Abstract
Background:
To identify the most important expectations that patients have from their physicians.
Methods:
We collected data from 199 hospitalized and 201 ambulatory patients (response rates 88% and 93% respectively). We used random sampling for selection of hospitalized patients and systematic sampling for the ambulatory ones. The questionnaire consisted of 18 different expectation items categorized in 5 domains. The participants scored each item from 1 to 9 using a VAS scale and ranked domains based on their importance. We analyzed the data using univariate and regression analyses.
Results:
Among the ambulatory patients, the mean±standard error of the most important expectations was as follows: competency (8.9±0.01), courteousness (8.8±0.04), consultation in case of need (8.8±0.4), clear explanation of the disease (8.8±0.05) and attentiveness (8.8±0.04). In hospitalized patients, the following items were the most important: competency (8.4±0.08), courteousness (8.4±0.09), availability of physician (8.4±0.09), consultation in case of need (8.2±0.11), setting following appointments (8.2±0.1), and disease follow-up (8.2±0.09). In both groups, the most important domain of expectations was “competency and quality of care” followed by “availability” in hospitalized and “giving information and patient autonomy” among ambulatory patients.
Conclusions:
Our findings are similar to what reported in the literature from other countries and cultures. In addition to physician expertise and knowledge, patients value giving information and efficient doctor-patient relationship.
Keywords: Patient expectation, Patient priority, Patient-centered care
Introduction
Medical care has experienced revolutionary changes in recent years and availability of various therapeutic options and increased knowledge of patients have led to a patient-oriented medicine with a more focused attention toward patient preferences (1, 2).
A good physician seeks a holistic view of the patient and his reasonable expectations and needs. In fact, one of the current challenges of health systems is how to respond and fulfill patients’ expectations. Despite these, knowing what patients want and what matters to them are relatively ignored aspects of medical care (2–4). Knowledge of patients’ priorities and using that knowledge in practice will improve quality of care and patient satisfaction (5–7). Furthermore, the physicians’ interpretation of priority may be different from that of patients’ (8–11) and this difference may lead to neglect of certain aspects of patient care.
All the studies focusing on patient priorities have been carried out in European or American countries (2, 5) and it is not clear if one can generalize their results to a country like Iran that has a different cultural, social and economical background (12).
This study was conducted to investigate what patients expect of their physicians in order to offer interventions to improve patient satisfaction and medical care.
Materials and Methods
Sampling
The study was carried out in an academic general hospital in Tehran, Iran on patients older than 14 yr during Jan–Feb 2007. Four hundred patients (199 hospitalized and 201 ambulatory) participated in the study. Each day we randomly selected 15 hospitalized patients from the hospital’s admission list excluding patients from pediatrics, obstetrics and emergency wards. Patients were entered if they were able and willing to participate. We used a systematic sampling approach for selection of ambulatory patients so that each day we approached 15 patients with odd admission numbers at the hospital’s polyclinic.
Questionnaire
The questionnaire was comprised of 18 items categorized within five domains (Table 1). We developed the questionnaire using selected previously published studies (2, 5, 10) and a pilot study of 30 patients about their expectations.
Table 1:
Patient expectation items and domains
| A- Physician’s availability |
|
| B- Giving information and patient autonomy |
|
| C- Compassion□ |
|
| D. Doctor- patient relationship |
|
| E. Physician competency and quality of care |
|
We asked six experts to review the original questionnaire and classify the items under the domains. Additionally, we asked twenty patients to tell their understanding of the items of the initial questionnaire and modified the questions accordingly.
We then formatted the domains in two forms of Visual Analogue Scale (VAS) and a ranking scale. Each format of the questionnaire was tested on ten medical students twice, two weeks apart. Due to lack of reliability in ranking scale method, the VAS format was chosen for the main study. Based on internal consistency test of expectations in each domains a few items were re-categorized into domains and the final version of the questionnaire was tested on ten patients. Validity of the final questionnaire was assessed by calculating Cronbach’s alpha which lied between 0.63 and 0.82 for all domains except “Availability” domain (0.35).
Data collection and analysis
The patients were asked to score each item on a VAS of 1 to 9. They were then asked to rank domains according to their level of importance. Knowing that a fraction of patients visiting this center are illiterate (13), we conducted face-to-face interviews with all participants and the responses were marked by the interviewer. The interviewers were fluent in both Persian and Azari and a Azari version of the questionnaire was also prepared. Oral consent was obtained after explaining the objectives and methods of the study to each patient. The research ethics committee of Tehran University of Medical Sciences approved the study.
We used univariate analyses to compare the hospitalized and ambulatory patients’ views. We used linear regression to analyze the factors that influenced patients’ views about each domain. To do so, factors like age, sex, years of education, ethnicity, and marital status, cause of visit, mode of visit, number of visits or length of stay were entered as independent variables and each domain was entered as a dependent variable in separate regression models. We converted non-quantitative variables to dichotomous nominal variables.
Results
Fourteen out of 215 ambulatory patients and 28 out of 227 hospitalized patients were unwilling or unable to respond to the questionnaire (respective response rates: 93% and 88%).
Patient characteristics were meaningfully different between two groups as shown in table 2. In summary, hospitalized patients were older, less educated and more likely to be men and speak Azari.
Table 2:
Comparison of demographic characteristics between ambulatory and hospitalized patients
| Characteristic | Ambulatory participants number (percentage) or mean | Hospitalized patients number (percentage) or mean | P value | |
|---|---|---|---|---|
| Total | 201 | 199 | ||
| Age (year) | 34.73 | 42.02 | <0.001 | |
| Years of education | 8.61 | 6.81 | <0.001 | |
| Female sex | 154 (77%) | 101 (50.8%) | <0.001 | |
| Turkish speaking | 2 (1%) | 41 (20.6%) | <0.001 | |
| Marital status | Single | 62 (30.8%) | 36 (18.2%) | 0.04 |
| Married | 130 (64.7)% | 152 (76.8%) | ||
| Divorced | 3 (1.5%) | 3 (1.5%) | ||
| Widow | 6 (3%) | 7 (3.5%) | ||
| Reason of visit | Referral | 80 (39.8%) | 31 (15.7%) | <0.001 |
| Emergency | 11 (5.5%) | 24 (12.2%) | ||
| Ambulatory | 93 (46.3%) | 44 (22.3%) | ||
| Voluntary | 17 (8.5%) | 98 (49.7%) | ||
| Mode of visit | Taxi | 72 (36.9%) | 17 (8.7%) | <0.001 |
| Bus | 63 (32.3%) | 55 (28.1%) | ||
| On-demand taxi | 18 (9.2%) | 51 (26%) | ||
| On foot | 37 (19%) | 60 (30.6%) | ||
| Personal car | 5 (2.6%) | 13 (6.6%) | ||
| Number of visits | Once | 141 (70.1%) | 1–4 days 23 (11.8%) | - |
| Twice | 28 (13.9%) | 5–10 days 122 (62.6%) | ||
| Three times | 32 (15.9%) | >10 days 50 (25.6%) | ||
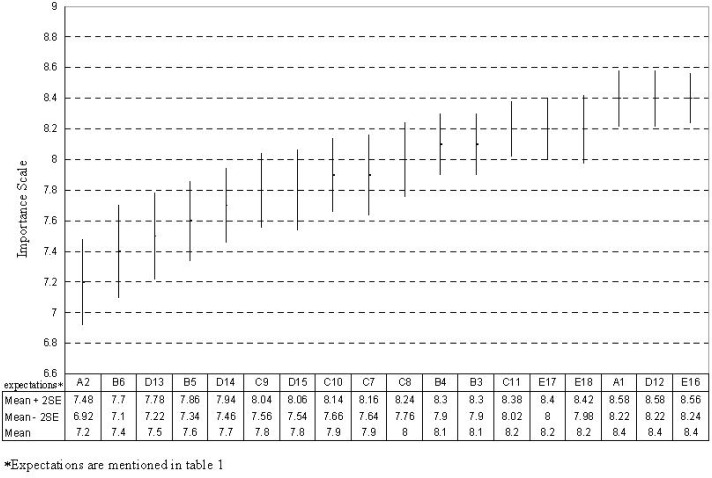
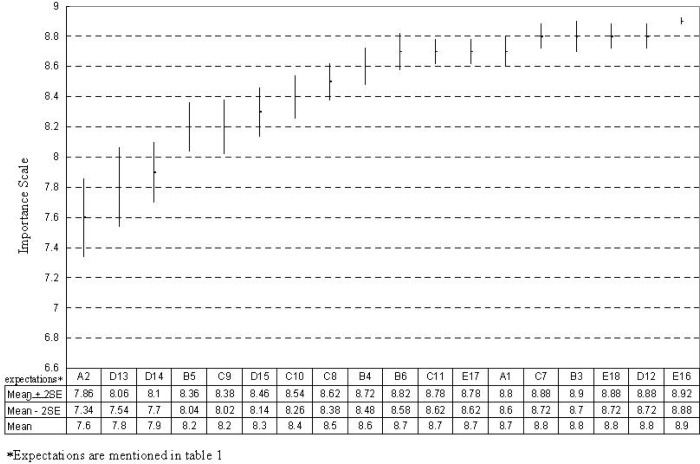
Responses given to the items included in five domains are shown in figures 1 and 2 for hospitalized and ambulatory patients. For all items hospitalized and ambulatory patients’ responses are statistically different (P< 0.05) except for of D13 (“decency”) and D14 (“cost of care”) items.
Fig. 1:
Patient expectations in order of importance in the hospitalized group
Fig. 2:
Patient expectations in order of importance in the ambulatory group
The patients were also asked to rate the five domains in order of priority, starting from 1 for the lowest priority to 5 for the highest. The response to this question was significantly different between the two groups (P< 0.05) (Table 3).
Table 3:
Comparison of priorities between ambulatory and hospitalized patients
| Domain priorities for ambulatory patients | Domain priorities for hospitalized patients | ||
|---|---|---|---|
|
| |||
| Mean (SE) | Mean (SE) | ||
| Physician competency and quality of care | 4.4 (0.06) | Physician competency and quality of care | 3.8 (0.09) |
| Giving information and patient autonomy | 3.21 (0.07) | Physician availability | 3.5 (0.09) |
| Physician availability | 2.9 ((0.07) | Giving information and patient autonomy | 2.8 (0.08) |
| Doctor-patient relationship | 2.5 (0.08) | Compassion | 2.6 (0.09) |
| Compassion | 1.8 (0.09) | Doctor-patient relationship | 2.1 (0.08) |
Ambulatory patients
No variable significantly explained variation in “physician availability” or “competency and quality of care” domains.
Persian speaking patients (β=−0.14, P= 0.04) and those using own car or on-demand taxi (β= −0.27, P< 0.001) to arrive at the center gave significantly less importance to “information and patient autonomy” domain (R2=15%). No other influential factors were identified.
For “compassion” domain, mode of visit and years of education were meaningfully related to the domain (R2=19%). Patients using own car or on-demand taxi for the visit gave significantly more importance to this domain (β= 0.22, P= 0.002). Increase in years of education was associated with decreased importance of this domain (β= −0.31, P< 0.001).
Level of education, age, and marital status meaningfully affected prioritizing the “doctor-patient relationship” domain (R2= 9%). Married patients and those with more years of education gave more importance to this domain (β=0.21, P= 0.01; β=0.18, P= 0.02), while higher age was associated with a decreased importance (β= −0.17, P= 0.048).
Hospitalized patients
Regression analysis of responses provided by hospitalized patients showed no relation between background factors and “physician availability” and “information and patient autonomy” domains.
“Doctor-patient relationship” domain was significantly less important for women and those with more years of education (β= −0.19, P= 0.01; β= −0.21, P= 0.014; R2= 11%).
Patients with more years of education gave significantly higher scores to the “competency and quality of care” domain (β= 0.31, P< 0.001) while other variables had no significant contribution (R2= 15%).
Discussion
Our study showed that patients’ most important expectations fall into “competency and quality of care” domain followed by “information and autonomy” in ambulatory and “physician availability” in the hospitalized patients.
Demographic characteristics were widely different between the ambulatory and the hospitalized groups. While the medical center under study is equipped with specialty wards and serves as a referral center providing inpatient services for patients from all around the country, the majority of patients seeking ambulatory consultation are residents of Tehran; hence the demographic differences were anticipated. Heterogeneous demographic traits may naturally lead to distinctive expectations.
In short, for ambulatory patients the top five expectation items were: doctor expertise (E16), courteousness (D12), consultation with other physicians in case of need (E18), giving clear explanation (B3), and doctors’ patience and attentiveness (C7). For the hospitalized patients the top five were: doctor expertise (E16), courteousness (D12), on time visit (A1), consultation with other physicians in case of need (E18), and setting following appointments (E17). In other words, for both ambulatory and hospitalized patients competency, courteousness and consultation with other physicians where needed were among the top priorities of the patients.
In Schattner et al. study, competency, patience and attentiveness were selected as top priorities by patients (9). In other studies on ambulatory patients doctor-patient relationship ranked first in the list of patient expectations (5, 14, 15). Wensing et al. systematically reviewed nineteen studies regarding patient preferences and demonstrated that most desirable issues for patients were competency, joint decision-making, time spared for the patient, and information while accessibility and organizational issues received less importance (10). Our findings for ambulatory and not hospitalized patients were similar to Wensing et al., while hospitalized patients gave high importance to physician’s availability. This can be explained in part by difference in severity of illness between inpatients and outpatients. Furthermore, in our setting, patients’ basic expectations for availability and consistency of care might not have been fulfilled, and hence dissatisfaction of patients with timing of visits and concerns over follow up appointments after discharge may have led to their greater concern about these items. Eventually, in Iran patients have limited access to physicians in public (and especially academic) hospitals. The short-term relationship between under-training physicians (interns and residents) and the patients may be further disrupted by frequent rotations and shift changes resulting in patient dissatisfaction.
The results of our study highlight the importance of professional expertise, as the domain most valued by patients, and supports efforts toward enhancement of scientific and practical skills. A common finding in both groups was appreciation of professional consultation when necessary. This indicates the fact that patients do not regard consultation as a sign of incompetence, on the contrary they appreciate physician’s efforts and concern about their well-being.
Courteousness, a priority for both hospitalized and ambulatory patients, is achievable at a very low cost but can dramatically improve patient satisfaction. Patients are likely to be frail and vulnerable therefore, it is necessary that physicians treat them with utmost patience and friendliness and talk to them about their even sometimes unreasonable expectations. However, this is only possible through provision of suitable conditions at work in addition to training and preparation of appropriate cultural grounds. A physician who has been on duty for 24 hours is more likely to be bad-tempered than one who has benefited enough rest at home.
A number of studies have investigated the effect of various demographic factors such as age (16) and education (17) on patient expectations. In our study however, these factors had little predictive value with years of education, as an indicator of socioeconomic status, being the most influential factor for a few domains. Although mode of arrival to the center was also analyzed as an estimate for socioeconomic status, it lacks validity since it reflects only one event of arrival. This is further confirmed by inconsistency observed between effects of mode of arrival on expectation domains compared with years of education.
Despite the valuable insight provided by this study, it should be noted that modification of behavior based on the preferences of the average patient will not necessary lead to a high patient satisfaction and that individual patient needs should be addressed and met. In this regard, physicians should bear in mind the importance of fulfillment of patient preferences and medical centers should adopt policies that will facilitate this approach.
Our study was limited in a number of ways. Although ranking is an excellent method to discover the most important patient expectations, a considerable fraction of the participants were illiterate and could not use a self-answered questionnaire, therefore an interviewer had to question them about each item. As shown by the pre-test, it was not possible for the patients to keep all the items in mind and prioritize them; therefore, we had to use VAS method to analyze and compare the importance of expectations. Since the participants valued all the items highly (gave them high scores), there was little difference between the expectation scores and did not provide an accurate ranking. Nevertheless, the highest and lowest priorities were demonstrated with an acceptable certitude.
The hospital under study has some distinctive features that make it difficult to generalize our findings to patients attending other centers around the country. However, the results can be used to anticipate patient expectations in similar centers. It would be worthwhile to conduct similar studies in hospitals with different settings. Moreover, our results are suitably similar to those of other studies. This shows that there are not major differences (with few exceptions) between Iranian patients’ expectations and those reported in the literature.
In conclusion, to our knowledge, this is the first study in Iran that explores patients’ expectations of a “good physician” with the above method. In summary, we conclude that patients expect their doctors to not only improve their knowledge and skill but also to treat them courteously, to provide them with relevant information and to listen to them patiently. They also appreciate the physician consult his colleagues when his own skill or knowledge falls short along the course of care.
Acknowledgments
According to contract number 132/10850 dated Feb 7, 2007, this study was funded by Tehran University of Medical Sciences. The authors wish to thank Dr Saharnaz Nejat who assisted us in reliability and validity evaluation of the questionnaire. The authors declare that they have no conflict of interest.
References
- 1.Neuberger J. The educated patient: new challenges for the medical profession. J Intern Med. 2000;247:6–10. doi: 10.1046/j.1365-2796.2000.00624.x. [DOI] [PubMed] [Google Scholar]
- 2.Schattner A, Bronstein A, Jellin N. Information and shared decision-making are top patients’ priorities. BMC Health Serv Res. 2006;6:21. doi: 10.1186/1472-6963-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levinson W, Gorawara-Bhat R, Lamb J. A study of patient clues and physician responses in primary care and surgical settings. JAMA. 2000;284:1021–7. doi: 10.1001/jama.284.8.1021. [DOI] [PubMed] [Google Scholar]
- 4.Marvel MK, Epstein RM, Flowers K, Beckman HB. Soliciting the patient’s agenda: have we improved? JAMA. 1999;281:283–87. doi: 10.1001/jama.281.3.283. [DOI] [PubMed] [Google Scholar]
- 5.Grol R, Wensing M, Mainz J, Ferreira P, Hearnshaw H, Hjortdahl P, et al. Patients’ priorities with respect to general practice care: an international comparison. European Task Force on Patient Evaluations of General Practice (EUROPEP) Fam Pract. 1999;16:4–11. doi: 10.1093/fampra/16.1.4. [DOI] [PubMed] [Google Scholar]
- 6.Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med. 2002;17:243–52. doi: 10.1046/j.1525-1497.2002.10905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Little P, Everitt H, Williamson I, Warner G, Moore M, Gould C, et al. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. BMJ. 2001;323:908–11. doi: 10.1136/bmj.323.7318.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kassirer JP. Incorporating patients’ preferences into medical decisions. N Engl J Med. 1994;330:1895–96. doi: 10.1056/NEJM199406303302611. [DOI] [PubMed] [Google Scholar]
- 9.Schattner A, Rudin D, Jellin N. Good physicians from the perspective of their patients. BMC Health Serv Res. 2004;4:26. doi: 10.1186/1472-6963-4-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wensing M, Jung HP, Mainz J, Olesen F, Grol R. A systematic review of the literature on patient priorities for general practice care. Part 1: Description of the research domain. Soc Sci Med. 1998;47:1573–88. doi: 10.1016/s0277-9536(98)00222-6. [DOI] [PubMed] [Google Scholar]
- 11.Jung HP, Wensing M, Grol R. What makes a good general practitioner: do patients and doctors have different views? Br J Gen Pract. 1997;47:805–9. [PMC free article] [PubMed] [Google Scholar]
- 12.Grol R. Quality improvement: an international commodity? Qual Health Care. 1996;5:1–2. doi: 10.1136/qshc.5.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Asghari F, Mirzazadeh A, Fotouhi A. Patients’ preferences for receiving clinical information and participating in decision-making in Iran. J Med Ethics. 2008;34:348–52. doi: 10.1136/jme.2007.021873. [DOI] [PubMed] [Google Scholar]
- 14.Baron-Epel O, Dushenat M, Friedman N. Evaluation of the consumer model: relationship between patients’ expectations, perceptions and satisfaction with care. Int J Qual Health Care. 2001;13:317–23. doi: 10.1093/intqhc/13.4.317. [DOI] [PubMed] [Google Scholar]
- 15.Ogden J, Jain A. Patients’ experiences and expectations of general practice: a questionnaire study of differences by ethnic group. Br J Gen Pract. 2005;55:351–56. [PMC free article] [PubMed] [Google Scholar]
- 16.Lin CT, Albertson GA, Schilling LM, Cyran EM, Anderson SN, Ware L, et al. Is patients’ perception of time spent with the physician a determinant of ambulatory patient satisfaction? Arch Intern Med. 2001;161:1437–42. doi: 10.1001/archinte.161.11.1437. [DOI] [PubMed] [Google Scholar]
- 17.Toubai S, Dehbozorgi G. Patients’ Expectations of Internist, Pcychologists and Surgeons. Hormozgan Medical Journal. 2004;8:41–7. [Google Scholar]