Abstract
Background:
The medical and economic problem of thalassaemia are considered to be a vast public health problem in the thalassaemia belt countries, emphasizing more on prenatal diagnosis as the solution of the problem.
Methods:
A cross-sectional descriptive study was conducted in the Institute of Haematology & Transfusion Medicine located in Medical College, Kolkata, India to assess the socio-demographic profile, clinical presentation, expenditure for treatment of thalassaemia patients and awareness about cause and prevention of the disease.
Results:
Thalassaemia patients attended the Govt. setting were mostly from lower socioeconomic status with low level of literacy. Annual expenditure for treatment of thalassaemia ranged from $ 108 to 432; depending on type of treatment with average cost per transfusion was $ 5.2±2.2. Average 18.5%±14.3 of the total annual income was spent on the treatment for thalassaemia. Average man days or school days lost for the patients was 29.87±18.5 and 19.07±12.7 for the accompanying persons.
Conclusion:
Blood transfusion and carrier screening facilities should be decentralized to decrease the expenditure for treatment and alleviate the harassment of the families. Folate and calcium tablets, hepatitis B vaccination can be made available at government setting free of cost.
Keywords: Thalassaemia, Blood transfusion, Expenditure for treatment, Man days lost
Introduction
Thalassaemia syndromes are a heterogeneous group of single gene disorders, inherited in an autosomal recessive manner, prevalent in certain parts of the world, especially Mediterranean belt. Thalassaemia is one of the most challenging diseases being faced by the mankind with virtually no permanent cure. Every year approximately 100,000 children are born worldwide with thalassaemia major, of which 10,000 are born in India (1). The estimated prevalence is 16% in people from Cyprus, 1% in Thailand, and 3–8% in populations from Bangladesh, China, India, Malaysia and Pakistan (2). It is estimated that there are about 65,000–67,000 β-thalassaemia patients in India and approximately 30 million carriers of β-thalassaemia with a mean prevalence of 3.3%(1). But among certain communities and religions like Punjabis, Sindhis, Bengalis, Jains and Muslims, the incidence ranges between 8–15% (3).
Once a child is diagnosed to have thalassaemia homozygous disorders, he/she has to take lifelong treatment. Management includes regular filtered packed red cell transfusions, chelation therapy for iron overload, management of complications of iron overload and transfusions, including osteoporosis, cardiac dysfunction, endocrine problems, Hepatitis B & C, HIV infection, CMV etc. However, this optimal treatment comes at a prohibitive cost. The cost of treatment of an average weight 4 yr old thalassaemic child is around $ 1948–2164 annually in a private set-up (1). Therefore, not more than 5–10% of thalassaemic children born in India receive optimal treatment (1). World Health Organization (4) has estimated that an annual average consumption of 27 units of blood and $ 8658 worth of the drug are needed to manage each patient according to recommended standards. Stem cell transplantation as a curative treatment is out of reach for majority of children. Besides bearing the cost of treatment, the psychological stress to both the patient and the parents/family is phenomenal. The birth of a thalassaemic child thus places considerable strain not only on affected child and family but on the country as a whole. Therefore emphasis has shifted from treatment to prevention of birth of such children in future, which can be achieved by prenatal diagnosis and genetic counseling of the carriers of the gene.
Under these circumstances, the present study has been carried out with the following objectives:
To study the socio-demographic profile and clinical presentation of the thalassaemia patients attending Institution of Haematology & Transfusion Medicine located in Medical College, Kolkata.
To assess the annual expenditure for treatment of these thalassaemia patients and to assess how much burden it incurred to the family
To study the level of awareness of the patients and their families regarding the cause and prevention of the disease
Materials and Methods
The present cross-sectional and observational study was conducted in the Thalassaemia OPD of Institute of Hematology & Transfusion Medicine located in Medical College, Kolkata, India. Study population was the diagnosed thalassaemia patients attending the OPD who fulfilled the inclusion and exclusion criteria. The patients who had history of blood transfusion for at least 1 yr were included in the study and all the new patients registered were not considered. Based on the statistics available from the institute of the year 2007–08, total number of thalassaemia patients registered was 682. Twenty percent of the registered patients were considered as sample, which came as 136. Usually the patients were being advised to come for a 3 weekly follow up in the thalassaemia OPD which is run on every Monday. Data collection was started on 1st day selecting the 1st patient randomly followed by every 5th patient from the old patient register. If a patient did not fit the inclusion criteria, next patient was selected, thus collecting data till the sample size was met. Ultimately data could be collected from 135 patients in a period of 3 month i.e. June to August 2008. Adult patients or parents or accompanying family members of the younger patients were interviewed with a pre-designed and pretested proforma.
Data was collected regarding socio-demographic variables, details of treatment adopted by the patients and number of units of blood transfused in the last 1 yr (1st June 2007 to 31st May 2008) from each patient, which was also corroborated from the treatment card available with the patient and the expenditure incurred.
Ethical consideration
Before conducting the study ethical clearance from the Ethical Committee of the college and informed consent from the patients were taken.
Results
The study population i.e. the thalassaemia patients who attended the Thalassaemia OPD of Medical College & Hospital were mainly in the age group of 5–14 yr (44.4%) and 15–45 yr (37.8%) with male preponderance (54.8%) mostly belonged to Hindu religion (81%) and majority of rural background (74%) (Table 1). A good percentage of them (75%) had completed primary education, 48% were still students but 37% of the thalassaemia patients were not engaged in any activity, either educational or livelihood earning. Sixty four percent belonged to the nuclear family. Majority of the patients were from grade II, III & IV economic status according to Prasad’s scale (5) and their fathers or husbands (in case of female patients) were mostly unskilled workers (52.6%) or doing small scale business (26.7%). Thalassaemia status of 63% of the patients was first diagnosed at Govt setting. Sixty three percent were diagnosed at or below the age of 5 yr, where as 19% between 6–10 yr, 7% between 11–15, 11% above the age of 15 yr. 6 female patients were diagnosed thalassaemic during their first pregnancy. At the time of diagnosis, 55.6% presented with fever as chief complaints, 46.7% with weakness, 29.6% with jaundice, 28.9% as inability to take food or severe anorexia, 18.5% with repeated infections. 15.6% with pallor, 11.8% with abdominal swelling and 5.2% with the complaints of failure to thrive. 2.2% had presented with oedema and 12.6% with various other complaints like dyspnoea, palpitation and dizziness.
Table 1:
Socio-demographic profile of the thalassaemia patients (n =135)
| Socio-demographic variables | n | % |
|---|---|---|
| Age (years) | ||
| <5 | 23 | 17.04 |
| 5 – 14 | 60 | 44.44 |
| 15 – 45 | 51 | 37.78 |
| >45 | 1 | 0.74 |
| Sex | ||
| Male | 74 | 54.81 |
| Female | 61 | 45.18 |
| Residence | ||
| Rural | 100 | 74 |
| Urban | 35 | 26 |
| Occupation | ||
| Unemployed | 123 | 91.12 |
| Unskilled worker | 5 | 3.7 |
| Skilled worker | 2 | 1.48 |
| Business | 5 | 3.7 |
| Educational status (n= 99)* | ||
| Illiterate | 11 | 11.11 |
| Primary | 35 | 35.35 |
| Middle school | 39 | 39.40 |
| Madhyamik | 8 | 8.08 |
| HS & above | 6 | 6.06 |
| Per capita per month income** ($) | ||
| >47.6 | 8 | 5.93 |
| 23.9 – 47.6 | 15 | 11.11 |
| 14.4 – 23.8 | 33 | 24.44 |
| 7 – 14.3 | 47 | 34.82 |
| <7 | 32 | 23.70 |
| Educational status of parents | ||
| Fathers or guardians with more than primary education | 88 | 65.18 |
| Mothers with more than primary education (n= 127)*** | 66 | 51.97 |
Only above 7 years were considered
According to Prasad’s scale (5). Here INR was converted into USD ($)
In case of married thalassaemia patients, education level of their husbands were considered
So far as thalassaemia status of the parents were concerned, 98(72%) of the patients had both parents diagnosed as carriers. Four (3%) had father thalassaemic & mother carrier, but only 1 had mother thalassaemic & father carrier. Seven (5%) patients had mother carrier but status of fathers were unknown. For 2 patients, both parents were thalassaemia victims and in 23 i.e 17.5% of cases carrier status of both parents were unknown.
Out of 135 patients, all of them received blood transfusion so far as treatment, 84.4% were prescribed either folate or calcium or both preparation, 20% iron chelation and 10.4% had splenectomy. In last 1 yr i.e. 1st June 2007 to 31st May 2008, 66.7% families of the thalassaemia patients had to spend up to $ 108 annually for treatment of thalassaemia, where as 17.8%, 8.9% and 5.2% spent $ 109–216, $ 217–324, $ 325–432 respectively. Only 1.5% spent above $ 432, who were coming from neighboring state. Average cost of treatment was $ 137.9±47.8. This expenditure included dollars spent for blood transfusion & related expenses, iron chelation therapy (if prescribed), folate and calcium supplementation therapy. It also included expenditure incurred in the recall period for investigations (viz. serum ferritin level, Hb estimation), splenectomy (if done in last 1 yr), vaccination for Hepatitis B and others like treatment costs for adverse effects of transfusion. Few patients received iron chelating tablets free of cost from a NGO working in collaboration with the institute; otherwise average cost was $ 26 to 32.5 per month for iron chelating oral preparations and $ 4.3 for calcium supplementation.
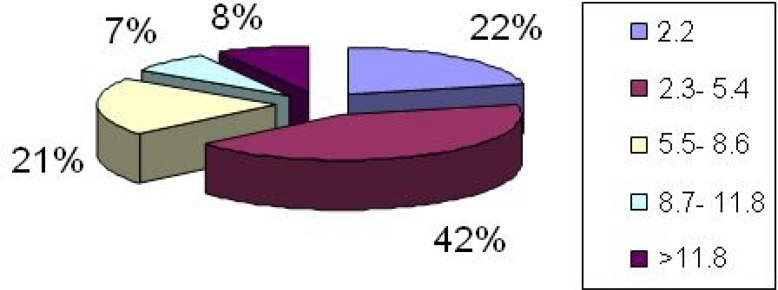
From the history or treatment card available, it was evident that 23.7% received up to 5 units of blood transfusion, 29.6% 6–10 units and 30.4% from 11 to 15 units in the recall period of 1 yr. 12.6% received more than 20 units in that period. Average number of units transfused was 10.2±3.8. Expenditure for blood transfusion included cost of blood units, hospital stay and for procedure, charges for relevant investigations and expenditure for travel, food and shelter for patient and accompanying person. The procedure charges were related to buying syringe & needle necessary for transfusion. As in most of the cases blood was available free, cost for travel, food and shelter formed the main bulk of expenditure. Average expenditure per blood transfusion was $ 5.2 ± 2.2 (Fig. 1).
Fig. 1:
Average expenditure per tranfusion of thalassaemia patients ($) (n = 135)
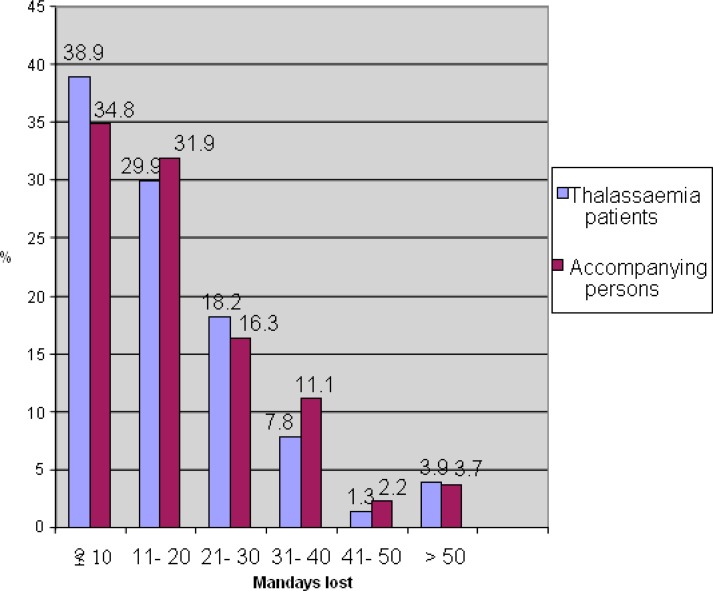
Due to repeated blood transfusions, these patients suffered from various hazards of transfusion since the therapy started viz. 1 had Hepatitis C, 2 had Hepatitis B, 19(14%) had cellulitis & thrombophlebitis and 112 i.e. (83%) developed some non specific reactions like fever, chill and rigor. Considering the financial burden to the families, 70% of the study population had to spend up to 20% of their total family income for treatment in last year, where 20% spent 21–40% and 10% spent above 40% of their annual income. Average 18.5%±14.3 of annual family income was spent. Attending regularly the institute for blood transfusion and OPD for follow up visits incurred a huge man days lost for the patients and accompanying persons (Fig. 2). Average man days or school days lost for the patient was 29.87±18.5 and average man days lost for the accompanying person was 19.07±12.7. Regarding the social problems, 20.7% of the thalassaemia patients faced some form of social isolation in the neighbourhood or school and 2.2% faced marital problems due to disease condition.
Fig. 2:
Total man days lost for the patients (n= 77)* and for the accompanying persons (n= 135)
*For thalassaemia patients, loss of man days or school days were considered in case of working persons and school going children
Among the thalassaemia patients and their families, 68.9% were aware about the cause of the disease and 60.7% knew how to prevent it. Regarding prevention, it was observed that only 64.5% patients (if married) and/ or their families (if unmarried) had been counseled to adopt family planning methods for prevention. 70 (51.8%) patients or their families adopted some form of family planning methods. Among them, 49% were using oral pills, 21% barrier methods, 1% IUD and 29% had tubectomy.
Discussion
Thalassaemia major is an inherited blood disorder passed on from parents to their children, causing an inability to produce adequate amount of hemoglobin and leading to severe hemolytic anemia. Symptoms appear a few months after birth and without treatment death will ensue in early childhood. Due to available treatment by repeated blood transfusions and iron chelation therapy, it is now possible to extend the life into adulthood though very cumbersome and costly. In the present study, 37.8% patients were seen in the age group of 15–45 yr, whereas a study conducted in a Govt Medical college of Kolkata in 2001 (6) hardly found any patient above 15 yr. Study conducted in Bombay (7) had shown also remarkable improvement of survival from 3% to 84% in the thalassaemia families in last 2 decades. Similarly in North America (8) mean age of thalassaemia major patients had improved from 6.2 to 16.7 in 2 decades. Similar to the present study, most of the studies conducted in Kolkata (6), Chattagram (9) and Rawalpindi (10) had found male preponderance among thalassaemia patients. Probable underlying reasons might be the gender inequality in the care seeking behaviour for chronic illnesses. Majority of the thalassaemia patients were coming to Govt setting from rural area and of low socio economic status as also seen in studies conducted in Lukhnow (11) & Pakistan (12). Prevention and adherence to treatment depend on awareness, which is frequently contributed by educational level of parents. The present study observed 65.2% fathers and 58% mothers had more than primary education, similar to study in Kolkata (6), but educational level of parents was seen better in Mumbai (7) & Pakistan (12).
The economic burden of thalassaemia depends on the birth prevalence of the disease; their survival; availability, effectiveness and cost of the treatment and finally extent of social support. Regular blood transfusion is available in most of the countries, is lifesaving and improves short time quality of life. But iron chelation therapy is essential for long term survival. The present study observed that 70% of the families had to spend up to 20% of their yearly income for treatment of thalassaemia, similar to Mumbai (7). In Kolkata (6), average was seen as 23.8%±19.5 in Govt setting in 2001, where as the present study observed it as 18.5%±14.3. In Pakistan (12), a family has to spend $ 4330 to 12987 for 10 yr, where as in Iran (13) it is 25 US dollar cost for each bottle blood transfusion and 280 US dollar for iron chelation therapy per month. In Israel (14), the yearly treatment cost during the first 5 yr of life without chelation therapy is estimated as 4,619 U$S, where as cost per patient for 50 yr of life is an average of 25.134 U$S per year. Eight five percent of patients had average expenditure per blood transfusion up to $ 11.9 as observed in the present study, where as in Mumbai (7) the yearly expenditure varied from 21.6 to 86.6 $ for average 12 transfusions a year depending on type of hospitals.
Only 1 patient was seen positive for hepatitis C virus and 2 patients for Australia antigen, similar to the findings of Ocak et al. (15) at Turkey (4.5% & .75% respectively), where as Shah et al. (16) found it more in Pakistan as 56.8% & 8.4% respectively.
Different research works conducted worldwide had already established the cost effectiveness of prevention program for thalassaemia and the prevention program includes population education, mass screening of high risk communities, genetic counseling and prenatal Diagnosis. The present study observed that 68.9% were aware about the cause and 60.7% about prevention, where almost all did know about cause, prevention and sequele of the disease in Mumbai (7). Fifty two percent of families had adopted some form of family planning methods, where as it was 73% in Mumbai (7) and 43% in Kolkata (6). But experience of social isolation and stigmatization was similar to Mumbai (7).
In conclusion, the study found the scope still exists regarding improvement of awareness about the disease and how to prevent it and recommends compulsory premarital screening for thalassaemia. In this regard, the birth registrars, Purohits or Moulavis could be involved. Decentralization of blood transfusion and carrier screening facilities at the district level should be organized to decrease the expenditure for treatment, alleviate the harassment of the families and also to improve extended carrier screening for the relatives of the affected families. Folate and calcium tablets, Hepatitis B vaccination can be made available at Government setting free of cost.
Acknowledgments
The authors deeply acknowledge the Director of Institute of Hematology & Transfusion Medicine and the Principal, Medical College, Kolkata, India for asserting permission for conducting the study. The authors declare that they have no conflicts of interest.
References
- 1.Center for Education. Mission Thalassaemia. http://www.cedranchi.com/index.htm (accessed on 14th Jan 2009)
- 2.http://en.wikipedia.org/wiki/thalassaemia (accessed on 31st May 2009)
- 3.Marwah RK, Lal A. Present status of haemoglobinopathies in India. Indian Pediatrics. 1994;31:267–71. [PubMed] [Google Scholar]
- 4.Modell M, editor. Guidelines for the control of haemoglobin disorders. 1994. WHO Hereditary disease programme.
- 5.Hiremath DA, Hiremath D Lalita. Essentials of Community Medicine- A practical approach. Jaypee Brothers, New Delhi. 2004:13. [Google Scholar]
- 6.Bandyopadhyay B, Nandi S, Mitra K, et al. A comparative study on perceptions and practices among patients of thalassaemic children attending two different institutions. Ind J Comm Med. 2003;28(3):128–32. [Google Scholar]
- 7.Sangani B, Sukumaran PK, Mahadik C. Thalassaemia in Bombay: Role of medical genetics in developing countries. Bulletin. 1990;68(1):75–81. [PMC free article] [PubMed] [Google Scholar]
- 8.Pearson Howard A, Cohen Alan R, Giardina Patricia-Jane V, Kazazian Haig H., Jr The Changing Profile of Homozygous β Thalassemia: Demography, Ethnicity, and Age Distribution of Current North American Patients and Changes in Two Decades. Pediatrics. 1996;97(3):352–6. [PubMed] [Google Scholar]
- 9.Ahmed J, Seraj UM, Chowdhury MA, Chowdhury S. An epidemiologic study on thalassaemia, its quick diagnosis and influence of malaria in Chittagong area of Bangladesh. Pakistan J of Biollogical Sciences. 2004;7(11):1953–57. [Google Scholar]
- 10.Rai ME, Tanoli ZM, Gandapur ASK. Clinical spectrum of patients of beta thalassaemia: a review of fifty four patients. Glomal J Medical sciences. 2005;3(2):55–60. [Google Scholar]
- 11.Saxena A, Phadke SR. Thalassaemia control by carrier screening: The Indian scenario. Current science. 2002;83(3):291. [Google Scholar]
- 12.Rehaman S, Batool S, Qadir R. Socio economic status impact thalassaemia child on families of Faisalabad district. Pakistan J of Applied Sciences. 2002;2(2):202–5. [Google Scholar]
- 13.Ghotbi N, Tsukatani T. An economic review of the national screening policy to prevent thalassaemia major in Iran 2002 [Google Scholar]
- 14.Koren A, Levin C, Profeta L, et al. Beta thalassemia prevention in northern Israel- cost benefit analysis. Haematologica. 2008;93(s1):400. doi: 10.4084/MJHID.2014.012. Abs. 1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ocak S, Kaya H, Cetin M, et al. Seroprevalence of hepatitis B and hepatitis C in patients with thalassaemia and sickle cell anaemia in a long term follow up. Archives of Medical Research. 2008;37(7):895–98. doi: 10.1016/j.arcmed.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 16.Shah SMA, Khan MT, Zahour Ullah, Ashfaq NY. Prevalence of hepatitis B and hepatitis C virus infection in a multitransfused thalassaemia major patients in North West Frontier province. Pakistan J Medical Sciences. 2009. http://www.cababstractsplus.org/abstracts/Abstract.asp (accessed on 1st June 2009).