Abstract
Despite importance of blood transfusion services as life saving procedures, some countries are unable to meet their national requirements for blood and blood components in a timely manner. Since establishment of Iran Blood Transfusion Organization (IBTO) in 1974 as an integral part of national health system, Iran has experienced a drastic improvement both in availability and safety of blood and blood products. Iran now has not only reached to a 100% non remunerated voluntary blood donation but also secured a national self sufficiency of blood and blood components. Efforts of IBTO as the sole player of transfusion medicines in Iran enabled the country for timely providing of life saving blood transfusion services for all Iranian patients in need of such services. In order to meet the country’s demand in 2011 about 2 million units of whole blood for a population of about 75 million collected by IBTO. This indicates 26.2 donations per 1000 population. Currently about 94% of blood donors in Iran are 25–35 years old males and contribution of female donors in blood donation is less than 6%. IBTO screen all donated blood for important transfusion transmissible infections such as HBV, HIV, HCV and syphilis. Prevalence of HBsAg, HCV and HIV in donated blood in IBTO in 2011 was 0.20%, 0.06% and 0.004% respectively.
Keywords: Iran Blood Transfusion Organization, Blood safety, Blood donation
Introduction
Iran, a country with a population of about 75 millions, is one of the most populated countries of the Middle East. Due to substantial investments by the government of Iran on health care system in past decades the country now enjoys a fairly advanced health system infrastructure. Iran has a primary healthcare network covering the entire population of the country. Iran Ministry of Health (MOH) is the responsible body for providing and regulating health care services for the nation. This includes services related to the transfusion medicine.
Blood transfusion is an essential component of health care which worldwide saves millions of lives each year. Despite encouraging results, researches are not able to introduce artificial substitutes that can routinely replace the need for donated human blood. Therefore, blood and blood components are still required for the management of patients suffering from cancer, blood diseases, trauma and emergencies. In some countries, transfusion is mostly used to support advanced medical and surgical procedures e.g. cardiovascular surgery, neurosurgery and transplantation. However, in developing countries majority of blood is used to treat trauma cases, women with obstetric emergencies and children suffering from severe anemia and malnutrition. Therefore, lack of access to sufficient quantities of safe blood and its components may compromise the obvious right of patients to health care. While the need for blood is universal, millions of patients requiring transfusion do not have timely access to safe blood and there is also a major imbalance between developing and high income countries in access to safe blood.
According to WHO statistics (1) about 48% of around 92 million blood donations which are collected annually worldwide from all types of blood donors (voluntary, family/replacement and paid) collected in high-income countries. These countries are home to about 15% of the world’s population. On the other hand residents of 43 countries in the African region with more than 12% of world population reported collecting only 4 million units of blood (represents for 4.3% of global donations). Although in 62 countries including Iran, national blood supplies are based on 100% voluntary unpaid blood donations, in 40 countries less than 25% of their national blood supplies donated by voluntary blood donors (2).
In Iran blood transfusion is an integral part of the national health system. Blood donation is voluntary and unpaid and blood and its components may not be a source of income. The costs of collection, components preparation, preserving and distribution of blood and its components are paid by the government. Currently blood and its components are free of charge for all Iranian patients in need of such treatments.
New era of blood transfusion in Iran started in 1940s with a non centralized and inappropriately supervised service. Until the early 1970s Iran had no organized blood service and the requirements of hospitals were supplied by commercial and “professional” blood donors. Since 1970s Iran has adopted the basic principles of blood safety criteria set by WHO for a national blood organization (3) including well organized nationally coordinated blood transfusion services with quality systems in all areas, the collection of blood only from voluntary non-remunerated blood donors of low risk populations, the quality assured testing of all donated blood, the safe and appropriate use of blood and blood products and global collaboration for blood safety.
In 1974 based on a parliamentary law, Iran Blood Transfusion Organization (IBTO) was established in order to centralize all blood transfusion activities from donor recruitment to production of blood components and delivery of blood and blood products under one umbrella. The law banned all other public and private organizations to perform any activity in blood transfusion section. The establishment of IBTO was a milestone toward emergence of a developed and scientifically based blood transfusion system in Iran.
IBTO is a public and non-profit organization that relies on the government of Iran for its financial budget and delivers all of its basic services including produced basic blood components free of charge both to the public and private hospitals. According to its constitution the main scope and responsibilities of IBTO are to define standards for transfusion services, to recruit voluntary donors and conduct donation screening tests, to develop blood supply network throughout the country and to prepare blood components and deliver them to health centers. Self sufficiently of country for blood and blood components has always been one of the main objectives of IBTO. Therefore IBTO has spent enormous efforts on increasing blood collection form volunteer donors.
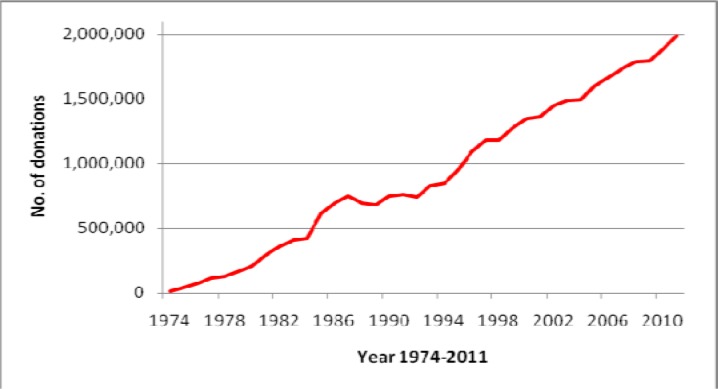
During Islamic revolution in 1978–79, blood donation statistics shows a peak (Fig. 1). This is due to the need to more blood for treatment of injuries from street conflicts between people and the regime forces. This trend was also continued afterward during an eight year long (1980–88) war of Iraq against Iran. Despite the long period of the war blood supplies had been always adequate to meet needs of the war related injuries.
Fig. 1:
Trend of blood donation in Iran, 1974–2011
Currently 283 fixed blood donation sites are available throughout the country which collects 80% of the donated blood. Mobile collecting blood units at work places, educational institutes and cities are responsible for collecting the other 20%. In 2011 Iranian donors donated about 2 million units of blood (Fig. 1). Despite the fact that Iran population has increased about 24% between 1996 and 2010 Fig. 1 shows a 74% increase in blood donation by the donors during this period. In recent decade administration of whole blood in health centers of Iran has drastically declined and therefore majority of donated blood are converted to blood components including RBC, platelets and plasma. Due to high number of thalessemic patients in Iran, more than 25% of packed RBCs produced by IBTO are administered to these patients (4).
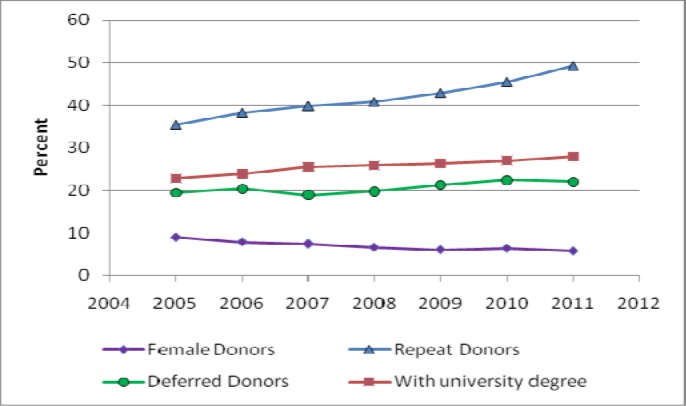
Demographic evaluation of Iranian blood donors indicates that most of the donors are educated young male donors. More than 51% of blood donors in IBTO aged between 25–35 years. Currently about 28% of donors have a university degree showing an increase from 22% in 2002 (Fig. 2). Obviously in addition to educational activities of IBTO increasing literacy rate among general population has contributed to this improvement. Although it is reported that about 39% of blood donors worldwide are women (1), participation of women in blood donation in Iran is very low and female donors consist only 6% of Iranian blood donors (Fig. 2).
Fig. 2:
Characteristics of blood donors at IBTO
Despite increasing campaign by IBTO to recruit more female donors, blood donation by Iranian women has declined in past decade. Implementation of more strict national standards for blood donation has increased percentage of deferred potential donors from blood donation. Percent of potential donors who deferred from blood donation has increased from 14% in 2001 to about 22% in 2011 (Fig. 2). Causes related to safety of donors such as low blood pressure, low hemoglobin (5) and low weight are the main reasons for deferral of potential donors at IBTO. However, in addition to this some very strict regulations regarding to potentially risky behaviors including travel to some specific regions or possible risky sex behaviors are among other reasons for increasing percentage of deferred potential donors. All donors in IBTO centers meticulously interviewed and physically examines by trained physicians. Although this has caused to substantial deferral of the donors from donation, it has significantly improved safety profile of donated blood in Iran.
Today developing countries face considerable obstacles to ensuring a safe blood supply and safe blood transfusions. The leading source of blood in the less developed and developing countries is replacement donors. However Iran has successfully removed “family donors” from its national transfusion policy. Since 2007 Iran has reached to a 100% voluntary donation and IBTO collect blood only from non remunerated voluntary blood donors (2). After reaching to 100% voluntary donation IBTO has focused on increasing share of “repeat” donors in national blood pool. This is mainly because repeat donors have a better safety profile (6) and IBTO could rely on these donors for improving the blood safety profile at national level. Currently more than 49% of Iranian blood donors are repeat donors (Fig. 2).
Current status of blood safety in Iran
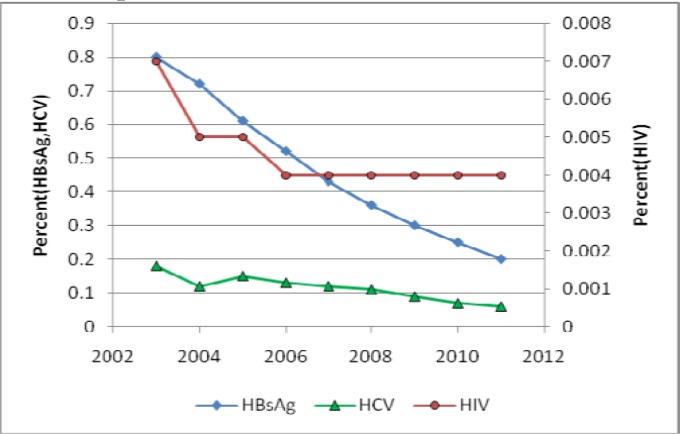
Serious blood shortages and the lack of a reliable donor base and inadequate quality assurance system for screening donors and testing donated blood contribute to an increased risk of transfusion-transmitted infections such as HIV and viral hepatitis. An inadequate stock of blood forces a reliance on unsafe replacement or paid donors and also increases the risk of the issue of blood without adequate testing. Therefore, many recipients are exposed to avoidable, life-threatening risks through the transfusion of unsafe blood. According to data published by WHO (1) in 39 countries blood donations are still not routinely tested for transfusion-transmissible infections including HIV, hepatitis B, hepatitis C and syphilis and 47% donations in low-income countries are tested in laboratories without quality assurance. The essential purpose of IBTO is a sufficient supply of blood and blood components with maximum efficiency and minimum risk to the donors and recipients. The main purpose of donor selection procedures including donor interview and physical examination by a qualified physician and testing procedures are protection of the donors and minimizing the adverse reaction from blood donation. In Iran in addition to the screening of the donors through interviewing, all donated bloods undergo lab testing for possible presence of important and known blood borne disease including HBV, HCV, HIV and Syphilis. Currently IBTO uses serological (Ab/Ag) methods for screening of donated bloods and has recently implemented a pilot NAT system in its screening protocol for donated bloods. Percent of confirmed HBsAg positive samples in blood donated by Iranian donors has drastically decreased from 0.8% in 2002 to 0.20% in 2011. Although this is partly due to national strategies on controlling HBV in general population (7), improving donor selection and screening strategies at IBTO have also significantly contributed to this achievement. Prevalence of confirmed HCV positive results in donated bloods has also decreased from 0.18% in 2002 to 0.06% in 2011. Despite increasing prevalence of HIV in general population, IBTO succeeded to reduce confirmed positive HIV samples in donated bloods from 0.007% in 2002 to 0.004 in 2011 (8–9). Figure 3 shows trend of prevalence of important transfusion transmissible infections in IBTO in past decade.
Fig. 3:
Trend of prevalence of important transfusion transmissible infections in IBTO
Although currently IBTO is evaluating cost effectiveness of implementing a NAT system for improvement of blood safety, it has recognized that implementation of an efficient look-back and hemovigilance system can contribute effectively to improve blood safety. Therefore, IBTO has also recently implemented a nationwide hemovigilance system as a powerful tool to improve transfusion safety. Currently implemented “look back” system in IBTO is mainly concern with reports about safety of the blood and blood components (10). Every report indicating possible breach of safety of the donated bloods and/or patients receiving blood and blood components will be seriously traced through the product identity to the donors for appropriate actions.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc) have been completely observed by the authors.
Acknowledgments
The authors declare that there is no conflict of interest.
Reference
- 1.Key global facts and figures in 2011, WHO Blood safety; www.who.int/worldblooddonorday/media/who_blood_safety_factsheet_2011.pdf
- 2.Countries that reported having achieved 100% voluntary non-remunerated blood donation in 2008; WHO, www.who.int/bloodsafety/voluntary_donation/countries_100pct_vnrbd_2011.pdf
- 3.Screening donated blood for transfusion transmissible infections, WHO, www.who.int/bloodsafety/ScreeningDonatedBloodforTransfusion.pdf [PubMed]
- 4.Abolghasemi H, Amid A, Zeinali S, Radfar MH, Eshghi P. Thalassemia in Iran: epidemiology, prevention and management. J Pediatric Hematol Oncol. 2007;29:233–8. doi: 10.1097/MPH.0b013e3180437e02. [DOI] [PubMed] [Google Scholar]
- 5.Maghsudlu M, Nasizade S, Toogeh GhR, Zandie T. Short-term ferrous sulfate supplementation in female blood donors. Transfusion. 2008;48:1192–7. doi: 10.1111/j.1537-2995.2007.01671.x. [DOI] [PubMed] [Google Scholar]
- 6.Ibrahim NA, Mobley MF. Recruitment and retention of blood donors: a strategic linkage approach. Health Care Manage Rev. 1993;18:67–73. doi: 10.1097/00004010-199301830-00008. [DOI] [PubMed] [Google Scholar]
- 7.Alavian SM, Hajarizadeh B, Kabir A, Bagheri-Lankarani K. Hepatitis B Virus infection in Iran: A systematic review. Hepat Mon. 2008;8:281–294. [Google Scholar]
- 8.Cheraghali AM. Blood safety concerns in the Eastern Mediterranean region. Hepat Mon. 2011;11:422–6. [PMC free article] [PubMed] [Google Scholar]
- 9.Abolghasemi H, Maghsudlu M, Amini Kafiabad S, Cheraghali AM. Introduction to Iranian Blood Transfusion Organization and blood safety in Iran. Iranian J Publ Health. 2009;38:s1, 82–87. [Google Scholar]
- 10.Cheraghali AM, Abolghasemi H. Plasma fractionation, a useful means to improve national transfusion system and blood safety: Iran experience. Hemophilia. 2008:1–7. doi: 10.1111/j.1365-2516.2008.01936.x. [DOI] [PubMed] [Google Scholar]