Abstract
This paper provides a short overview of the Danish health care system and the organization of care for type 2 diabetes patients in Denmark. It also describes the supplementary data sources that are used for collection of baseline data in the nationwide Danish Centre for Strategic Research in Type 2 Diabetes (DD2) Project. The Danish National Health Service provides tax-funded medical care for all 5.6 million Danish residents. The health care system is characterized by extensive individual-level registration of data used for planning, administration, quality improvement, and research. It is estimated that there are currently at least 250,000 individuals with known diabetes in Denmark (approximately 4.5% of the Danish population), of which an estimated 80% are followed and treated by their general practitioners and approximately 20% are followed at hospital specialist outpatient clinics. These health care providers form the basis for recruiting diabetes patients in the DD2 project, and the data sources that these providers use in clinical practice give access to important supplementary patient data. The DD2’s patient-enrollment system is designed to be fast and simple, and thus only collects primary interview data that cannot be extracted from already existing data sources. Thus, in addition to an online DD2 questionnaire filled out by general practitioners and hospital physicians at the time of patient enrollment, supplementary data are obtained from the Danish Diabetes Database for Adults, a nationwide clinical quality improvement registry. Both hospital physicians and a growing number of general practitioners routinely report data to this database. For general practitioners, the Danish General Practice Database acts as an important feeder database for the Danish Diabetes Database for Adults and thereby also for the DD2 project.
Keywords: type 2 diabetes, data sources, epidemiology, health care, Danish Diabetes Database for Adults (DDDA), Danish General Practice Database (Dansk AlmenMedicinsk Database [DAMD])
Introduction
The nationwide Danish Centre for Strategic Research in Type 2 Diabetes (DD2) Project will be one of the world’s largest prospectively designed diabetes research projects. The DD2 project started enrolling the first patients in the pilot study phase in November 2010. Patient enrollment and data collection in the DD2 project takes advantage of Denmark’s universal national health care system covering all citizens and residents. The extensive registration of individual-level data in the Danish health care system makes it possible to retrieve valuable information from existing data sources covering the entire health care system. It is thus possible to extract and link individual patient health care data from both primary care general practitioners (GPs) and from all hospitals in Denmark. This paper provides a short overview of the Danish health care system and the organization of care for type 2 diabetic patients in Denmark. The paper also describes the supplementary data sources used for collecting baseline data in the DD2 project.
Organization of health care in Denmark
Denmark has 5.6 million inhabitants and is a welfare state with tax-financed universal access to health care services.1 The Danish National Health Service thus guarantees unfettered free access, from the point of delivery to primary and secondary health care, and provides partial reimbursement for prescribed medications. Except for emergencies and certain conditions cared for by privately practicing eye specialists, ear, nose, and throat specialists, and dermatologists, patients’ initial contact with the health care system is always through their GP.1 GPs act as gatekeepers and provide referrals to public hospital-based specialist physicians, when necessary. The primary health care sector consists of about 3600 GPs, 1200 privately practicing specialists, and 4600 dentists, as well as physiotherapists, chiropractors, and home nurses. In addition, Denmark has about 300 community pharmacies.2 Home care services are delivered by the 98 municipalities in Denmark, and this system is also unfettered and free. The secondary health care sector currently consists of approximately 40 public hospitals run by the five administrative Danish regions.1 The hospital structure is changing toward fewer hospitals and more specialized and centralized care. There are also a number of private hospitals and clinics mainly providing elective surgical treatment; however, the private hospitals and clinics provide neither services related to emergencies nor treatment or follow-up of patients with chronic conditions, including diabetes.
The Danish health care registries
Danish health care, disease, and population registries are recognized as being among the best in the world, in particular because of their large size, long record period, high validity, and completeness.3 The extensive data registration in the Danish health care system is based on the Danish National Health Service. Since 1968, all Danish residents have been assigned a unique personal identifier, the civil registration number, which is used in all public data sources and which facilitates unambiguous computerized record linkage.4
In order to design a fast, simple patient-enrollment system for the DD2 project, we have based the system on the unique possibility offered by the Danish registries to withdraw well-defined data from data sources covering the entire health care system. The registries make us able, at regular intervals, to recover individual-level data about the quality of diabetes care. For example, we can obtain data on glycemic control, blood pressure, and lipid profiles for individual patients enrolled in the DD2 project. These data sources will also be used to detect and follow newly enrolled patients with type 2 diabetes over time.
Diabetes care and epidemiology in Denmark
Adult patients with type 2 diabetes in Denmark are most often diagnosed for the first time by their GP. They may then be followed and treated by their GP, or referred to diabetes outpatient specialist clinics at the public hospitals, at the discretion of their GP. The system of diabetes care is not static; ie, there is a continuous flow of diabetic patients between primary care and the hospital outpatient clinics, and vice versa. The presence of chronic diabetes complications increases the likelihood of referral to a hospital outpatient clinic.
The Danish National Diabetes Register5,6 monitors the incidence and prevalence of diagnosed diabetes in the Danish population with three linked nationwide medical databases that include diabetes data from primary and secondary health care:
the Danish National Patient Register7 (containing inhospital and outpatient contacts with a recorded diagnosis of diabetes),
the Danish National Health Service Register8 (containing information on all primary care services provided by general and specialist practitioners in Denmark, including glucose measurement and chiropody services for patients with diabetes),7 and
the Danish National Prescription Registry9,10 (containing information on all prescriptions for antidiabetic drugs issued by hospital physicians or GPs and dispensed at Danish pharmacies).
The estimated coverage of the Danish National Diabetes Register, as compared with diabetes diagnoses confirmed by the patients’ GPs, is 96%.6 The number of new (incident) cases with diabetes was estimated at approximately 25,000 individuals per year, between 2005 and 20095 (for updated numbers, see http://www.sst.dk/Indberetning%20og%20statistik/Sundhedsdata/Diabetes.aspx). It is estimated that there are currently at least 250,000 individuals with known diabetes in Denmark, corresponding to 4.5% of the entire population. The prevalence of known diabetes has increased 2.5-fold since 1995, likely due to a real increase in diabetes incidence together with an increase in diagnostic intensity.6 Of the 250,000 diabetic individuals, an estimated 200,000 patients (80%) are followed and treated by their GPs, and 50,000 patients (20%) are followed at hospital outpatient clinics. There are virtually no privately practicing diabetes specialists providing diabetes care outside the hospital clinic setting.
Enrollment of patients in the DD2 project
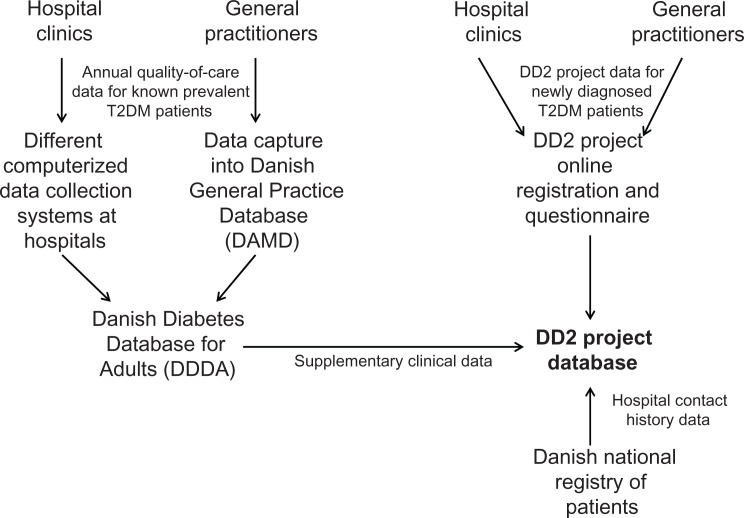
As seen from the above paragraph, the GPs and hospital outpatient clinics are the natural basis for recruiting patients to the DD2 project. The logistics of patient enrollment and data entry in the DD2 project is described in more detail by Nielsen et al,11 whereas the collection of DD2 baseline patient data from additional supplementary data sources is described in the next section. In brief, enrollment in the DD2 project consists of baseline registration by GPs and hospital physicians (see Figure 1) of selected patient-specific variables via an online questionnaire form and the collection of blood and urine samples to be stored in a biobank. The DD2 online registration form and samples are described in detail in Nielsen et al.11 The baseline data are electronically transferred to the DD2 database managed by the Department of Clinical Epidemiology at Aarhus University Hospital (see http://www.dce.au.dk) (Figure 1). The DD2 enrolled the first patient in November 2010. The goal is to enroll 10,000 patients annually when fully implemented, and to enroll 50,000 patients in total over a period of at least 5 years.
Figure 1.
Flow chart.
Supplementary data sources for DD2 baseline data
Patients enrolled in the DD2 database have their primary data linked with other data sources, both to enrich baseline variables and to collect subsequent outcome data. The collecting of subsequent outcomes during follow-up is described in detail in Beck-Nielsen et al.12 For collecting additional baseline data in the DD2 project, the key data source is the Danish Diabetes Database for Adults (DDDA) (Figure 1). Both hospital physicians and a growing number of GPs routinely transfer diabetes data to the DDDA; this database will be described in more detail in the following section.
The Danish Diabetes Database for Adults (DDDA)
The DDDA is one of several nationwide public clinical quality improvement registries financed and operated by the Danish Regions (see http://www.nip.dk). The aim of the DDDA is to monitor and improve the quality of diabetes care provided by hospitals, GPs, and ophthalmologists in Denmark using a set of quality of care indicators. The DDDA was established in 2005. All patients with ≥17 years of diabetes who have had contact with a hospital outpatient clinic or with a GP in Denmark are eligible for inclusion in the DDDA, and quality of care data must be submitted for them annually. Quality of care indicators include (1) the proportion of diabetic patients who have an annual measurement of HbA1c and blood pressure, a biennial measurement of blood lipids and albuminuria, and regular examinations of eyes and feet; (2) the actual results of these measurements; and (3) the relevant treatments instituted (antidiabetics, antihypertensives, hypolipidemics, ACE-inhibitors, ATII-antagonists). Importantly, these laboratory tests and measurements are mandatory for all patients with diabetes in the DDDA; for example, more than 90% of all patients have their HbA1c and lipids measured regularly. Other variables collected include diabetes type, body mass index, and tobacco smoking. A detailed overview of all baseline data variables available in the DDDA is provided by Thomsen et al.13
DDDA data flow from hospital outpatient clinics
All Denmark’s hospital outpatient clinics caring for patients with diabetes are obliged to report data on diabetes care to the DDDA. At present, approximately 90% of the relevant adult diabetes patients who are regularly followed at hospital specialist outpatient clinics (corresponding to approximately 40,000 individuals) are reported to the DDDA each year by the clinics. Their data are entered by physicians into web-based data management systems, using the patient’s unique civil registration number. From these web-based systems, data are electronically transferred to the DDDA (Figure 1). In the DDDA, individual-level data for diabetes patients from all hospital outpatient diabetes clinics are thus stored, including the prospectively collected patient characteristics and measurements described above. Each participating outpatient clinic in the DDDA continuously receives information on their own performance: the proportion of diabetes patients fulfilling the defined quality of care criteria during the last year. From the DDDA, diabetes data are transferred to the DD2 project database to enrich data collected for DD2 patients (Figure 1). Some data delay can be expected, because the DD2 is meant to enroll newly diagnosed type 2 diabetes patients and collect baseline data from them immediately at diagnosis, whereas the DDDA is meant to collect data from examinations done during the previous year in known prevalent type 2 diabetes patients.13
DDDA data flow from general practitioners
The DDDA has collected data from GPs on a voluntary basis since 2007. Approximately 15% of Danish GPs currently participate and report data to the DDDA, and approximately 9000 diabetes patients had data reported from general practice in 2010. Among the GPs who currently participate in the DDDA, the completeness of inclusion of relevant type 2 diabetes patients is estimated at 90%. The number of GPs who report data to the DDDA is rapidly increasing at present, because all GPs in Denmark are obliged to have an IT program called Sentinel Data Capture installed in their electronic health record systems no later than April 2013. Sentinel Data Capture was developed by the Danish Quality Unit of General Practice (DAK-E) (see http://www.dak-e.dk) in cooperation with the Research Unit for General Practice at the University of Southern Denmark. The IT program is designed to automatically collect key patient data as they are entered into the Danish GPs’ twelve different electronic health record systems nationwide. The collected data include prescribed drugs; National Health Service disbursement codes for services provided (eg, consultations, laboratory tests); Nomenclature, Properties and Units (NPU) codes and International Union of Pure and Applied Chemistry (IUPAC) codes for measurements; and International Classification of Primary Care (ICPC) diagnoses. The NPU and IUPAC codes have been developed to register structured information such as laboratory data and other clinical data (eg, smoking habits and blood pressure) in a systematic and uniform way. All data will be stored in the nationwide Danish General Practice Database (Dansk AlmenMedicinsk Database [DAMD]) (Figure 1), which is meant to systematically collect primary care data for quality improvement and research.
Each GP subscribes individually through his/her own personal computer to the quality development or research projects in which he/she wishes to participate and wants to use Sentinel Data Capture. For example, for the DDDA, when the GP enters the ICPC diagnosis of diabetes (T89 and T90) for a given patient, a pop-up screen will automatically appear once a year, and additional DDDA-relevant data for the patient must be filled in. It takes one to two minutes to fill in the pop-up screen. The necessary diabetes key data from the data capture module and the data from the pop-up screen are automatically transferred to the Danish General Practice Database, and transferred from there to the DDDA (Figure 1). Sentinel Data Capture can also be used for primary DD2 patient data. Thus, the GPs connected to Sentinel Data Capture can have a list in the system containing all his/her diabetes patients eligible for participating in the DD2 project. The list is based on the data from the annual DDDA pop-up screen, and the list is restored online. As soon as the patient is included in the DD2 project, the patient will be automatically removed from the DD2-eligible list. New patients with type 2 diabetes will be automatically included on the list.
Conclusion
Unlike conventional Danish historical, registry-based research that often relies on hospital diagnoses and lacks clinical detail, the DD2 database is designed to collect detailed primary data in newly diagnosed type 2 diabetes patients, including those in the primary care sector. The patient enrollment and data collection in the DD2 project takes advantage of Denmark’s universal national health care system covering all citizens. Because virtually all diabetes patients in Denmark are followed and treated either by their GP or by hospital specialist outpatient clinics, the DD2 project draws on additional computerized diabetes data sources that are already used by the GPs and hospital specialists, to keep the burden of project data registration low. In the first years of the DD2 project, type 2 diabetic patients in hospital care will be over-represented; however, the primary care sector will rapidly catch up, from 2013 onward, due to mandatory GP reporting to the DDDA. In this paper, we have provided, for the interested researcher, a short overview of the Danish health care system and the organization of diabetes care; and we have described the key supplementary diabetes data sources that are used for the collection of baseline data in the DD2 project. Linkage with these and other Danish population-based databases will also enable researchers to follow the quality of care and outcomes over time for patients with newly diagnosed type 2 diabetes included in the DD2 project.
Acknowledgments
DD2 is the acronym for ‘The Danish Centre for Strategic Research in Type 2 Diabetes’ supported by the Danish Agency for Science (grant no. 09-067009 and 09-075724). DD2 is also supported by The Danish Health and Medicines Authority, The Danish Diabetes Association and an unrestricted donation from Novo Nordisk A/S. The partners of the project are listed on the project website www.DD2.nu
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Ministry of the Interior and Health. Health care in Denmark Report. Copenhagen, Denmark, 2008. Available from: http://www.sum.dk/Aktuelt/Publikationer/Publikationer/UK_Healthcare_in_DK.aspx Accessed January 17, 2012.
- 2.Ehrenstein V, Antonsen S, Pedersen L. Existing data sources for clinical epidemiology: Aarhus University Prescription Database. Clin Epidemiol. 2010;2:273–279. doi: 10.2147/CLEP.S13458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frank L. Epidemiology. When an entire country is a cohort. Science. 2000;287(5462):2398–2399. doi: 10.1126/science.287.5462.2398. [DOI] [PubMed] [Google Scholar]
- 4.Pedersen CB. The Danish Civil Registration System. Scand J Public Health. 2011;39(Suppl 7):S22–S25. doi: 10.1177/1403494810387965. [DOI] [PubMed] [Google Scholar]
- 5.Carstensen B, Kristensen JK, Ottosen P, Borch-Johnsen K. The Danish National Diabetes Register: trends in incidence, prevalence and mortality. Diabetologia. 2008;51(12):2187–2196. doi: 10.1007/s00125-008-1156-z. [DOI] [PubMed] [Google Scholar]
- 6.Carstensen B, Kristensen JK, Marcussen MM, Borch-Johnsen K. The National Diabetes Register. Scand J Public Health. 2011;39:58–61. doi: 10.1177/1403494811404278. [DOI] [PubMed] [Google Scholar]
- 7.Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health. 2011;39(Suppl 7):S30–S33. doi: 10.1177/1403494811401482. [DOI] [PubMed] [Google Scholar]
- 8.Andersen JS, Olivarius ND, Krasnik A. The Danish National Health Service Register. Scand J Public Health. 2011;39:34–37. doi: 10.1177/1403494810394718. [DOI] [PubMed] [Google Scholar]
- 9.Leegaard A, Riis A, Kornum JB, et al. Diabetes, glycemic control, and risk of tuberculosis: a population-based case-control study. Diabetes Care. 2011;34(12):2530–2535. doi: 10.2337/dc11-0902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kildemoes HW, Sorensen HT, Hallas J. The Danish National Prescription Registry. Scand J Public Health. 2011;39:38–41. doi: 10.1177/1403494810394717. [DOI] [PubMed] [Google Scholar]
- 11.Nielsen JS, Steffensen C, Thomsen RW, Christiansen JS. The Danish Centre for Strategic Research in Type 2 Diabetes (DD2) study: implementation of a nationwide patient enrollment system. Clin Epidemiol. 2012;4(Suppl 1) doi: 10.2147/CLEP.S30838. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beck-Nielsen H, Solomon TPJ, Lauridsen T, et al. The Danish Centre for Strategic Research in Type 2 Diabetes (DD2): outcome data. Clin Epidemiol. 2012;4(Suppl 1) doi: 10.2147/CLEP.S30655. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thomsen RW, Nielsen JS, Ulrichsen SP, Pedersen L, Hansen A, Nilsson T. The Danish Centre for Strategic Research in Type 2 Diabetes (DD2) study: collection of baseline data from the first 580 patients. Clin Epidemiol. 2012;4(Suppl 1) doi: 10.2147/CLEP.S30083. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]