology of CNS disorders [see 4, for a review].
To date, there is no evidence that abnormalities in the Wnt signalling pathway are causally related to any psychiatric disorder; however, alterations of individual components of the pathway have been found in psychiatric disorders. The evidence that β-catenin levels are reduced in the hippocampal CA3 and CA4 regions, and Wnt1 levels are increased in the hippocampal CA4 region of post-mortem schizophrenic brains [5,6] fostered interest into the role of the Wnt signalling pathway in psychiatric disorders. Because lithium inhibits glycogen synthase kinase3β (GSK3β [7,8], a component of the canonical Wnt pathway (see below), the pathway has been proposed as a specific target in the treatment of bipolar disorders [9-12]. Here, we discuss (i) the physiological role of the Wnt pathway; (ii) preclinical data that suggest an involvement of the pathway in the pathophysiology of mood disorders (ii); the evidence for alterations in Wnt signalling in mood disorders; and (iv) the modulation of the Wnt pathway by drugs that are currently used in the treatment of mood disorders.
2. METHODS
We searched the PubMed database using different strategies according to the section of the review. We used a general set of key words with all expressions denoting the pathway itself or the molecules known to be components of the Wnt signalling pathway (e.g., Wnt*, or wingless, or armadillo, or Dvl, or Dishevelled, or axin, or catenin*, or glycogen synthase kinase, or Frizzled, or Dickkopf*, or LRP5/6 receptors etc.). This set we used in all individual searches. To review the role of the Wnt pathway in human physiology and normal development, we crossed the above set with other key words, like neurodevelopment, development, apoptosis, cellular death, proliferation, oncogenesis, physiology, subsequently restricting to human studies. To gather behavioural studies of the Wnt pathway, we used the same strategy as above regarding the pathway, and crossed with general terms like behaviour and behavioural, specific terms like depression, psychosis, anxiety, hyperactivity, exploratory, immobility, avoidance, aggression, aggressiveness, aggressive, sedation, sniffing, grooming and the like, and paradigm-related terms, like forced swim test, tail suspension, open-field, marble burying etc. To identify studies dealing with the involvement of the Wnt pathway in mood disorders, we crossed the above set with another set containing terms like bipolar, depression, depressive, dysthymia or dysthymic, mixed state, agitation, mania, manic, rapid cycling, hyperthymic, dysphoric or dysphoria, suicide, suicidality, killed and self, and mood. Finally, to explore the effects of drugs used in the mood disorders on the Wnt pathway, we crossed the general set with subsets composed of keywords, like mood stabilisers or each one of them (i.e., lithium, carbamazepine, valproic acid or valproate or divalproate, oxcarbazepine, and lamotrigine, as well as the benzodiazepine clonazepam), antipsychotics or each antipsychotic, and antidepressants or each antidepressant. We then selected retrieved articles according to their relevance and further searched their References.
3. THE WNT PATHWAY IN HUMAN PHYSIOLOGY AND NORMAL DEVELOPMENT
The Wnt family in humans consists of 19 secreted proteins, termed Wnt1, Wnt2, Wnt2B, Wnt3, Wnt3A, Wnt4, Wnt5A, Wnt5B, Wnt6, Wnt7A, Wnt7B, Wnt8A, Wnt8B, Wnt9A, Wnt9B, Wnt10A, Wnt10B, Wnt11, and Wnt16. All these proteins undergo post-translational modifications and are 350-400 amino acid-long.
Wnt ligands interact with a number of surface receptors, which include Frizzled (Fzd) receptors, the low-density lipoprotein receptor-related protein 5 and -6 (LRP5/6), and the tyrosine kinase receptors, Ryk and Ror [13-15].
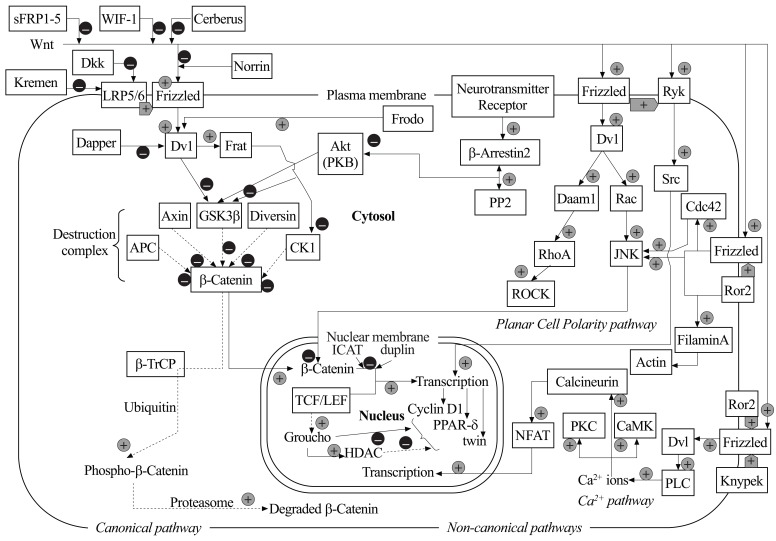
Wnt signalling pathways are classified as β-catenin-dependent and β-catenin-independent, also known as canonical and non-canonical Wnt pathways, respectively (Fig. 1). β-Catenin is an intracellular protein that exert pleiotropic functions, including adherent junction formation and gene expression regulation (see below).
Fig. (1).
Schematic drawing of Wnt-related pathways. The canonical pathway depends always on β-catenin, whereas the other, non-canonical pathways may interact with β-catenin–dependent processes, but do not depend on the presence of β-catenin. Different Wnts may have different effects on overall cellular function, depending on the receptors involved and on the availability of co-receptors (LRP, Knypek, Ror2, Ryk etc.) Depicted are also some molecules not strictly belonging to the Wnt pathways, but having a central role in switching on or off β-catenin–regulating steps. Solid arrows in the canonical pathway show events with Wnt stimulating Frizzled; dashed arrows show events occurring in the absence of Wnt. Black arrows for the canonical pathway, grey arrows for the non-canonical; CaMK, calmodulin kinase; CK1, Casein Kinase 1; Dkk, Dickkopf; HDAC, histone deacetylase; Daam1, Disheveled-associated activator of morphogenesis 1; ICAT, Inhibitor of β-catenin and T-cell factor; JNK, Jun kinase; PKB, protein kinase B or Akt; PKC, protein kinase C; PLC, phospholipase Cβ; PP2, protein phosphatase 2A; PPAR-δ, Peroxisome proliferator-activated receptor delta; ROCK, Rho-associated kinase; sFRP1-5, secreted Frizzled-related proteins 1-5; β-TrCP, β-Transducin repeat Containing Protein; WIF-1, Wnt-inhibiting factor 1; +, enhancement, activation; –, down-regulation, inhibition.
In the “canonical” pathway, Wnt binds to Fzd and LRP5/6, thereby recruiting the scaffold protein, Dishevelled (Dvl), to the ligand-receptor complex. Activated Dvl binds to, and destabilises, a “β-catenin-destruction complex”, composed by GSK3β, adenomatous poliposys coli (APC), and axin. Within the destruction complex, GSK3β phosphorylates β-catenin, which is then committed to proteasomal degradation [13]. It is noteworthy that this is not the only function of GSK3β. GSK3β is a constitutively active serine/threonine kinase that phosphorylates a wide range of substrates, thereby regulating fundamental processes such as protein synthesis, glycogen synthesis, and apoptotic cell death [16-18]. To what extent these additional mechanisms of GSK3β are regulated by Wnt signalling is unclear. Activation of the canonical Wnt pathway causes an accumulation of undegraded β-catenin in the cytoplasm. β-Catenin then translocates into the nucleus, where it combines with the T-cell factor/lymphoid enhancer factor (TCF/LEF) family of transcription factors to regulate gene expression [13-19]. GSK3β is a point of convergence of multiple signalling pathways, including the phosphatidylinositol-3-kinase (PI3K)/Akt pathway, which is activated by a variety of G-protein coupled receptors and tyrosine kinase receptors, including the insulin receptor [20]. Phospho(activated)-Akt inhibits GSK3β by phosphorylating a serine residue (Ser9) in the N-terminus domain of the enzyme. The precise details of Wnt inhibition of GSK3β are unclear. One should bear in mind that the canonical Wnt pathway prevents the phosphorylation of β-catenin by GSK3β, but could leave other GSK3β functions intact. However, studies in Wnt overexpressing PC12 cells show that (i) activated Dvl recruits protein kinase B (Akt) at the β-catenin destruction complex; (ii) Akt inhibits β-catenin degradation by phosphorylating GSK3β on Ser9; and (iii) a negative dominant mutant of Akt decreases free β-catenin levels [21].
Some Wnt isotypes, including Wnt4, Wnt5a, and Wnt11, are able to activate “non-canonical” β-catenin-independent pathways, such as the Planar Cell Polarity (PCP) and Wnt/Ca2+ pathways [13,22] (Fig. 1). In the Wnt/Ca2+ pathway, Wnt5a signalling through Fzd and Dvl activates phospholipase-Cβ, which stimulates the hydrolysis of phosphatidylinositol-4,5-bisphosphate with ensuing formation of the second messengers, inositol-1,4,5-trisphosphate (InsP3) and diacylglycerol (DAG). InsP3 stimulates Ca2+ release from intracellular stores, whereas DAG facilitates the activation of protein kinase C (PKC). PKC in turn activates Cdc42 (cell division control protein 42), a regulator of cell adhesion, cell migration and tissue pattering. The increase in intracellular Ca2+ activates a mitogen-activated protein kinase (MAPK) pathway composed of the transforming growth factor-β-activated protein kinase (TAK1), which is a MAPK kinase kinase, and the nemo-like kinase (NLK), which is a MAPK. This pathway negatively regulates the canonical Wnt pathway by inhibiting gene transcription mediated by the β-catenin/TCF complex [13,23-26]. In the PCP pathway, Wnt-mediated activation of Fzd and Dvl promotes the formation of the scaffold protein-Daam1 complex, which in turn activates the G-protein Rho. Rho activates ROCK (Rho-associated kinase), which is a key regulator of cytoskeleton dynamics [17,26,27]. The PCP pathway contributes to major developmental processes, such as body axis elongation and neural tube formation [28,29].
4. WNT IN NEURODEVELOPMENT
There are four major classes of secreted extracellular signalling molecules which are expressed in the developing brain during embryogenesis and participate in the patterning of the nervous system: Wnts, fibroblast growth factors (FGFs), Sonic Hedgehog (SHH), and Bone Morphogenetic Proteins (BMPs) [30]. Wnts, like BMPs, stem from the cortical hem, comprising the medial margin of each hemisphere. Wnt signalling has a recognized function in neurodevelopment since the early report of cerebellar and midbrain atrophy in Wnt1 knockout mice [31]. Regional specification of the developing brain depends on an anteroposterior gradient of Wnt signalling, being low for anterior structures and high for posterior structures [32,33]. Wnt signalling is also involved in processes of morphogenesis, neuronal migration and specification, and proliferation of neuronal progenitors [5,34]. In addition, a large body of evidence suggests a role for Wnt signalling in axon guidance, neurite outgrowth, and synaptic plasticity, including the regulation of long-term potentiation (LTP) of excitatory synaptic transmission in the adult brain [reviewed in 16]. Last, the Wnt signalling pathway contributes to the physiological cross-talk between neurons and astrocytes; disrupting this specific function may lead to neuro-degeneration in age-related disorders, such as Alzheimer's disease [2,35].
5. THE IMPORTANCE OF NEURODEVELOPMENT IN PSYCHIATRIC DISORDERS
The pathophysiology of most psychiatric disorders is still unclear. Recent data indicate a neurodevelopmental origin for schizophrenia [36-38], bipolar disorder [39], attention deficit/hyperactivity disorder [40], and autism and mental retardation [38,41,42]. Several studies suggest a role for Wnt-related proteins in the aetiology of autism, schizophrenia [4,34,43,44], and mood disorders [10,45].
6. BEHAVIOURAL STUDIES AND THE WNT PATHWAY
Recent data show that GSK3 regulates mood-related behaviour. The expression levels of GSK3β are associated with depression- and anxiety-like behaviours, as shown by an increased exploratory activity [46], reduced amphetamine-induced hyperactivity, and reduced immobility in the forced swim test [47] in mice lacking one copy of the GSK3β gene. However, GSK3β-overexpressing mice also show a reduced immobility in the forced swim test, a phenomenon that has been associated with a 20% reduction in the brain size [48]. Haploinsufficiency of the GSK3β gene also reduces depression-like behaviour in serotonin-deficient mice [49]; however, others found contrasting data [50]. An increased locomotor activity has been observed in mice expressing a constitutive active mutated form of GSK3β bearing a Ser to Ala substitution in position 9 [51]. Mice expressing an Akt-resistant form of GSK3β also display a reduced immobility time in the forced swim test, as well as a tendency to walk a longer distance in the unprotected area, and a higher number of unprotected head dips in the O-maze [52]. Recently, it has been shown that blockade of Dvl function and over-expression of GSK3β in the nucleus accumbens render mice more susceptible to social defeat stress and promote depression-like behaviour [53]. GSK3α knockin mice show decreased exploratory activity, decreased immobility time in the forced swim test, and reduced aggressive behaviour [54], suggesting that the two GSK3 isoforms have similar effects on behaviour. Accordingly, GSK3α/β knockin mice with serine-to-alanine mutations show increased susceptibility to amphetamine-induced hyperactivity and stress-induced depressive-like behavior, and serine-phosphorylation of GSK3 is reduced during mood-related behavioural responses [55]. These data raise the possibility that GSK3α and GSK3β have redundant functions in regulating mood-related behaviour [56-58]. As expected from the data of transgenic mice, pharmacological inhibition of GSK3 with lithium, NP031115, alsterpaullone, SB216763, L-803-mts and AR-A014418, decreases both the immobility time in the forced swim test, and amphetamine-induced hyperactivity [47,59-61].
Finally, GSK3 activity regulates circadian rhythms, with genetic depletion or inhibition of GSK3 resulting into a significant delay in the periodicity of the endogenous clock [62].
7. WNT AND MOOD DISORDERS
7.1. Bipolar Disorder Type I/II
Bipolar disorder (BP), also known as bipolar affective disorder or manic-depressive illness, is associated with alterations in synaptic formation and plasticity [63]. BP causes, in both childhood and adulthood, unusual shifts in mood, energy, and activity levels, from manic phases, characterised by euphoric mood, increased motor activity and energy, to phases of depression, characterised by loss of both energy and pragmatism. Manic episodes are characterised by periods of abnormally and persistently elevated mood (elation) or abnormal expansivity or irritability for at least one week (or needing hospitalisation), not due to substance use or medication or somatic antidepressant treatment. During these periods, affected persons show elevated self-esteem or grandiosity, increased energy and decreased need for sleep, early awakenings, pressured or racing thoughts, flight of ideas, loosening of associations, inappropriate talkativeness, goal-directedness, and involvement in immediately rewarding activities despite high probability of long-term damage. Behaviour during these periods may lead to social or occupational impairment or it may be characterised by psychotic symptoms. Major depressive episodes are characterised by depressed mood or loss of interest or pleasure in usually pleasurable activities, and extreme and opposite symptoms, like weight loss or gain, insomnia or hypersomnia, psychomotor agitation or retardation, or also decreased energy and fatigue, feelings of worthlessness or guilt, reduced ideational production, undecidedness, inability to concentrate or to store or retrieve memories, and recurrent thinking about death, although not necessarily about suicide and not simply fear of dying, and possible suicidal thoughts and plans. These symptoms must occur at least in a subset of five out of nine and in the same 2-week period (at least) and must not overlap with a manic episode. When the latter occurs, a mixed episode diagnosis is posed in the context of bipolar disorder. A hypomanic episode is similar to a manic one, save for the social-occupational impairment/psychotic symptom criterion. Major or unipolar depression is the occurrence of one or more major depressive episodes and is ruled-out when criteria for BP are met. BP is BPI when manic episodes occur and may alternate or co-occur (mixed episodes) with major depressive episodes; it is BPII when manic episodes have never occurred and hypomanic episodes alternate or co-occur with major depressive episodes. A BPII may become BPI and stay so, a BPI patient never becomes BPII [64].
7.1.1. Animal Studies
Rats treated with the mood stabilisers, lithium and valproate, show increased levels of β-catenin, which is indicative of an activation of the Wnt pathway, in the frontal cortex [65]. GSK3β is inhibited by lithium, valproate, and antipsychotics by increasing GSK3β serine phosphorylation or directly inhibit enzyme activity [7,66-70]. A role for GSK3β in the pathophsiology of BP is suggested by the following observations: (i) mice overexpressing GSK3β show hyperactivity [51]; (ii) an increase in amphetamine-induced hyperactivity is associated with reduced serine-dephosphorylation of GSK3β [47]; and (iii) GSK3β inhibitors (as well as lithium) produce antidepressant-like effects [47,60,71].
7.1.2. Human Studies
Post-mortem studies suggest that defects in neurodevelopment and neuroplasticity underlie BP. Grey matter volume is reduced by about 40% in the subgenual prefrontal cortex of BP patients [72] (Drevets et al., 1997), and this reduction is associated with glial cell loss and reduced neuronal number or size [73,74]. These findings prompted investigators to focus on Wnt-related molecules in post-mortem BP brain.
No changes in GSK3 expression were found in BP brains, compared healthy control brains [75,76]. Measurements of GSK3 activity in post-mortem human brain tissue are difficult because enzyme activity rapidly declines after death [77]. GSK3 activity can be assessed reliably in peripheral blood mononuclear cells (PBMCs) [78]. PBMC studies showed a significant decrease in serine phosphorylation of both GSK3α and GSK3β in symptomatic BP patients, as compared to healthy controls [55]. PBMCs were also used to assess GSK3 activity in response to drug treatment. Interestingly, phospho-Ser9-GSK3β levels were 8-fold in BP patients stabilized on lithium, compared to healthy controls [78]. These findings were confirmed in a group of patients with BPI who were hospitalized for a manic episode. Symptom improvement during an eight-week period of treatment with lithium, valproate, or atypical antipsychotics was associated with increased PBMC inhibitory GSK3β serine phosphorylation [79].
GSK3β gene studies have shown that some polymorphisms may underlie the susceptibility to mood disorders and may serve as potential markers of severity of such disorders [80]. Studying monozygotic twin pairs with one affected and one healthy member, four Wnt-related genes, KCNK1, MAL, PFN2, TCF7, and PGK1, were found to be overexpressed in BP [81]. Two SNPs (single nucleotide polymorphisms) in the promoter region of the GSK3β gene have been associated with BP; the –50T/C SNP and the C-variant polymorphism were found to be related to later onset, and to better response to acute sleep deprivation in BP patients [82-84]. The −1727A/T SNP has been associated with age at onset and presence of psychotic symptoms in BP [85]. In another study, the rs2267665 and rs9462082 SNPs in the PPARD (peroxisome proliferators-activated receptor type-δ) gene showed a significant association with BP, with rs9562082 being also related to symptom severity [86]. Studying the GSK3β locus, a copy number variation (CNV) in the 3' non-coding region, was found to be more frequent in BP patients than in healthy controls [87]. In a wider meta-analysis, the GSK3β locus was found to be implicated in BP by the widest array of studies, including association analysis, gene expression, pharmacogenomics, structural variants, and mouse models [88]. GSK3 mRNA levels were found to be lower in membranes and cytosolic fractions of platelets from drug-free patients with bipolar mania than in healthy controls or drug-free patients with major depressive disorder (MDD) [89]. Treatment with mood stabilisers restored GSK3 mRNA levels in BP-I patients, while antidepressant treatment did not affect GSK3 mRNA levels in platelets of patients with MDD [89].
Whether changes in the genes encoding for other Wnt-related molecules are associated with BP remains to be established. Four polymorphisms in the FZD3 gene (rs960914, rs2241802, rs2323019, and rs352203) have not been associated with BP [90].
7.2. Major Depressive Disorder (MDD)
As in bipolar disorder, abnormalities in neuronal plasticity and neurogenesis strongly concur to the pathogenesis of MDD. Recent studies suggest an important role for Wnt signalling pathway in MDD.
Different Wnt isotypes, including Wnt2, 3a, and 7a, are expressed in the rat hippocampus, where an increased Wnt2 expression was shown after chronic treatment with various classes of antidepressants [91] or after chronic electro-convulsive seizures [92]. In addition, viral-induced overexpression of Wnt2 in the hippocampal dentate gyrus produced a clear-cur antidepressant effects using behavioural paradigms endowed with pharmacological validity as tests for antidepressant medication [91]. Furthermore, Wnt3a contributes to hippocampal neurogenesis [14] and Wnt7a promotes synaptogenesis, dendrite maturation and an increase in excitatory synapses [93,94].
Along the Wnt signalling pathway, various components have been specifically implicated in physiological neurogenesis and its anomalies, like Frizzled receptors, Dvl, and GSK3β and β-catenin.
Regarding the Frizzled receptor family, Fdz6 is a seven transmembrane-spanning receptor whose Wnt binding regulates activation of canonical and non-canonical pathways, specifically Ca2+- and PCP-pathways [95]. Fdz6 knockdown models have been studied to better understand behavioural changes; knockdown was related to decreased sucrose preference, which is assumed to represent an anhedonic response, and to increased anxiety in the suppressed feeding test and in the elevated plus maze (EPM); similar data were obtained also through chronic unpredictable stress (CUS) exposure. CUS has also shown decreased Fzd6 expression, suggesting that Fzd6 modulation can concur to the behavioural effects of CUS [96,97]. These results show a specific action of Fdz6 on anhedonia and anxiety, but not on despair, with decreased escapes in the learned helplessness test [96,97]. The way Fdz6 regulates these behaviours is still unknown.
Dvl and β-catenin play a critical role in dendritic arborisation [98] and in axon differentiation, respectively. Concerning GSK3β, its direct inhibition shows an antidepressant-like activity [60]. On the other side, GSK3β is inhibited by antidepressants with serotonergic activity [99].
Genetic studies have thoroughly investigated the role of GSK3β polymorphisms and genes involved in Wnt signalling in the cerebral cortex. These studies shed light on the association between polymorphisms and various regional changes in brain structure observed in MDD patients [100,101]. Several lines of evidence implicate such polymorphisms in vulnerability for mood disorders [80,100,101].
Regional grey matter (GM) volume changes in MDD patients were found in temporolateral and medial prefrontal cortices, in association with SNPs in canonical Wnt signalling pathway genes and in GSK3β substrate proteins genes [100]. GM volume changes in the right hippocampus and bilateral superior temporal gyri are strictly associated with a specific SNP, –157T/C, an intronic polymorphism that regulates the selection of splice acceptor sites of GSK3β, influencing GSK3β transcription [101].
Other four SNPs in the non-coding region of the GSK3β, –50 T/C, +9227 A/G, +11660 G/T and +4251 T/A have been significantly associated with 4-week antidepressant response [102].
Post-mortem studies showed increased activity of GSK3β in suicide victims with MDD [103] and abnormal GSK3β activity in patients with MDD [55]. A study of GSK3β mRNA expression showed an increase in the hippocampus of MDD patients compared with healthy controls [104]. These post-mortem studies should be interpreted with caution for the same reasons we explained in the bipolar disorder section.
Combining these data we may state that Fzd receptors play a role in neurogenesis, synaptic and neuronal plasticity. Thus, it is possible that they are involved in the pathogenesis of MDD. Genetic studies heretofore identified polymorphisms of genes encoding interacting proteins in brain regions involved in MDD, such as hippocampus and temporal gyrus. Genetic variations along the Wnt pathway may be not only involved in disease vulnerability, but also in treatment response. These data need replication.
7.3. Suicide
Suicidal ideation occurs more frequently in mood disorders and death by self-killing is more frequently associated with depression, a state common to BP and MDD and the major source of burden in both disorders.
The Wnt signalling pathway in suicide has not been widely studied so far. Recent post-mortem studies showed increased GSK3β and decreased Akt activities in brains of suicide victims with MDD, but not in suicide victims without depression [103].
One genetic study tackled the issue of genetic polymorphisms and suicidality, focusing on polymorphisms of two common GSK3β SNPs, –1727A/T and –50C/T [105]. Findings showed that SNP alleles, genotypes, and haplotypes did not differ between suicidal MDD patients, non-suicidal MDD patients and healthy controls. Another study was a genoma-wide association study in a suicide attempt bipolar population [106]. This study compared SNP genotypes of more than 1000 bipolar suicide attempters with those of a comparable bipolar population without suicide attempt history. Investigators identified 2507 SNPs with evidence for association at P<0.001; however, when these SNPs were subsequently tested for association in another large and independent bipolar sample, no one was found to be significantly associated after correcting for multiple testing. Despite this, the combined analysis of all sample sets produced an association signal at the threshold of genome-wide significance only for 2p25 (rs300774), with the associated SNPs on 2p25 falling in a large linkage disequilibrium block containing the ACP1 (acid phosphatase 1) gene, a gene whose expression was significantly elevated in people with bipolar disorder who committed suicide. The ACP1 protein is a Wnt signalling influencing tyrosine phosphatase.
8. THE EFFECTS OF DRUGS USED IN MOOD DISORDERS ON THE WNT SIGNALLING PATHWAY
8.1. Mood Stabilisers
8.1.1. Lithium
Lithium is the gold standard in the treatment of BP. It is widely used in the treatment of acute manic episodes and in the prophylaxis of manic and depressive episodes. In addition, lithium possesses an independent antisuicidal action [107]. Lithium has multiple mechanisms of action in neurons, which include the modulation of ion channels and membrane transporters, and the inhibition of intracellular enzymes such as inositol monophosphate phosphohydrolase [108,109], phosphoglucomutase [19], protein kinase C (PKC), and GSK3β [7]. Lithium protects neurons against a variety of insults [110-116], an effect that has been attributed to GSK3 inhibition [7,12,89,107,117].
Klein and Melton [7] and Hedgepeth et al., [8] showed for the first time that “therapeutic” concentrations of lithium could inhibit GSK3, with ensuing activation of β-catenin-mediated gene transcription. This suggested that (i) GSK3β is involved in the pathophysiology of BP; and (ii) lithium interferes with the canonical Wnt pathway. Lithium inhibits GSK3 through direct and indirect mechanisms. Lithium directly inhibits GSK3β through competition for a low affinity Mg2+ binding site [19]. The indirect mechanism is mediated by the activation of enzymes that phosphorylate a serine residue at the N-terminal domain of GSK3β, consequently inhibiting enzyme activity. This action of lithium was shown in PBMCs [78], cultured cells [118], and mouse brain [67]. How lithium increases serine phosphorylation of GSK3β is not entirely clear. The disruption of a β-arrestin/Akt/protein phosphatase-2A (with resultant Akt activation) or indirect protein phosphatase 1 inhibition were advanced to explain it [118-120]. Thus, the synergistic effects of multiple mechanisms may account for the substantial inhibition of GSK3β by lithium [121].
A series of genetic studies in an Italian population indicated that a SNP in the promoter region of GSK3β (–50T/C) was associated with BP, with the C-variant being associated with later onset and better response to lithium or acute sleep deprivation [82-84]. In an independent study, the C-carriers of the -50T/C SNP responded better to lithium augmentation in acutely depressed, antidepressant-resistant BP and MDD patients [122]; however, Szczepankiewicz et al., [123] did not find a significant association between the –50T/C SNP and GSK3β response to prophylactic lithium in BP.
A role for GSK3β inhibition (and the ensuing activation of the canonical Wnt pathway) in the therapeutic action of lithium in mood disorders is supported by preclinical studies. Acute administration of lithium or valproate increases β-catenin levels in the rat frontal cortex [65]. Lithium treatment mimicked the effect of GSK3β inhibitors or the effect of loss-of-function mutations of GSK3β in reducing amphetamine-induced hyperactivity and depressive-like behaviour in rodents [47,59,60,124]. Selective GSK3β inhibitors and lithium attenuate locomotor hyperactivity in response to novelty in mice carrying mutations in the circadian gene, Clock [124]. Clock-mutant mice were advanced as a genetic mouse model for bipolar mania [125], and polymorphisms of the CLOCK gene have been associated with BP and other mood disorders [126-129] (but see also [130] and [131] for contrasting results). The administration of lithium with olanzapine mimicked the effect of GSK3β inhibitors in a new model of mania in male adult mice, as they both reduced amphetamine-induced rearing locomotion [132].
Lithium proved to reverse stress-induced alterations in spatial memory [133] and dendrite architecture in the hippocampus [134]. In addition, lithium treatment blocked stress-induced depressive-like behaviour and hippocampal cell fate, and prevented stress-induced changes in the expression of GSK3β and its target genes in the hippocampus [135]. This suggests that GSK3β is a nodal point in the processes of maladaptive neuronal plasticity triggered by chronic stress and is largely involved in the therapeutic effects of lithium in mood disorders.
8.1.2. Other Mood Stabilisers: Valproate, Lamotrigine, Carbamazepine
The discovery that lithium acts as an inhibitor of GSK3 raised interest in examining whether other mood stabilisers are able to modulate GSK3 activity.
Valproate, a simple branched-chain fatty acid (2-propylpentanoic acid), is an antiepileptic drug with demonstrated efficacy in the treatment of BP-associated acute mania and in the prevention of manic episodes of BP. Valproate is sometimes used to reduce the risk for manic switch in patients with bipolar depression, when antidepressants are concurrently used [136], despite the drug lacks antidepressant effects of its own [137].
Whether valoproate acts as an inhibitor of GSK3β is matter of debate [66,138-143]. Valproate was shown to inhibit GSK3 through a variety of mechanisms, such as serine phosphorylation [66,68,139], tau protein phosphorylation-mediated GSK3 inhibition in human neuroblastoma cell lines overexpressing GSK3β [144], or through the action of metabolites that potently inhibit GSK3 activity in vivo [138]. If present, inhibition of GSK3β by valproate is seen at therapeutic concentrations [65]. Valproate is less potent than lithium in inhibiting GSK3β [68]; however, valproate and lithium increase serine phosphorylation via two different mechanisms, which results into a synergic enzyme inhibition when the two drugs are combined [145]. Valproate acts as a week inhibitor of histone deacetylases (HDACs), a mechanisms that is apparently not shared by lithium. HDAC inhibition enhances Akt phosphorylation, with ensuing inhibition of GSK3β [67,68,146,147]. In spite of this additional mechanism, valproate did not share the ability of lithium to inhibit GSK3β activity in cultured cortical neurons [148]. In cultured cerebellar granule cells lithium, but not valproate, inhibited GSK3β and was protective against apoptotic death [143]. In another study, however, both lithium and valproate were able to protect cultured granule cells against GSK3-mediated apoptosis [149]. Data of in vivo studies are not homogeneous. Kozlovsky et al., [150] showed that subchronic valproate treatment did not change GSK3β levels or activity in the adult rat frontal cortex. However, the same paradigm of valproate administration was found to increase the levels of Ser9 phosphorylated (inhibited)-GSK3β in the frontal cortex [68]. In another study, valproate administration attenuated hypoxia-induced dephosphorylation of brain GSK3α and GSK3β without altering total GSK3 protein content in mice [151].
The influence of valproate on the Wnt pathway is not restricted to the inhibition of GSK3β. Zhou et al., [152] have found that chronic treatment with valproate (or with lithium) induces changes in the hippocampal levels of the microRNAs, let-7b, let-7c, miR-128a, miR-30c, miR-221, and miR-144. Some of the mRNA targets for these miRNAs encode for proteins of the canonical Wnt pathway.
Human studies on valproate and the Wnt/GSK3β/β-catenin pathway have generated contrasting data. An eight-week treatment of BP patients with valproate, lithium, and/or atypical antipsychotics enhanced serine phosphorylation of GSK3 in peripheral blood mononuclear cells. Interestingly, concomitant electroconvulsive therapy prevented this effect [79]. Post-mortem studies did not show alterations in GSK3β and β-catenin levels [76,153,154], GSK3α and GSK3β mRNA levels, or total GSK3 activity [153] in the frontal cortex of BP patients. More importantly, no changes were found after treatment with mood stabilisers, including valproate [154].
Thus, whether and how precisely valproate influences Wnt signalling, and whether this contributes to the therapeutic efficacy of valproate in BPs, remains unclear.
Few studies have investigated the effect of treatment with antiepileptic drugs used as mood stabilisers, such as carbamazepine or lamotrigine, on GSK3β and other Wnt-related proteins. There is only an unpublished observation that chronic lamotrigine treatment increased serine phosphorylation of GSK3 in the mouse hippocampus or cerebral cortex (reported in [147]). Other studies consistently failed to show GSK3 inhibition by carbamazepine or lamotrigine [147,148,155] (Table 1).
Table 1.
Wnt Pathway Molecules Involved in the Action of Mood Stabilisers, Antipsychotics, and Antidepressants
| Wnt Molecules | ||||
|---|---|---|---|---|
| Drugs | GSK3 function | GSK3β Ser9 Phosphorylation Inactivation | AKT Phosphorylation | β-Catenin |
| Mood stabilisers | ||||
| Lithium | ↓ | ↑ | ⬄ | ↑ |
| Valproate | ⬄ | ↑ | ↑ | ↑ |
| Carbamazepine | ⬄ | ⬄ | n.d. | ⬄ |
| Lamotrigine | ⬄ | ⬄↑ | n.d. | n.d. |
| Antipsychotics | ||||
| Haloperidol | ↑ | ↑ | ↑, transient | ↑ |
| Clozapine | ↑ | ↑ | ↑ | ⬄-↑ |
| Risperidone | ↑ | ↑ | ⬄ | ↑ |
| Olanzapine | n.d. | ↑ | n.d. | n.d. |
| Quetiapine | n.d. | ↑ | n.d. | n.d. |
| Ziprasidone | n.d. | ↑ | n.d. | n.d. |
| Antidepressants | ||||
| Imipramine | ⬄ | ↑ | ↑ | n.d. |
| Fluoxetine | n.d. | ↑ | n.d. | ↑ |
| Fluvoxamine | n.d. | n.d. | ↑ | ↑ |
| Sertraline | n.d. | n.d. | ↓ | n.d. |
| Venlafaxine | n.d. | n.d. | * | ↑ |
increase;
decrease;
conflicting evidence or lack of effect; n.d., no data, not determined,
increases levels, but no data on phosphorylation.
8.2. Antipsychotic Drugs
Antipsychotics are used in patients with schizophrenia, in the manic phase of BP, in other psychotic disorders, like delusional disorder or shared psychotic disorder, and in depression with psychotic features. Atypical antipsychotic drugs antagonize 5-HT2A serotonin receptors, and, with the exception of risperidone and 9-hydroxy-risperidone, show a low D2 dopamine receptor occupancy and are therefore devoid of extrapyramidal side effects. It is generally believed that psychosis is associated with an increased activity of the meso-limbic dopaminergic system, and a reduced activity of the meso-cortical dopaminergic system [156-159]. Beaulieu et al., [47] showed that an increased dopaminergic transmission resulting from amphetamine administration or deletion of the high affinity dopamine transporter caused inactivation of Akt and concomitant activation of GSK3α and GSK3β in the striatum, an effect reversed by lithium or D2 receptor blockade. Others confirmed that dopaminergic drugs increase the activity of GSK3β [55,160], while antipsychotic drugs produce the opposite effect [69,161-165].
Clozapine, haloperidol, and risperidone were found to increase GSK3 phosphorylation, as well as Dvl-3 and β-catenin levels in the rat medial prefrontal cortex and striatum [166]. Levels of Dvl-3, GSK3, and β-catenin were also increased in the hippocampus and ventral midbrain following repeated antipsychotic treatment [167]. X. Li et al., [69] found that acute treatment with atypical antipsychotics, such as clozapine, risperidone, olanzapine, quetiapine, and ziprasidone, increased Ser9 phosphorylation of GSK3 in the mouse cerebral cortex, hippocampus, striatum, and cerebellum. There was a synergism between risperidone and antidepressants (monoamine oxidase inhibitors or fluoxetine) in enhancing GSK3 phosphorylation, an evidence that supports the use of risperidone in mood disorders [69]. Chronic treatment with clozapine or haloperidol also increased levels of Wnt-5a (but not Wnt1 and Wnt3a), Axin, Dvl-3, total and Ser9-phosphorylated GSK3, and β-catenin in the frontal cortex [162]. As outlined above, GSK3β can be phosphorylated on Ser9 by multiple signalling pathways including the canonical Wnt pathway and the PI3K/Akt pathway. Roh et al., [168] found that clozapine and haloperidol differentially regulate signals upstream of GSK3 in the rat frontal cortex. Both drugs were able to phosphorylate GSK3α/β on Ser9 and Ser21; however, only clozapine increased Dvl phosphorylation. In neuroblastoma cell lines showed that clozapine increased Ser9 phosphorylation of GSK3β via the activation of the canonical Wnt pathway, but not via the activation of the PI3K/Akt pathway [161]. Whether, and to what extent, haloperidol inhibits GSK3 via the PI3K/Akt pathway is matter of debate [169-171]. On the basis of these findings, it is counterintuitive that spiperone, an antipsychotic agent structurally related to haloperidol inhibits Wnt signalling. This unexpected effect is secondary to increases in intracellular free Ca2+ which results from a thapsigargin-like activity of spiperone at intracellular Ca2+ stores [172]. This adds further complexity to the mechanisms whereby antipsychotic drugs regulate Wnt signalling (see also Beaulieu [173].
The modulation of Wnt signalling by antipsychotic drugs might have a strong impact on the alterations of neuronal connectivity and cell fate associated with psychotic disorders. In a recent elegant study, Brennand et al., [174] demonstrated that fibroblasts from schizophrenic patients reprogrammed into pluripotent stem cells and then differentiated into neurons show diminished connectivity and an altered expression of many components of the Wnt pathway, including Axin2, Wnt2B, Wnt3, Pik3R3, TCF4, LEF1, RAP2A, LRP5, and Wnt7A. Interestingly, these alterations are corrected by treatment with loxapine, but not with other antipsychotics.
Taken together, these data suggest that antipsychotics share the ability of lithium and valproate to activate Wnt signalling through the inhibition of GSK3β or other mechanisms (Table 1). This may underlie the antimanic and mood-stabilising activity of antipsychotics in BP.
8.3. Antidepressants
Few studies investigated the action of antidepressant drugs on the Wnt pathway.
GSK3 activity is regulated by 5-HT2 and D2 receptors in specific neurons [175]. Serotonergic and dopaminergic mechanisms are involved in the action of all antidepressant drug classes, from tricyclic antidepressants and monoamine oxidase inhibitors to selective serotonin reuptake inhibitors (SSRIs) and serotonin and noradrenaline reuptake inhibitors (SNRIs). Much like antipsychotics and mood stabilisers, monoamine-regulating antidepressant drugs inhibit GSK3. For example, both imipramine and fluoxetine and imipramine greatly increased inhibitory serine GSK3 phosphorylation in the mouse brain [49,99]. However, we should stress that antidepressant drugs inhibit GSK3 activity a few hours after a single administration, whereas their therapeutic efficacy in MDD requires 3-4 weeks of daily administration. Thus, we may consider GSK3 inhibition as an initial event leading to slowly developing neuroadaptation, which underlies the therapeutic efficacy of antidepressants on mood disorders. Interestingly, Wnt signalling activation has been associated with antidepressant-induced increased hippocampal neurogenesis [176]. Accordingly, fluoxetine promotes neurogenesis in the hippocampal dentate gyrus by up-regulating Wnt3a [177], whereas subchronic fluoxetine increases non-nuclear β-catenin expression [178] and chronic treatment with venlafaxine enhances both the proliferation of neuro-progenitor cells and nuclear translocation of β-catenin in the hippocampus [179]. Antidepressants may affect the function of the canonical Wnt pathway through manipulation of Akt-1 phosphorylation, which is enhanced by fluvoxamine, both acutely [180] and chronically [181], and inhibited by sertraline [182]. Imipramine, like fluvoxamine, increased phospho-Ser473 Akt level, but did not affect total Akt levels [183]. Generally, antidepressants increase neuroplasticity through Wnt-related pathways or through pathways that affect sideways the canonical Wnt pathway. However, each drug may have its own specific actions which may be clinically important and contrasting on specific functions; for example, fluvoxamine increases Akt-phosphorylation through sigma1-receptors [180,181], while sertraline decreases it [182].
9. CONCLUSIONS
Data suggesting a possible involvement of the Wnt signalling pathway in the pathophysiology of BP and MDD are sound, but not always consistent. We should underline that Wnt signalling has not been studied in other mood disorders, such as dysthymic disorder or mood disorder, not otherwise specified. The Wnt-related protein that has been consistently associated with BP or MDD is GSK3β; however, this molecule is at the crossroads between other signalling pathways that also appear to be involved in mood and psychotic disorders (see Fig. 1). The relative contribution of the Wnt pathway and other signalling pathways to the dysregulation of GSK3β associated with BP or MDD remains to be established.
The action of some drugs used in mood disorders, particularly lithium, valproate, and antipsychotic drugs, involves the canonical Wnt pathway. These drugs regulate Wnt signalling through a number of mechanisms that are both drug-specific and brain region specific. Whether non-canonical Wnt pathways are also involved in the action of antipsychotic drugs is entirely unknown. Drugs that selectively activate the canonical Wnt pathway (e.g., selective GSK3 inhibitors) might improve mood disorders without the adverse effects associated with the use of the current antidepressants or mood stabilisers. However, the complexity of the mechanisms underlying the pathophysiology of mood disorders might favour the use of drugs with multiple mechanisms of action over the use of small molecule inhibitors of individual enzymes. This particular issue is critical to the design of new drugs in psychiatric disorders and warrants further investigation.
ACKNOWLEDGEMENTS
We gratefully acknowledge the contribution of the Librarians of the Sant’Andrea Hospital – Sapienza University, School of Medicine and Psychology Library, Ms. Felicia Proietti, Ms. Tiziana Mattei, and Ms. Mimma Ariano in facilitating our bibliographic consultation.
ABBREVIATIONS
- ACP1
= Acid phosphatase 1
- Akt
= Protein kinase B/Non-specific serine/threonine protein kinase family
- APC
= Adenomatous poliposys coli
- BP
= Bipolar disorder
- BMPs
= Bone Morphogenetic Proteins
- Ca2+
= Calcium ion
- Cdc42
= Cell division control protein 42
- CNV
= Copy number variation
- CUS
= Chronic unpredictable stress
- DAG
= Diacylglycerol
- Dvl
= Dishevelled
- EPM
= Elevated plus maze
- FGF
= Fibroblast growth factor
- FZD
= Frizzled
- GM
= Grey matter
- GSK3(α/β)
= Glycogen synthase kinase-3(alpha, beta)
- HDAC
= Histone deacetylase
- InsP3
= Inositol-1,4,5-trisphosphate
- LRP5/6
= Low Density Lipoprotein receptor-related protein 5 and -6
- LTP
= Long-term potentiation
- MAPK
= Mitogen-activated protein kinase
- Mg2+
= magnesium ions
- MDD
= Major Depressive Disorder
- NLK
= Nemo-like kinase
- PPARD
= Peroxisome proliferators-activated receptor type-δ
- PBMC
= Peripheral blood mononuclear cell
- PCP
= Planar Cell Polarity
- PI3K
= Phosphatidylinositol-3-kinase
- PKC
= Protein kinase C
- ROCK
= Rho-associated kinase
- SHH
= Sonic Hedgehog
- SNP
= Single Nucleotide Polymorphism
- TAK1
= Transforming growth factor-β-activated protein kinase
- TCF/LEF
= T-cell factor/lymphoid enhancer factor family of transcription factors
- Wnt
= Wingless
CONFLICT OF INTERESTS
Paolo Girardi has received in the past three years research support from Lilly and Janssen, has participated in Advisory Boards for Lilly, Organon, Pfizer, and Schering, and has received honoraria from Lilly and Organon; Giorgio D. Kotzalidis is the recipient of an Italian Ministry of Education Ph.D. Grant for Early Intervention in the Psychoses.
All other authors of this paper have no relevant affiliations or financial involvement with any organisation or entity with a financial interest in, or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties. No writing assistance was utilised in the production of this manuscript.
REFERENCES
- 1.Peifer M, Rauskolb C, Williams M, Riggleman B, Wieschaus E. The segment polarity gene armadillo interacts with the wingless signalling pathway in both embryonic and adult pattern formation. Development. 1991;111:1029–1043. doi: 10.1242/dev.111.4.1029. [DOI] [PubMed] [Google Scholar]
- 2.Ille F, Sommer L. Wnt signalling: multiple functions in neural development. Cell. Mol. Life Sci . 2005;62:1100–1108. doi: 10.1007/s00018-005-4552-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fišar Z, Hroudová J. Intracellular signalling pathways and mood disorders. Folia Biol (Praha) 2010;56:135–148. [PubMed] [Google Scholar]
- 4.De Ferrari GV, Moon RT. The ups and downs of Wnt signalling in prevalent neurological disorders. Oncogene. 2006;25:7545–7553. doi: 10.1038/sj.onc.1210064. [DOI] [PubMed] [Google Scholar]
- 5.Cotter D, Kerwin R, al-Sarraji S, Brion JP, Chadwich A, Lovestone S, Anderton B, Everall I. Abnormalities of Wnt signalling in schizophrenia-evidence for neurodevelopmental abnormality. Neuroreport. 1998;9:1379–1383. doi: 10.1097/00001756-199805110-00024. [DOI] [PubMed] [Google Scholar]
- 6.Miyaoka T, Seno H, Ishino H. Increased expression of Wnt-1 in schizophrenic brains. Schizophr. Res. 1999;38:1–6. doi: 10.1016/s0920-9964(98)00179-0. [DOI] [PubMed] [Google Scholar]
- 7.Klein PS, Melton DA. A molecular mechanism for the effect of lithium on development. Proc. Natl. Acad. Sci. U. S. A . 1996;93:8455–8459. doi: 10.1073/pnas.93.16.8455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hedgepeth CM, Conrad LJ, Zhang J, Huang HC, Lee VM, Klein PS. Activation of the Wnt signalling pathway: a molecular mechanism for lithium action. Dev. Biol. 1997;185:82–91. doi: 10.1006/dbio.1997.8552. [DOI] [PubMed] [Google Scholar]
- 9.Detera-Wadleigh SD. Lithium-related genetics of bipolar disorder. Ann. Med. 2001;33:272–285. doi: 10.3109/07853890108998756. [DOI] [PubMed] [Google Scholar]
- 10.Gould TD, Manji HK. Signalling networks in the pathophysiology and treatment of mood disorders. J. Psychosom. Res. 2002;53:687–697. doi: 10.1016/s0022-3999(02)00426-9. [DOI] [PubMed] [Google Scholar]
- 11.Gould TD, Dow ER, O’Donnell KC, Chen G, Manji HK. Targeting signal transduction pathways in the treatment of mood disorders: recent insights into the relevance of the Wnt pathway. CNS Neurol. Disord. Drug Targets. 2007;6:193–204. doi: 10.2174/187152707780619308. [DOI] [PubMed] [Google Scholar]
- 12.Hu LW, Kawamoto EM, Brietzke E, Scavone C, Lafer B. The role of Wnt signalling and its interaction with diverse mechanisms of cellular apoptosis in the pathophysiology of bipolar disorder. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2011;35:11–17. doi: 10.1016/j.pnpbp.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 13.Komiya Y, Habas R. Wnt signal transduction pathways. Organogenesis . 2008;4:68–75. doi: 10.4161/org.4.2.5851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lie DC, Colamarino SA, Song HJ, Desire L, Mira H, Consiglio A, Lein ES, Jessberger S, Lansford H, Dearie AR, Gage FH. Wnt signalling regulates adult hippocampal neurogenesis. Nature. 2005;437:1370–1375. doi: 10.1038/nature04108. [DOI] [PubMed] [Google Scholar]
- 15.Logan CW, Nusse R. The Wnt signalling pathway in development and disease. Cell. Dev. Biol. 2004;20:781–810. doi: 10.1146/annurev.cellbio.20.010403.113126. [DOI] [PubMed] [Google Scholar]
- 16.Okerlund ND, Cheyette BNR. Synaptic Wnt signalling. A contributor to major psychiatric disorders? J. Neurodev. Disord. 2011;3:162–174. doi: 10.1007/s11689-011-9083-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gao C, Chen YG. Dishevelled: The hub of Wnt signalling. Cell. Signal. 2010;22:717–727. doi: 10.1016/j.cellsig.2009.11.021. [DOI] [PubMed] [Google Scholar]
- 18.Doble BW, Woodgett JR. GSK-3: tricks of the trade for a multitasking kinase. J. Cell. Sci. 2003;116:1175–1186. doi: 10.1242/jcs.00384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gurvich N, Klein PS. Lithium and valproic acid: parallels and contrasts in diverse signalling contexts. Pharmacol. Ther. 2002;96:45–66. doi: 10.1016/s0163-7258(02)00299-1. [DOI] [PubMed] [Google Scholar]
- 20.McManus EJ, Sakamoto K, Armit LJ, Ronaldson L, Shpiro N, Marquez R, Alessi DR. Role that phosphorylation of GSK3 plays in insulin and Wnt signalling defined by knockin analysis. EMBO J. 2005;24:1571–1583. doi: 10.1038/sj.emboj.7600633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fukumoto S, Hsieh CM, Maemura K, Layne MD, Yet SF, Lee KH, Matsui T, Rosenzweig A, Taylor WG, Rubin JS, Perrella MA, Lee ME. Akt participation in the Wnt signalling pathway through Dishevelled. J. Biol. Chem. 2001;276:17479–17483. doi: 10.1074/jbc.C000880200. [DOI] [PubMed] [Google Scholar]
- 22.Sugimura R, Li L. Noncanonical Wnt signalling in vertebrate development, stem cells, and diseases. Birth Defects Res. C Embryo Today. 2010;90:243–256. doi: 10.1002/bdrc.20195. [DOI] [PubMed] [Google Scholar]
- 23.Ishitani T, Ninomiya-Tsuji J, Nagai S, Nishita M, Meneghini M, Barker N, Waterman M, Bowerman B, Clevers H, Shibuya H, Matsumoto K. The TAK1-NLK-MAPK-related pathway antagonizes signalling between β-catenin and transcription factor TCF. Nature. 1999;399:798–802. doi: 10.1038/21674. [DOI] [PubMed] [Google Scholar]
- 24.Ishitani T, Kishida S, Hyodo-Miura J, Ueno N, Yasuda J, Waterman M, Shibuya H, Moon RT, Ninomiya-Tsuji J, Matsumoto K. The TAK1-NLK mitogen-activated protein kinase cascade functions in the Wnt-5a/Ca2+ pathway to antagonize Wnt/beta-catenin signalling. Mol. Cell. Biol. 2003;23:131–139. doi: 10.1128/MCB.23.1.131-139.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li M, Wang H, Huang T, Wang J, Ding Y, Li Z, Zhang J, Li L. TAB2 scaffolds TAK1 and NLK in repressing canonical Wnt signalling. J. Biol. Chem . 2010;285:13397–13404. doi: 10.1074/jbc.M109.083246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kohn AD, Moon RT. Wnt and calcium signalling: β-Catenin-independent pathways. Cell Calcium. 2005;38:439–446. doi: 10.1016/j.ceca.2005.06.022. [DOI] [PubMed] [Google Scholar]
- 27.Habas R, He X. Activation of Rho and Rac by Wnt/frizzled signalling. Methods Enzymol. 2006;406:500–511. doi: 10.1016/S0076-6879(06)06038-1. [DOI] [PubMed] [Google Scholar]
- 28.Mlodzik M. Planar cell polarisation: do the same mechanisms regulate Drosophila tissue polarity and vertebrate gastrulation? Trends Genet. 2002;18:564–571. doi: 10.1016/s0168-9525(02)02770-1. [DOI] [PubMed] [Google Scholar]
- 29.Simons M, Mlodzik M. Planar cell polarity signalling: from fly development to human disease. Annu. Rev. Genet . 2008;42:517–540. doi: 10.1146/annurev.genet.42.110807.091432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stevens HE, Smith KM, Rash BG, Vaccarino FM. Neural stem cell regulation, fibroblast growth factors, and the developmental origins of neuropsychiatric disorders. Front. Neurosci. 2010;4:59. doi: 10.3389/fnins.2010.00059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thomas KR, Capecchi MR. Targeted disruption of the murine int-1 proto-oncogene resulting in severe abnormalities in midbrain and cerebellar development. Nature. 1990;346:847–850. doi: 10.1038/346847a0. [DOI] [PubMed] [Google Scholar]
- 32.Machon O, Backman M, Machonova O, Kozmik Z, Vacik T, Andersen L, Krauss S. A dynamic gradient of Wnt signalling controls initiation of neurogenesis in the mammalian cortex and cellular specification in the hippocampus. Dev. Biol. 2007;311:223–237. doi: 10.1016/j.ydbio.2007.08.038. [DOI] [PubMed] [Google Scholar]
- 33.Patapoutian A, Reichardt LF. Roles of Wnt proteins in neural development and maintenance. Curr. Opin. Neurobiol. 2000;10:392–399. doi: 10.1016/s0959-4388(00)00100-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hur EM, Zhou FQ. GSK3 signalling in neural development. Nat. Rev. Neurosci. 2010;11:539–551. doi: 10.1038/nrn2870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cerpa W, Toledo EM, Varela-Nallar L, Inestrosa NC. The role of Wnt signalling in neuroprotection. Drug News Perspect. 2009;22:579–591. doi: 10.1358/dnp.2009.10.1436817. [DOI] [PubMed] [Google Scholar]
- 36.Harrison PJ, Weinberger DR. Schizophrenia genes, gene expression, and neuropathology: on the matter of their convergence. Mol. Psychiatry . 2005;10:40–68. doi: 10.1038/sj.mp.4001558. Errata corrige 10, 420; 10, 804. [DOI] [PubMed] [Google Scholar]
- 37.Fatemi SH, Folsom TD. The neurodevelopmental hypothesis of schizophrenia, revisited. Schizophr. Bull. 2009;35:528–548. doi: 10.1093/schbul/sbn187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guilmatre A, Dubourg C, Mosca AL, Legallic S, Goldenberg A, Drouin-Garraud V, Layet V, Rosier A, Briault S, Bonnet-Brilhault F, Laumonnier F, Odent S, Le Vacon G, Joly-Helas G, David V, Bendavid C, Pinoit JM, Henry C, Impallomeni C, Germano E, Tortorella G, Di Rosa G, Barthelemy C, Andres C, Faivre L, Frébourg T, Saugier Veber P, Campion D. Recurrent rearrangements in synaptic and neurodevelopmental genes and shared biologic pathways in schizophrenia, autism, and mental retardation. Arch. Gen. Psychiatry. 2009;66:947–956. doi: 10.1001/archgenpsychiatry.2009.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Blumberg HP, Kaufman J, Martin A, Charney DS, Krystal JH, Peterson BS. Significance of adolescent neurodevelopment for the neural circuitry of bipolar disorder. Ann. N. Y. Acad. Sci . 2004;1021 :376–383. doi: 10.1196/annals.1308.048. [DOI] [PubMed] [Google Scholar]
- 40.Vaidya CJ. Neurodevelopmental abnormalities in ADHD. Curr. Top. Behav. Neurosci. 2011. May 4, Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 41.Sutcliffe JS. Heterogeneity and the design of genetic studies in autism. Autism Res. 2008;1:205–206. doi: 10.1002/aur.37. [DOI] [PubMed] [Google Scholar]
- 42.Bourgeron T, Leboyer M, Delorme R. Autism: more evidence of a genetic cause. Bull. Acad. Natl. Med. 2009;193:299–305. [PubMed] [Google Scholar]
- 43.Lovestone S, Killick R, Di Forti M, Murray R. Schizophrenia as a GSK-3 dysregulation disorder. Trends Neurosci. 2007;30:142–149. doi: 10.1016/j.tins.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 44.Scassellati C, Bonvicini C, Perez J, Bocchio-Chiavetto L, Tura GB, Rossi G, Racagni G, Gennarelli M. Association study of -1727 A/T, -50 C/T and (CAA)n repeat GSK-3beta gene polymorphisms with schizophrenia. Neuropsychobiology. 2004;50:16–20. doi: 10.1159/000077936. [DOI] [PubMed] [Google Scholar]
- 45.Kozlovsky N, Belmaker RH, Agam G. GSK-3 and the neurodevelopmental hypothesis of schizophrenia. Eur. Neuropsychopharmacol. 2002;12:13–25. doi: 10.1016/s0924-977x(01)00131-6. [DOI] [PubMed] [Google Scholar]
- 46.O’Brien WT, Harper AD, Jové F, Woodgett JR, Maretto S, Piccolo S, Klein PS. Glycogen synthase kinase-3beta haploinsufficiency mimics the behavioral and molecular effects of lithium. J. Neurosci. 2004;24:6791–6798. doi: 10.1523/JNEUROSCI.4753-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Beaulieu JM, Sotnikova TD, Yao WD, Kockeritz L, Woodgett JR, Gainetdinov RR, Caron MG. Lithium antagonizes dopamine-dependent behaviors mediated by an AKT/glycogen synthase kinase 3 signalling cascade. Proc. Natl. Acad. Sci. U. S. A. 2004;101:5099–5104. doi: 10.1073/pnas.0307921101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Spittaels K, Van den Haute C, Van Dorpe J, Terwel D, Vandezande K, Lasrado R, Bruynseels K, Irizarry M, Verhoye M, Van Lint J, Vandenheede JR, Ashton D, Mercken M, Loos R, Hyman B, Van der Linden A, Geerts H, Van Leuven F. Neonatal neuronal overexpression of glycogen synthase kinase-3 beta reduces brain size in transgenic mice. Neuroscience. 2002;113:797–808. doi: 10.1016/s0306-4522(02)00236-1. [DOI] [PubMed] [Google Scholar]
- 49.Beaulieu JM, Zhang X, Rodriguiz RM, Sotnikova TD, Cools MJ, Wetsel WC, Gainetdinov RR, Caron MG. Role of GSK3β in behavioral abnormalities induced by serotonin deficiency. Proc. Natl. Acad. Sci. U. S. A. 2008;105:1333–1338. doi: 10.1073/pnas.0711496105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bersudsky Y, Shaldubina A, Kozlovsky N, Woodgett JR, Agam G, Belmaker RH. Glycogen synthase kinase-3β heterozygote knockout mice as a model of findings in postmortem schizophrenia brain or as a model of behaviors mimicking lithium action: negative results. Behav. Pharmacol . 2008;19:217–224. doi: 10.1097/FBP.0b013e3282feb099. [DOI] [PubMed] [Google Scholar]
- 51.Prickaerts J, Moechars D, Cryns K, Lenaerts I, van Craenendonck H, Goris I, Daneels G, Bouwknecht JA, Steckler T. Transgenic mice overexpressing glycogen synthase kinase 3beta: a putative model of hyperactivity and mania. J. Neurosci . 2006;26:9022–9029. doi: 10.1523/JNEUROSCI.5216-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ackermann TF, Kempe DS, Lang F, Lang UE. Hyperactivity and enhanced curiosity of mice expressing PKB/SGK-resistant glycogen synthase kinase-3 (GSK-3) Cell. Physiol. Biochem. 2010;25:775–786. doi: 10.1159/000315097. [DOI] [PubMed] [Google Scholar]
- 53.Wilkinson MB, Dias C, Magida J, Mazei-Robison M, Lobo M, Kennedy P, Dietz D, Covington H, Russo S, Neve R, Ghose S, Tamminga C, Nestler EJ. A novel role of the WNT-dishevelled-GSK3β signalling cascade in the mouse nucleus accumbens in a social defeat model of depression. J. Neurosci . 2011;31:9084–9092. doi: 10.1523/JNEUROSCI.0039-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kaidanovich-Beilin O, Lipina TV, Takao K, van Eede M, Hattori S, Laliberté C, Khan M, Okamoto K, Chambers JW, Fletcher PJ, MacAulay K, Doble BW, Henkelman M, Miyakawa T, Roder J, Woodgett JR. Abnormalities in brain structure and behavior in GSK-3alpha mutant mice. Mol. Brain. 2009;2:35. doi: 10.1186/1756-6606-2-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Polter A, Beurel E, Yang S, Garner R, Song L, Miller CA, Sweatt JD, McMahon L, Bartolucci AA, Li X, Jope RS. Deficiency in the inhibitory serine-phosphorylation of glycogen synthase kinase-3 increases sensitivity to mood disturbances. Neuropsychopharmacology. 2010;35:1761–1774. doi: 10.1038/npp.2010.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liang MH, Chuang DM. Differential roles of glycogen synthase kinase-3 isoforms in the regulation of transcriptional activation. J. Biol. Chem. 2006;281:30479–30484. doi: 10.1074/jbc.M607468200. [DOI] [PubMed] [Google Scholar]
- 57.Liang MH, Chuang DM. Regulation and function of glycogen synthase kinase-3 isoforms in neuronal survival. J. Biol. Chem. 2007;282:3904–3917. doi: 10.1074/jbc.M605178200. [DOI] [PubMed] [Google Scholar]
- 58.Lucas JJ, Hernández F, Gómez-Ramos P, Morán MA, Hen R, Avila J. Decreased nuclear beta-catenin, tau hyperphosphorylation and neurodegeneration in GSK-3beta conditional transgenic mice. EMBO J. 2001;20:27–39. doi: 10.1093/emboj/20.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gould TD, Einat H, Bhat R, Manji HK. AR-A014418, a selective GSK-3 inhibitor, produces antidepressant-like effects in the forced swim test. Int. J. Neuropsychopharmacol. 2004;7:387–390. doi: 10.1017/S1461145704004535. [DOI] [PubMed] [Google Scholar]
- 60.Kaidanovich-Beilin O, Milman A, Weizman A, Pick CG, Eldar-Finkelman H. Rapid antidepressive-like activity of specific glycogen synthase kinase-3 inhibitor and its effect on beta-catenin in mouse hippocampus. Biol. Psychiatry. 2004;55:781–784. doi: 10.1016/j.biopsych.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 61.Rosa AO, Kaster MP, Binfaré RW, Morales S, Martín-Aparicio E, Navarro-Rico ML, Martinez A, Medina M, García AG, López MG, Rodrigues AL. Antidepressant-like effect of the novel thiadiazolidinone NP031115 in mice. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2008;32:1549–1556. doi: 10.1016/j.pnpbp.2008.05.020. [DOI] [PubMed] [Google Scholar]
- 62.Kaladchibachi SA, Doble B, Anthopoulos N, Woodgett JR, Manoukian AS. Glycogen synthase kinase 3, circadian rhythms, and bipolar disorder: a molecular link in the therapeutic action of lithium. J. Circadian Rhythms . 2007;5:3. doi: 10.1186/1740-3391-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schloesser RJ, Huang J, Klein PS, Manji HK. Cellular plasticity cascades in the pathophysiology and treatment of bipolar disorder. Neuropsychopharmacology. 2008;33:110–133. doi: 10.1038/sj.npp.1301575. [DOI] [PubMed] [Google Scholar]
- 64.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition-Text Revision (DSMIVTR) Washington, D.C: American Psychiatric Publishing; 2000. pp. 345–428. [Google Scholar]
- 65.Gould TD, Quiroz JA, Singh J, Zarate CA, Manji HK. Emerging experimental therapeutics for bipolar disorder: insights from the molecular and cellular actions of current mood stabilisers. Mol. Psychiatry. 2004;9:734–755. doi: 10.1038/sj.mp.4001518. [DOI] [PubMed] [Google Scholar]
- 66.Chen G, Huang LD, Jiang YM, Manji HK. The mood-stabilizing agent valproate inhibits the activity of glycogen synthase kinase-3. J. Neurochem. 1999;72:1327–1330. doi: 10.1046/j.1471-4159.2000.0721327.x. [DOI] [PubMed] [Google Scholar]
- 67.De Sarno P, Li X, Jope RS. Regulation of Akt and glycogen synthase kinase-3 beta phosphorylation by sodium valproate and lithium. Neuropharmacology. 2002;43:1158–1164. doi: 10.1016/s0028-3908(02)00215-0. [DOI] [PubMed] [Google Scholar]
- 68.Kozlovsky N, Amar S, Belmaker RH, Agam G. Psychotropic drugs affect Ser9-phosphorylated GSK-3 beta protein levels in rodent frontal cortex. Int. J. Neuropsychopharmacol. 2006;9:337–342. doi: 10.1017/S1461145705006097. [DOI] [PubMed] [Google Scholar]
- 69.Li X, Rosborough KM, Friedman AB, Zhu W, Roth KA. Regulation of mouse brain glycogen synthase kinase-3 by atypical antipsychotics. Int. J. Neuropsychopharmacol. 2007;10:7–19. doi: 10.1017/S1461145706006547. [DOI] [PubMed] [Google Scholar]
- 70.Rowe MK, Wiest C, Chuang DM. GSK-3 is a viable potential target for therapeutic intervention in bipolar disorder. Neurosci. Biobehav. Rev. 2007;31:920–931. doi: 10.1016/j.neubiorev.2007.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gould TD, Chen G, Manji HK. In vivo evidence in the brain for lithium inhibition of glycogen synthase kinase-3. Neuropsychopharmacology. 2004;29:32–38. doi: 10.1038/sj.npp.1300283. [DOI] [PubMed] [Google Scholar]
- 72.Drevets WC, Price JL, Simpson JR , Jr, Todd RD, Reich T, Vannier M, Raichle ME. Subgenual prefrontal cortex abnormalities in mood disorders. Nature. 1997;386:824–827. doi: 10.1038/386824a0. [DOI] [PubMed] [Google Scholar]
- 73.Ongür D, Drevets WC, Price JL. Glial reduction in the subgenual prefrontal cortex in mood disorders. Proc. Natl. Acad. Sci. U. S. A. 1998;95:13290–13295. doi: 10.1073/pnas.95.22.13290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rajkowska G, Miguel-Hidalgo JJ, Wei J, Dilley G, Pittman SD, Meltzer HY, Overholser JC, Roth BL, Stockmeier CA. Morphometric evidence for neuronal and glial prefrontal cell pathology in major depression. Biol. Psychiatry. 1999;45:1085–1098. doi: 10.1016/s0006-3223(99)00041-4. [DOI] [PubMed] [Google Scholar]
- 75.Kozlovsky N, Belmaker RH, Agam G. Low GSK-3beta immunoreactivity in postmortem frontal cortex of schizophrenic patients. Am. J. Psychiatry. 2000;157:831–833. doi: 10.1176/appi.ajp.157.5.831. [DOI] [PubMed] [Google Scholar]
- 76.Lesort M, Greendorfer A, Stockmeier C, Johnson GV, Jope RS. Glycogen synthase kinase-3β, β-catenin, and t in postmortem bipolar brain. J. Neural Transm. 1999;106:1217–1222. doi: 10.1007/s007020050235. [DOI] [PubMed] [Google Scholar]
- 77.Li X, Friedman AB, Roh MS, Jope RS. Anesthesia and post-mortem interval profoundly influence the regulatory serinephosphorylation of glycogen synthase kinase-3 in mouse brain. J. Neurochem. 2005;92:701–704. doi: 10.1111/j.1471-4159.2004.02898.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Li X, Friedman AB, Zhu W, Wang L, Boswell S, May RS, Davis LL, Jope RS. Lithium regulates glycogen synthase kinase-3beta in human peripheral blood mononuclear cells: implication in the treatment of bipolar disorder. Biol. Psychiatry. 2007;61:261–222. doi: 10.1016/j.biopsych.2006.02.027. Erratum, 61, 261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Li X, Liu M, Cai Z, Wang G, Li X. Regulation of glycogen synthase kinase-3 during bipolar mania treatment. Bipolar Disord. 2010;12:741–752. doi: 10.1111/j.1399-5618.2010.00866.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Saus E, Soria V, Escaramís G, Crespo JM, Valero J, Gutiérrez-Zotes A, Martorell L, Vilella E, Menchón JM, Estivill X, Gratacòs M, Urretavizcaya M. A haplotype of glycogen synthase kinase 3β is associated with early onset of unipolar major depression. Genes Brain Behav. 2010;9:799–807. doi: 10.1111/j.1601-183X.2010.00617.x. [DOI] [PubMed] [Google Scholar]
- 81.Matigian N, Windus L, Smith H, Filippich C, Pantelis C, McGrath J, Mowry B, Hayward N. Expression profiling in monozygotic twins discordant for bipolar disorder reveals dysregulation of the WNT signalling pathway. Mol. Psychiatry. 2007;12:815–825. doi: 10.1038/sj.mp.4001998. [DOI] [PubMed] [Google Scholar]
- 82.Benedetti F, Serretti A, Colombo C, Lorenzi C, Tubazio V, Smeraldi E. A glycogen synthase kinase 3-beta promoter gene single nucleotide polymorphism is associated with age at onset and response to total sleep deprivation in bipolar depression. Neurosci. Lett. 2004;368:123–126. doi: 10.1016/j.neulet.2004.06.050. [DOI] [PubMed] [Google Scholar]
- 83.Benedetti F, Bernasconi A, Lorenzi C, Pontiggia A, Serretti A, Colombo C, Smeraldi E. A single nucleotide polymorphism in glycogen synthase kinase 3-β promoter gene influences onset of illness in patients affected by bipolar disorder. Neurosci. Lett. 2004;355:37–40. doi: 10.1016/j.neulet.2003.10.021. [DOI] [PubMed] [Google Scholar]
- 84.Benedetti F, Serretti A, Pontiggia A, Bernasconi A, Lorenzi C, Colombo C, Smeraldi E. Long-term response to lithium salts in bipolar illness is influenced by the glycogen synthase kinase 3-β –50 T/C SNP. Neurosci. Lett . 2005;376:51–55. doi: 10.1016/j.neulet.2004.11.022. [DOI] [PubMed] [Google Scholar]
- 85.Youn-Jung L Yong-Ku K. The impact of glycogen synthase kinase 3β gene on psychotic mania in bipolar disorder patients. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2011;35:1303–1308. doi: 10.1016/j.pnpbp.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 86.Zandi PP, Belmonte PL, Willour VL, Goes FS, Badner JA, Simpson SG, Gershon ES, McMahon FJ, DePaulo JR, Jr, Potash JB. Bipolar Disorder Phenome Group, National Institute of Mental Health Genetics Initiative Bipolar Disorder Consortium. Association study of Wnt signalling pathway genes in bipolar disorder. Arch. Gen. Psychiatry. 2008;65:785–793. doi: 10.1001/archpsyc.65.7.785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lachman HM. Pedrosa E, Petruolo OA. Cockerham M, Papolos A. Novak T, Papolos DF. Stopkova P. Increase in GSK3β gene copy number variation in bipolar disorder. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2007;144B:259–265. doi: 10.1002/ajmg.b.30498. [DOI] [PubMed] [Google Scholar]
- 88.Luykx JJ, Boks MP, Terwindt AP, Bakker S, Kahn RS. The involvement of GSK3β in bipolar disorder: integrating evidence from multiple types of genetic studies. Eur. Neuropsychopharmacol. 2010;20:357–368. doi: 10.1016/j.euroneuro.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 89.Pandey GN, Ren X, Rizavi HS, Dwivedi Y. Glycogen synthase kinase-3β in the platelets of patients with mood disorders: effect of treatment. J. Psychiatr. Res . 2010;44:143–148. doi: 10.1016/j.jpsychires.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 90.Hashimoto R, Suzuki T, Iwata N, Yamanouchi Y, Kitajima T, Kosuga A, Tatsumi M, Osaki N, Kamijima K, Kunugi H. Association study of the frizzled-3 (FZD3) gene with schizophrenia and mood disorders. J. Neural Transm. 2005;112:303–307. doi: 10.1007/s00702-004-0264-2. [DOI] [PubMed] [Google Scholar]
- 91.Okamoto H, Voleti B, Banasr M, Sarhan M, Duric V, Girgenti MJ, Dileone RJ, Newton SS, Duman RS. Wnt2 expression and signalling is increased by different classes of antidepressant treatments. Biol. Psychiatry. 2010;68:521–527. doi: 10.1016/j.biopsych.2010.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Voleti B, Tanis KQ, Newton SS, Duman RS. Analysis of target genes regulated by chronic electroconvulsive therapy reveals role for Fzd6 in depression. Biol. Psychiatry. 2012;71:51–58. doi: 10.1016/j.biopsych.2011.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ciani L, Boyle KA, Dickins E, Sahores M, Anane D, Lopes DM, Gibb AJ, Salinas PC. Wnt7a signalling promotes dendritic spine growth and synaptic strength through Ca2+/ Calmodulin-dependent protein kinase II. Proc. Natl. Acad. Sci. U. S. A. 2011;108:10732–10737. doi: 10.1073/pnas.1018132108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sahores M, Gibb A, Salinas PC. Frizzled-5, a receptor for the synaptic organizer Wnt7a, regulates activity-mediated synaptogenesis. Development. 2010;137:2215–2225. doi: 10.1242/dev.046722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Schulte G, Bryja V. The Frizzled family of unconventional Gprotein-coupled receptors. Trends Pharmacol. Sci. 2007;28:518–525. doi: 10.1016/j.tips.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 96.Banasr M, Valentine GW, Li XY, Gourley SL, Taylor JR, Duman RS. Chronic unpredictable stress decreases cell proliferation in the cerebral cortex of the adult rat. Biol. Psychiatry. 2007;62:496–504. doi: 10.1016/j.biopsych.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 97.Banasr M, Duman RS. Glial loss in the prefrontal cortex is sufficient to induce depressive-like behaviors. Biol. Psychiatry. 2008;64:863–870. doi: 10.1016/j.biopsych.2008.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yu X, Malenka RC. β-catenin is critical for dendritic morphogenesis. Nat. Neurosci. 2003;6:1169–1177. doi: 10.1038/nn1132. [DOI] [PubMed] [Google Scholar]
- 99.Li X, Zhu W, Roh MS, Friedman AB, Rosborough K, Jope RS. In vivo regulation of glycogen synthase kinase-3β (GSK3β) by serotonergic activity in mouse brain. Neuropsychopharmacology. 2004;29:1426–1431. doi: 10.1038/sj.npp.1300439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Inkster B, Nichols TE, Saemann PG, Auer DP, Holsboer F, Muglia P, Matthews PM. Pathway-based approaches to imaging genetics association studies: Wnt signalling, GSK3beta substrates and major depression. NeuroImage. 2010;53:908–917. doi: 10.1016/j.neuroimage.2010.02.065. [DOI] [PubMed] [Google Scholar]
- 101.Inkster B, Nichols TE, Saemann PG, Auer DP, Holsboer F, Muglia P, Matthews PM. Association of GSK3β polymorphisms with brain structural changes in major depressive disorder. Arch. Gen. Psychiatry. 2009;66:721–728. doi: 10.1001/archgenpsychiatry.2009.70. [DOI] [PubMed] [Google Scholar]
- 102.Tsai SJ, Liou YJ, Hong CJ, Yu YW, Chen TJ. Glycogen synthase kinase-3β gene is associated with antidepressant treatment response in Chinese major depressive disorder. Pharmacogenom., J. 2008,;8:384–390. doi: 10.1038/sj.tpj.6500486. [DOI] [PubMed] [Google Scholar]
- 103.Karege F, Perroud N, Burkhardt S, Schwald M, Ballmann E, La Harpe R, Malafosse A. Alteration in kinase activity but not in protein levels of protein kinase B and glycogen synthase kinase-3beta in ventral prefrontal cortex of depressed suicide victims. Biol. Psychiatry. 2007;61:240–245. doi: 10.1016/j.biopsych.2006.04.036. [DOI] [PubMed] [Google Scholar]
- 104.Oh DH, Park YC, Kim SH. Increased glycogen synthase kinase-3β mRNA level in the hippocampus of patients with major depression: a study using the stanley neuropathology consortium integrative database. Psychiatry Investig. 2010;7:202–207. doi: 10.4306/pi.2010.7.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yooh HK, Kim YK. Association between glycogen synthase kinase-3β gene polymorphisms and major depression and suicidal behavior in a Korean population. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2010;34:331–334. doi: 10.1016/j.pnpbp.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 106.Willour VL, Seifuddin F, Mahon PB, Jancic D, Pirooznia M, Steele J, Schweizer B, Goes FS, Mondimore FM, Mackinnon DF, Perlis RH, Lee PH, Huang J, Kelsoe JR, Shilling PD, Rietschel M, Nöthen M, Cichon C, Gurlings H, Purcell S, Smoller JW, Craddock N, Depaulo JR, Jr, Schulze TG, McMahon FJ, Zandi PP, Potash JB. A genome-wide association study of attempted suicide. The Bipolar Genome Study (BiGS) Consortium. Mol. Psychiatry. 2011. [DOI] [PMC free article] [PubMed]
- 107.Manji HK, Bebchuk JM, Moore GJ, Glitz D, Hasanat KA, Chen G. Modulation of CNS signal transduction pathways and gene expression by mood-stabilizing agents: therapeutic implications. J. Clin. Psychiatry. 1999;60 (Suppl 2 ):27–39. [PubMed] [Google Scholar]
- 108.Beaulieu JM, Caron MG. Looking at lithium: molecular moods and complex behaviour. Mol. Interv. 2008;8:230–241. doi: 10.1124/mi.8.5.8. [DOI] [PubMed] [Google Scholar]
- 109.Quiroz JA, Gould TD, Manji HK. Molecular effects of lithium. Mol. Interv. 2004;4:259–272. doi: 10.1124/mi.4.5.6. [DOI] [PubMed] [Google Scholar]
- 110.Nonaka S, Chuang DM. Neuroprotective effects of chronic lithium on focal cerebral ischemia in rats. Neuroreport. 1998;9:2081–2084. doi: 10.1097/00001756-199806220-00031. [DOI] [PubMed] [Google Scholar]
- 111.Nonaka S, Hough CJ, Chuang DM. Chronic lithium treatment robustly protects neurons in the central nervous system against excitotoxicity by inhibiting N-methyl-D-aspartate receptor-mediated calcium influx. Proc. Natl. Acad. Sci. U. S. A. 1998;95:2642–2647. doi: 10.1073/pnas.95.5.2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Nonaka S, Katsube N, Chuang DM. Lithium protects rat cerebellar granule cells against apoptosis induced by anticonvulsants, phenytoin and carbamazepine. J. Pharmacol. Exp. Ther. 1998;286:539–547. [PubMed] [Google Scholar]
- 113.Alvarez G, Muñoz-Montaño JR, Satrústegui J, Avila J, Bogónez E, Díaz-Nido J. Lithium protects cultured neurons against beta-amyloid-induced neurodegeneration. FEBS Lett. 1999;453:260–264. doi: 10.1016/s0014-5793(99)00685-7. [DOI] [PubMed] [Google Scholar]
- 114.Alvarez G, Muñoz-Montaño JR, Satrústegui J, Avila J, Bogónez E, Díaz-Nido J. Regulation of tau phosphorylation and protection against beta-amyloid-induced neurodegeneration by lithium. Bipolar Disord. 2002;4:153–165. doi: 10.1034/j.1399-5618.2002.01150.x. [DOI] [PubMed] [Google Scholar]
- 115.Wei H, Leeds PR, Qian Y, Wei W, Chen R, Chuang D. β-amyloid peptide-induced death of PC 12 cells and cerebellar granule cell neurons is inhibited by long-term lithium treatment. Eur. J. Pharmacol. 2000;392:117–123. doi: 10.1016/s0014-2999(00)00127-8. [DOI] [PubMed] [Google Scholar]
- 116.Wei H, Qin ZH, Senatorov VV, Wei W, Wang Y, Qian Y, Chuang DM. Lithium suppresses excitotoxicity-induced striatal lesions in a rat model of Huntington's disease. Neuroscience. 2001;106:603–612. doi: 10.1016/s0306-4522(01)00311-6. [DOI] [PubMed] [Google Scholar]
- 117.Manji HK, Moore GJ, Chen G. Lithium at 50: have the neuroprotective effects of this unique cation been overlooked? Biol. Psychiatry. 1999;46:929–940. doi: 10.1016/s0006-3223(99)00165-1. [DOI] [PubMed] [Google Scholar]
- 118.Chalecka-Franaszek E, Chuang DM. Lithium activates the serine/threonine kinase Akt-1 and suppresses glutamate-induced inhibition of Akt-1 activity in neurons. Proc. Natl. Acad. Sci. U. S. 1999;96:8745–8750. doi: 10.1073/pnas.96.15.8745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Beaulieu JM, Marion S, Rodriguiz RM, Medvedev IO, Sotnikova TD, Ghisi V, Wetsel WC, Lefkowitz RJ, Gainetdinov RR, Caron MG. A beta-arrestin 2 signalling complex mediates lithium action on behavior. Cell. 2008;132:125–136. doi: 10.1016/j.cell.2007.11.041. [DOI] [PubMed] [Google Scholar]
- 120.Zhang F, Phiel CJ, Spece L, Gurvich N, Klein PS. Inhibitory phosphorylation of glycogen synthase kinase-3 (GSK-3) in response to lithium. Evidence for autoregulation of GSK-3. J. Biol. Chem. 2003;278:33067–33077. doi: 10.1074/jbc.M212635200. [DOI] [PubMed] [Google Scholar]
- 121.Jope RS. Lithium and GSK-3: one inhibitor, two inhibitory actions, multiple outcomes. Trends Pharmacol. Sci. 2003;24:441–443. doi: 10.1016/S0165-6147(03)00206-2. [DOI] [PubMed] [Google Scholar]
- 122.Adli M, Hollinde DL, Stamm T, Wiethoff K, Tsahuridu M, Kirchheiner J, Heinz A, Bauer M. Response to lithium augmentation in depression is associated with the glycogen synthase kinase 3-beta –50T/C single nucleotide polymorphism. Biol. Psychiatry. 2007;62:1295–1302. doi: 10.1016/j.biopsych.2007.03.023. [DOI] [PubMed] [Google Scholar]
- 123.Szczepankiewicz A, Rybakowski JK, Suwalska A, Skibinska M, Leszczynska-Rodziewicz A, Dmitrzak-Weglarz M, Czerski PM, Hauser J. Association study of the glycogen synthase kinase-3β gene polymorphism with prophylactic lithium response in bipolar patients. World J. Biol. Psychiatry. 2006;7:158–161. doi: 10.1080/15622970600554711. [DOI] [PubMed] [Google Scholar]
- 124.Kozikowski AP, Gunosewoyo H, Guo S, Gaisina IN, Walter RL, Ketcherside A, McClung CA, Mesecar AD, Caldarone B. Identification of a Glycogen Synthase Kinase-3β Inhibitor that Attenuates Hyperactivity in CLOCK Mutant Mice. Chem. Med. Chem. 2011;6:1593–1602. doi: 10.1002/cmdc.201100188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Roybal K, Theobold D, Graham A, DiNieri JA, Russo SJ, Krishnan V, Chakravarty S, Peevey J, Oehrlein N, Birnbaum S, Vitaterna MH, Orsulak P, Takahashi JS, Nestler EJ, Carlezon WA, Jr, McClung CA. Mania-like behavior induced by disruption of CLOCK. Proc. Natl. Acad. Sci. U. S. A. 2007;104:6406–6411. doi: 10.1073/pnas.0609625104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Serretti A, Benedetti F, Mandelli L, Lorenzi C, Pirovano A, Colombo C, Smeraldi E. Genetic dissection of psychopathological symptoms: insomnia in mood disorders and CLOCK gene polymorphism. Am. J. Med. Genet. B. Neuropsychiatr. Genet. 2003;121:35–38. doi: 10.1002/ajmg.b.20053. [DOI] [PubMed] [Google Scholar]
- 127.Benedetti F, Serretti A, Colombo C, Barbini B, Lorenzi C, Campori E, Smeraldi E. Influence of CLOCK gene polymorphism on circadian mood fluctuation and illness recurrence in bipolar depression. Am. J. Med. Genet. B. Neuropsychiatr. Genet. 2003;123:23–26. doi: 10.1002/ajmg.b.20038. [DOI] [PubMed] [Google Scholar]
- 128.Kishi T, Kitajima T, Ikeda M, Yamanouchi Y, Kinoshita Y, Kawashima K, Okochi T, Okumura T, Tsunoka T, Inada T, Ozaki N, Iwata N. Association study of clock gene (CLOCK) and schizophrenia and mood disorders in the Japanese population. Eur. Arch. Psychiatry Clin. Neurosci. 2009;259:293–297. doi: 10.1007/s00406-009-0869-4. [DOI] [PubMed] [Google Scholar]
- 129.Lee KY, Song JY, Kim SH, Kim SC, Joo EJ, Ahn YM, Kim YS. Association between CLOCK 3111T/C and preferred circadian phase in Korean patients with bipolar disorder. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2010;34:1196–1201. doi: 10.1016/j.pnpbp.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 130.Bailer U, Wiesegger G, Leisch F, Fuchs K, Leitner I, Letmaier M, Konstantinidis A, Stastny J, Sieghart W, Hornik K, Mitterauer B, Kasper S, Aschauer HN. No association of clock gene T3111C polymorphism and affective disorders. Eur. Neuropsychopharmacol. 2005;15:51–55. doi: 10.1016/j.euroneuro.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 131.Kishi T, Yoshimura R, Fukuo Y, Kitajima T, Okochi T, Matsunaga S, Inada T, Kunugi H, Kato T, Yoshikawa T, Ujike H, Umene-Nakano W, Nakamura J, Ozaki N, Serretti A, Correll CU, Iwata N. The CLOCK gene and mood disorders: a case-control study and meta-analysis. Chronobiol. Int . 2011;28:825–833. doi: 10.3109/07420528.2011.609951. [DOI] [PubMed] [Google Scholar]
- 132.Kalinichev M, Dawson LA. Evidence for antimanic efficacy of glycogen synthase kinase-3 (GSK3) inhibitors in a strain-specific model of acute mania. Int. J. Neuropsychopharmacol . 2011;14:1051–1067. doi: 10.1017/S1461145710001495. [DOI] [PubMed] [Google Scholar]
- 133.Vasconcellos AP, Tabajara AS, Ferrari C, Rocha E, Dalmaz C. Effect of chronic stress on spatial memory in rats is attenuated by lithium treatment. Physiol. Behav. 2003;79:143–149. doi: 10.1016/s0031-9384(03)00113-6. [DOI] [PubMed] [Google Scholar]
- 134.Wood GE, Young LT, Reagan LP, Chen B, McEwen BS. Stress-induced structural remodeling in hippocampus: prevention by lithium treatment. Proc. Natl. Acad. Sci. U. S. A. 2004;101:3973–3978. doi: 10.1073/pnas.0400208101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Silva R, Mesquita AR, Bessa J, Sousa JC, Sotiropoulos I, Leão P, Almeida OF, Sousa N. Lithium blocks stress-induced changes in depressive-like behavior and hippocampal cell fate: the role of glycogen-synthase-kinase-3β. Neuroscience. 2008;152:656–669. doi: 10.1016/j.neuroscience.2007.12.026. [DOI] [PubMed] [Google Scholar]
- 136.Fountoulakis KN, Vieta E, Sanchez-Moreno J, Kaprinis SG, Goikolea JM, Kaprinis GS. Treatment guidelines for bipolar disorder: a critical review. J. Affect. Disord. 2005;86:1–10. doi: 10.1016/j.jad.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 137.Bowden CL. Valproate. Bipolar Disord . 2003;5:189–202. doi: 10.1034/j.1399-5618.2003.00031.x. [DOI] [PubMed] [Google Scholar]
- 138.Werstuck GH, Kim AJ, Brenstrum T, Ohnmacht SA, Panna E, Capretta A. Examining the correlations between GSK-3 inhibitory properties and anti-convulsant efficacy of valproate and valproate-related compounds. Bioorg. Med. Chem. Lett . 2004;14:5465–5467. doi: 10.1016/j.bmcl.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 139.Kim AJ, Shi Y, Austin RC, Werstuck GH. Valproate protects cells from ER stress-induced lipid accumulation and apoptosis by inhibiting glycogen synthase kinase-3. J. Cell Sci . 2005;118:89–99. doi: 10.1242/jcs.01562. [DOI] [PubMed] [Google Scholar]
- 140.Phiel CJ, Zhang F, Huang EY, Guenther MG, Lazar MA, Klein PS. Histone deacetylase is a direct target of valproic acid, a potent anticonvulsant, mood stabiliser, and teratogen. J. Biol. Chem . 2001;276:36734–36741. doi: 10.1074/jbc.M101287200. [DOI] [PubMed] [Google Scholar]
- 141.Hall AC, Brennan A, Goold RG, Cleverley K, Lucas FR, Gordon-Weeks PR, Salinas PC. Valproate regulates GSK-3-mediated axonal remodeling and synapsin I clustering in developing neurons. Mol. Cell Neurosci . 2002;20:257–270. doi: 10.1006/mcne.2002.1117. [DOI] [PubMed] [Google Scholar]
- 142.Eickholt BJ, Towers GJ, Ryves WJ, Eikel D, Adley K, Ylinen LM, Chadborn NH, Harwood AJ, Nau H, Williams RS. Effects of valproic acid derivatives on inositol trisphosphate depletion, teratogenicity, glycogen synthase kinase-3beta inhibition, and viral replication: a screening approach for new bipolar disorder drugs derived from the valproic acid core structure. Mol. Pharmacol . 2005;67:1426–1433. doi: 10.1124/mol.104.009308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Jin N, Kovacs AD, Sui Z, Dewhurst S, Maggirwar SB. Opposite effects of lithium and valproic acid on trophic factor deprivation-induced glycogen synthase kinase-3 activation, c-Jun expression and neuronal cell death. Neuropharmacology. 2005;48:576–583. doi: 10.1016/j.neuropharm.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 144.Grimes CA, Jope RS. CREB DNA binding activity is inhibited by glycogen synthase kinase-3 beta and facilitated by lithium. J. Neurochem. 2001;78:1219–1232. doi: 10.1046/j.1471-4159.2001.00495.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Leng Y, Liang MH, Ren M, Marinova Z, Leeds P, Chuang DM. Synergistic neuroprotective effects of lithium and valproic acid or other histone deacetylase inhibitors in neurons: roles of glycogen synthase kinase-3 inhibition. J. Neurosci. 2008;28:2576–2588. doi: 10.1523/JNEUROSCI.5467-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Lamarre M, Desrosiers RR. Up-regulation of protein l-isoaspartyl methyltransferase expression by lithium is mediated by glycogen synthase kinase-3 inactivation and beta-catenin stabilisation. Neuropharmacology. 2008;55:669–676. doi: 10.1016/j.neuropharm.2008.05.033. [DOI] [PubMed] [Google Scholar]
- 147.Aubry JM, Schwald M, Ballmann E, Karege F. Early effects of mood stabilisers on the Akt/ GSK-3beta signalling pathway and on cell survival and proliferation. Psychopharmacology (Berl) 2009;205:419–429. doi: 10.1007/s00213-009-1551-2. [DOI] [PubMed] [Google Scholar]
- 148.Ryves WJ, Dalton EC, Harwood AJ, Williams RS. GSK-3 activity in neocortical cells is inhibited by lithium but not carbamazepine or valproic acid. Bipolar Disord. 2005;7:260–265. doi: 10.1111/j.1399-5618.2005.00194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Tong N, Sanchez JF, Maggirwar SB, Ramirez SH, Guo H, Dewhurst S, Gelbard HA. Activation of glycogen synthase kinase 3 beta (GSK-3β) by platelet activating factor mediates migration and cell death in cerebellar granule neurons. Eur. J. Neurosci. 2001;13:1913–1922. doi: 10.1046/j.0953-816x.2001.01572.x. [DOI] [PubMed] [Google Scholar]
- 150.Kozlovsky N, Nadri C, Belmaker RH, Agam G. Lack of effect of mood stabilisers or neuroleptics on GSK-3 protein levels and GSK-3 activity. Int. J. Neuropsychopharmacol. 2003;6:117–120. doi: 10.1017/S1461145703003353. [DOI] [PubMed] [Google Scholar]
- 151.Roh MS, Eom TY, Zmijewska AA, De Sarno P, Roth KA, Jope RS. Hypoxia activates glycogen synthase kinase-3 in mouse brain in vivo: protection by mood stabilisers and imipramine. Biol. Psychiatry. 2005;57:278–286. doi: 10.1016/j.biopsych.2004.10.039. [DOI] [PubMed] [Google Scholar]
- 152.Zhou R, Yuan P, Wang Y, Hunsberger JG, Elkahloun A, Wei Y, Damschroder-Williams P, Du J, Chen G, Manji HK. Evidence for selective microRNAs and their effectors as common long-term targets for the actions of mood stabilisers. Neuropsychopharmacology. 2009;34:1395–1405. doi: 10.1038/npp.2008.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Agam G, Shaltiel G, Kozlovsky N, Shimon H, Belmaker RH. Lithium inhibitable enzymes in postmortem brain of bipolar patients. J. Psychiatr. Res. 2003;37:433–442. doi: 10.1016/s0022-3956(03)00044-x. [DOI] [PubMed] [Google Scholar]
- 154.Beasley C, Cotter D, Everall I. An investigation of the Wnt-signalling pathway in the prefrontal cortex in schizophrenia, bipolar disorder and major depressive disorder. Schizophr. Res. 2002;58:63–67. doi: 10.1016/s0920-9964(01)00376-0. [DOI] [PubMed] [Google Scholar]
- 155.Mai L, Jope RS, Li X. BPNF-mediated signal transduction is modulated by GSK3β and mood stabilizing agents. J. Neurochem. 2002;82:75–83. doi: 10.1046/j.1471-4159.2002.00939.x. [DOI] [PubMed] [Google Scholar]
- 156.Weinberger DR. Implications of normal brain development for the pathogenesis of schizophrenia. Arch. Gen. Psychiatry. 1987;44:660–669. doi: 10.1001/archpsyc.1987.01800190080012. [DOI] [PubMed] [Google Scholar]
- 157.Weinberger DR, Berman KF, Illowsky BP. Physiological dysfunction of dorsolateral prefrontal cortex in schizophrenia. III. A new cohort and evidence for a monoaminergic mechanism. Arch. Gen. Psych. 1988;45:609–615. doi: 10.1001/archpsyc.1988.01800310013001. [DOI] [PubMed] [Google Scholar]
- 158.Breier A, Su TP, Saunders R, Carson RE, Kolachana BS, de Bartolomeis A, Weinberger DR, Weisenfeld N, Malhotra AK, Eckelman WC, Pickar D. Schizophrenia is associated with elevated amphetamine-induced synaptic dopamine concentrations: evidence from a novel positron emission tomography method. Proc. Natl. Acad. Sci. U. S. A. 1997;94:2569–2574. doi: 10.1073/pnas.94.6.2569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Molina V, Sanz J, Sarramea F, Benito C, Palomo T. Prefrontal atrophy in first episodes of schizophrenia associated with limbic metabolic hyperactivity. J. Psychiatr. Res. 2005;39:117–127. doi: 10.1016/j.jpsychires.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 160.Beaulieu JM, Gainetdinov RR, Caron MG. The Akt-GSK-3 signalling cascade in the actions of dopamine. Trends Pharmacol. Sci. 2007;28:166–172. doi: 10.1016/j.tips.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 161.Kang UG, Seo MS, Roh MS, Kim Y, Yoon SC, Kim YS. The effects of clozapine on the GSK-3-mediated signalling pathway. FEBS Lett. 2004;560:115–119. doi: 10.1016/S0014-5793(04)00082-1. [DOI] [PubMed] [Google Scholar]
- 162.Sutton LP, Honardoust D, Mouyal J, Rajakumar N, Rushlow WJ. Activation of the canonical Wnt pathway by the antipsychotics haloperidol and clozapine involves disheveled-3. J. Neurochem. 2007;102:153–169. doi: 10.1111/j.1471-4159.2007.04527.x. [DOI] [PubMed] [Google Scholar]
- 163.Beaulieu JM. Not only lithium: regulation of glycogen synthase kinase-3 by antipsychotics and serotonergic drugs. Int. J. Neuropsychopharmacol. 2007;10:3–6. doi: 10.1017/S1461145706006857. [DOI] [PubMed] [Google Scholar]
- 164.Beaulieu JM, Gainetdinov RR, Caron MG. Akt/GSK3 signalling in the action of psychotropic drugs. Annu. Rev. Pharmacol. Toxicol. 2009;49:327–347. doi: 10.1146/annurev.pharmtox.011008.145634. [DOI] [PubMed] [Google Scholar]
- 165.Sutton LP, Rushlow WJ. The effects of neuropsychiatric drugs on glycogen synthase kinase-3 signalling. Neuroscience. 2011;199:116–24. doi: 10.1016/j.neuroscience.2011.09.056. [DOI] [PubMed] [Google Scholar]
- 166.Alimohamad H, Rajakumar N, Seah YH, Rushlow W. Antipsychotics alter the protein expression levels of β-catenin and GSK-3 in the rat medial prefrontal cortex and striatum. Biol. Psychiatry. 2005;57:533–542. doi: 10.1016/j.biopsych.2004.11.036. [DOI] [PubMed] [Google Scholar]
- 167.Alimohamad H, Sutton L, Mouyal J, Rajakumar N, Rushlow WJ. The effects of antipsychotics on β-catenin, glycogen synthase kinase-3 and disheveled in the ventral midbrain of rats. J. Neurochem. 2005;95:513–525. doi: 10.1111/j.1471-4159.2005.03388.x. [DOI] [PubMed] [Google Scholar]
- 168.Roh MS, Seo MS, Kim Y, Kim SH, Jeon WJ, Ahn YM, Kang UG, Juhnn YS, Kim YS. Haloperidol and clozapine differentially regulate signals upstream of glycogen synthase kinase 3 in the rat frontal cortex. Exp. Mol. Med. 2007;39:353–360. doi: 10.1038/emm.2007.39. [DOI] [PubMed] [Google Scholar]
- 169.Emamian ES, Hall D, Birnbaum MJ, Karayiorgou M, Gogos JA. Convergent evidence for impaired AKT1-GSK3β signalling in schizophrenia. Nat. Genet. 2004;36:131–137. doi: 10.1038/ng1296. [DOI] [PubMed] [Google Scholar]
- 170.Ukai W, Ozawa H, Tateno M, Hashimoto E, Saito T. Neurotoxic potential of haloperidol in comparison with risperidone: implication of Akt-mediated signal changes by haloperidol. J. Neural. Transm. 2004;111:667–681. doi: 10.1007/s00702-004-0109-z. [DOI] [PubMed] [Google Scholar]
- 171.Dai Y, Wei Z, Sephton CF, Zhang D, Anderson DH, Mousseau DD. Haloperidol induces the nuclear translocation of phosphatidylinositol 3’-kinase to disrupt Akt phosphorylation in PC12 cells. J. Psychiatry Neurosci. 2007;32:323–330. [PMC free article] [PubMed] [Google Scholar]
- 172.Lu D, Carson DA. Spiperone enhances intracellular calcium level and inhibits the Wnt signalling pathway. BMC Pharmacol. 2009;9:13. doi: 10.1186/1471-2210-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Beaulieu JM. A role for Akt and glycogen synthase kinase-3 as integrators of dopamine and serotonin neurotransmission in mental health. J Psychiatry Neurosci 2011 110011 doi: 101503/jpn110011. . 2011;36(4):110011. doi: 10.1503/jpn.110011. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Brennand KJ, Simone A, Jou J, Gelboin-Burkhart C, Tran N, Sangar S, Li Y, Mu Y, Chen G, Yu D, McCarthy S, Sebat J, Gage FH. Modelling schizophrenia using human induced pluripotent stem cells. Nature. 2011;473:221–225. doi: 10.1038/nature09915. Erratum: Nature. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Li X, Jope RS. Is glycogen synthase kinase-3 a central modulator in mood regulation? Neuropsychopharmacology. 2010;35:2143–2154. doi: 10.1038/npp.2010.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Malberg JE, Eisch AJ, Nestler EJ, Duman RS. Chronic antidepressant treatment increases neurogenesis in adult rat hippocampus. J. Neurosci. 2000;20:9104–9110. doi: 10.1523/JNEUROSCI.20-24-09104.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Pinnock SB, Blake AM, Platt NJ, Herbert J. The roles of BPNF, pCREB and Wnt3a in the latent period preceding activation of progenitor cell mitosis in the adult dentate gyrus by fluoxetine. PLoS One. 2010;5:e13652. doi: 10.1371/journal.pone.0013652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Pilar-Cuéllar F, Vidal R, Pazos A. Subchronic treatment with fluoxetine and ketanserin increases hippocampal brain-derived neurotrophic factor, β-catenin and antidepressant-like effects. Br. J. Pharmacol. 2012;165:1046–1057. doi: 10.1111/j.1476-5381.2011.01516.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Mostany R, Valdizán EM, Pazos A. A role for nuclear β-catenin in SNRI antidepressant-induced hippocampal cell proliferation. Neuropharmacology. 2008;55:18–26. doi: 10.1016/j.neuropharm.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 180.Nakano M, Osada K, Misonoo A, Fujiwara K, Takahashi M, Ogawa Y, Haga T, Kanai S, Tanaka D, Sasuga Y, Yanagida T, Asakura M, Yamaguchi N. Fluvoxamine and sigma-1 receptor agonists dehydroepiandrosterone (DHEA)-sulfate induces the Ser473-phosphorylation of Akt-1 in PC12 cells. Life Sci. 2010;86:309–314. doi: 10.1016/j.lfs.2009.11.017. [DOI] [PubMed] [Google Scholar]
- 181.Bhuiyan MS, Tagashira H, Fukunaga K. Sigma-1 receptor stimulation with fluvoxamine activates Akt-eNOS signalling in the thoracic aorta of ovariectomized rats with abdominal aortic banding. Eur. J. Pharmacol. 2011;650:621–628. doi: 10.1016/j.ejphar.2010.10.055. [DOI] [PubMed] [Google Scholar]
- 182.Reddy KK, Lefkove B, Chen LB, Govindarajan B, Carracedo A, Velasco G, Carrillo CO, Bhandarkar SS, Owens MJ, Mechta-Grigoriou F, Arbiser JL. The antidepressant sertraline downregulates Akt and has activity against melanoma cells. Pigment Cell Melanoma Res. 2008;21:451–456. doi: 10.1111/j.1755-148X.2008.00481.x. [DOI] [PubMed] [Google Scholar]
- 183.Basta-Kaim A, Budziszewska B, Jaworska-Feil L, Tetich M, Kubera M, Leskiewicz M, Lason W. Inhibitory effect of imipramine on the human corticotropin-releasing-hormone gene promoter activity operates through a PI3-K/AKT mediated pathway. Neuropharmacology. 2005;49:156–164. doi: 10.1016/j.neuropharm.2005.02.008. [DOI] [PubMed] [Google Scholar]